Abstract
To understand how institutional environments and socioeconomic backgrounds may influence health outcomes, we examined the relationship among special education environments, socioeconomic status (SES), and likelihood of ADHD remission in children. While the majority of children experience remission by adulthood, the likelihood of remission varies across different SES levels and education environments. We find that for low SES children the likelihood of remission is higher in states that have more inclusive special education regimes. In contrast, for more advantaged children, the odds of remission do not depend on the level of special education inclusivity. Our findings suggest that providing more inclusive education can reduce disparities in behavioral disorders and are particularly important for less advantaged children. In doing so, this study contributes to the fundamental cause and health inequality literature by adding to a growing body of work showing how institutional environments can affect socioeconomic gradients in health treatment and outcomes.
Keywords: ADHD, Remission, Inclusive special education, Socioeconomic status, Institutional environment, Health inequalities
Highlights
-
•
The majority of children experience ADHD remission by adulthood
-
•
Low SES children are less likely to experience remission
-
•
Low SES children's odds of remission are higher in states with inclusive education
-
•
High SES children's remission rates are unaffected by education policies
-
•
Inclusive special education may help alleviate childhood health inequalities
Introduction
Three out of four children diagnosed with Attention Deficit Hyperactivity Disorder will no longer meet the diagnostic criteria for ADHD by adulthood (Agnew-Blais et al., 2016). Evidence about the importance of family context and economic advantage on long-term outcomes of children with ADHD is mixed (Agnew-Blais et al., 2016; Faraone, Biederman, & Mick, 2006). To date, little is known about how institutional and educational environments may influence the likelihood of ADHD remission. ADHD remission is known to be associated with improved cognitive functioning such as better attention-vigilance and error detection (Cheung et al., 2016; Michelini et al., 2016). Given the long-term consequences of persistent ADHD, further research investigating whether and how socioeconomic advantage and social context may translate into an increased likelihood of remission is warranted.
A voluminous literature has documented a link between socioeconomic status and health outcomes. For the vast majority of conditions there exists a negative socioeconomic gradient such that individuals with fewer economic resources are more likely to experience adverse health outcomes or early mortality (Link, Northridge, Phelan, & Ganz, 1998; Link & Phelan, 1995). Individuals of higher socioeconomic status draw upon their relatively greater income, education, and social connections to access new services and disproportionately benefit from medical advances (Chang & Lauderdale, 2009; King & Bearman, 2011). This literature would anticipate that economically advantaged children should be more likely than their less advantaged peers to experience ADHD remission.
Institutional environments can also profoundly affect individuals' physical and mental health, and thus have the ability to exacerbate or attenuate health inequalities (Freese & Lutfey, 2011). Research examining the social determinants of health has documented the significant role that prisons, schools, and work environments have on health outcomes (Cutler & Lleras-Muney, 2012; Moen, Kelly, Tranby, & Huang, 2011; Schnittker & John, 2007). Schools themselves have been demonstrated to have an important impact on myriad children's health outcomes including: weight and body mass (Martin, Frisco, Nau, & Burnett, 2012; Miller, 2011; Mueller, Pearson, Muller, Frank, & Turner, 2010), substance use (De Clercq, Pfoertner, Elgar, Hublet, & Maes, 2014; Turner, West, Gordon, Young, & Sweeting, 2006), risk behaviors (Pavic Simetin, Kern, Kuzman, & Pförtner, 2013), stress (Oberle & Schonert-Reichl, 2016), psychosomatic and depressive symptoms (Elovainio et al., 2011; Walsemann, Bell, & Maitra, 2011), and emotional and behavior problems (Dufur, Parcel, & Mckune, 2008; Nielsen et al., 2015; Saab & Klinger, 2010).
With respect to ADHD, schools in particular play an important role in both the diagnosis and treatment of ADHD. In the absence of biomarkers or blood tests for ADHD, diagnoses are made based on symptomatic presentation and evaluations by teachers and parents. Teachers are often the first to suggest a diagnosis of ADHD. Beyond the level of the classroom, scholar have documented that school accountability policies, which scrutinized schools academic performance, are associated with an increased likelihood of ADHD diagnosis and subsequent medication use. Work by King, Jennings, and Fletcher (2014) found that economically advantaged children were more likely than their less advantaged peers to selectively use ADHD medications in response to academic pressure and school accountability. Thus, schools may play a key role in explaining variation in ADHD prevalence and remission.
The past decade has seen a dramatic rise in behavioral disorders diagnosed in childhood. Prevalence rates of ADHD, autism, and bipolar disorder have increased precipitously (Blumberg et al., 2013; Hinshaw & Scheffler, 2014; Visser et al., 2014). Consistent with the fundamental cause literature, strong SES gradients exists for each of these conditions (King & Bearman, 2011; Visser et al., 2014). Our work adds to a growing body of literature that highlights the importance of social context and institutional conditions for understanding both the steep increase in prevalence of childhood behavioral disorders, as well as their socioeconomic gradients (Hinshaw & Scheffler, 2014). While this literature has expanded our understanding of how social contexts have contributed to rising prevalence rates, little research has examined the role that social and institutional conditions play in remission rates. Our study contributes to the literature by showing that special education can either mitigate or exacerbate health inequalities depending on how institutions execute the provision. Understanding how institutions may exacerbate or mitigate health inequalities through differential remission patterns has important implications for the literature on health and inequality, as well as public policy.
This study examines the association between socioeconomic status, educational environments and ADHD remission. Educational environments profoundly shape the likelihood of ADHD remission- but only for less advantaged children. Remission rates of socioeconomically advantaged children do not vary significantly across special education regimes. Creating more inclusive special education environments appears to be a key step towards reducing ADHD disparities.
ADHD prevalence and remission
ADHD is defined as a “persistent pattern of inattention and/or hyperactivity-impulsivity that is more frequently displayed and is more severe than is typically observed in individuals at comparable level of development” (DSM IV [American Psychiatric Association, 2000]). ADHD is the most common psychiatric disorder among children in the United States. Nationally, more than 11% of school-aged youth have been diagnosed with ADHD (Visser et al., 2014). Prevalence rates have risen remarkably in recent years, increasing by more than 40% between 2003 and 2011 alone. There is also considerable geographic variability in how frequently children are diagnosed with ADHD. The percent of school-aged children diagnosed with ADHD varies from a high of 18.7 percent of children in Kentucky to a low of 5.6 percent of children in Nevada (Visser et al., 2014). A large body of work has documented higher rates of ADHD among lower-SES youth (see Russell, Ford, Williams, & Russell, 2015 for review). For instance, data from the National Center of Health Statistics found that.
ADHD prevalence was higher (10.4%) for children whose family's annual income is less than 200% of the federal poverty level than for higher SES children whose families were above the 200% threshold (8.8%). Evidence of rapidly rising prevalence rates, geographic variability, and a strong socioeconomic gradient suggest that social and institutional factors are important drivers of ADHD diagnosis.
Despite considerable scholarly effort directed toward understanding the diagnostic variability, very little is known about what social and institutional conditions are associated with ADHD remission. To explain rapid changes in the measured prevalence of any health-condition, one needs to account for not only how patients obtain the diagnosis but also how they lose the diagnosis. This paper aims to suggest that socioeconomic status — an individual-level factor — and educational environment — an institutional factor — interact to shape remission rates of children with ADHD. Socioeconomic status has long been identified as a fundamental cause of health conditions, creating negative gradients for most health outcomes (Link & Phelan, 1995). This is not only because lower socioeconomic status groups likely have greater exposure to risk factors but also because they lack access to treatment options. Accordingly, we expect that lower SES families will have difficulties accessing and negotiating treatment options. When families lack the resources to secure adequate treatment for their children, behavioral interventions available at school could potentially help mitigate disparities.
Our work highlights the potential role of educational environments in creating ADHD remission gradients. Many treatment modalities of ADHD require parental engagement. However, the sociology of education literature has established that parental engagement may effective for children's educational achievements only when the parents have an adequate cultural understanding of classroom expectations (e.g., McNeal Jr. 2001), thereby producing disadvantages for less advantaged families. In the case of special education, parents with lower socioeconomic status are less likely to participate in school activities and to have expectations that their children will successfully graduate from high school, which has a positive impact on children's academic achievement (Zhang, Hsu, Kwok, Benz, & Bowman-Perrott, 2011). Because of these differences in parental engagement, when families must individually negotiate to obtain the best possible accommodations for their children, children from less advantaged families are less likely to benefit. On the other hand, if special education regimes are more inclusive and prone to provide adjustments for children's individual needs, children from lower socioeconomic backgrounds will benefit.
