Abstract
Androgenetic alopecia (AGA), also known as androgenic or pattern alopecia, is a frequently reported disorder that affects both the sexes, with a higher incidence generally reported in men. AGA has immense psychological effects on the patient, irrespective of the age or stage of baldness. This consensus document has been developed taking into account the opinions of leading experts in the field of dermatology. The objective of this article is to provide the dermatologists with an evidence-based platform for choosing efficacious and safe therapy for patients with AGA. This review articulately summarizes the key opinions of the experts on all aspects of treatment for the effective management of AGA.
Key words: Androgenetic alopecia, management, treatment
INTRODUCTION
Androgenetic alopecia (AGA), also called androgenic or pattern alopecia, is an extremely common disorder affecting both sexes, although its incidence is generally greater in men than in women.[1] AGA has immense psychological impact on patients, irrespective of age or the stage of baldness.[2]
It has been noted that early-onset AGA is a strong predictor of premature initiation of severe coronary heart disease and metabolic syndrome. People with high body mass index may suffer from severe AGA.[3]
NEED FOR A CONSENSUS PAPER
The purpose of this consensus document is to provide dermatologists with an evidence-based platform for choosing an efficacious and safe therapy for patients with AGA.[4] A group of 120 renowned hair experts (dermatologists and plastic surgeons) were involved in focused group discussions across eleven Indian cities, and brainstormed on etiopathogenesis, clinical features, diagnostics, and therapeutics of this condition. The discussions conducted in phasic manner were recorded and meticulously transcribed. The moderators critically reviewed the compiled manuscript and added their comments for incorporating specific modifications in the document to ensure its authenticity. This paper is a summary of the experts' discussion covering all aspects of alopecia management.
DEFINING THE PROBLEM
AGA is a genetic disorder characterized by gradual conversion of terminal hairs into indeterminate, and finally into vellus hairs.[5]
EPIDEMIOLOGY
In men, AGA is considered to be the most common type of baldness characterized by progressive hair loss. People of all races can be affected though the prevalence rates may vary.
In the Indian context, a prevalence rate of 58% in males aged 30–50 years has been found. In all cases, the incidence gradually increases with age.[2] In women, epidemiological data are scarce.
RECALLING THE PATHOLOGY
In AGA patients, terminal hairs gradually get converted into indeterminate hairs and finally to vellus hairs. The terminal-to-vellus hair ratio is reduced from the normal 7:1 to <4:1. Miniaturization of the follicles is followed by development of fibrous tracts. AGA is typically characterized by a patterned distribution of hair loss.[5]
Genetic variants of the androgen receptor are believed to be responsible for causing AGA in men. Dihydrotestosterone (DHT), produced by the action of 5-alpha-reductase on testosterone, plays a key role. Male-pattern baldness is not related to androgen levels in the blood but is due to a genetically variable sensitivity of hair follicles to normal levels of circulating androgen.[6] Development of AGA involves multiple genes. The gene for the androgen receptor lies on the X chromosome; thus, the tendency in men to develop AGA in later life is inherited from the maternal line. There is limited information on female AGA, but genetic predisposition is known to play a major role.[6]
CLINICAL FEATURES AND GRADING
In men, the most accepted grading system for AGA is the modified Norwood–Hamilton classification consisting of seven broad groups and four specific variant types [Table 1].[1,2]
Table 1.
