Abstract
Background
High-sensitivity cardiac troponin assays enable the early risk stratification of patients with suspected acute coronary syndrome to identify those at low risk of myocardial infarction or cardiac death. We evaluated the performance of a novel high-sensitivity cardiac troponin I assay in early rule out pathways.
Methods
In 1920 patients with suspected acute coronary syndrome, cardiac troponin was measured using the Siemens Atellica high-sensitivity cardiac troponin I assay (99th centile: 34 ng/L women, 53 ng/L men). We evaluated three pathways which use either low risk-stratification thresholds of cardiac troponin (High-SensitivityTroponin in the Evaluation of patients with Acute Coronary Syndrome (High-STEACS) and the European Society of Cardiology (ESC) 1 hour pathway) or the 99th centile diagnostic threshold (ESC 3 hour pathway) to rule out myocardial infarction.
Results
The primary outcome of myocardial infarction or cardiac death at 30 days occurred in 14.4% (277/1920). The High-STEACS pathway ruled out 63% of patients (1218/1920), with five missed events for a negative predictive value (NPV) of 99.5% (95% CI (CI) 99.1% to 99.8%). Similar performance was observed for the ESC 1 hour pathway with an NPV of 99.0% (97.6% to 99.8%). In contrast, the ESC 3 hour pathway ruled out 65% of patients (1248/1920), but missed 25 events for an NPV of 98.0% (97.1% to 98.7%).
Conclusions
A novel high-sensitivity cardiac troponin I assay can safely identify patients at low risk of myocardial infarction or cardiac death. Diagnostic pathways that use low cardiac troponin concentrations for risk stratification miss fewer events than those that rely on the 99th centile to rule out myocardial infarction.
Trial registration
Keywords: acute coronary syndromes
Introduction
High-sensitivity assays enable quantification of low concentrations of cardiac troponin in healthy men and women, and permit accurate identification of the normal reference range and the 99th centile threshold recommended for the diagnosis of myocardial infarction.1 In addition to improvements in diagnostic accuracy, high-sensitivity cardiac troponin assays have the potential to improve the efficiency and safety of healthcare delivery by improving early risk stratification in patients with suspected acute coronary syndrome.
In a meta-analysis of 22 457 patients with suspected acute coronary syndrome, a high-sensitivity cardiac troponin I concentration <5 ng/L identified half of all patients as low risk with a negative predictive value (NPV) of 99.5% for myocardial infarction or cardiac death at 30 days.2 The High-Sensitivity Troponin in the Evaluation of patients with A cute Coronary Syndrome (High-STEACS) pathway incorporates this threshold at presentation with serial testing at 3 hours and misses less than one event in every 200 patients tested.3 The European Society of Cardiology (ESC) recommend a similar 1 hour pathway, which applies assay specific risk stratification thresholds and has excellent diagnostic performance.4–6 The ESC 3 hour pathway uses the 99th centile to rule in and rule out myocardial infarction, but the safety of this pathway has been challenged.3 7
Many early rule out pathways use assay specific thresholds, which has limited wider implementation of these promising approaches in practice. Here, we evaluate the diagnostic performance of a novel high-sensitivity cardiac troponin I assay (Atellica IM high-sensitivity troponin I, Siemens Healthineers) across three established risk stratification pathways currently used in clinical practice.
Methods
Study population
Patients with suspected acute coronary syndrome were recruited from the Emergency Department of the Royal Infirmary of Edinburgh, a tertiary care hospital in Scotland, between 1 June 2013 and 31 March 2017 into a substudy of the High-STEACS trial. All patients in whom the attending clinician requested cardiac troponin for suspected acute coronary syndrome were eligible. We did not enrol patients with ST-segment elevation myocardial infarction, those unable to provide consent or those from outside our region to ensure complete follow-up. Blood samples were obtained at presentation and at 6–12 hours as part of routine clinical care, with surplus serum or lithium-heparin plasma samples collected. Patients provided written informed consent for additional sampling at 1 or 3 hours (supplementary table S1). Samples were centrifuged, aliquoted and stored at −80°C for batch processing.
heartjnl-2018-314093supp001.docx (164KB, docx)
High-sensitivity cardiac troponin I assay
The Siemens Atellica IM High Sensitivity Troponin I assay (Siemens Healthineers) is a three-site sandwich immunoassay with a limit of detection of 1.6 ng/L and limit of quantification of 2.5 ng/L. The upper reference limit 99th centile was determined in 2007 samples from healthy individuals as 34 ng/L in women, and 53 ng/L in men, with a single threshold of 45 ng/L. In the reference range population, 75% of patients had values greater than the limit of detection. All measurements were undertaken by Siemens Healthineers at a central laboratory, who were blinded to all clinical information with results provided to the research team and linked to the trial database for analysis.