Roughly, 80 percent of children diagnosed with ADHD no longer meet the full diagnostic criteria by the end of adolescence (Agnew-Blais et al., 2016; Biederman, Petty, O’Connor, Hyder, & Faraone, 2012; Faraone et al., 2006; Kessler et al., 2005). Risk factors associated with ADHD persistence are childhood symptomatic severity (Agnew-Blais et al., 2016; Biederman et al., 2012; Cheung et al., 2015; Kessler et al., 2005), psychiatric comorbidity and family history of mental disorders (Biederman et al., 2011, Biederman et al., 2012), and IQ (Agnew-Blais et al., 2016; Cheung et al., 2015).
Evidence of an association between family socioeconomic status and remission is mixed. Cheung et al. (2015) found that higher socioeconomic status is associated with a decline in ADHD symptoms over time, while others did not find such association (Agnew-Blais JC et al., 2016; Biederman et al., 2011; Biederman et al., 2012; Kessler et al., 2005).
Treatment of ADHD, however, is of vital importance since ADHD poses serious academic and social challenges (Arnold, Hodgkins, Kahle, Madhoo, & Kewley, 2015; Loe & Feldman, 2007). Successfully managing ADHD symptoms not only contributes to successful schooling but also may affect employment outcomes.
Treatment of ADHD among children and adolescents
Treatment of children and adolescents with ADHD can be broadly classified into medical treatment and psychosocial interventions (Chronis, Jones, & Raggi, 2006). Meta-analyses have found that medication combined with behavioral interventions are the most successful treatment for managing ADHD symptoms. Medication is the most common method of addressing ADHD symptoms. In 2011, 69 percent of children with ADHD took at least one prescription medication to manage symptoms (Visser et al., 2014). Most research on ADHD treatment has consistently shown that medication manages ADHD symptoms effectively (for review, see Swanson, Baler, & Volkow, 2011). Stimulants improve academic performance, decrease aggression and inappropriate behavior (Chronis et al., 2006) and facilitate social relationships with peers (Whalen et al., 1989). These effects of pharmacological treatment of ADHD, however, tend to be short-lived. Medication only suppresses symptoms of ADHD instead of curing the underlying disorder. Little is known about long-term effectiveness of medication (Chronis et al., 2006; Craig, Davies, Schibuk, Weiss, & Hechtman, 2015; Smith, Waschbusch, Willoughby, & Evans, 2000), suggesting that pharmacological treatment alone may be insufficient to cause ADHD remission.
There are three major modes of psychosocial treatment: family-, peer-, and school-based interventions. Family-based interventions target parents as the foci of behavioral treatment and are designed to train parents to promote accurate understanding of ADHD symptoms and treatment as well as to modify parenting behaviors. Second, peer-based interventions such as social skills training and summer treatment programs are designed to help improve the social functioning of children and adolescents with ADHD (Chronis et al., 2006). Finally, school-based interventions are designed to improve student's performance at school. Teachers can use behavioral modification strategies to cater special needs of students with ADHD. Specifically, teachers can help students with ADHD to perform academic tasks better by giving them additional academic instructions or materials, structuring homework time, modifying instructions, collaborating with parents as well as having children with ADHD use goal-setting, peer tutoring, computer-assisted instruction, and strategy training (Chronis et al., 2006). Successful implementation of classroom behavior management depends on teachers' willingness to give additional academic instructions and to implement special accommodations and modifications as well as environmental factors that enable teachers and paraeducators to help students with special needs.
School-based interventions may help ameliorate or exacerbate treatment disparities. Other treatment modalities are often stratified by socioeconomic status. First, pharmacological treatment trajectories differ for low and high SES children. That is, low SES children are less likely to adhere to prescribed medications (Brown, Borden, Wynne, Spunt, & Clingerman, 1987; Firestone, 1982). Second, the outcomes of behavioral treatment are also stratified by SES. Low SES children did not show substantial improvement when receiving a combination of medication and behavioral treatment, whereas high SES children's symptoms where significantly improved when they received combined treatment, rather than medication alone (Rieppi et al., 2002). Such differential outcomes may partially have driven by the level of parental engagement. Note that some, if not most, of the school-based treatment methods require a fair amount of collaboration between teachers and parents. However, consistent participation in parental training has been found to be more difficult for parents with fewer economic resources (Firestone & Witt, 1982). They are also less likely to engage in school activities (Zhang et al., 2001). As a result, the effect of family-based interventions is stratified (McMahon, Forehand, Griest, & Wells, 1981). When greater familial advocacy or participation is necessary for children to receive optimal behavioral interventions in school, less economically advantaged children may not fully benefit. On the other hand, schools can be an important arena for less advantaged children to receive behavioral therapy and have the opportunity to develop skills. In this paper, we focus on how differences in school-based treatment processes across states could affect low and high SES children differently, thereby, contributing to SES gradients.
School-based interventions
The Individuals with Disabilities Education Act (IDEA) governs the provision of all special education services in the United States (deBettencourt, 2002). IDEA ensures that students with disabilities are provided with the same educational opportunities as their non-disabled peers. IDEA requires public schools to offer free services to meet the educational needs of children with disabilities and provides federal funding to states. At the heart of the IDEA is the individualized education program (IEP). For each child eligible for special education services, public schools are required to develop and implement an individualized education plan in order to meet her unique special needs. An IEP details the current status of a child including academic performance and obstacles stemming from her disability as well as a special education plan including services, special accommodations and modifications to be provided, the schedule, and measurable annual goals and objectives (Drasgow, Yell, & Robinson, 2001). A child is eligible for special education services under the IDEA if her IEP team finds that she has one or more disabilities. Although ADHD alone does not constitute a distinct disability category, it is listed as a condition under the “other health impairment.”
One of the important decisions in an IEP development is where to place the child. The IEP team determines the educational environment based on the child's IEP – i.e. unique educational needs of the child (34 C.F.R. 300.116(b)(2)). Importantly, the federal law, Part B of the IDEA, requires that schools must pursue full inclusion of children with disabilities in regular classroom with their non-disabled peers by providing appropriate accommodations, modifications, and supplementary aids and services. If such attempts do not work, schools may place children in separate classrooms while ensuring the children are educated along with their non-disabled peers to the maximum extent appropriate. The least restrictive environment, along with the IEP, is an important principle of special education provision under the IDEA. Accordingly, the implementation of an IEP and its least restrictive environment provision is one basis of the federal funding allocation.
The least restrictive environment, inclusive special education, and remission from ADHD
Research suggests that for children with various types of disabilities inclusive special education has positive effects on academic achievement (Banerji & Dailey, 1995; Cosier, Causton-Theoharis, & Theoharis, 2013; Waldron & McLeskey, 1998), social functioning (Fisher & Meyer, 2002; Fryxell & Kennedy, 1995; Kennedy, Shukla, & Fryxell, 1997; Rea et al., 2002), affective gains (Banerji & Dailey, 1995), and behavioral outcomes (Rea et al., 2002). Whereas children in restrictive environments are self-contained in special education classrooms, those educated in inclusive environments can generalize principles learned from behavioral interventions to broader, more general academic and social settings as they interact with peers with no disabilities (Chronis et al., 2006), resulting in improved academic achievement, social functioning, and behavioral outcomes.
The interpretation of the least restrictive environment, parental involvement in special education provision, and the geographic variation in ADHD gradient
The least restrictive environment guideline is a guiding principle rather than a specific requirement. Because the least restrictive environment is open for interpretation, one would expect the degree of inclusive placement could vary across geographic areas. Empirical examinations of placement of children with disabilities found that inclusion varies widely across states (Danielson & Bellamy, 1989; McLeskey & Henry, 1999). Existing, taken-for-granted practices of educational communities drive placement decisions (Kurth & Mastergeorge, 2010).
Parents are another driver of placement decisions. Parents of children with disabilities play a significant role in writing and implementing IEPs and their cooperation with teachers is of great importance in the IDEA provision (Palley, 2004). Parents can influence the special education provision process in numerous ways: they can initiate an evaluation of their children's eligibility under the IDEA, influence the IEP eligibility decision, negotiate disability labels, and advocate for more inclusive educational environments for their children, and so forth.