Modified Norwood-Hamilton classification of male pattern androgenetic alopecia
| Clinical definition | Type |
|---|---|
| I. Minimal recession of hairline along the anterior border in the FT region |  |
| II. The anterior border of the hair in the FT region has triangular areas of recession that tend to be symmetrical. These areas extend no further posterior than approximately 2 cm anterior to a line drawn in a coronal plane between the external auditory meatus on both the sides. Hair is either lost or sparse along the mid-frontal border of the scalp |  |
| IIa. The entire anterior border of the hairline lies high on the forehead. The usual mid-frontal island of hair is represented by only a few sparse hairs. The area of denudation extends no further than 2 cm from the frontal line | 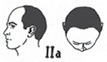 |
| IIIa. The area of denudation reaches the mid-coronal line |  |
| III. Characterized by deep FT hair recession, usually symmetrical and either bald or sparsely covered with hair. These areas of hair recession extend further posterior to a point that lies approximately 2 cm anterior to a line drawn in a coronal plane between the external auditory meatus on either side |  |
| IIIv (vertex). Hair is mainly lost in the vertex. There may be some frontal recession, but it does not exceed that seen in type |  |
| IV. The frontal and FT recession is more severe than in type III. There is also sparseness or absence of hair in the vertex area. These bald areas are extensive, but separated from each other by a band of moderately dense hair that joins the fully haired fringe on each side of the head |  |
| IVa. The area of denudation extends beyond the mid-coronal line, and there may be considerable thinning of hair posterior to the actual hair line | 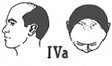 |
| V. The hair loss over the vertex and FT areas is larger than in type IV and the band of hair between them are narrower and sparser |  |
| Va. Most advanced degree of alopecia; however, the bald area does not reach the vertex |  |
| VI. The hair loss over the FT and vertex regions is confluent and the bridge of hair that crosses the crown is absent |  |
| VII. There is only a narrow horseshoe-shaped band of hair that begins laterally, just anterior to the ear and extends posteriorly on the sides and fairly low on the occipital area |  |
FT – Frontotemporal
In women, the most common grading scales used for AGA are the three-point Ludwig scale [Table 2] and the five-point Sinclair scale [Table 3].[1,2]
Table 2.
Ludwig’s scale for female androgenetic alopecia
| Stage | Severity of female hair loss |
|---|---|
 Stage 1 Stage 1 |
Thinning of hair is seen mainly over the anterior part of the crown with minimal widening of the parting width |
 Stage 2 Stage 2 |
Thinning of the crown becomes more evident because of an increase in the number of thin and short hairs |
 Stage 3 Stage 3 |
The crown becomes almost total bald. There is significant widening of the parting width, but the frontal hairline is still maintained |
Table 3.
Sinclair scale for female pattern androgenetic alopecia
| Grade | Characeristics |
|---|---|
| Grade 1 | Normal. This pattern is found in all girls prior to puberty but in only 45% of women aged 80 or over |
| Grade 2 | Widening of the central part |
| Grade 3 | Widening of the central part and thinning of hair on either side of the central part |
| Grade 4 | Diffuse hair loss over the top of the scalp |
| Grade 5 | Advanced hair loss |
DIAGNOSIS
History
A good history examination is essential to exclude other causes of hair loss, such as telogen effluvium (TE). The usual complaints are those of chronic hair loss with thinning mainly over the frontal, parietal, or vertex areas. There may also be pruritus and trichodynia.[2]
The panel recommends that the following aspects should be covered in history by asking specific questions:
Genetic background and hormones: History of hair loss among relatives from maternal and paternal sides should be asked for
Metabolic syndrome: It can have significant links with male-pattern hair loss
Androgen sensitivity: In women, a history of polycystic ovary disease should be considered
Protein powder intake: The patient should be asked about intake of pre- and post-workout protein shakes, such as powders containing whey isolates. These products are known to contain anabolic steroids
Other contributing factors that need to be enquired are: age of onset, disease progression, and smoking. The first two are important clues to differentiate between TE and AGA.
Consensus point 1:
“All patients with suspected AGA must be subjected to a detailed history-taking exercise and asked direct questions about the age of onset of hair fall, a history of hair fall among relatives (both paternal and maternal), medical conditions such as metabolic syndrome and insulin resistance, intake of anabolic steroids in the form of pure whey isolates or protein shakes, and smoking habits.”
EXAMINATION
According to the panel, history and pattern of hair loss are usually sufficient to make a diagnosis, with the pattern being the telltale sign. In women, widening of the hair parting should be ascertained. Different part width in the affected area and normal part width in the unaffected area reveal part width anisotrichosis. In males, baldness is evident in the frontotemporal region. The panel noted that in some patients, chronic alopecia areata incognita may occur in a patterned distribution; which should be differentiated by performing a trichoscopy. In addition, the panel pointed out that most patients of AGA can have spikes of hair loss throughout the progressive period.