Baseline characteristics
Patient characteristics, clinical observations and cardiac investigations were obtained from a dedicated case record form, patient questionnaire and the electronic patient record.
Diagnostic adjudication
The final diagnosis was adjudicated by two independent cardiologists, with consensus from a third cardiologist where there was discrepancy following review of all clinical information, investigations and outcomes from presentation to 30 days (supplementary appendix). Any high-sensitivity cardiac troponin I concentration above the sex-specific 99th centile upper reference limit (Siemens Healthineers Atellica TnIH; 34 ng/L for women, 53 ng/L for men) was considered evidence of myocardial necrosis. Patients were classified as having type 1 myocardial infarction, type 2 myocardial infarction or myocardial injury in accordance with the third universal definition of myocardial infarction as reported previously.5 8
Clinical outcomes
The primary outcome was a composite of index type 1 myocardial infarction or type 1 myocardial infarction or cardiac death at 30 days. We used regional and national registries in addition to individual patient follow-up at 30 days, as previously described.3 All subsequent events were adjudicated using the same approach as for the index presentation. Cardiac death was defined as any death due to myocardial infarction, arrhythmia or heart failure.3
Clinical pathways
We evaluated the safety and efficacy of the High-STEACS pathway, the ESC 1 hour and the ESC 3 hour pathways.3 5 We determined diagnostic performance to rule out a composite outcome of index type 1 myocardial infarction, and type 1 myocardial infarction or cardiac death at 30 days.
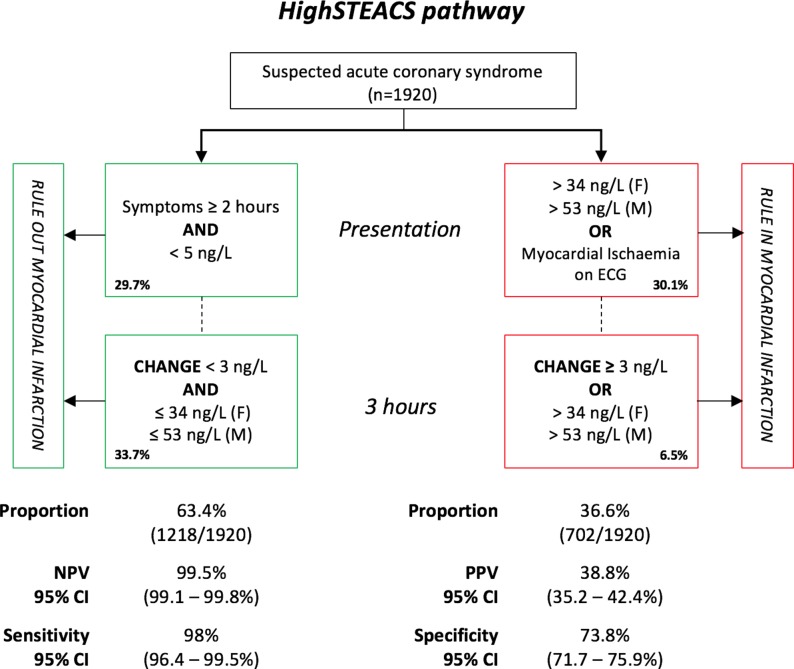
High-STEACS pathway
The derivation and validation of the High-STEACS pathway was undertaken using the Abbott ARCHITECTSTAT high-sensitivity cardiac troponin I assay,3 8 with the same thresholds applied to the Siemens Healthineers Atellica TnIH assay without recalibration. Patients without myocardial ischaemia on the ECG and cardiac troponin concentrations<5 ng/L at presentation were considered low risk, with myocardial infarction ruled out without further testing, unless they present early with symptom onset <2 hours from presentation where cardiac troponin was retested 3 hours after presentation. Patients with cardiac troponin concentrations≥5 ng/L at presentation were retested at 3 hours after presentation. Myocardial infarction was ruled out at 3 hours if cardiac troponin concentrations are unchanged (delta <3 ng/L) and remain ≤99th centile.
