Abstract
Objective
Academic pathology is facing a crisis; an ongoing decline in academic pathology posts, a paucity of academic pathologist’s in-training and unfilled posts at a time when cellular pathology departments are challenged to deliver increasing numbers of molecular tests. The National Cancer Research Institute initiative in Cellular & Molecular Pathology commissioned a survey to assess attitudes of cellular pathology consultants towards research in order to understand barriers and identify possible solutions to improve this situation. As cellular pathology is encompassing an increasing number of diagnostic molecular tests, we also surveyed the current approach to and extent of training in molecular pathology.
Methods
The survey was distributed to all UK-based consultant pathologists via the Pathological Society of Great Britain & Ireland and Royal College of Pathologist networks. Heads of Department were contacted separately to obtain figures for number of academic training and consultant posts.
Results
302 cellular pathologists completed the survey which represents approximately 21% of the total cellular histopathology workforce. Most respondents (89%) had been involved in research at some point; currently, 22% were undertaking research formally, and 41% on an informal basis. Of those previously involved in research, 57% stopped early in their consultant career. The majority of substantive academic posts were Professors of which 60% had been in post for >20 years. Most respondents (84%) used molecular pathology in diagnostic work, independent of where they worked or the length of time in post. Notably, 53% of consultants had not received molecular pathology training, particularly more senior consultants and consultants in district general hospitals.
Conclusions
The survey reveals that the academic workforce is skewed towards senior individuals, many of whom are approaching retirement, with a missing cohort of ‘junior consultant’ academic pathologists to replace them. Most pathologists stop formal research activity at the beginning of a consultant career. While molecular pathology is an increasing part of a pathologist’s workload, the majority of consultant cellular pathologists have not received any formal molecular training.
Keywords: academic pathology, molecular pathology, workforce
Introduction
Academic cellular pathology plays a pivotal role in advancing medical research and patient care. The 100 000 Genomes Project1 is a current example of a translational research initiative to which academic cellular pathology is making a substantial contribution; cellular pathologists’ morphological and molecular understanding is vital for the correct interpretation of study results.2 Furthermore, cellular pathologists are the gate-keepers of tissue biobanks, assess the quality of tissue used for translational molecular research and are at the forefront of the implementation of digital microscopy platforms3 which enable pathology research to be shared across continents.4 It is therefore of grave concern that the field of academic cellular pathology is in continuing decline.5
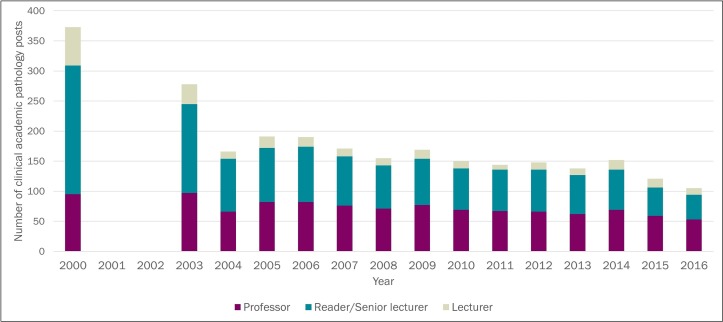
Over the past 15 years, the Medical Schools Council6 (MSC) has documented a stable number of overall clinical academic posts in the UK (figure 1) but an ongoing decline in the number of academic pathology posts (figure 2). Between 2000 and 2016, the MSC data6 show that the number of academic pathology consultants decreased by 69.8%, despite the overall number of pathology consultants increasing by 35%. In comparison with other specialties, pathology experienced the second greatest decline in academic posts6 in the preceding year (−11.5%); in contrast, the closely related specialties of oncology, radiology and surgery experienced only a minimal decline of −1.2%.
Figure 1.