In the view of the panel, clinical tests such as hair-pull test, trichoscopy, and dermoscopy may help in the diagnosis. Dermoscopy expresses yellow dots and variable diameter of the hair shafts (anisotrichosis). Perifollicular scaling indicates scarring alopecia, not AGA. A hair-pull test may be performed to diagnose coexisting TE. It would also be useful to check the terminal-to-vellus hair ratio.
Consensus key point 2
“A good history and clinical examination of the scalp for pattern of hair loss usually suffice to arrive at a diagnosis. Additional tests such as the hair-pull test, trichoscopy, and dermoscopy, and checking the terminal to vellus hair ratio, perifollicular scaling, and variation in thickness may also help.”
LABORATORY INVESTIGATIONS
The expert panel concurred that laboratory investigations are usually not needed in AGA. In males, the diagnosis is chiefly based on history and clinical examination. On the other hand, women with pattern hair loss may be investigated for testosterone, DHEAS (Dehydroepiandrosterone sulfate), insulin, and prolactin levels. Thus, hormonal and nutritional assessments form the basis of investigation. If coexisting TE is suspected, appropriate investigations should be done to determine the underlying cause.
Scalp biopsy is not routinely recommended in AGA because of its invasive nature.[2] The panel concluded that punch biopsy may be performed if deemed relevant by the clinician. In such cases, transverse and longitudinal sections of biopsy can be taken. Biopsy is informative for alopecia areata or lichen planus.
Consensus key point 3
“Laboratory investigations are usually not needed in AGA, especially in males. Females, however, may be investigated to rule out any underlying condition. Scalp biopsy may be done if required to clear any doubt.”
TREATMENT
Counseling
Counseling is required to address the problems of lowered self-esteem and lowered quality of life, particularly in women. Psychotherapy and anxiolytic therapy may also be considered in extreme cases.[7]
Nutritional supplementation
There is no clear cut evidence to support the use of oral supplementation of amino acids, biotin, zinc, and other micronutrients in hair loss of any origin.[7]
While the expert panel agreed that the role of nutritional supplements is limited in AGA compared to TE, they may be prescribed in case of abnormally high hair loss in AGA patients or in cases of TE or malnutrition. Nutritional supplements rich in amino acids can also be prescribed along with minoxidil, probably for 3–4 months, while initiating therapy. Amino acids, trace elements (Cu, Zn, Iron, etc.), and vitamins, including biotin, are considered to be beneficial. According to the panel, saw palmetto is thought to have similar effects as finasteride but lacks good quality clinical data to prove its efficacy. Similarly, data supporting the use of grape seed extracts, green tea, and proanthocyanins are also lacking.
MEDICAL TREATMENT
Minoxidil
The panel agreed that minoxidil remains the mainstay of therapy for AGA in men. According to the expert panel, minoxidil may also be prescribed in female pattern hair loss (FPHL), but counseling about the possibility of hypertrichosis must be given. Proper instructions on the usage of minoxidil should be provided by the clinician. The panel concurred that combining minoxidil with topical preparations such as procapil, capexil, aminexil, and others may have additive effects, but supporting evidence are lacking.
5-alpha reductase inhibitors
The expert panel agreed that minoxidil and finasteride are the approved drugs for hair loss treatment. Finasteride 1 mg shows better results than minoxidil with regard to regrowth of hair. Finasteride decreases the median scalp DHT levels as indicated in the treatment of AGA in men.
The panel further recommended that finasteride should be given for at least 6–12 months. But if it is well tolerated and shows good results, it may be used for longer periods. The drug should be used daily and patients' counseled about the side effects. In case of anxious patients, 1 mg finasteride may be given on alternate days. The response to treatment should be assessed after 6 months, though in some patients, it may take up to 12 months to become apparent.[2]
Since finasteride prevents the rise in prostate-specific antigen (PSA) levels and masks laboratory evidence of prostate carcinoma or benign prostate hyperplasia, the panel recommended that in patients aged >40 years and baseline PSA level should be measured before prescribing finasteride.