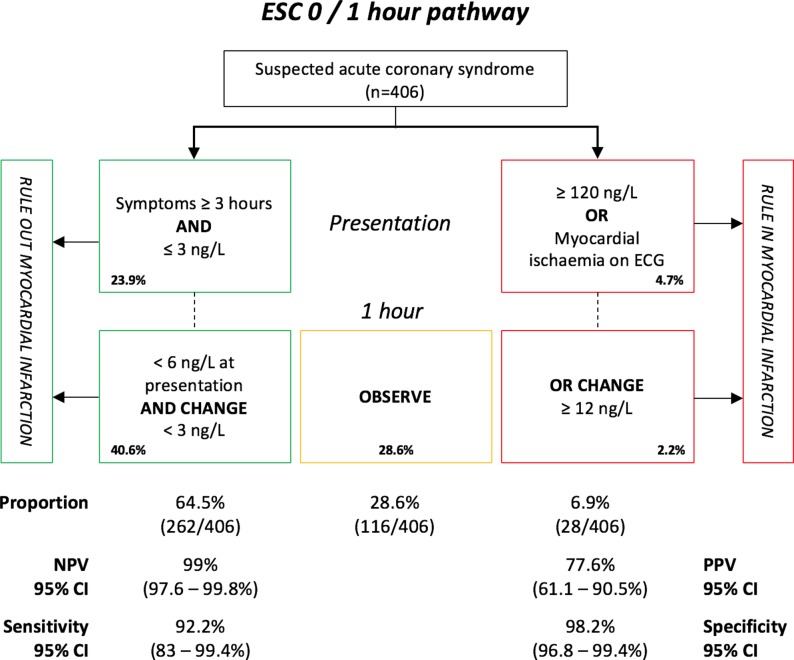
ESC 1 hour pathway
For the ESC 1 hour pathway, in patients without ischaemia on the ECG, myocardial infarction was ruled out where cardiac troponin concentrations were <3 ng/L at presentation and symptoms were present for >3 hours. In all other patients, myocardial infarction was ruled out if cardiac troponin concentrations were <6 ng/L at presentation with a change of <3 ng/L after 1 hour. Patients were ruled in where there was myocardial ischaemia on the ECG, if troponin concentrations were ≥120 ng/L at presentation, or a change of ≥12 ng/L was observed at 1 hour. These thresholds were recently derived and validated using the Siemens ADVIA Centaur assay and did not feature in the original ESC guidelines.4
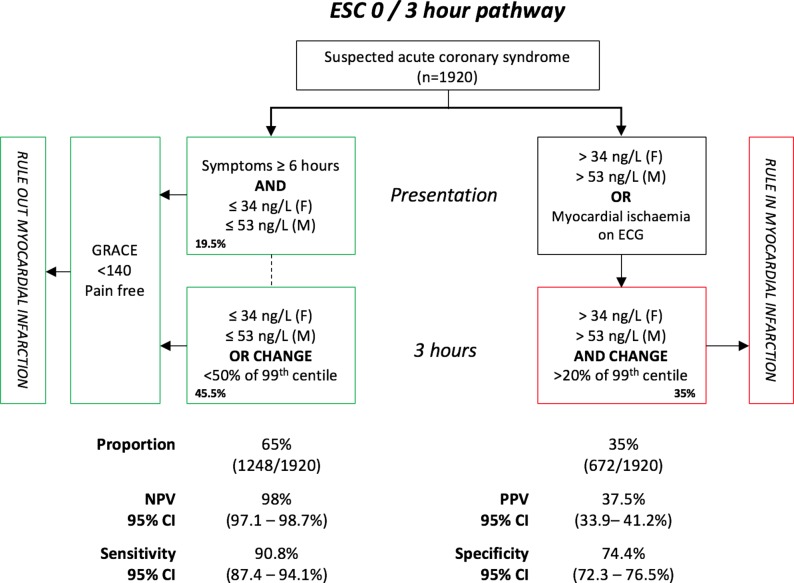
ESC 3 hour pathway
For the ESC 3 hour pathway, myocardial infarction was ruled out in patients without ischaemia on the ECG where cardiac troponin concentrations were <99th centile at presentation in patients with symptoms for >6 hours. In patients with symptoms for <6 hours, a second troponin measurement was performed 3 hours from presentation, with myocardial infarction ruled out if cardiac troponin remains <99th centile or was >99th centile without a significant change in concentration.5 Previously published guidance recommended use of a change in cardiac troponin concentration >50% of the 99th centile upper reference limit at 3 hours where the initial concentration was ≤99th centile, or >20% when the initial concentration was >99th centile. Patients were ruled out if pain free, and the GRACE score was <140.9 We calculated the GRACE score for in hospital death; this algorithm is available online.10
Subgroup and sensitivity analyses
We evaluated the performance of all pathways in prespecified subgroups, by age (≤65 vs >65 years), sex, history of ischaemic heart disease and time from symptom onset to presentation (2, 3 or 6 hours). As not all centres employ sex-specific thresholds, we repeated the primary analysis using a single diagnostic threshold (>45 ng/L). In a sensitivity analysis, we determined the performance of all pathways for a composite outcome of any myocardial injury (type 1 or type 2 myocardial infarction, or myocardial injury, or cardiac death at 30 days).