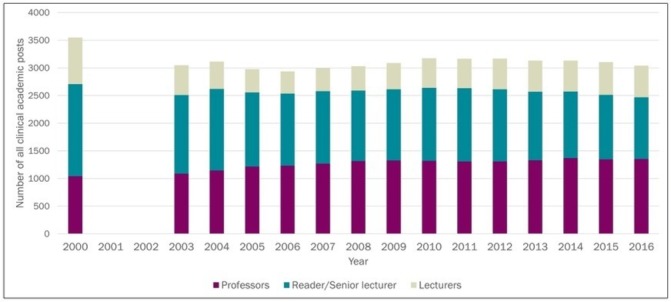
All clinical academic posts in the UK between 200 and 2016.
Figure 2.
Clinical academic pathology posts. There is a sharp decline of academic pathology posts at all levels but in particular Clinical Lecturers, Readers and Senior Lecturers. Data for 2001 and 2002 was not available.
There are approximately 103 histopathology departments in the UK, with a total of 1444 Histopathology and Cytopathology consultants, 165 unfilled consultant posts and approximately 100 University-funded consultant posts (Royal College of Pathologists (RCPath) workforce data). The 2017 MSC data indicate that 7% of academic pathology posts are unfilled.6
Of particular concern, there is a paucity of junior academic pathologists (who represent the ‘next generation’ of the academic pathology workforce); 81.5% of academic pathologists hold a senior post (which we have defined as Senior Lecturer/Reader or Professor).6 This reflects a wider general histopathology recruitment problem; the 2017 histopathology training recruitment round had a fill rate of only 71% compared with 98% in 2016.7 8 The ‘top-heaviness’ of the academic pathology workforce is set to continue; between 2015 and 2016, the number of Professors increased by 76.2% while the number of Lecturers declined by 46.7% and the number of Readers/Senior Lecturers declined by 53.1%, suggesting promotion of established academics, with an insufficient supply of new appointments at Senior Lecturer level to maintain the workforce.6
The current official UK academic histopathology training pathway is optional; it comprises four stages and extends the duration of training. First Academic Foundation training which provides doctors in their first 2 years of general physician training with 4 months of research time. Subsequently, doctors in their first 3 years of histopathology specialty training (ST1–ST3) can apply for an Academic Clinical Fellowship post that allocates 25% of training time to research. The aim is to generate sufficient pilot data to apply for an MD or PhD research training post. Trainees, who have completed a PhD, have passed the Fellow of the Royal College of Pathologist (FRCPath) Part 1 exam and are ST3 level or above are then eligible to apply for a Clinical Lecturer (CL) post. This has 50% training time ring-fenced for research. At the end of training, trainees can apply for a Consultant position with or without time protected for research or a University position with an honorary contract with the National Health Service (NHS; as a Reader/Senior Lecturer). It is important to highlight that there are different pathways for trainees into research from a standard trainee specialist post to obtain a MD or PhD.
Molecular pathology is a discipline of pathology which is focused on the identification and analysis of various molecules within tissues, rather than analysis solely based on morphology. This includes a wide variety of techniques from immunohistochemistry to sequencing technologies.9 10 Over the last decade, opportunities for molecular pathology training have expanded greatly as the DNA technology field has mushroomed with so many advancements.10 11
The National Cancer Research Institute initiative in Cellular and Molecular Pathology (CM-Path)12 was launched in 2016 to re-energise UK academic and molecular cellular pathology and to maximise tissue-based research within the NHS and in clinical trials. The aim of the CM-Path survey that we herein report was to assess current attitudes of UK histopathology consultants towards research. As Cellular Pathology is encompassing an increasing number of diagnostic molecular tests,2 we also surveyed the current approach to and extent of training in molecular pathology.