Although all parents have the right to advocate for better educational environments for their children, not all parents are able to do so. For example, Lalvani (2012) found that high SES parents are more likely to be aware of inclusive education, successfully negotiate access to inclusive education, and expend time, effort, and resources to negotiate the IEP. As a result, the extent to which special education services meet the needs of students with ADHD is stratified by socioeconomic status such that low SES children with ADHD are more likely to have unmet needs than high SES counterparts (Bussing, Zima, Perwien, Belin, & Widawski, 1998) when inclusivity is not the default.
Therefore, we expect that high SES children's remission likelihood will be invariant across educational regimes. This is because, on the one hand, high SES parents educating their children in restrictive environments likely negotiate their children's placement and increase time spent in regular classrooms. On the other hand, even when their children are placed in self-contained classrooms, high SES parents can seek alternative treatment options outside the school. It is, however, unlikely that low SES parents negotiate placement or provide quality care outside the school. For low SES children, the institutional environment of special education regime can be critical.
Data and methods
We analyzed data from the National Survey of Children's Health (NSCH). The NSCH is a telephone survey designed to provide national and state-specific prevalence estimates for non-institutionalized children ages 0–17 on physical, emotional, and behavioral health indicators, as well as indicators of children's experiences with the health care system. Repeated cross-sectional data were collected in 2003–2004, 2007–2008, and 2011–2012. The total sample sizes in these respective years were 102,353, 91,642, and 95,677, with approximately 1800 surveys per state per year.
The outcome of interest is ADHD remission. Ideally, we would want to observe a child with ADHD over time and identify whether and when the child drops ADHD symptoms. However, because NSCH data is cross-sectional, we do not have repeated observations of same children. Instead, we exploited the survey design of the NSCH. In 2007–2008 and 2011–2012, the NSCH included two different questions about ADHD diagnostic status. The first question asks whether a surveyed child has ever been diagnosed with ADHD. For children who have been diagnosed, the second question asks if they still maintain diagnosis at the time of survey. Previous research has established that parental reports of ADHD diagnosis are extremely accurate and reliable measures of physician diagnosis with a sensitivity of 94 and a positive predictive power of 98 (Faraone, Biederman, & Milberger, 1995). We excluded 2003–2004 survey from analysis because the second question about the current diagnostic status was not asked. We further restricted our sample to 2007–2008 data because some state-level control variables are only available for 2007. Among respondents of 2007–2008 survey, we limited our analyses to children who have ever been diagnosed with ADHD and estimated the likelihood of losing diagnosis. We consider children who report having ever been—but not currently—diagnosed with ADHD as experiencing remission. Overall, 22 percent of our sample experienced remission. Among 17-year-olds, the remission rate was 70 percent. Prior research has found similar remission rate for adolescents. For instance, a recent study by Agnew-Blais JC and colleagues (2016) found roughly 75 percent of children with ADHD lose their diagnosis by adulthood.
Of central interest are the relationship between socioeconomic status, educational environment, and ADHD remission. The NSCH provides socioeconomic status (SES) information as a categorical variable. Eight SES categories were defined with respect to the federal poverty line (FPL): below 100 percent of FPL, above 100 percent to at or below 133 percent, above 133 percent to at or below 150 percent, above 150 percent to at or below 185 percent, above 185 percent to at or below 200 percent, above 200 percent to at or below 300 percent, above 300 percent to at or below 400 percent, and above 400 percent of FPL. Out of these eight categories, we aggregate six middle categories into one group. That is, we defined a family as low SES if its household income falls between 0 and 99 percent of the FPL, as high socioeconomic status if its income exceeds 400 percent of the FPL, and as middle socioeconomic status otherwise. We chose to aggregate the middle groups because our interest lies in examining comparing how low SES children respond to inclusive education and whether their reaction differs from high SES children's. To ensure that our choice of trichotomy does not affect the results, we ran additional analysis using eight categories for socioeconomic status as provided in the NSCH data and found that the results do not change. We report the results using three SES categories for conciseness.
As a potential source of variation in the likelihood of remission, we examine special education environments. To this end, we further restricted our analyses to school-aged children and adolescents. To measure special education environment, we used data available in the U.S. Department of Education's online data archive (U.S. Department of Education, 2010). The online archive provides information about special education provisions submitted annually by states to the Department of Education in compliance with Section 618 of the IDEA. To classify inclusive special education environments, we relied on the time children with disabilities spent in regular versus self-contained special education classrooms. States report the number of children belonging to each of the following three categories: inside regular classroom 80 percent or more of the day, inside regular classroom 40 percent to 79 percent of day, and inside regular classroom less than 40 percent of day. We included all fifty states and the District of Columbia in our analyses.
To collect information on potential state-level confounders, we relied on several external sources. First, to measure academic accountability policies, we borrowed Dee and Jacob's (2011) coding of accountability systems. Their coding scheme identifies 30 states that had their own accountability systems in place prior to the introduction of No Child Left Behind (NCLB) in 2002. Second, we account for state-level variation in bills and resolutions that prohibit teachers and school personnel from coercive labeling of children with mental disorders and recommending psychiatric treatment including psychotropic medication. This information came from AbleChild's website. We coded whether each state passed a bill or resolution prior to the introduction of a federal-level ban in 2004. Fourteen states instituted bans before the federal act. In addition, we included data on the percent of the population in a state with health insurance from the 2010 census. The number of psychiatrist per 1000 which was calculated with data from the American Medical Association.
Descriptive analyses
First, we describe ADHD prevalence among children with different socioeconomic backgrounds. To do so, we plotted the percent of children who were currently diagnosed with ADHD, stratified by socioeconomic status. Next, we examined ADHD remission rates by socioeconomic status and special education environment. We coded a state's special education environment as inclusive if children with disabilities spend considerable amount of time in general classrooms and little time in self-contained, separate classrooms. Specifically, we measured the proportion of children spending less than 40 percent of the day in general classroom and reverse-coded the proportion to denote inclusiveness. The Department of Education provides breakdown of time spending data by thirteen disability categories. Children with ADHD are eligible for special education service under the “other health impairment” category. However, we aggregated information across all the disability categories. This is because of the high rate of co-morbidities of ADHD with other disabilities. In fact, two thirds of students in the “other health impairment” category had ADHD as did almost 60 percent of children in the emotional disturbance category, one fifth of students in intellectual disability category, and four percent of students in the specific learning disability category (Schnoes, Reid, Wagner, & Marder, 2006). Because children with ADHD are likely to receive care under other categories due to co-morbidities, we used the overall placement pattern as an indicator of a given state's general stance toward inclusive special education. We log-transformed “inclusive special education environment” because of skewness and mean-centered to facilitate interpretation. For plotting, we categorized states into three groups based on the extent to which their special education is inclusive. Top third states (0.20 ≤ and ≤ 1.27) were coded as the “most inclusive” and the bottom third states (−0.90 ≤ and < −0.176) as the “least inclusive.”
Logistic regression models
To examine whether special education environments are associated with the likelihood of ADHD remission, we estimated logistic regressions for school-aged children and adolescents. Our aim in this analysis is to examine whether low and high SES children's remission rates are associated with special education environments after controlling for confounders.
The dependent variable, “remission from ADHD,” is an indicator variable that takes one if a surveyed child, who had been diagnosed with ADHD, no longer has ADHD at the point of survey. Our independent variables of interest are the inclusiveness of a state's special education and child's SES. To examine whether special education environments are more or less important for children from less advantaged backgrounds, we include an interaction between individual SES and state special education environment.
We included several individual-level covariates that are expected to correlate with special education environment, SES, and remission of children with different SES. First, we included demographic variables such as age, sex, and race as control variables in all models. Research has been documented that remission rate increases with age (Biederman, Mick, & Faraone, 2000). We included an indicator variable for sex and a categorical variable of race because different groups might have varying levels of access to treatment and adherence to treatment. Female and white were reference groups. Second, we controlled for insurance type because high SES children are more likely to have insurance with better coverage, which in turn, increases the odds of remission. There were three types of insurance in the NSCH data: private, public, and not-insured. Privately insured is the reference category. Third, family structure was included because of its potential association with children's educational outcomes. Living with two biological parents was the reference category. Fourth, we controlled for type of school because high SES children are more likely to attend private schools and public and private schools provide different services and contexts for children with ADHD. Four types of school were used: attending private school, attending public school, home-schooled, and not enrolled. Attending public school was the reference category. Last, co-morbidity was included in the analysis as a proxy for a child's severity of behavioral disorder. To control for co-morbidity, we included indicator variables that for each of the following mental and behavioral disorders: depression, anxiety problems, behavioral or conduct problems, autism spectrum disorders, developmental delay, speech problems, and learning disability. The indicator variables were coded as one if a child has been diagnosed with the respective disorder.