The panel noted that finasteride is not approved for FPHL and is contraindicated in women of reproductive age, due to its teratogenic effects if it has to be used in women, the dosage should be 5 mg and a washout period of minimum 3 months should elapse before use. Other anti-androgens such as spironolactone may be considered, the panel suggested.
Consensus key point 4
“Nutritional supplements may be prescribed in case of abnormally high hair loss, TE, or malnutrition. Otherwise, minoxidil remains the mainstay of therapy for male AGA. It may also be prescribed in FPHL with proper counseling. Finasteride 1 mg shows better results than minoxidil with regard to hair regrowth. Platelet-rich plasma (PRP) therapy can be used but only as an adjuvant to minoxidil/finasteride, and not as monotherapy.”
Hormonal treatment
Hormonal therapy, such as use of anti-androgens in male AGA, has not been found to be very effective. The only evidence-based indication is the use of cyproterone acetate in female patients with clinical and biochemical evidence of hyperandrogenism.[2]
Platelet-rich plasma
PRP, a new treatment modality, is an autologous preparation of plasma with a high concentration of platelets. It contains various growth factors and cytokines that improve the body's inherent capacity to repair and regenerate. It has been used for treating acne scars, nonhealing wounds, hair loss, and enhancing fat graft survival.[8]
The expert panel was of the view that patient selection is crucial in PRP; the procedure should not be prescribed for all patients with AGA. In hair transplant, PRP can be a good holding solution for the grafts causing no harm to patients. However, the panel concurred that it is unsustainable in the long term and can be used for a maximum 6 months. The panel recommended that PRP should not be used as monotherapy, but as an adjuvant to minoxidil/finasteride. The mechanism of PRP therapy involves proliferation of dermal papilla cells induced by the growth factors of the activated PRP. The main disadvantages of PRP are pain during the procedure and an unsustainable schedule due to reversible effects.
Surgery
Hair transplantation
Patient selection for hair transplantation: According to standard guidelines of care,[9] hair transplantation can be done in any person with pattern hair loss, with good donor area, who is in good general health and has reasonable expectations. However, one should exercise caution in the following cases:
Young patients with early, evolving alopecia
Patients with Norwood grade VI or VII with poor hair density.
The expert panel opined that counseling is very important in patients undergoing hair transplantation. Criteria to be considered for patients who require hair transplantation include:
Grade 3 Norwood classification
Stable hair loss that is not rapidly progressive
Failure of adequate medical treatment
If age <25, transplant should be done only in cases of extensive baldness; if age >25 years with grade 3 Norwood's classification, transplant may be considered
Bitemporal hair loss or frontal hairline baldness
In female patients, transplantation may be considered only after adequate trial of medical treatment, with proper investigations to identify the cause.
FOLLICULAR UNIT TRANSPLANTATION VERSUS FOLLICULAR UNIT EXTRACTION
Hair transplant procedures are of two types: follicular unit transplantation (FUT/Strip) and follicular unit extraction (FUE). In FUT/strip, a strip of tissue is removed from the donor area in the back and sides of the scalp, from which individual follicular units are removed by stereomicroscopic dissection. The wound edges are then closed, leaving a single, fine scar. In the FUE method, small circular incisions are made over a considerably larger donor area, from which hairs are harvested, leaving small, round, light skin-colored scars.[10]
Comparing the two procedures, the panel came up with the following conclusions:
Follicular unit transplantation
It can cover larger areas as it provides larger number of grafts
It is currently the gold standard for dermatologists
It provides good and fine quality grafts
It is significantly more painful
It is inconvenient for the patient because of the linear scar
Only the central occipital area is the donor area
Grafts extracted through FUT have better survival rate due to lesser transaction risk.