Material and methods
The need to collect more precise information about academic and molecular pathology (as the MSC and RCPath data provide only a general overview) was initially addressed in a survey written by Dr Bridget Wilkins in 2015 that collected detailed information from all the major UK academic pathology centres.13 The present survey was designed to capture further information, focusing on whether consultants had ever been involved in research, if they are currently involved in research and whether they are doing so formally (with allocated paid academic sessions) or informally. The survey also asked streamlined questions regarding attitudes towards the Research Excellence Framework (online supplementary data 1). The survey asked for the contact details of the respondent’s Head of Department. We emailed Heads of Department separately to obtain figures for the number of academic training and consultant posts within each Department. The second section of the survey asked about training in molecular pathology.
jclinpath-2018-205568supp001.pdf (148.6KB, pdf)
We did not give a specific definition of academic pathology or molecular pathology.
The survey was distributed to all UK-based consultant pathologists via the Pathological Society of Great Britain & Ireland and RCPath email networks. It was distributed over a 4-month period with completion of March 2017. The complete text of the survey can be found in online supplementary file 1.
Statistical analysis was performed via the Statistical Package for the Social Sciences (SPSS V.20.0, Chicago, IL, USA) and Excel.
Patient and public involvement
This was a questionnaire which was only distributed to Histopathology Consultants. There was no patient involvement in this survey.
Results
Academic pathology
A total of 347 consultants completed the survey, of which 302 were cellular pathologists (representing 21% of the total UK cellular pathology consultant workforce.) Of these, 88% were histopathologists, 7% neuropathologists, 2% oral and maxillofacial pathologists (not represented by the MSC data), 1.5% paediatric pathologists, 1% cytopathologists and 0.5% forensic pathologists.
Involvement in research
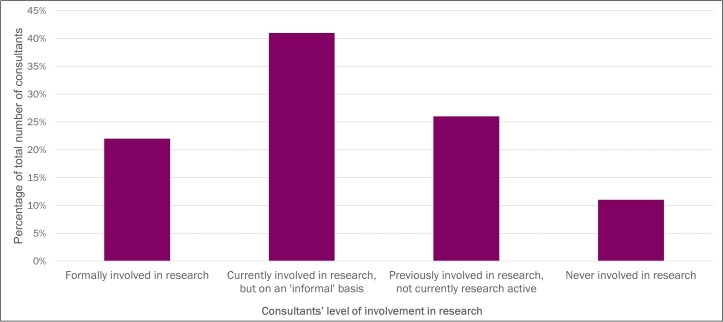
The majority of respondents (89%) had been involved in research at some point (figure 3). The majority of this group were still involved in research on an informal basis (41%), with a further 22% formally undertaking research and 26% who had previously been involved in research but were no longer involved. 11% of respondents were never involved in research.
Figure 3.
Consultants’ level of involvement in research.
Length of time as a consultant
The survey asked how long each respondent had been working as a consultant: there were 302 responses. The highest percentage was the group who had been working for over 20 years (36%) with the remainder of the responses subdivided as follows: 15–19 years (12%), 10–14 years (18%), 2–4 years (22%), 5–9 years (7%) and 0–1 year (1%). In the subgroup of Consultants that were never involved in research, the responses subdivided as follows: 15–19 and over 20 years (33%), 10–14 years (12%), 2–4 years (15%), 5–9 years (33%) and 0–1 year (12%)
Current work context
The majority of consultants were working in a teaching hospital (227); of the remainder, 73 were working in a district general hospital, 76 at a University and two in industry (of note, for this question, multiple answers were permitted.) In the subgroup of Consultants that were never involved in research, 58% were working in a district hospital and 42% in a teaching hospital.