In addition, we controlled for potential state-level confounders. First, we included the NCLB treatment as a control variable. The NCLB treatment is an indicator variable and was coded as one if a state had no accountability system prior to the NCLB and hence, the NCLB was a “treatment” to the state's education regime. When accountability pressure is recently introduced, teachers and school personnel might want to keep distracted children in self-contained environments to increase the academic performance of “regular” students (Cawelti, 2006). Such tendency will affect both the inclusiveness of special education and remission rates. Second, we controlled for the psychiatric service recommendation ban. This is an indicator variable and was coded as one if a state had had any prohibition bill or registration against teachers' and school personnel's recommendation of psychiatric diagnosis, treatment, or medication before the federal ban was introduced in 2004. When school personnel's or teachers' recommendation is permitted, they might do so to parents in order to manage classrooms more easily and improve the academic performance of children. States that had prohibited treatment recommendations before the federal ban are likely to have been favoring the use of behavioral treatment and accommodations for children with special needs, and therefore, may already have narrowed the remission gap between low and high SES children. Third, we controlled for several potential confounders that can affect low SES children's access to treatment. These variables include the proportion of insured children, the number of psychiatrist per 100,000 children, and income per capita (i.e., overall resourcefulness of the state).
To examine the relationship between remission rates, SES and special education regimes, we ran three sets of analyses to ensure our findings are robust to modeling choices. We first ran a set of logistic regressions stratified by SES. In the stratified models, our goal is to determine whether the association between the odds of remission and inclusive special education are different among high and low SES samples. Next, to ensure the same pattern holds with the complete sample, we ran a logistic regression model using cases across all SES levels and added interaction terms between SES and inclusive special education. The goal of this analysis is to test whether the odds ratio of the interaction term between inclusive education and low SES category is significantly greater than one, which would suggest that the odds of low SES children's remission increase at a faster rate as a function of inclusive education than those of high SES children's. In both stratified and interaction models, we clustered standard errors by states because our independent variable as well as some s control variables are state-level covariates. Finally, we ran a random-intercept multilevel logistic regression to account for the facts that children are nested in states. In estimating the interaction effect between an individual-level and a state-level covariate – in our case, the interaction between low SES and inclusive education –, multilevel modeling accounts for the fact that children are nested in states and therefore, error terms are likely correlated as such. In the interaction and multilevel models, we use high SES as the reference category.
Results
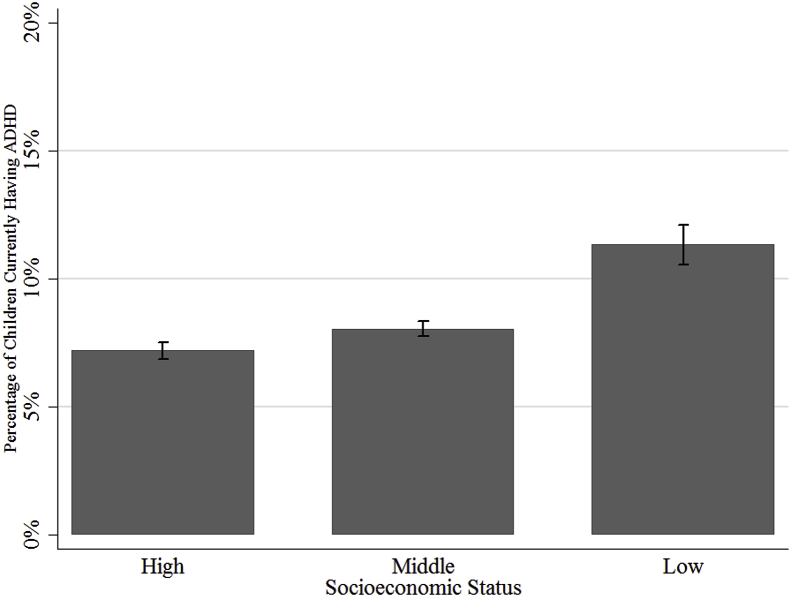
To explore whether ADHD gradient exists, we first plotted the percent of children with ADHD by SES group. In 2007–2008 survey, 8 percent of children were reported to currently have ADHD. Fig. 1 indicates that higher fraction of low SES children has ADHD than their more advantaged peers. Of families with household income below the federal poverty line (low SES families), 11.33 percent reported that their children currently have ADHD whereas 7.19 percent of families with household income above 400 percent of the federal poverty line (high SES families) reported that their children have the diagnosis. This difference in ADHD prevalence between high and low SES groups was statistically significant (t = 10.98, p < 0.001), suggesting that the overall gradient in ADHD prevalence be negative.
Fig. 1.
Percent of school-aged children currently having ADHD by socioeconomic status.
Note: Authors' calculation based on data from the National Survey of Children's Health, 2007–2008.
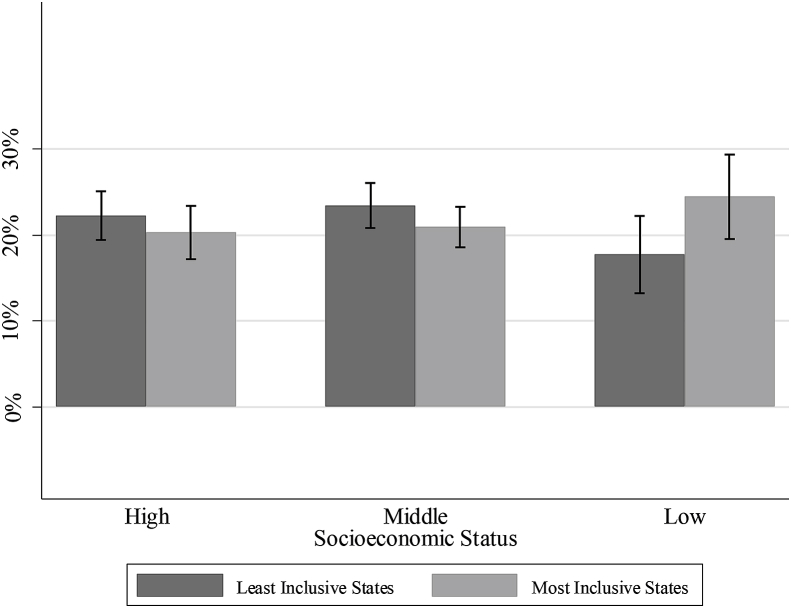
Next, we plotted remission rates of high and low SES children by special education regime. Fig. 2 shows that low SES children's remission rates are higher in most inclusive states than in least inclusive states. Although the confidence intervals for the inclusive and restrictive states overlap, a t-test with independent samples revealed that the group means for the two group were significantly different form each other (t = 1.97, p < 0.05). In contrast, high SES children's remission rates did not significantly differ in more and less inclusive states (t = −0.92, p = 0.179).
Fig. 2.
Percent of school-aged children remitted from ADHD by socioeconomic status and special education environment.
Note: Authors' calculation based on data from National Survey of Children's Health, 2007–2008. Based on the inclusiveness of special education, we labeled top third of states as most inclusive states. Bottom third of states was coded as least inclusive states. High SES children's remission rates in least and most inclusive states are not statistically different (t = −0.92, p = 0.179). Low SES children's remission rate is higher in inclusive states than in restrictive states (t = 1.97, p < 0.05).
Finally, to ensure that the relationship between remission, SES, and special education environment holds after controlling for potential confounders, we turned to regression models. Table 1 summarizes descriptive statistics of variables used in statistical analysis. The overall remission rate was 22 percent. For the purpose of easier interpretation of effect sizes, we standardized inclusive education. To put the standardized measure into perspective, mean inclusive education indicates that special-education children in those states spend roughly 11 percent of their time at school in self-contained classrooms. One-standard deviation above the mean translates into roughly 8 percent of time in self-contained environments, and one-standard deviation below the mean stands for roughly 18 percent of time in such restrictive settings.
