Abstract
Introduction:
Despite the accumulating Canadian evidence regarding the relations between urban form and health behaviours, less is known about the associations between urban form and health conditions. Our study aim was to undertake a scoping review to synthesize evidence from quantitative studies that have investigated the relationship between built environment and chronic health conditions, self-reported health and quality of life, and injuries in the Canadian adult population.
Methods:
From January to March 2017, we searched 13 databases to identify peer-reviewed quantitative studies from all years that estimated associations between the objectivelymeasured built environment and health conditions in Canadian adults. Studies undertaken within urban settings only were included. Relevant studies were catalogued and synthesized in relation to their reported study and sample design, and health outcome and built environment features.
Results:
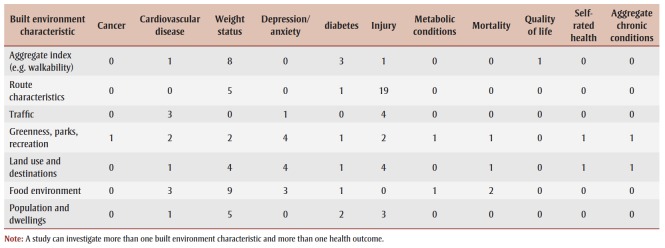
Fifty-five articles met the inclusion criteria, 52 of which were published after 2008. Most single province studies were undertaken in Ontario (n = 22), Quebec (n = 12), and Alberta (n = 7). Associations between the built environment features and 11 broad health outcomes emerged from the review, including injury (n = 19), weight status (n = 19), cardiovascular disease (n = 5), depression/anxiety (n = 5), diabetes (n = 5), mortality (n = 4), self-rated health (n = 2), chronic conditions (n = 2), metabolic conditions (n = 2), quality of life (n = 1), and cancer (n = 1). Consistent evidence for associations between aggregate built environment indicators (e.g., walkability) and diabetes and weight and between connectivity and route features (e.g., transportation route, trails, pathways, sidewalks, street pattern, intersections, route characteristics) and injury were found. Evidence for greenspace, parks and recreation features impacting multiple health outcomes was also found.
Conclusion:
Within the Canadian context, the built environment is associated with a range of chronic health conditions and injury in adults, but the evidence to date has limitations. More research on the built environment and health incorporating rigorous study designs are needed to provide stronger causal evidence to inform policy and practice.
Keywords: disease, neighbourhood, built environment, injury, health, mental health
Highlights
The most frequently reported associations among Canadian studies on urban form and health outcomes were related to injury and weight status.
Not all provinces and territories were represented in this review, with much of the evidence coming from studies in Ontario, Quebec, and Alberta.
Objectively-measured aggregate built environment indicators, connectivity and route features, destinations, food environment, population density, and greenspace, parks and recreation features are associated with a range of modifiable health conditions and injury.
This scoping review identifies that more Canadian research, with rigorous designs that allow for causal inference, is required to inform policy and practice.
Introduction
The World Health Organization’s 1986 Ottawa Charter for Health Promotion acknowledged the need to create healthsupportive environments.1 Health-supportive environments, whether on local or global scales are responsive to changes in energy production, technology, work, and urbanization, and positively support interrelationships between the environment and human health.1 Creating such environments continues to be an important strategy for reducing the chronic disease risk and promoting health and wellbeing in Canada and globally.2,3 Since the early 20th century, urban planning strategies in Canadian cities have contributed to poor health due to the rapid geographic expansion of metropolitan areas resulting in increased intra- and inter-neighbourhood distances between homes and destinations, lower city and neighbourhood population densities, disconnected regional and neighbourhood street patterns, and scattered suburban neighbourhood development. 4 Previous and often contemporary urban planning strategies continue to negatively impact transportation walking and cycling, encourage dependence on private motorized transportation, and contribute to increased obesity, pedestrian injury, and chronic disease risk.4
Neighbourhoods, which incorporate interrelated urban form and social characteristics, are important settings that positively and negatively influence the health and wellbeing of individuals and populations. Neighbourhood urban form or built environment – the human-modified physical surroundings and features such as parks, streets, buildings, destinations and land uses, connectivity, density, sidewalks and paths, lighting, aesthetics, and architecture – supports physical activity,5,6 sedentary behaviour,7,8 diet,9 and socializing.10,11 Informed by evidence, Northridge et al.’s12 conceptual framework proposed links between urban form and population health, in particular positing land use (e.g., industrial, residential, mixed or single use), services (e.g., shopping, banking), transportation systems, public resources (e.g., parks), zoning regulations, and buildings as important broadlydefined community level determinants. Similarly, Frank et al.’s13 conceptual framework links land use patterns (i.e., arrangement of destinations, mix of uses, distribution of parks and recreational opportunities), urban design characteristics (i.e., micro-scale characteristics influencing safety, aesthetics, friendliness, and vibrancy), and transportation systems (i.e., road, sidewalk/pathway and other transportation infrastructure, connections, and linkages) to the public health of communities and cities.