Higher research degree
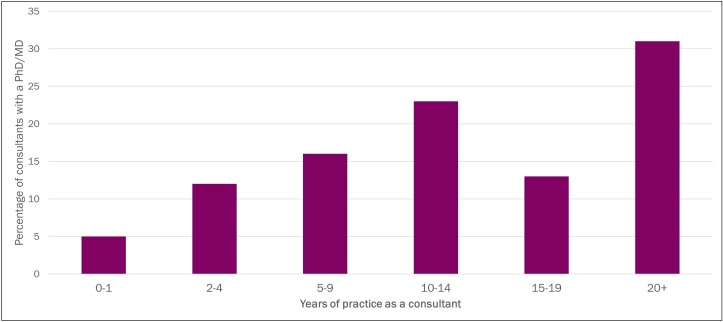
Just over a third of consultants (39%) held a higher degree (PhD or MD); the majority of these consultants (67%) had been a consultant for 10 years or more (figure 4). The majority (85%) of consultants with a higher degree were still involved in research either formally (37%) or informally (48%). Of all consultants formally involved in research, 64% had a higher degree and of those informally involved in research, 45% had a higher degree. The ‘informally involved in research’ consultant group is a hidden academic workforce which has the potential to strengthen and expand the pathology research community; the main barriers this group identified to becoming more formally involved in research were lack of time, resources, funding, departmental support and training. One suggestion from this group to improve the situation was to increase the availability of funded research programmed activities (PAs) within consultant job plans.
Figure 4.
The number of years that Consultants with a higher degree had been practising as a Consultant.
Academic appointments
Overall, 59 consultants held a substantive academic position: 51% were Professors, 14% Readers, 30% Senior Lecturers and 5% Lecturers/CLs. From emailing Heads of Departments, we obtained the following UK-level data: there are currently 22 National Institute of Health Research (NIHR)-funded Academic Clinical Fellow (ACF) posts, 11 NIHR-funded Academic CL posts, 36 Senior Lecturers, 3 Readers and 43 Professors. Although the academic grade of ‘Reader’ is not available in all Universities, the low number is concerning, as Readers are often promoted to Professor. Bart’s and the Royal London, Liverpool, Edinburgh and Leeds had higher than average cellular pathology clinical academic positions.
Academic appointment and length of time working as a consultant
The majority (60%) of Professors had been working for more than 20 years, 20% between 15 and 19 years and 20% between 10 and 14 years, indicating that a significant proportion of Professors will be approaching retirement in the next decade. Approximately a third (37.5%) of Readers had been a Consultant for 5–9 years, whereas the rest had worked as a Consultant for at least 10 years. Of the Senior Lecturers, 17% had worked 0–1 year as a consultant, 11% 2–4 years, 22% 5–9 years, 28% 10–14 years, 5% 15–19 years and 17% over 20 years.
When consultants stopped their involvement with research
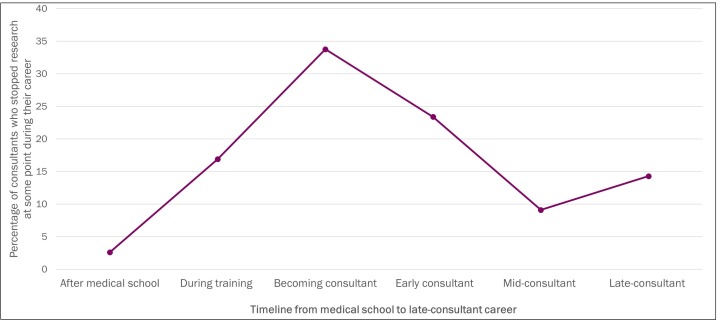
Of the consultants who had previously been involved in research, 57% stopped research either on becoming a consultant or during their early consultant career (figure 5).
Figure 5.
The percentage of consultants that stopped doing research at various times in their careers.
Molecular pathology
The molecular pathology questions were completed by 274 consultants.
Use of molecular pathology in diagnosis
The majority of respondents (84%) stated that they use molecular pathology in their diagnostic work, with half of these stating that they use molecular pathology ‘a lot’. Only 8% did not use molecular pathology for diagnosis. Responses were similar across consultants working in both teaching hospitals (39% using it ‘a lot’) and district general hospitals (37% using it ‘a lot’) and across the different categories of length of time consultants had been in post (from 0 to 1 year to 20+years), indicating that similar proportions of consultants at all levels working in both major types of hospital setting are using molecular pathology diagnostically. Of the consultants that have never been involved in research, 24% use molecular pathology a lot, in comparison with 43% of consultants that are formally involved in research.