Table 1.
Descriptive statistics.
| Individual-level variables | Obs. | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|
| Remission | 5967 | 0.220 | |||
| Socioeconomic status | |||||
| High | 5967 | 0.348 | |||
| Middle | 5967 | 0.507 | |||
| Low | 5967 | 0.144 | |||
| Age | 5967 | 12.719 | 3.185 | 6 | 17 |
| Sex | |||||
| Female | 5967 | 0.290 | |||
| Male | 5967 | 0.710 | |||
| Race | |||||
| White | 5967 | 0.732 | |||
| Black | 5967 | 0.103 | |||
| Multiracial | 5967 | 0.080 | |||
| Other | 5967 | 0.085 | |||
| Insurance | |||||
| Private | 5967 | 0.631 | |||
| Public | 5967 | 0.313 | |||
| Non (Cash) | 5967 | 0.056 | |||
| Family structure | |||||
| Two parent--biological or adopted | 5967 | 0.515 | |||
| Two parent--step family | 5967 | 0.144 | |||
| Single mother--no father present | 5967 | 0.237 | |||
| Other family type | 5967 | 0.103 | |||
| School | |||||
| Public | 5967 | 0.866 | |||
| Private | 5967 | 0.109 | |||
| Home-schooled | 5967 | 0.022 | |||
| Not-enrolled | 5967 | 0.003 | |||
| Comorbidity | |||||
| Depression | 5967 | 0.216 | |||
| Anxiety | 5967 | 0.257 | |||
| Behavioral disorder | 5967 | 0.273 | |||
| Autism | 5967 | 0.082 | |||
| Developmental problem | 5967 | 0.214 | |||
| Speech disorder | 5967 | 0.132 | |||
| Tourette syndrome |
5967 |
0.020 |
|||
|
State-level variables |
Obs. |
Mean |
Std. Dev. |
Min |
Max |
| Inclusive education (standardized) | 5967 | 0.000 | 1.000 | −2.141 | 2.903 |
| State-prohibition of drug recommendation | 5967 | 0.272 | |||
| NCLB as a treatment | 5967 | 0.389 | |||
| IDEA determination (Does not need intervention) | 5967 | 0.218 | |||
| Proportion insured | 5967 | 0.862 | 0.039 | 0.749 | 0.945 |
| Psychiatrist per 10,000 children | 5967 | 1.757 | 1.299 | 0.696 | 9.817 |
| Income per capita | 5967 | 0.123 | 0.144 | 0.008 | 0.711 |
We employed three sets of logistic regressions: 1) stratified models, 2) an interaction model, and 3) a random-intercept multilevel model. Models 1 and 2 of Table 2 shows that among high and middle class children, there are no significant differences in remission rates across special education regimes. In contrast, Model 3 suggests that the remission rate of low SES children of inclusive states is on average by 1.3 times higher than that of restrictive states (OR: 1.259, p < 0.01).
Table 2.
Factors associated with the odds of remission from ADHD among school-aged children.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
Model 5 |
|
|---|---|---|---|---|---|
| Stratified: High SES |
Stratified: Middle SES |
Stratified: Low SES |
Interaction | Random-intercept Multi-level |
|
| Inclusive education (Standardized) | 0.989 | 0.959 | 1.259** | 0.969 | 0.965 |
| (0.871) | (0.463) | (0.006) | (0.631) | (0.572) | |
| Poverty level: 3 Categories (Ref: Above 400%) | |||||
| Middle SES (Above 100% to at or below 400%) | 1.138 | 1.139 | |||
| (0.065) | (0.090) | ||||
| Low SES (At or below 100% poverty level) | 1.168 | 1.175 | |||
| (0.270) | (0.202) | ||||
| Middle SES X Inclusive education | 0.995 | 1.001 | |||
| (0.929) | (0.987) | ||||
| High SES X Inclusive education | 1.294** | 1.290* | |||
| (0.006) |
(0.016) |
||||
| N | 2078 | 3028 | 861 | 5967 | 5967 |
| Clustered SE | State | State | State | State | No |
Note: To measure the inclusiveness of states' education environments, we used each state's proportion of students educated in regular classroom less than 40 percent of their time. We reverse coded the proportions to denote inclusiveness and mean-centered them for easier interpretation. Families with income between 100% and 400% of the Federal Poverty Line (FPL) were coded as Middle SES. Families with income below 100% of the FPL were coded as low SES. High SES (>400% of the FPL) was omitted. For all models, we included the following individual-level control variables: age, sex, race, insurance, family structure, school, and co-morbidity. We also controlled for state-level covariates: state treatment recommendation ban prior to the federal ban, No Child Left Behind (NCLB) as treatment, proportion of the insured, psychiatrist per 10,000, and income per capita. Exponentiated coefficients are reported; p-values in parentheses. In Models 1, 2, 3, and 4, standard errors are clustered by state.
Exponentiated coefficients; p-values in parentheses.
*p < 0.05 **p < 0.01 ***p < 0.001.
We find the same pattern in a logistic regression model with interaction effects. Model 4 of Table 2 indicates that the effect of inclusive special education on remission rate is much larger among low SES children than among high SES children (OR: 1.294, p < 0.01). Fig. 3 plots the interaction effects between SES and special education regime. Low SES children are more likely to experience remission when educated in more inclusive environments whereas high SES children's remission rate is relatively invariant across special education environments. In the range of the least and most inclusive states, the remission rate increased from 22 percent to 20 percent, and the difference was insignificant statistically. The effect size of inclusive environment for low SES children is large – holding other variables at means, the remission rate of low SES children is estimated to larger by two-fold in more inclusive states (defined as two-standard deviation above the mean) than that in less inclusive states (defined as two-standard deviation below the mean). In other words, low SES children's remission probability in more inclusive state is estimated to be 32 percent while that in less inclusive state is 16 percent. Thus, inclusive educational environments appear to be particularly beneficial to disadvantaged children. Finally, we ran a random-intercept multilevel logistic regression model to confirm that our results hold even after we account for the fact that children are nested in states. When we compare Model 4 and Model 5, the odds ratios of the interaction term between low SES and inclusive education environment are very similar although the multilevel model has a wider confidence interval (Model 4 – OR: 1.294, p < 0.01; Model 5 – OR: 1.290, p < 0.05). In sum, inclusive special education environments facilitate low SES children's remission whereas high SES children do not respond to state-level variation in special education regimes.
Fig. 3.
Odds of remission by special education environment, stratified by socioeconomic status.
Note: Marginal effects from Model 4 shown in Table 1. Middle socioeconomic status was omitted for visualization. Note that inclusive education was standardized (M = 0.000; SD = 0.999).
Discussion
Special education environments are associated with differential remission rates among more and less advantaged children. While high SES children do not respond significantly to special education environments, low SES children educated in inclusive settings have a better prognosis than their peers in restrictive environments. This suggests that schools may be particularly important in ameliorating disparities in childhood behavioral disorders.
Our study has several limitations. First, we rely on cross-sectional data on ADHD remission at the individual level in conjunction with educational environment data at the state level. Ideally, we would use repeated observations of same individuals over time and trace their ADHD diagnosis and remission as well as their placement in special education environments, rather than relying on reported changes in diagnosis. The cross-sectional nature of the NSCH data and our measure of special education environments at the state level limit our ability to identify clear causal relationship. With longitudinal observations on children's mental health in combination with their placement data, one could make stronger causal claim about the relationship among differences in the utilization of special education services by families with different socioeconomic background, remission from ADHD, and geographic variation in gradient. However, using data at the state level helps assuage some potential selection concerns. If our analysis examined whether or not an individual child was placed in a more or less restrictive environment, we worry that the characteristics determining placement would be associated with the likelihood of remission. While using state level data on restrictiveness has limitations, it helps us overcome individual selection issues.