Statistical analysis
Baseline characteristics are summarised as mean (SD) or median (IQR) as appropriate. The primary outcome was the NPV of each pathway for the composite outcome estimated used a Bayesian approach with a Jeffrey’s prior as this is more robust when CIs approach 0 or 1.11 We determined absolute (hs-TnI3hr – hs-TnI0hr) and relative ([(hs-TnI3hr – hs-TnI0hr)/hs-TnI0hr] x 100) change in cardiac troponin concentration from presentation to 3 hours, and determined sensitivity, specificity and positive predictive value (PPV) with 95% CIs using a Bayesian approach as per the NPV. We determined the number of patients ruled in or ruled out as a proportion of the analysis population. As the ESC 1 hour algorithm stratifies patients into an observation group, where patients are neither ruled in or ruled out, these patients are not included in calculations of NPV and sensitivity (rule out group), or PPV and specificity (rule in group). We report in accordance with the STARD criteria for diagnostic accuracy studies.12 All analyses were performed using R V. 3.2.2.
Results
We enrolled 1951 patients with suspected acute coronary syndrome, of whom 1920 had a cardiac troponin I result available at presentation (table 1 and supplementary figure S1, respectively). The adjudicated diagnosis was type 1 myocardial infarction in 274 patients (14.3%), type 2 myocardial infarction in 64 patients (3.3%) and myocardial injury in 28 patients (1.5%), with six deaths from a cardiac cause at 30 days. Cardiac troponin concentrations were above the limit of detection in 90.8% (1743/1920) of patients, and higher at presentation in patients with type 1 myocardial infarction compared with those without (150 ng/L, IQR 57–800 ng/L vs 4 ng/L, IQR 2–7 ng/L).
Table 1.
Baseline characteristics of the study population
| All patients (n=1920) |
≤99th centile (n=1620) |
>99th centile (n=300) |
P values | |
| Baseline characteristics | ||||
| Age | 61.5 (14.2) | 60.3 (14.1) | 67.7 (13.3) | <0.001 |
| Male (%) | 1174 (61.1) | 975 (60.2) | 199 (66.3) | 0.052 |
| Chest pain (%) | 1613 (84.3) | 1369 (84.8) | 244 (81.3) | 0.389 |
| Symptom to arrival time (min) | 199 (118–461.5) | 199 (115–445) | 199 (134–521) | 0.044 |
| Medical history | ||||
| Diabetes mellitus (%) | 281 (14.6) | 222 (13.7) | 59 (19.7) | 0.009 |
| Hypertension (%) | 763 (39.7) | 614 (37.9) | 149 (49.7) | <0.001 |
| Hyperlipidaemia (%) | 760 (39.6) | 630 (38.9) | 130 (43.3) | 0.167 |
| Family history (%) | 922 (48.0) | 782 (48.3) | 140 (46.7) | 0.654 |
| Ischaemic heart disease (%) | 578 (30.1) | 474 (29.3) | 104 (34.7) | 0.071 |
| Previous myocardial infarction (%) | 455 (23.7) | 361 (22.3) | 94 (31.3) | 0.001 |
| Previous percutaneous coronary intervention (%) | 363 (18.9) | 294 (18.1) | 69 (23.0) | 0.059 |
| Previous coronary artery bypass grafting (%) | 117 (6.1) | 88 (5.4) | 29 (9.7) | 0.007 |
| Previous heart failure (%) | 64 (3.3) | 46 (2.8) | 18 (6.0) | 0.009 |
| Previous stroke (%) | 119 (6.2) | 96 (5.9) | 23 (7.7) | 0.309 |
| Smoker (%) | 385 (20.1) | 327 (20.2) | 58 (19.3) | 0.581 |
| Medication on admission | ||||
| Aspirin (%) | 650 (33.9) | 530 (32.7) | 120 (40.0) | 0.017 |
| Clopidogrel (%) | 250 (13.0) | 201 (12.4) | 49 (16.3) | 0.078 |
| Beta-blocker (%) | 518 (27.0) | 427 (26.4) | 91 (30.3) | 0.176 |
| ACE Inhibitor (%) | 578 (30.1) | 469 (29.0) | 109 (36.3) | 0.013 |
| Statin (%) | 819 (42.7) | 678 (41.9) | 141 (47.0) | 0.111 |
| Calcium channel blocker (%) | 240 (12.5) | 195 (12.0) | 45 (15.0) | 0.183 |
| Warfarin (%) | 104 (5.4) | 83 (5.1) | 21 (7.0) | 0.238 |