Furthermore, 46% of consultants anticipated that molecular pathology will become ‘increasingly important’ in the near future and a further 45% anticipated that it will become ‘essential’ (total 91%). These attitudes were similar among consultants working at district general hospitals (75%) and teaching hospitals (84%). In the subgroup of consultants that were never involved in research, 53% anticipated that molecular pathology will become ‘increasingly important’ in the near future and a further 28% anticipated that it will become ‘essential’ (total 86%). 15% of responders stated that it is ‘not important as I am reaching the end of my career’. In the group of consultants which are formally involved in research, 25% anticipated that molecular pathology will become ‘increasingly important’ in the near future and a further 57% anticipated that it will become ‘essential’ (total 82%). 1.5% of responders stated that it is ‘not important as I am reaching the end of my career’.
Almost a fifth (19%) of consultants stated that they are involved in the delivery of molecular pathology services. The majority of these consultants (96%) were currently involved in research either formally (43%) or informally (53%) and almost all were working in a teaching hospital (96%).
Training in molecular pathology
Of concern, 53% of consultants had not received any molecular pathology training; 39% had been trained informally (the majority of which is local support interpreting reports) and 9% had undergone some formal training. Importantly, senior consultants were less likely to have received any molecular pathology training despite molecular pathology being used diagnostically by consultants at all levels. Furthermore, despite molecular pathology being used diagnostically by similar proportions of consultants working in teaching hospitals and district general hospitals, consultants working in district general hospitals were less likely to have received any molecular training (63% compared with 42% of consultants working in teaching hospitals) and were less likely to have received any formal training (3% compared with 9% of consultants working in teaching hospitals). The majority (79%) of consultants who had received formal training in molecular pathology were currently involved in research (either formally or informally), indicating the overlap between molecular and academic pathology.
Consultants stated that most of their molecular pathology training stemmed from interacting with the scientists that produce molecular pathology reports through the following: establishing local molecular services; research activities; learning ‘on the job’ and self-directed reading and attending courses. Consultants identified a number of key training topics, including genomics, bioinformatics, biomarker validation and digital pathology. Ideally, they felt that training should be clinically applicable, specialty specific, provided within study leave time and budget and delivered as an initial training session followed by updates. A minority of consultants felt that molecular training was inappropriate for them, citing approaching retirement and an inappropriate division of labour/duplicating skill sets.
The perceived barriers to the use of molecular pathology were a lack of funding, too many competing commitments, a lack of specialty-specific training, a lack of clear guidance, the increasing rate of use of new molecular techniques and the perception of molecular pathology as a distinct entity.
Discussion
Given the current parlous state of academic cellular pathology and the importance of molecular pathology in mainstream diagnostic pathology, this survey was designed to assess UK consultant cellular pathologists’ attitudes to these areas, in particular focusing on barriers to research and training in molecular pathology, so that the results of the survey might direct solutions to address these issues.
The survey data should be interpreted with the caveat that only 21% of the total consultant cellular pathology workforce completed the survey. The consultant cellular pathology workforce is defined as consultant cellular pathologists who are registered with the RCPath and working in the UK. Perhaps due to distribution of the survey via the Pathological Society, which is a highly research-focused society for pathologists, 70% of the academic cellular pathology consultant workforce completed the survey. This means that our data may represent a more favourable picture of the attitudes of consultants towards academic pathology than is present in the total UK pathology workforce. However, it is unlikely to present a more favourable view of attitudes towards molecular pathology as this part of our survey revealed similar attitudes among all respondents.
Self-identification and differences in interpretation of the terms of molecular pathology and academic pathology are limitations of the survey. However, we made every effort to confirm the number of substantive academic consultants by contacting the relevant Heads of Department.
