To the Editor:
Global travel numbers have been increasing worldwide, by 3.3% per year since 2010, and are expected to reach 1.8 billion travelers by 2030 (1). More travelers from the United States are now visiting cities in Asia and Africa, and megacities in these regions are known to have high levels of particulate matter (PM) pollution, at times resulting in major air pollution episodes. Therefore, international travelers can be exposed to very high levels of PM pollution if they arrive in these cities during an air pollution episode, and they lack the necessary adaptation and precautionary measures to minimize the associated health risks (2).
To date, we have not found any published studies that have researched the respiratory impacts of acute exposure to high levels of air pollution when individuals travel abroad to cities with significantly higher PM concentrations than their city of residence. To examine this issue, we measured and analyzed health and indoor PM exposure data from individuals who traveled from the United States to selected cities abroad, to test the hypothesis that when individuals travel abroad, exposure to higher levels of PM ≤2.5 μm in aerodynamic diameter (PM2.5) than are encountered in their home city will adversely impact their lung function.
Our study initially enrolled 42 nonsmoking, healthy young adults who traveled from the New York City metropolitan area to selected cities abroad, which were categorized into four regions: Europe, South Asia, East Asia, and Africa. Eight subjects were excluded from the analyses because of confounding activities and/or insufficient data (i.e., if they provided less than 5 days of data for baseline or when abroad). To be included in the study, subjects were required to 1) have traveled to a city abroad for at least a week, 2) be ≥21 years old, and 3) be a nonsmoker (self-reported). The New York University School of Medicine Institutional Review Board approved the study. Participants were pretrained to measure and record their lung function and personal indoor PM exposure levels using a portable spirometer (Koko PeakPro6; Ferraris) (3) and a low-cost PM2.5 sensor (AirBeam; Habitatmap), respectively. Health and PM2.5 data were obtained in the morning and evening of each day for 1 week before travel, 1 week during the stay abroad, and 1 week after the subjects returned to their home city (each subject provided at least 5 days of morning and evening measurements at each location). Lung function measurements were obtained in accordance with American Thoracic Society guidelines (4), and the highest value of three consecutive efforts was used for analyses. AirBeams were individually precalibrated using concentrated ambient particles at the New York University Sterling Forest laboratory. The measured PM2.5 concentrations were used to categorize cities into “polluted cities” categories (low [0–35 μg/m3], medium [36–100 μg/m3], and high [>100 μg/m3]), and lung function was assessed by the observed change in FEV1 by low, medium, or highly polluted categories. A mixed-effects statistical model was applied to repeated-measures longitudinal data for lung function and indoor PM2.5 measurements (total n of >700 data points) to study the association between FEV1 and PM2.5 exposure concentrations, using a subject-specific random intercept term (subject as random effect), along with covariates (age and height), and fixed terms (pollution level).
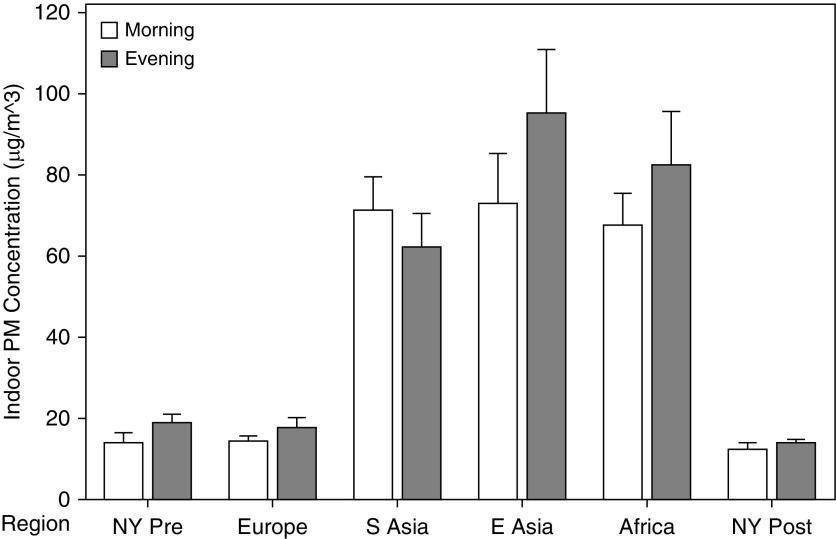
The study population consisted of healthy young adults (based on age, height, weight, and body mass index) who were mostly university students based in the New York City metropolitan area and New Jersey. In some regions, mean indoor PM2.5 concentrations in cities abroad were significantly higher than pretravel New York concentrations, particularly in South and East Asia. Cities in East Asia, as a group, had the highest (mean ± SD) indoor PM2.5 measurements (73 ± 96 μg/m3 and 95 ± 114 μg/m3 for morning and evening measurements, respectively). The mean PM2.5 concentrations in European cities were significantly lower than those in East and South Asia (Figure 1).