| ECG findings | ||||
| ST depression (%) | 112 (5.8) | 62 (3.8) | 50 (16.7) | <0.001 |
| ST elevation (%) | 58 (3.0) | 40 (2.5) | 18 (6.0) | 0.002 |
| T-wave inversion (%) | 298 (15.5) | 213 (13.1) | 85 (28.3) | <0.001 |
| Adjudicated index diagnosis | ||||
| Type 1 myocardial infarction (%) | 274 (14.3) | 54 (3.3) | 220 (73.3) | <0.001 |
| Type 2 myocardial infarction (%) | 64 (3.3) | 17 (1.0) | 47 (15.7) | <0.001 |
| Myocardial injury (%) | 28 (1.5) | 2 (0.1) | 26 (8.7) | <0.001 |
| 30-Day outcomes | ||||
| Type 1 myocardial infarction at 30 days (%)* | 8 (0.4) | 2 (0.1) | 6 (2.0) | <0.001 |
| Cardiac death at 30 days (%) | 6 (0.3) | 2 (0.1) | 4 (1.3) | 0.004 |
| Type 1 myocardial infarction or cardiac death at 30 days (%) | 277 (14.4) | 57 (3.5) | 220 (73.3) | <0.001 |
Troponin strata based on presentation concentration. Values are mean (SD), median (IQR) or n(%).
*Excluding index events.
High-STEACS pathway
The High-STEACS pathway identified 63.4% (1218/1920) of patients as low risk, with five missed events (four index type 1 myocardial infarction and one type 1 myocardial infarction at 30 days) for an NPV of 99.5% (95% CI 99.1% to 99.8%) and sensitivity of 98.0% (95% CI 96.4% to 99.5%). The PPV and specificity for the overall pathway were 38.8% (95% CI 35.2% to 42.4%) and 73.8% (95%CI 71.7% to 75.9%), respectively (figure 1).
Figure 1.
Diagnostic performance of the High-Sensitivity Troponin in the Evaluation of patients with Acute Coronary Syndrome (High-STEACS) pathway. NPV, negative predictive value; PPV, positive predictive value.
ESC 1 hour pathway
Where samples were available at presentation and 1 hour (406/1920; 21%), we evaluated performance of the ESC 1 hour rule out pathway. In this population, the prevalence of the primary outcome was 7.6% (31/406). The ESC 1 hour pathway identified 64.5% (262/406) of patients as low risk at 1 hour, with two missed cases, for an NPV of 99.0% (95% CI 97.6% to 99.8%) and sensitivity of 92.2% (95% CI 83% to 99.4%). The pathway identified 6.9% (28/406) of patients as high-risk for a PPV of 77.6% (95% CI 61.1% to 90.5%) and specificity of 98.2% (95% CI 96.8% to 99.4%). There were 28.6% (116/406) of patients who did not meet the rule in or rule out criteria, and were placed in the observe group (figure 2).
Figure 2.
Diagnostic performance of the European Society of Cardiology (ESC) 1 hour pathway. NPV, negative predictive value; PPV, positive predictive value.
ESC 3 hour pathway
The ESC 3 hour pathway identified 65% (1248/1920) of patients as low risk, with 25 missed events (24 index type 1 myocardial infarction and one cardiac death at 30 days) for an NPV of 98.0% (95% CI 97.1% to 98.7%) and sensitivity of 90.8% (87.4 to 94.1%)%). The PPV and specificity for the overall pathway were 37.5% (95% CI 33.9% to 41.2%) and 74.4% (95% CI 72.3% to 76.5%), respectively (figure 3).
Figure 3.
Diagnostic performance of the European Society of Cardiology (ESC) 3 hour pathway. NPV, negative predictive value; PPV, positive predictive value.
Prespecified subgroup analyses
We repeated the primary analysis in subgroups, stratified by age, gender, history of ischaemic heart disease and time of symptom onset. The performance of the High-STEACS pathway was robust in all groups (supplementary figure S2). The ESC 3 hour pathway (99th centile only) performed less well in patients with a history of ischaemic heart disease, where the NPV was 96.5% (95% CI 94.5% to 98%, supplementary figure S3). No significant heterogeneity was observed in the ESC 1 hour pathway (supplementary figure S4).