A further limitation of the survey was that data on gender were not collected. This is unfortunate, as independent data indicate14 that there are more male than female clinical academic pathologists, particularly at more senior, Professorial positions. In our data, we saw the sharpest decline in individuals’ involvement in research (despite having a higher degree) at the beginning of, or in the early years of, their consultant careers (figure 5). Data from other specialties suggest that the attrition of academic medicine workforce numbers at the point of transition to consultant is greater for females compared with males.15 A further, wider question is how clinic academic careers can be made more attractive for not just women but all consultant pathologists with caring responsibilities, for example flexible working hours, support with childcare arrangements especially during conferences16 17 and availability of academic funds to support research during career breaks.18 These issues are closely linked to the work of the Athena Swan Charter. These data raise the question of whether programme to provide payment for research-specific clinical sessions for academically trained cellular pathologists might effectively reduce the number of consultants stopping research at this point of their careers.19
The data collected from Heads of Departments confirm that there is a small number of UK academic cellular pathologists. These data are in keeping with the MSC data which have shown a marked decline in academic pathologists over the last decade. The majority (67%) of consultants who have a higher degree have been a consultant for 10 years or more and the academic post after retirement have not been replaced like-for-like. There is also an indication of a paucity of pathology trainees currently undertaking higher degrees. Of the few that do, many stop their formal involvement in research early in their consultant career due to a lack of dedicated time for research, a lack of senior academic University posts, the high requirements for transition to Senior Lecturer and very high requirements to gain a substantial Clinical Research Fellowship such as a Clinican Scientist Fellowship. This missing cohort of ‘junior consultant’ academic pathologists at Senior Lecturer level represents one of the key findings emerging from this survey. Universities should be persuaded that maintaining a research active cohort of Senior Lecturers in academic cellular pathology is important for maintaining future research efforts both in Pathology and in wider research areas. The skewing of the academic workforce towards more senior individuals, a large proportion of whom are approaching retirement, will mean that there is an imminent decline in mentors and role models to inspire and guide the next generation of cellular pathology academics.
The survey has also highlighted the need to nurture the next generation of academic cellular pathologists. A possible solution to improve the total number of academic pathologists could be to increase early visibility through promotion of pathology and academic medicine at medical school and to increase the number of academic foundation histopathology posts. This should continue by supporting a higher number of cellular pathology trainees to undertake research including increased numbers of ACFs, funded PhD research fellowships and CL positions. The Pathological Society of Great Britain and Ireland is championing academic pathology throughout this academic training pathway. Members of CM-Path have met with representatives of the RCPath to develop proposals for revising the existing optional research module within the Histopathology Curriculum.
Of particular interest, the survey reveals that a large proportion of consultant pathologists are undertaking research informally outwith their job plans; many would like to increase their research activities but feel they require dedicated research time to do so. This group represents a trained and enthusiastic ‘hidden academic workforce’, which could contribute more to pathology research, if better supported. A proportion of senior lecturers in our survey have honorary contracts with a university but no paid sessional commitment in job plans for research. It is important to highlight the goodwill of these Consultants who are supporting academic pathology within their own time and to consider the costs to the NHS and academic pathology if this goodwill was lost through, for example, lack of support and increasing competing work pressures. This would have wide implications, for example, for the collection of tissue samples, trials, education of technical staff and trainees. One possible approach to address this would be by providing dedicated funded research sessions, such as through clinical trials funding or major programmatic research funding and for pathologists to insist on funded research PAs when agreeing to contribute pathological expertise to research programme and trials. Another possibility could be offering re-training and research exposure to Histopathology Consultants that were once research active. It is extremely reassuring to note that the MRC and NIHR have recently launched a funded scheme supporting NHS consultants with a PhD or MD (or equivalent higher research degree) to collaborate with biomedical researchers working in centres of research excellence; histopathologists who are eligible should be encouraged to apply.20
The molecular pathology section of the survey has revealed that the majority of consultant cellular pathologists are using molecular pathology in their diagnostic work yet are doing so without any formal training. The survey indicates that fewer senior consultants and cellular pathologists working in district general hospitals have received training in molecular pathology compared with their more junior colleagues and those working in teaching hospitals, despite consultant pathologists of all grades and hospital settings using molecular pathology diagnostically to a similar degree. Centralisation of NHS services over the past few decades has meant that there is now a greater concentration of histopathologists working in teaching hospitals; however, there should not be such inequity in molecular pathology training. The RCPath has formally introduced molecular pathology into the current histopathology training curriculum so that histopathology trainees are receiving molecular pathology training and there remains scope to expand and improve this further2; however, training for the existing consultant workforce has not been formalised.