Systematic review findings, which are often based on a synthesis of studies from multiples countries, provide some evidence for associations between a variety of built environment features (e.g., food environment, walkability, greenery) and weight status,14,15 blood pressure,15 metabolic syndrome,15 diabetes,15,16 and major cardiovascular outcomes such as myocardial infarctions, coronary heart disease, congestive heart failure and stroke.15Further, built environment features are associated with motor vehicle-related bicyclist (e.g., presence of bike routes, lanes, and paths)17 or pedestrian (e.g., traffic-calming infrastructure and roadway design)18,19 injuries among adults, and associated with the risk of outdoor falls and fall-related injuries in older adults (e.g., perceived personal safety and neighbourhood disorder20,21 and sidewalk quality21). In addition to associations with physical health, evidence also suggests that built environment features are associated with mental health (e.g., depression, anxiety, and distress)11,22 and intervening variables such as stress, social support and social capital.10,11,22-24 The built environment can affect the subjective experience of residents, for example through perceptions of safety and the stress process, which in turn can result in physical and mental health consequences.22
In Canada, approximately 34% of adults report having at least one of the five major chronic diseases (i.e., cancer, cardiovascular diseases, diabetes, chronic respiratory diseases, and mood/anxiety disorders).25 Among those 12 years and older, at least one-quarter report less than very good mental health and approximately 13% report having a diagnosed mood or anxiety disorder.25 Thus, a better understanding regarding the nature of the neighbourhood built environment for promoting health and wellbeing and preventing multiple chronic diseases in Canada is needed. Previous systematic reviews on built environment and health typically do not stratify their findings by country or geography, and the findings are often weighted towards US and European studies, which despite being informative, lack specificity, and potentially some relevance for aiding local decision-making. The climatic, cultural, political, legislative, and healthcare system differences between countries (among other differences) suggest that synthesizing findings from studies undertaken within a single country might be a better strategy for informing local urban planning strategies and policies that have the potential to impact health. While some findings support the generalizability of built environment and physical activity associations between countries,26,27 country and regional differences in relations between built environment and rates of bicycling,28-30 bicycling injuries and crashes,17 transportation walking,30 and obesity31 found elsewhere exemplify the need for synthesis of local evidence. Country-specific literature reviews on the association between built environment and different health outcomes are scarce.32
Generating and sharing local evidence (e.g., via literature reviews) with stakeholders, practitioners, and decision-makers is identified as one of several vital approaches needed for the development and implementation of land use and transportation policies for a health-supportive environment within the Canadian context. 33 Thus, the aim of our study was to undertake a scoping review to synthesize and map evidence from quantitative studies that have investigated the built environment and its associations with modifiable health conditions, self-reported health, quality of life, and injuries in the Canadian adult population. Evidence from this review is intended to inform the direction of the Canadian research agenda by identifying knowledge gaps and to consolidate findings from existing studies investigating associations between urban form and health that could inform local policy and practice.
Methods
Overview
Our scoping review approach was informed by the steps proposed by Arksey and O’Malley.34 Our review: 1) included a comprehensive systematic search of the peer-reviewed literature to identify healthfocussed quantitative studies that included an objective measure of the built environment; 2) catalogued and mapped study characteristics (types of built environment exposures, types of chronic disease and injury outcomes, study populations, methods, geographical contexts, journal types, funding sources, and findings); 3) summarized the relationships between the built environment and health status and injury (e.g., cardiovascular-related diseases, diabetes, depression, weight status, quality of life, and injury); and 4) identified knowledge and evidence gaps.