Second, our measure of special education environment might be capturing other factors. We interpreted the proportion of students in restrictive placements in a given state as a measure of access to better special education services. Alternatively, our measure could indicate overall quality of special education in the region – i.e. the financial and human resource availability of schools in a state to provide special service, accommodations, and modifications that would cater special needs of children with disability. We attempt to address this issue by controlling for the Individuals with Disabilities Education Act (IDEA) determination. Released by the U.S. Department of Education's Office of Special Education and Rehabilitative Services, the IDEA determination assesses each state's special education performance. We used the IDEA determination of 2006 (U.S. Department of Education, 2007) and created an indicator variable of whether a state met the requirements of the statue. Even after the IDEA determination was included in the models, the effect of inclusive education environment on low SES children's remission was positive and significant (results available upon request). This suggests that inclusive education has a direct relationship with the remission rate among low SES children net of its indirect influence on the remission rate through the effectiveness of overall special education provision. In addition to this analytic strategy, interpreting our measure of inclusive environment as overall quality of special education cannot explain the empirical pattern of geographic variability by SES. That is, if inclusive education environment translates to higher levels of resources availability and capacity to provide special education services, we would expect to see higher remission rates among all children in inclusive states compared to their peers in more restrictive states. The quality-of-service-provision intervention alone cannot explain the unequal remission rates between low and high SES children in states with more and less inclusive special education practices.
Third, it is also possible that children from more advantaged backgrounds would prefer to maintain their diagnosis in order to access medication and other benefits afforded by a diagnosis. If this were the case, we would expect them to have lower remission rates in general. While we do not observe this, their invariant response to educational environments is consistent with this explanation. While our study focuses on the benefits of more inclusive environments for lower SES children, further work should examine why these benefits do not accrue to higher SES children.
Finally, it may be important to note that ADHD can be mis-diagnosed and that individual or environmental characteristics, such as SES, can drive over- or under-diagnosis (Bruchmüller, Margraf, & Schneider, 2012; Morley, 2010; Reyes, Baumgardner, Simmons, & Buckingham, 2013).1 In this regard, one might be concerned that misdiagnosis may confound our results. That is, low SES children that do not actually meet the diagnostic criteria are more likely to be mis-diagnosed with ADHD in inclusive states than in restrictive states (i.e., false positives), and their higher remission rates in inclusive states may result from the mis-categorization of low SES children whose behavior only mildly resembles the symptoms of ADHD. In other words, low SES children diagnosed with ADHD in inclusive states are easier to “fix” than those in restrictive states.
Unfortunately, our data do not include information regarding children's symptoms and their diagnostic processes. We, however, believe that inclusive education would not be associated with over-diagnosis of low SES children. First, healthcare professionals, working outside education systems, have no reason to be more biased in inclusive states to produce false positive diagnoses. Second, nether inclusive nor restrictive regimes have an incentive to push low-SES children for diagnosis. If anything, the reason for schools and education systems to push for diagnosis would be for the ease and effectiveness of classroom management. Such a tendency toward effective classroom management is likely high when the academic pressure is present. To address this concern, in our statistical models, we controlled for the presence of academic pressure at the state level, by including an indicator variable that denotes whether No Child Left Behind policy increased pressure for academic accountability for the given state around 2007. Our results show that even after controlling for the presence of academic pressure, inclusive states had higher remission odds of low SES children.
Furthermore, for inclusive states, ease of classroom management wouldn't be an incentive to push low SES children's diagnosis at all. Recall that inclusive regimes will place children with disabilities in regular classrooms to the maximal extent. Given that children most vulnerable to over-diagnosis would have only mild behavioral problems, they will likely remain in regular classrooms with their peers even if they obtain ADHD diagnosis. At the other extreme is restrictive states. We contend that the primary reason that restrictive regimes place special education students in self-contained classrooms is the lack of resources. Note that education systems are evaluated by the federal agency, and federal funding is allocated according to the evaluation. One important evaluation criterion is the degree of inclusiveness of special education provision. Therefore, a concern for losing federal funding likely counteract the incentive to push for ADHD diagnosis even if the separation of special education children from regular students may make it easier to manage classrooms. That is, for restrictive states, a concern of losing federal funding likely triumphs a desire for ease of classroom management.
This article makes three contributions. First, to our knowledge our study is the first to link ADHD remission and schooling. Estimates of remission (Agnew-Blais JC et al., 2016; Biederman et al., 2011; Biederman et al., 2012; Faraone et al., 2006; Kessler et al., 2005) as well as studies of behavioral interventions in schools exist (Banerji & Dailey, 1995; Fryxell & Kennedy, 1995; Kennedy et al., 1997; Rea et al., 2002; Waldron & McLeskey, 1998). However, little attention has been drawn to the context in which treatment and intervention are delivered. We highlighted special education environments as an important context in which behavioral treatments takes place. The significance of schooling in treatment of mental health and behavioral disorders is paramount because children and adolescents spend the majority of time at school or doing school-related activities and tasks. Second, our findings contribute to the fundamental cause tradition by empirically examining how an institutional environment can interact with individual's socioeconomic status to produce gradients in a health outcome. Finally, our study sheds light on a potential implication of special education regimes in the reproduction of social inequality. Schools are of critical importance in reducing disparities in access to treatment because other treatment modalities, such as medication, psychiatric treatment, and family-based interventions, are stratified by socioeconomic status. In our study, higher SES children are invariant in their response to educational environment suggesting they may have access to treatment outside of the school system. Institutional environments, on the other hand, impact low SES children's prognosis, increasing or decreasing disparities in health. Our study suggests that inclusive special education environments may help reduce mental health disparities among children and adolescents. Health gradients in children's health can reproduce, if not amplify, social stratification because they affect other important outcomes such as educational attainment, occupational choice, and income. Therefore, it is important to ensure that our institutions provide adequate social arrangements from which children with little family resources can receive otherwise unavailable care and services.
Ethical approval
The study is exempt because it uses publicly available deidentified data.
Funding
The authors declare that they have no relevant or material financial interests that relate to the research described in this paper.
Footnotes
Our empirical analyses focus on children who have been diagnosed with ADHD and on how SES is associated with their remission. However, it is important to note that getting a diagnosis in the first place is also likely shaped by sociocultural factors such as SES. Researchers argue that ADHD is often mis-diagnosed and that certain populations are more prone to over- or under-diagnosis (Morley, 2010). For example, ADHD diagnosis more prevalent among boys than girls (Bruchmüller et al., 2012). Prevalence rate also differs along racial and socioeconomic lines (Baumgardner et al., 2010; Reyes et al., 2013). One can think of various factors that may lead to differential diagnosis rate between low- and high- SES children. First, fundamental cause theory posits that low SES family have less resources that high SES ones (Link & Phelan, 1995). Low SES parents might be unable to spend time with their children as much as higher-SES parents. Low SES parents are likely unfamiliar with prevalence, symptoms, and consequences of ADHD. Both the lack of facetime with children and that of information about the disorder make low SES parents ill-equipped to notice behavioral problems of their children. Even if they note some problematic behavior, low SES parents could find it difficult to time and economic resources (i.e., insurance) to seek a diagnosis. Furthermore, even if they decide to bring their children to diagnosticians, they might be unable to adequately deliver their children's problem behavior. All these factors likely lead to underdiagnosis of ADHD among low SES children. On the other hand, there are a couple of reasons that ADHD in low SES population may be over-diagnosed. Healthcare providers might produce false positive diagnoses for low SES children when they do not adhere to the diagnostic guideline and instead rely on stereotype-based judgment (Bruchmüller et al., 2012; Manos, Giuliano, & Geyer, 2017). Teachers can also contribute to the over-diagnosis of low SES children because they might consider low SES children's classroom behavior as problematic and suggest getting a diagnosis to low SES parents. High-SES children, too, are subject to misdiagnosis. High SES parents can drive underdiagnosis if they are wary of stigma associated with the diagnostic label, and as a result, do want their children to obtain a diagnosis. On the other hand, high SES parents might have a motivation to pursue a diagnosis if they want to boost the academic performance of their children by having their children on stimulants. High SES parents' driving over-diagnosis appears to be plausible given the evidence that false positive rate is higher among high SES children than low SES children (Morley, 2010) and that high SES children's medication cycle is closely coupled with academic calendar (King et al., 2014).