A number of courses such as the Health Education England Master Degree or Postgraduate certificate in Genomic Medicine have been funded to address molecular pathology training and to develop a workforce of ‘morphomolecular’ pathologists.2 These courses have not been histopathology-specific (they are for doctors from all specialties and biomedical scientists); a dedicated histopathology-specific course could specifically address the clinical issues related to molecular pathology that histopathologists are facing. To this extent, the British Division of the International Academy of Pathology (BPIAP) and the CM-Path have organised several molecular pathology conferences/study days with the aim to update the workforce. Consultants need the encouragement, time and funding to attend such courses. The UK’s patchy and self-directed approach to molecular pathology training of consultants is in contrast to the formalised post-residency fellowship programme offered in the US.
While a minority of respondents felt that molecular training was inappropriate for them, citing approaching retirement and an inappropriate division of labour/duplicating skill sets, and while an increasing number of molecular tests are becoming automated,21 there is still and always will be a requirement for cellular pathologists to understand the molecular tests that they request and to interpret the results in the context of the sample quality and clinical information.10 Training will need to be ongoing throughout the career of a consultant histopathologist as molecular tests evolve and increase with the advancement of molecular technologies. Such ongoing training may not need to be formalised and could take the form of self-directed experiential learning and continuing professional development, with competency assessed and monitored by quality assurance schemes such as the NEQAS scheme for programmed death-ligand 1 (PD-L1) reporting.11
It is noteworthy that consultants who are involved currently in research, either formally or informally, are more likely to be involved in the delivery of molecular pathology services and to have received formal molecular pathology training. Their attitude towards molecular medicine is the strongest between all subgroups as more than half of this group stated that it is ‘essential’. This reiterates the importance of academic cellular pathology as pathology diagnostics become increasingly ‘morphomolecular’. Research-active consultant cellular pathologists have the potential to be an important resource in disseminating molecular knowledge to colleagues.
It is hoped that all of the aforementioned actions will start to address the issues facing academic and molecular cellular pathology. We plan to monitor progress with follow-up surveys as these initiatives are implemented and to use qualitative methods to explore attitudes, challenges and possible solutions in greater depth.
Take home messages.
The survey reveals that academic pathology is facing a crisis as the workforce is skewed towards senior individuals, many of whom are approaching retirement and a missing cohort of ‘junior consultant’ academic pathologists to replace them.
Most pathologists stop formal research activity at the beginning of a consultant career.
While molecular pathology is an increasing part of a pathologist’s workload, the majority of consultant cellular pathologists have not received any formal molecular training.
Footnotes
SB and CY contributed equally.
Handling editor: Tahir S Pillay.
Contributors: BS, CY, JL and GT designed data collection tools, monitored data collection for the whole study and wrote the statistical analysis plan. SB and CY cleaned and analysed the data. SB, CY, JL, MA, BW, GT, LJ, KO and KH drafted and revised the paper.
Funding: Funding was available from NCRI CM-Path.
Competing interests: None declared.
Patient consent for publication: Not required
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Genomics England Limited The 100,000 genomes project. Available: https://www.genomicsengland.co.uk/the-100000-genomes-project [Accessed Jan 2018].