Sensitivity analyses
We repeated all analyses using the recommended single diagnostic threshold of 45 ng/L and observed no variation in performance (supplementary table S2). We then repeated all analyses using a composite endpoint including type 1 or type 2 myocardial infarction, myocardial injury or cardiac death, and we observed no changes in safety or efficacy (supplementary table S3).
Discussion
In a prospective observational cohort study of patients with suspected acute coronary syndrome, we performed the first evaluation of a novel high-sensitivity cardiac troponin I assay in three commonly used rule out pathways, and make a number of observations. First, using this assay, cardiac troponin concentrations were measurable in >90% of patients. Second, when applied in pathways which use low concentrations of cardiac troponin for risk stratification, this assay reliably identified patients at low risk of myocardial infarction or cardiac death at 30 days, with one missed case in every 200 patients tested. These findings were consistent by age, sex, history of ischaemic heart disease and time of symptom onset. Third, when applied in the ESC 3 hour pathway which rules out myocardial infarction at the 99th centile, there was a much higher risk of missed events, particularly in those with a history of ischaemic heart disease.
High-sensitivity cardiac troponin assays are defined by analytical characteristics which reflect their precision. The International Federation of Clinical Chemistry recommends the term high-sensitivity be reserved for an assay meeting two criteria; the coefficient of variation must be ≤10% at the 99th centile, and concentrations should be measurable (above the limit of detection) in at least 50% of a healthy reference population.13 14 At present, just one commercially available high-sensitivity cardiac troponin I assay meets these criteria (ARCHITECTSTAT, Abbott Diagnostics). The Siemens Healthineers Atellica TnIH assay does meet these criteria and provides an additional choice of cardiac troponin I assay to hospital specialists considering implementing an early rule out pathway in clinical practice.
We evaluated the performance of the Atellica assay across three commonly applied risk stratification pathways. The ESC 3 hour pathway applies the 99th centile as the threshold both to rule in and rule out myocardial infarction in conjunction with the GRACE risk score. In this analysis, the NPV and sensitivity were low, at 98.0% and 90.1% respectively, below the performance considered to be clinically acceptable in practice.15 This pathway was established at a time when contemporary troponin assays with higher diagnostic thresholds were used for diagnosis, and now, new approaches are required to match the precision offered by high-sensitivity troponin assays.
The High-STEACS and ESC 1 hour pathways performed well, with no heterogeneity observed by age, sex, history of ischaemic heart disease or time of symptom onset. While the thresholds applied in the High-STEACS pathway were derived and validated using the Abbott ARCHITECTSTAT high-sensitivity cardiac troponin I assay, they translate well to the Atellica TnIH assay with comparable efficacy and safety. This is because the High-STEACS pathway is based on three basic principles that make it likely to perform well across all high-sensitivity assays without recalibration. First, low troponin concentrations at presentation identify those at low risk. The risk stratification threshold of <5 ng/L employed here has been validated for both troponin I and troponin T in >30 000 patients.2 16 Second, increasing troponin concentrations above this threshold may be important and require further investigation. We define this using a change in troponin concentration of ≥3 ng/L based on the lowest measurable change in concentration that exceeds the analytical variation of a high-sensitivity assay.17 Third, to ensure our pathway is consistent with international guidelines and easy to integrate into clinical practice, we use a sex-specific 99th centile to identify patients who require admission for further investigation.18 We accept that this threshold is imperfect19 and assay specific, and therefore use the manufacturer’s recommended 99th centile concentration. Similarly, the thresholds applied in the ESC 1 hour pathway were derived and validated using the Siemens ADVIA Centaur assay, but our results were consistent with this initial study, suggesting additional calibration is not required.4 20
For clinicians considering implementation of an early rule out pathway, using very low cardiac troponin concentrations to identify low-risk patients has major potential to improve safety and decision making in the emergency department. As both pathways incorporating risk stratification thresholds have demonstrated similar safety and efficacy in a number of studies, the choice of approach is best determined by clinicians and laboratory staff at a local level. Alternative approaches using clinically validated risk scores are possible, such as the History, ECG, Age, Risk Factors Troponin (HEART), Emergency Department Assessment of Chest Pain Score (EDACS), Global Registry of Acute Coronary Events (GRACE) and Thrombolysis in Myocardial Infarction (TIMI) scores,21–24 but to date they have not shown benefit over pathways applying risk stratification thresholds.25 It is recognised that in some centres a 1 hour sample interval may be difficult to achieve, given the time taken for a sample to be obtained, transported to the laboratory, analysed and reported. However, while implementation of any pathway may require service redesign and investment in infrastructure, the potential improvements in efficiency by identifying two-thirds of patients as low risk in the emergency department are large and could lead to significant cost savings.