Follicular unit extraction
It is easier to perform
It enables rapid healing of the donor area (in 1–2 days)
It does not cause scarring, is relatively painless, is ideal for patients who want short hair, and enables early resumption of daily activities
It requires a larger donor area to be selected
It is more time-consuming as compared to FUT.
Both techniques have their own merits and demerits. Thus, a treating physician needs to have a better clinical judgment to choose between the two procedures on a case-to-case basis. However, a combination of both can prove to be good for some patients.
Consensus key point 5
“Counselling is very important in patients undergoing hair transplant. Follicular Unit Transplant (FUT) is currently the gold standard treatment, but it is up to the treating physician to choose between FUT and FUE. Some patients may benefit from a combination of both.”
Pre- and post-transplant treatment
According to the panel, all patients seeking hair transplantation should be properly counseled before the procedure. Minoxidil treatment should be stopped 15 days before transplant as it is a vasodilator and may aggravate bleeding tendency. If the patient is taking anticoagulant and antiplatelet drugs, the physician's opinion should be taken on titration of medication. Posttransplantation, medical therapy should be continued as per the discretion of the treating physician.
CONCLUSION
This article highlights the effective management of AGA contributed by experts' opinion on evidence-based management practice.
Financial support and sponsorship
Nil.
Conflicts of interest
The expert meetings were done in association with Abbott Healthcare Pvt. Ltd. The views expressed and discussed in the meetings and stated in this consensus article are the views of the authors and not of Abbott Healthcare Pvt. Ltd.
Acknowledgment
The work of compilation and articulation of the consensus viewpoints of the contributors was supported by Scientimed Solutions Pvt. Ltd.
REFERENCES
- 1.Blumeyer A, Tosti A, Messenger A, Reygagne P, Del Marmol V, Spuls PI, et al. Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men. J Dtsch Dermatol Ges. 2011;9(Suppl 6):S1–57. doi: 10.1111/j.1610-0379.2011.07802.x. [DOI] [PubMed] [Google Scholar]
- 2.Kaliyadan F, Nambiar A, Vijayaraghavan S. Androgenetic alopecia: An update. Indian J Dermatol Venereol Leprol. 2013;79:613–25. doi: 10.4103/0378-6323.116730. [DOI] [PubMed] [Google Scholar]
- 3.Clarke P. Male baldness. Aust Fam Physician. 2016;45:186–8. [PubMed] [Google Scholar]
- 4.Kanti V, Messenger A, Dobos G, Reygagne P, Finner A, Blumeyer A, et al. Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men-short version. J Eur Acad Dermatol Venereol. 2018;32:11–22. doi: 10.1111/jdv.14624. [DOI] [PubMed] [Google Scholar]
- 5.Feinstein RP. Androgenetic Alopecia. [Last accessed on 2018 Mar 01]. Available from: https://www.emedicine.medscape.com/article/1070167-overview#showall .
- 6.Wolff H, Fischer TW, Blume-Peytavi U. The diagnosis and treatment of hair and scalp diseases. Dtsch Arztebl Int. 2016;113:377–86. doi: 10.3238/arztebl.2016.0377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singal A, Sonthalia S, Verma P. Female pattern hair loss. Indian J Dermatol Venereol Leprol. 2013;79:626–40. doi: 10.4103/0378-6323.116732. [DOI] [PubMed] [Google Scholar]
- 8.Cervantes J, Perper M, Wong LL, Eber AE, Villasante Fricke AC, Wikramanayake TC, et al. Effectiveness of platelet-rich plasma for androgenetic alopecia: A review of the literature. Skin Appendage Disord. 2018;4:1–11. doi: 10.1159/000477671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patwardhan N, Mysore V. Dermatosurgery Task Force. Hair transplantation: Standard guidelines of care. Indian J Dermatol Venereol Leprol. 2008;74(Suppl 1):S46–53. [PubMed] [Google Scholar]
- 10.FUE vs. FUT Hair Transplants: Overview. [Last accessed on 2018 Mar 04]. Available from: https://www.bernsteinmedical.com/hair-transplant/fue/fue-vs-fut/