Figure 1.
Mean indoor (AirBeam measured) PM2.5 concentrations by region. Error bars are 1 SE from the mean. NY Post = after returning to resident city; NY Pre = before travel; PM = particulate matter; PM2.5 = PM ≤2.5 μm in aerodynamic diameter.
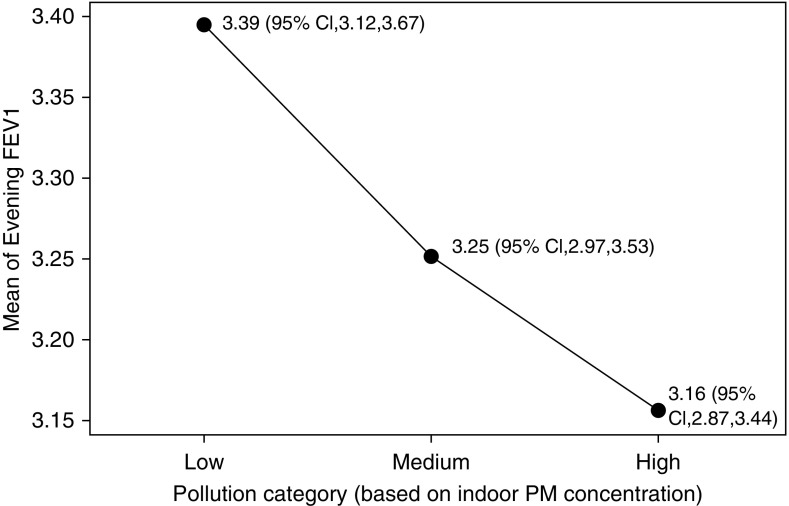
Results from the mixed-effects analysis showed that travel to a “high” polluted city was associated with a statistically significant mean decrement of 235 ml (95% confidence interval, −365 to −112 ml) in evening FEV1. Main effects plots showing the fitted (predicted) means of evening FEV1 for low, medium, and high polluted cities are given in Figure 2) (based on indoor PM2.5). When further analyzed using the maximum percentage change of FEV1, where maximum change = (minimum FEV1 abroad − mean pretravel FEV1/mean FEV1 in pretravel New York) × 100, travel to a highly polluted city was associated with a 6.5% reduction in evening FEV1 compared with the overall population mean.
Figure 2.
Main effects plot of fitted means for evening FEV1 with an indoor pollution category assigned to each city: low (0–35 μg/m3), medium (36–100 μg/m3), and high (>100 μg/m3). CI = confidence interval; PM = particulate matter.
We show, for the first time, that exposure to increased levels of indoor PM2.5 in cities abroad is associated with statistically significant acute changes in pulmonary function in healthy young adults. Together with increases in respiratory symptoms (data not shown), travelers to heavily polluted cities can be considered to encounter adverse health effects according to American Thoracic Society guidelines (5, 6). Similar results were obtained for outdoor PM2.5 (central monitor) concentrations and lung function reductions. It is important to note that the higher indoor concentrations recorded in some polluted cities abroad suggest that the traditional approach of staying indoors during high outdoor pollution episodes may not be effective. Although previous human chamber studies that exposed volunteers to fine PM showed no or very small decrements in lung function (7, 8), it is important to consider that owing to institutional review board and ethical considerations, chamber studies typically have limitations with respect to how high the PM concentrations can go. However, the subjects in this study were exposed to much higher PM levels in polluted cities abroad and for longer hours/days, and therefore their doses could have been much higher than those reported in chamber studies. Thus, travel provided a natural experiment in which individuals were exposed to high PM concentrations for long periods of time. The limitations of this study include not having a balanced number of subjects for each city, lack of time/activity pattern data for the subjects, and the possible influence of weather, although we believe that the results indicate that PM has greater impacts on lung function than these other potentially confounding factors.