- 2. Moore DA, Young CA, Morris HT, et al. . Time for change: a new training programme for morpho-molecular pathologists? J Clin Pathol 2018;71 10.1136/jclinpath-2017-204821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Williams BJ, Lee J, Oien KA, et al. . Digital pathology access and usage in the UK: results from a national survey on behalf of the National Cancer Research Institute's CM-Path initiative. J Clin Pathol 2018;71:463–6. 10.1136/jclinpath-2017-204808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jones JL, Oien KA, Lee JL, et al. . Morphomolecular pathology: setting the framework for a new generation of pathologists. Br J Cancer 2017;117:1581–2. 10.1038/bjc.2017.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wright N. The waxing and waning of academic pathology: a personal view. understanding disease: a centenary celebration of the pathological Society, 2006, 2006. ISBN0-470-03220-0. [Google Scholar]
- 6. Medical Schools Council Survey of medical ClinicalAcademic staffing levels 2017, 2018. Available: https://www.medschools.ac.uk/media/2026/medical-clinical-academic-staffing-levels-2017.pdf [Accessed Jan 2018].
- 7. Health Education England Competition ratios 2017 ST1. Available: https://specialtytraining.hee.nhs.uk/portals/1/Content/Resource%20Bank/Competition%20Ratio's/Competition%20Ratios%202017%20ST1.pdf [Accessed Jan 2018].
- 8. Health Education England Medical recruitment. Available: https://hee.nhs.uk/our-work/attracting-recruiting/medical-recruitment/specialty-recruitment-round-1-acceptance-fill-rate [Accessed Jan 2018].
- 9. The Royal College of Pathologists Overview of molecular pathology Bulletin, 2016. Available: https://www.rcpath.org/profession/publications/college-bulletin/college-bulletin/overview-of-molecular-pathology.html
- 10. Normanno N, Cree IA. Genomics driven-oncology: challenges and perspectives. BMC Cancer 2015;15 10.1186/s12885-015-1147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. NEQAS 4th cardiac marker Dialogues meeting. Available: https://ukneqas.org.uk/
- 12. NCRI The CM-Path initiative launched in June 2016 and aims to reinvigorate UK academic pathology. Available: https://cmpath.ncri.org.uk [Accessed Jan 2018].
- 13. Wilkins BS, Freeman A, Salto-Tellez M, et al. . Research capacity and attitudes in UK cellular pathology. NCRI Congress, 2015. [Google Scholar]
- 14. Medical Schools Council Survey of medical clinical academic staffing levels, 2017. Available: https://www.medschools.ac.uk/media/2026/medical-clinical-academic-staffing-levels-2017.pdf [Accessed Jan 2018].
- 15. Health Education England, NHS Education for Scotland 2017 UK-Wide survey of clinical andHealth research fellowships. Available: https://www.healthandcareresearch.gov.wales/uploads/2017%20Clinical%20and%20Health%20Research%20Fellowships%20Survey_final.pdf [Accessed Jan 2018].
- 16. Shen H. Lone-parent scientist. Nature 2016;531:129–31. 10.1038/nj7592-129a [DOI] [PubMed] [Google Scholar]
- 17. Calisi RM, Sci WGM, a Working Group of Mothers in Science . Opinion: how to tackle the childcare-conference conundrum. Proc Natl Acad Sci U S A 2018;115:2845–9. 10.1073/pnas.1803153115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cornelia Lawson AG, Finardi U. Scientists penalized by motherhood. Available: www.sciencedaily.com/releases/2018/03/180329095741.htm [Accessed 29 Mar 2018].
- 19. Ceci SJ, Ginther DK, Kahn S, et al. . Women in academic science: a changing landscape. Psychol Sci Public Interest 2014;15): :75–141. 10.1177/1529100614541236 [DOI] [PubMed] [Google Scholar]
- 20. Medical Research Council Clinical academic research partnerships. Available: https://mrc.ukri.org/funding/browse/carp/clinical-academic-research-partnerships/?utm_medium=email&utm_source=govdelivery [Accessed Dec 2018].
- 21. Uguen A, Troncone G. A review on the Idylla platform: towards the assessment of actionable genomic alterations in one day. J Clin Pathol 2018;71:757–62. 10.1136/jclinpath-2018-205189 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jclinpath-2018-205568supp001.pdf (148.6KB, pdf)