References
- deBettencourt L.U. Understanding the differences between IDEA and section 504. Teaching Exceptional Children. 2002;34:16–23. [Google Scholar]
- Agnew-Blais J.C., Polanczyk G.V., Danese A., Wertz J., Moffitt T.E., Arseneault L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry. 2016 doi: 10.1001/jamapsychiatry.2016.0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Association; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. [Google Scholar]
- Arnold L.E., Hodgkins P., Kahle J., Madhoo M., Kewley G. Long-term outcomes of ADHD academic achievement and performance. Journal of Attention Disorders. 2015 doi: 10.1177/1087054714566076. 1087054714566076. [DOI] [PubMed] [Google Scholar]
- Banerji M., Dailey R.A. A study of the effects of an inclusion model on students with specific learning disabilities. Journal of Learning Disabilities. 1995;28:511–522. doi: 10.1177/002221949502800806. [DOI] [PubMed] [Google Scholar]
- Baumgardner D., Schreiber A.L., Havlena J.A., Bridgewater F.D., Steber D.L., Lemke M.A. Geographic analysis of diagnosis of attention deficit/hyperactivity disorder in children: Eastern Wisconsin, USA. The International Journal of Psychiatry in Medicine. 2010;40(4):363–382. doi: 10.2190/PM.40.4.a. [DOI] [PubMed] [Google Scholar]
- Biederman J., Mick E., Faraone S.V. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. The Australian Journal of Pharmacy. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- Biederman J., Petty C.R., Clarke A., Lomedico A., Faraone S.V. Predictors of persistent ADHD: An 11-year follow-up study. Journal of Psychiatric Research. 2011;45:150–155. doi: 10.1016/j.jpsychires.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J., Petty C.R., O'Connor K.B., Hyder L.L., Faraone S.V. Predictors of persistence in girls with attention deficit hyperactivity disorder: Results from an 11-year controlled follow-up study. Acta Psychiatrica Scandinavica. 2012;125(2):147–156. doi: 10.1111/j.1600-0447.2011.01797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg S.J., Bramlett M.D., Kogan M.D., Schieve L.A., Jones J.R., Lu M.C. Changes in prevalence of parent-reported autism spectrum disorder in school-aged US children: 2007 to 2011–2012. National health statistics reports. 2013;65(20):1–7. [PubMed] [Google Scholar]
- Brown R.T., Borden K.A., Wynne M.E., Spunt A.L., Clingerman S.R. Compliance with pharmacological and cognitive treatments for attention deficit disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 1987;26:521–526. doi: 10.1097/00004583-198707000-00010. [DOI] [PubMed] [Google Scholar]
- Bruchmüller K., Margraf J., Schneider S. Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. Journal of Consulting and Clinical Psychology. 2012;80(1):128. doi: 10.1037/a0026582. [DOI] [PubMed] [Google Scholar]
- Bussing R., Zima B.T., Perwien A.R., Belin T.R., Widawski M. Children in special education programs: Attention deficit hyperactivity disorder, use of services, and unmet needs. American Journal of Public Health. 1998;88:880–886. doi: 10.2105/ajph.88.6.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawelti G. The side effects of NCLB. Educational Leadership. 2006;64(3):64–68. [Google Scholar]
- Chang V.W., Lauderdale D.S. Fundamental cause theory, technological innovation, and health disparities: The case of cholesterol in the era of statins. Journal of Health and Social Behavior. 2009;50:245–260. doi: 10.1177/002214650905000301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung C.H.M., Rijdijk F., McLoughlin G., Faraone S.V., Asherson P., Kuntsi J. Childhood predictors of adolescent and young adult outcome in ADHD. Journal of Psychiatric Research. 2015;62:92–100. doi: 10.1016/j.jpsychires.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung C.H.M., Rijsdijk F., McLoughlin G., Brandeis D., Banaschewski T., Asherson P. Cognitive and neurophysiological markers of ADHD persistence and remission. The British Journal of Psychiatry. 2016;208(6):548–555. doi: 10.1192/bjp.bp.114.145185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis A.M., Jones H.A., Raggi V.L. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clinical Psychology Review. Attention Deficit Hyperactivity Disorder From A Neurosciences And Behavioral Approach. 2006;26:486–502. doi: 10.1016/j.cpr.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Cosier M., Causton-Theoharis J., Theoharis G. Does access matter? Time in general education and achievement for students with disabilities. Remedial and Special Education. 2013;34:323–332. [Google Scholar]
- Craig S.G., Davies G., Schibuk L., Weiss M.D., Hechtman L. Long-term effects of stimulant treatment for ADHD: What can we tell our patients? Current Development Disorders Reports. 2015;2:1. [Google Scholar]
- Cutler D.M., Lleras-Muney A. National Bureau of Economic Research; 2012. Education and health: Insights from international comparisons (working paper No. 17738) [Google Scholar]
- Danielson L.C., Bellamy G.T. State variation in placement of children with handicaps in segregated environments. Exceptional Children. 1989;55:448–455. [Google Scholar]
- De Clercq B., Pfoertner T.-K., Elgar F.J., Hublet A., Maes L. Social capital and adolescent smoking in schools and communities: A cross-classified multilevel analysis. Social Science & Medicine. 2014;119:81–87. doi: 10.1016/j.socscimed.2014.08.018. [DOI] [PubMed] [Google Scholar]
- Dee T.S., Jacob B. The impact of no Child Left behind on student achievement. Journal of Policy Analysis and Management. 2011;30:418–446. [Google Scholar]
- Drasgow E., Yell M.L., Robinson T.R. Developing legally correct and educationally appropriate IEPs. Remedial and Special Education. 2001;22:359–373. [Google Scholar]
- Dufur M.J., Parcel T.L., Mckune B.A. Capital and context: Using social capital at home and at school to predict child social adjustment. Journal of Health and Social Behavior. 2008;49:146–161. doi: 10.1177/002214650804900203. [DOI] [PubMed] [Google Scholar]
- Elovainio M., Pietikäinen M., Luopa P., Kivimäki M., Ferrie J.E., Jokela J. Organizational justice at school and its associations with pupils' psychosocial school environment, health, and wellbeing. Social Science & Medicine. 2011;73:1675–1682. doi: 10.1016/j.socscimed.2011.09.025. [DOI] [PubMed] [Google Scholar]
- Faraone S.V., Biederman J., Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine null. 2006:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone S.V., Biederman J., Milberger S. How reliable are maternal reports of their children's psychopathology? One-year recall of psychiatric diagnoses of ADHD children. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:1001–1008. doi: 10.1097/00004583-199508000-00009. [DOI] [PubMed] [Google Scholar]
- Firestone P. Factors associated with children's adherence to stimulant medication. American Journal of Orthopsychiatry. 1982;52:447–457. doi: 10.1111/j.1939-0025.1982.tb01431.x. [DOI] [PubMed] [Google Scholar]
- Firestone P., Witt J.E. Characteristics of families completing and prematurely discontinuing a behavioral parent-training program. Journal of Pediatric Psychology. 1982;7:209–222. doi: 10.1093/jpepsy/7.2.209. [DOI] [PubMed] [Google Scholar]
- Fisher M., Meyer L.H. Development and social competence after two years for students enrolled in inclusive and self-contained educational programs. Research and Practice for Persons with Severe Disabilities. 2002;27:165–174. [Google Scholar]
- Freese J., Lutfey K. Fundamental causality: Challenges of an animating concept for medical sociology. In: Pescosolido B.A., Martin J.K., McLeod J.D., Rogers A., editors. Handbook of the sociology of health, illness, and healing. Springer New York; New York, NY): 2011. pp. 67–81. [Google Scholar]
- Fryxell D., Kennedy C.H. Placement along the continuum of services and its impact on students' social relationships. Research and Practice for Persons with Severe Disabilities. 1995;20:259–269. [Google Scholar]
- Hinshaw S.P., Scheffler R.M. Oxford University Press; 2014. The ADHD explosion: Myths, medication, money, and today's push for performance. [Google Scholar]
- Kennedy C.H., Shukla S., Fryxell D. Comparing the effects of educational placement on the social relationships of intermediate school students with severe disabilities. Exceptional Children. 1997;64:31–47. [Google Scholar]
- Kessler R.C., Adler L.A., Barkley R., Biederman J., Conners C.K., Faraone S.V. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: Results from the national comorbidity survey replication. Biological Psychiatry. 2005;57:1442–1451. doi: 10.1016/j.biopsych.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M.D., Bearman P.S. Socioeconomic status and the increased prevalence of autism in California. American Sociological Review. 2011;76:320–346. doi: 10.1177/0003122411399389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M.D., Jennings J., Fletcher J.M. Medical adaptation to academic pressure: Schooling, stimulant use, and socioeconomic status. American Sociological Review. 2014;79:1039–1066. [Google Scholar]