In conclusion, our study suggests that travel-related exposure to increased PM adversely impacts individuals’ pulmonary function and health, which can be particularly important for travelers with a preexisting respiratory or cardiac disease. Recommendations from physicians may include avoiding travel to highly polluted cities, carrying asthma medication, and using suitable particle masks (e.g., with physician guidance) while abroad.
Some of the data used in this study have been previously analyzed and reported in the form of abstracts (9, 10).
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank all of the study participants for enrolling and providing data for the study; Dr. Dan Costa, Dr. Rick Peltier, and Dr. Chris Sanford for their advice and input in developing the methods used in this work; and John Adragna and Mianhua Zhong for their help with processing central monitor data and calibrating the AirBeam PM monitors.
Footnotes
Supported by National Institute of Environmental Health Sciences Core Center (ES000260) and Training (ES007324; T.G.) grants, an Air and Waste Management Association Scholarship 2017 (M.J.R.V.), and a grant from the New York University College of Global Public Health (T.G.).
Author Contributions: M.J.R.V. and T.G. planned the project. M.J.R.V. conducted subject training, acquired data, and performed the statistical analyses. M.J.R.V., G.D.T., and T.G. advised on the study design and analysis, and edited the manuscript. L.-C.C. contributed with experimental methods and equipment. C.C.L. contributed to equipment calibrations and reviewed the statistical analyses. All of the authors approved the work and final version of the manuscript.
Originally Published in Press as DOI: 10.1164/rccm.201811-2235LE on March 13, 2019
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.UN World Tourism Organization. UNWTO tourism highlights, 2017 edition. Madrid, Spain: UN World Tourism Organization; 2017. [Google Scholar]
- 2.Vilcassim MJR, Gordon T, Sanford CA. Does air pollution contribute to travelers’ illness and deaths?-evidence from a case report and need for further studies. J Travel Med. 2018;25:tay002. doi: 10.1093/jtm/tay002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brouwer AF, Roorda RJ, Brand PL. Comparison between peak expiratory flow and FEV(1) measurements on a home spirometer and on a pneumotachograph in children with asthma. Pediatr Pulmonol. 2007;42:813–818. doi: 10.1002/ppul.20660. [DOI] [PubMed] [Google Scholar]
- 4.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 5.Thurston GD, Kipen H, Annesi-Maesano I, Balmes J, Brook RD, Cromar K, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J. 2017;49:1600419. doi: 10.1183/13993003.00419-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Thoracic Society. What constitutes an adverse health effect of air pollution? Official statement of the American Thoracic Society. Am J Respir Crit Care Med. 2000;161:665–673. doi: 10.1164/ajrccm.161.2.ats4-00. [DOI] [PubMed] [Google Scholar]
- 7.Ghio AJ, Kim C, Devlin RB. Concentrated ambient air particles induce mild pulmonary inflammation in healthy human volunteers. Am J Respir Crit Care Med. 2000;162:981–988. doi: 10.1164/ajrccm.162.3.9911115. [DOI] [PubMed] [Google Scholar]
- 8.Samet JM, Graff D, Berntsen J, Ghio AJ, Huang YC, Devlin RB. A comparison of studies on the effects of controlled exposure to fine, coarse and ultrafine ambient particulate matter from a single location. Inhal Toxicol. 2007;19:29–32. doi: 10.1080/08958370701492706. [DOI] [PubMed] [Google Scholar]
- 9.Vilcassim MJR, Chen LC, Thurston GD, Gordon T.Traveling to cities abroad: impact on the cardiopulmonary system due to exposure to varying air pollution levels. Presented at the 57th Annual Meeting of the Society of Toxicology, March 11–15, 2018, San Antonio, TX [Google Scholar]
- 10.Vilcassim MJR, Thurston GD, Chen LC, Gordon T.Impact on the cardiopulmonary system when traveling to cities abroad due to variations in air pollution levels. Presented at the 15th Conference of the International Society of Travel Medicine (CISTM15), May 14–18, 2017, Barcelona, Spain [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.