There are a number of limitations to this study which merit consideration. First, this was a single-centre observational cohort study, but as a tertiary cardiology centre with a large emergency department, we believe our findings are likely to be generalisable. Second, 1 hour samples for the evaluation of the ESC 1 hour pathway were only available in one in five patients, and in this population the prevalence of myocardial infarction or cardiac death was lower, indicating some selection bias and limiting the applicability of our findings. However, the observed performance is consistent with prior evaluations in other cohorts. Finally, no patients were managed on the basis of the measured cardiac troponin concentrations, and differences in clinical management and follow-up could have influenced outcomes. Two randomised controlled trials evaluating the implementation of risk stratification pathways are currently under way; an evaluation of the ESC 1 hour algorithm (LoDED trial; ISRCTN 86184521) and of the High-STEACS pathway (NCT:03005158).26
Conclusions
A novel high-sensitivity cardiac troponin I assay can safely identify two-thirds of patients with suspected acute coronary syndrome as low risk of myocardial infarction or cardiac death in the emergency department. Diagnostic pathways that harness the potential of high-sensitivity cardiac troponin testing by incorporating cardiac troponin concentrations within the reference range to risk stratify patients miss fewer events than pathways that rely on the 99th centile to rule out myocardial infarction.
Key messages.
What is already known on this subject?
High-sensitivity cardiac troponin assays can be applied as risk stratification tools in patients with suspected acute coronary syndrome.
A recent individual patient-level data meta-analysis in 22 457 patients demonstrated a high-sensitivity cardiac troponin I concentration <5 ng/L at presentation gave a high negative predictive value of 99.5% for myocardial infarction or cardiac death at 30 days.
What might this study add?
This is the first report of a new commercially available high-sensitivity cardiac troponin I assay and evaluates its performance across three commonly used risk stratification pathways in clinical practice.
We demonstrate pathways using low concentrations of cardiac troponin for risk stratification are safer and more effective than using the 99thcentile alone.
How might this impact on clinical practice?
The evidence provided in this study will allow clinicians and biochemists to make informed decisions as to the optimal approach for risk stratification of patients with suspected acute coronary syndrome in their hospitals.
Acknowledgments
The authors thank researchers from the Emergency Medicine Research Group Edinburgh for their support during the conduct of this trial.
Footnotes
Contributors: ARC and NLM were responsible for the concept, analysis and drafting of the manuscript, and take responsibility for the integrity of the data. All authors were involved in delivery of this clinical trial, contributed to analysis of the data and provided important critical revision of the manuscript.
Funding: The High-STEACS trial was funded by the British Heart Foundation (SP/12/10/29922 and PG/15/51/31596), and this analysis was supported by Siemens Healthcare Diagnostics. NLM and ARC are supported by the Butler Senior Clinical Research Fellowship (FS/16/14/32023) and a Clinical Research Training Fellowship (FS/16/75/32533), respectively, from the British Heart Foundation.
Competing interests: ASVS and ARC have received honoraria from Abbott Diagnostics. NLM has received honoraria or consultancy from Abbott Diagnostics, Roche Diagnostics, Siemens Healthcare Diagnostics and Singulex.
Patient consent: Not required.
Ethics approval: This clinical trial was registered (NCT:01852123), approved by the National Research Ethics Committee, and conducted in accordance with the Declaration of Helsinki.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data can be made available to others for the purposes of reproducing the results or for further analysis through a data sharing agreement.
References
- 1. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551–67. 10.1093/eurheartj/ehs184 [DOI] [PubMed] [Google Scholar]
- 2. Chapman AR, Lee KK, McAllister DA, et al. Association of high-sensitivity cardiac troponin i concentration with cardiac outcomes in patients with suspected acute coronary syndrome. JAMA 2017;318:1913–24. 10.1001/jama.2017.17488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chapman AR, Anand A, Boeddinghaus J, et al. Comparison of the efficacy and safety of early rule-out pathways for acute myocardial infarction. Circulation 2017;135:1586–96. 10.1161/CIRCULATIONAHA.116.025021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Boeddinghaus J, Twerenbold R, Nestelberger T, et al. Clinical validation of a novel high-sensitivity cardiac troponin i assay for early diagnosis of acute myocardial infarction. Clin Chem 2018;64:1347–60. 10.1373/clinchem.2018.286906 [DOI] [PubMed] [Google Scholar]
- 5. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267–315. 10.1093/eurheartj/ehv320 [DOI] [PubMed] [Google Scholar]
- 6. Mueller C, Giannitsis E, Christ M, et al. Multicenter evaluation of a 0-hour/1-hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin T. Ann Emerg Med 2016;68:76–87. 10.1016/j.annemergmed.2015.11.013 [DOI] [PubMed] [Google Scholar]
- 7. Pickering JW, Greenslade JH, Cullen L, et al. Validation of presentation and 3 h high-sensitivity troponin to rule-in and rule-out acute myocardial infarction. Heart 2016;102:1270–8. 10.1136/heartjnl-2015-308505 [DOI] [PubMed] [Google Scholar]
- 8. Shah AS, Anand A, Sandoval Y, et al. High-sensitivity cardiac troponin I at presentation in patients with suspected acute coronary syndrome: a cohort study. Lancet 2015;386:2481–8. 10.1016/S0140-6736(15)00391-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J 2012;33:2252–7. 10.1093/eurheartj/ehs154 [DOI] [PubMed] [Google Scholar]
- 10. Anderson F, FitzGerald G. Methods and formulas used to calculate the GRACE Risk Scores for patients presenting to hospital with an acute coronary syndrome. www.outcomes-umassmed.org/GRACE/publicfiles/GRACE_RiskModel_Coefficients.pdf2010.