- Kurth J., Mastergeorge A.M. Impact of setting and instructional context for adolescents with autism. The Journal of Special Education. 2010 [Google Scholar]
- Lalvani P. Parents' participation in special education in the context of implicit educational ideologies and socioeconomic status. Education and Training in Autism and Developmental Disabilities. 2012;47:474–486. [Google Scholar]
- Link B.G., Northridge M.E., Phelan J.C., Ganz M.L. Social epidemiology and the fundamental cause concept: On the structuring of effective cancer screens by socioeconomic status. The Milbank Quarterly. 1998;76:375–402. doi: 10.1111/1468-0009.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Loe I.M., Feldman H.M. Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology. 2007;32(6):643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- Manos M.J., Giuliano K., Geyer E. ADHD: Overdiagnosed and overtreated, or misdiagnosed and mistreated? Cleveland Clinic Journal of Medicine. 2017;84(11):873. doi: 10.3949/ccjm.84a.15051. [DOI] [PubMed] [Google Scholar]
- Martin M.A., Frisco M.L., Nau C., Burnett K. Social stratification and adolescent overweight in the United States: How income and educational resources matter across families and schools. Social Science & Medicine, Part Special Issue: Men, Masculinities and Suicidal Behaviour. 2012;74:597–606. doi: 10.1016/j.socscimed.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeskey J., Henry D. Inclusion: What progress is being made across states? Teaching Exceptional Children. 1999;31:56–62. [Google Scholar]
- McMahon R.J., Forehand R., Griest D.L., Wells K.C. Who drops out of treatment during parent behavioral training. Behavioral Counseling Quarterly. 1981;1:79–85. [Google Scholar]
- Michelini G., Kitsune G.L., Cheung C.H.M., Brandeis D., Banaschewski T., Asherson P. Attention-Deficit/hyperactivity disorder remission is linked to better neurophysiological error detection and attention-vigilance processes. Biological Psychiatry. 2016;80(12):923–932. doi: 10.1016/j.biopsych.2016.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller D.P. Associations between the home and school environments and child body mass index. Social Science & Medicine. 2011;72:677–684. doi: 10.1016/j.socscimed.2010.12.003. [DOI] [PubMed] [Google Scholar]
- Moen P., Kelly E.L., Tranby E., Huang Q. Changing work, changing health: Can real work-time flexibility promote health behaviors and well-being? Journal of Health and Social Behavior. 2011;52:404–429. doi: 10.1177/0022146511418979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley C.P. Disparities in ADHD assessment, diagnosis, and treatment. The International Journal of Psychiatry in Medicine. 2010;40(4):383–389. doi: 10.2190/PM.40.4.b. [DOI] [PubMed] [Google Scholar]
- Mueller A.S., Pearson J., Muller C., Frank K., Turner A. Sizing up peers adolescent girls' weight control and social comparison in the school context. Journal of Health and Social Behavior. 2010;51:64–78. doi: 10.1177/0022146509361191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen L., Koushede V., Vinther-Larsen M., Bendtsen P., Ersbøll A.K., Due P. Does school social capital modify socioeconomic inequality in mental health? A multi-level analysis in Danish schools. Social Science & Medicine. 2015;140:35–43. doi: 10.1016/j.socscimed.2015.07.002. [DOI] [PubMed] [Google Scholar]
- Oberle E., Schonert-Reichl K.A. Stress contagion in the classroom? The link between classroom teacher burnout and morning cortisol in elementary school students. Social Science & Medicine. 2016;159:30–37. doi: 10.1016/j.socscimed.2016.04.031. [DOI] [PubMed] [Google Scholar]
- Palley E. Balancing student mental health needs and discipline: A case study of the implementation of the individuals with disabilities education Act. Social Service Review. 2004;78:243–266. [Google Scholar]
- Pavic Simetin I., Kern J., Kuzman M., Pförtner T.-K. Inequalities in Croatian pupils' risk behaviors associated to socioeconomic environment at school and area level: A multilevel approach. Social Science & Medicine. 2013;98:154–161. doi: 10.1016/j.socscimed.2013.09.021. [DOI] [PubMed] [Google Scholar]
- Rea P.J., McLaughlin V.L., Walther-Thomas C. Outcomes for students with learning disabilities in inclusive and pullout programs. Exceptional Children. 2002;68:203–222. [Google Scholar]
- Reyes N., Baumgardner D.J., Simmons D.H., Buckingham W. The potential for sociocultural factors in the diagnosis of ADHD in children. Wisconsin Medical Journal. 2013;112(1):13–17. [PubMed] [Google Scholar]
- Rieppi R., Greenhill L.L., Ford R.E., Chuang S., Wu M., Davies M. Socioeconomic status as a moderator of ADHD treatment outcomes. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(3):269–277. doi: 10.1097/00004583-200203000-00006. [DOI] [PubMed] [Google Scholar]
- Russell A.E., Ford T., Williams R., Russell G. The association between socioeconomic disadvantage and attention deficit/hyperactivity disorder (ADHD): A systematic review. Child Psychiatry and Human Development. 2015:1–19. doi: 10.1007/s10578-015-0578-3. [DOI] [PubMed] [Google Scholar]
- Saab H., Klinger D. School differences in adolescent health and wellbeing: Findings from the Canadian health behaviour in school-aged children study. Social Science & Medicine. 2010;70:850–858. doi: 10.1016/j.socscimed.2009.11.012. [DOI] [PubMed] [Google Scholar]
- Schnittker J., John A. Enduring stigma: The long-term effects of incarceration on health. Journal of Health and Social Behavior. 2007;48:115–130. doi: 10.1177/002214650704800202. [DOI] [PubMed] [Google Scholar]
- Schnoes C., Reid R., Wagner M., Marder C. ADHD among students receiving special education services: A national survey. Exceptional Children. 2006;72:483–496. [Google Scholar]
- Smith B.H., Waschbusch D.A., Willoughby M.T., Evans S. The efficacy, safety, and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD) Clinical Child and Family Psychology Review. 2000;3:243–267. doi: 10.1023/a:1026477121224. [DOI] [PubMed] [Google Scholar]
- Swanson J., Baler R.D., Volkow N.D. Understanding the effects of stimulant medications on cognition in individuals with attention-deficit hyperactivity disorder: A decade of progress. Neuropsychopharmacology. 2011;36:207–226. doi: 10.1038/npp.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner K., West P., Gordon J., Young R., Sweeting H. Could the peer group explain school differences in pupil smoking rates? An exploratory study. Social Science & Medicine. 2006;62:2513–2525. doi: 10.1016/j.socscimed.2005.11.017. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Education Determination letters on state implementation of IDEA. 2007. https://www2.ed.gov/policy/speced/guid/idea/monitor/factsheet.pdf accessed 17.05.18.
- U.S. Department of Education . . 2010. IDEA section 618 data products: State level data files. Educational environments, 2007https://www2.ed.gov/programs/osepidea/618-data/state-level-data-files/part-b-data/educational-environments/benvironment2007.csv accessed 17.05.18. [Google Scholar]
- Visser S.N., Danielson M.L., Bitsko R.H., Holbrook J.R., Kogan M.D., Ghandour R.M. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53:34–46. doi: 10.1016/j.jaac.2013.09.001. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron N.L., McLeskey J. The effects of an inclusive school program on students with mild and severe learning disabilities. Exceptional Children. 1998;64:395–405. [Google Scholar]
- Walsemann K.M., Bell B.A., Maitra D. The intersection of school racial composition and student race/ethnicity on adolescent depressive and somatic symptoms. Social Science & Medicine, Part Special Issue: Genetics, healthcare, family and kinship in a global perspective. Situated processes of co-construction. 2011;Vol. 72:1873–1883. doi: 10.1016/j.socscimed.2011.03.033. [DOI] [PubMed] [Google Scholar]
- Whalen C.K., Henker B., Buhrmester D., Hinshaw S.P., Huber A., Laski K. Does stimulant medication improve the peer status of hyperactive children? Journal of Consulting and Clinical Psychology. 1989;57:545–549. doi: 10.1037//0022-006x.57.4.545. [DOI] [PubMed] [Google Scholar]
- Zhang D., Hsu H.Y., Kwok O. man, Benz M., Bowman-Perrott L. The impact of basic-level parent engagements on student achievement: Patterns associated with race/ethnicity and SES. Journal of Disability Policy Studies. 2011 1044207310394447. [Google Scholar]