- 11. Brown L, Cai T, DasGupta A. Interval estimation for a binomial proportion. Stat Sci 2001;16:101–33. [Google Scholar]
- 12. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015;351:h5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Apple FS, Sandoval Y, Jaffe AS, et al. Cardiac troponin assays: guide to understanding analytical characteristics and their impact on clinical care. Clin Chem 2017;63:73–81. 10.1373/clinchem.2016.255109 [DOI] [PubMed] [Google Scholar]
- 14. Apple FS, Jaffe AS, Collinson P, et al. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem 2015;48(4-5):201–3. 10.1016/j.clinbiochem.2014.08.021 [DOI] [PubMed] [Google Scholar]
- 15. Than M, Herbert M, Flaws D, et al. What is an acceptable risk of major adverse cardiac event in chest pain patients soon after discharge from the Emergency Department?: a clinical survey. Int J Cardiol 2013;166:752–4. 10.1016/j.ijcard.2012.09.171 [DOI] [PubMed] [Google Scholar]
- 16. Pickering JW, Than MP, Cullen L, et al. Rapid rule-out of acute myocardial infarction with a single high-sensitivity cardiac troponin t measurement below the limit of detection: a collaborative Meta-analysis. Ann Intern Med 2017;166:715–24. 10.7326/M16-2562 [DOI] [PubMed] [Google Scholar]
- 17. Kavsak PA, Don-Wauchope AC, Hill SA, et al. Acceptable analytical variation may exceed high-sensitivity cardiac troponin i cutoffs in early rule-out and rule-in acute myocardial infarction algorithms. Clin Chem 2016;62:887–9. 10.1373/clinchem.2016.255448 [DOI] [PubMed] [Google Scholar]
- 18. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. Eur Heart J 2018;2018. [DOI] [PubMed] [Google Scholar]
- 19. Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 2018;392:919–28. 10.1016/S0140-6736(18)31923-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Boeddinghaus J, Nestelberger T, Twerenbold R, et al. Direct comparison of 4 very early rule-out strategies for acute myocardial infarction using high-sensitivity cardiac troponin I. Circulation 2017;135:1597–611. 10.1161/CIRCULATIONAHA.116.025661 [DOI] [PubMed] [Google Scholar]
- 21. Van Den Berg P, Body R. The HEART score for early rule out of acute coronary syndromes in the emergency department: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care 2018;7:2048872617710788 10.1177/2048872617710788 [DOI] [PubMed] [Google Scholar]
- 22. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol 2013;168:2153–8. 10.1016/j.ijcard.2013.01.255 [DOI] [PubMed] [Google Scholar]
- 23. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA 2000;284:835–42. [DOI] [PubMed] [Google Scholar]
- 24. Than M, Flaws D, Sanders S, et al. Development and validation of the emergency department assessment of chest pain score and 2 h accelerated diagnostic protocol. Emerg Med Australas 2014;26:34–44. 10.1111/1742-6723.12164 [DOI] [PubMed] [Google Scholar]
- 25. Chapman AR, Hesse K, Andrews J, et al. High-sensitivity cardiac troponin i and clinical risk scores in patients with suspected acute coronary syndrome. Circulation 2018;138:1654–65. 10.1161/CIRCULATIONAHA.118.036426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chapman AR, Mills NL. A single blood test to rule out acute coronary syndrome. Heart 2018;104:632–3. 10.1136/heartjnl-2017-312269 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
heartjnl-2018-314093supp001.docx (164KB, docx)