Search strategy
In consultation with a Health Sciences librarian, we developed a preliminary list of search terms pertaining to built environment, health outcomes, and the Canadian context and identified relevant databases informed by the Public Health Agency of Canada’s Chronic Disease Indicator Framework (CDIF).35 This framework was developed as a reference tool for practitioners and policymakers to inform chronic disease surveillance in Canada. Despite updates to the framework— including the removal of injury as an indicator25—we report on injury in this scoping review. Studies estimating associations between the built environment and health behaviours (e.g., physical activity, diet, sedentary behaviour, socializing) were not included.
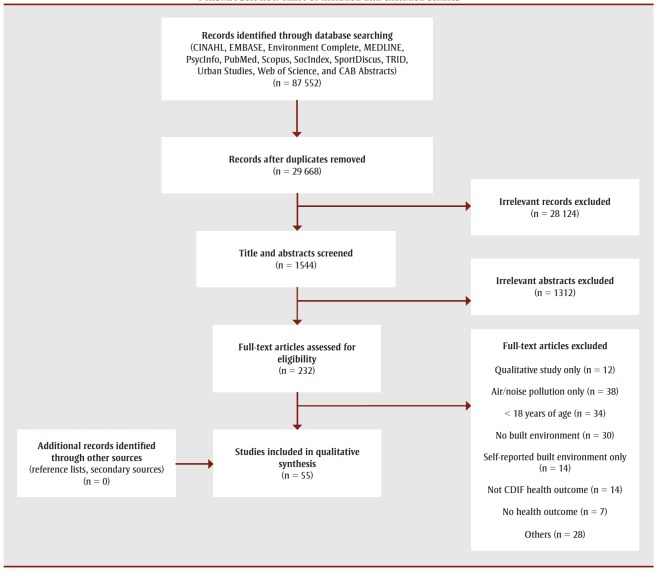
Thirteen scientific databases (CINAHL, EMBASE, Environment Complete, MEDLINE, PsycInfo, PubMed, Scopus, SocIndex, SportDiscus, TRID, Urban Studies, Web of Science, and CAB Abstracts) were identified as likely indexing journals and articles relevant for our review. A pilot test of our search strategy using Medline alone yielded over 80 000 titles. A preliminary check of these titles suggested that the initially included term “nature” was contributing many irrelevant titles, and thus this term was excluded. We also added “suburb” as a built environment term. A trained research assistant (RL) undertook the database search in March 2017 (Table 1). Separate title, abstract, and keywords searches were conducted for the built environment (n = 28), health (n = 29), and then Canadian geography (n = 14) terms. The results for the three separate search strings were combined to identify relevant titles. The database search resulted in 87 552 titles. These titles and abstracts were imported into the Endnote reference management software for further processing. After removal of duplicate titles and screening of title relevance, 1544 remained for full abstract screening. Following the detailed abstract screening and removal of conference proceedings, book reviews, commentaries, editorials, and non-peer reviewed articles, 232 titles were identified as relevant to undergo fulltext assessment (i.e., whereby the abstract mentioned both the built environment and at least one health outcome).
Table 1. Study count by health outcomes and type of built environment characteristics examined.
RL and GRM independently reviewed the 232 full-text articles (percent of overall agreement = 84.7%; kappa = 0.68) against our review’s inclusion criteria. A consensus was reached for those articles where RL and GRM disagreed regarding their inclusion. Studies included in the review were primary quantitative or mixed-methods studies, included adults (age ≥ 18 years) from a Canadian geographical location, and estimated and reported an association between an objective measure of the built environment (derived from geographical information systems or virtual or in-person audits) or neighbourhood type (e.g., expert-determined) and at least one relevant self-reported, clinically assessed, or administrative data determined outcome associated with either cancer, cardiovascular disease, aggregate chronic conditions, depression/anxiety, diabetes, injury, metabolic conditions, mortality, quality of life, self-rated health, and weight status.
Studies that recruited a rural sample only or compared rural to urban only, examined air or noise pollution as an exposure only, included road proximity or traffic volume as a proxy for pollution exposure, included a self-reported measure of the built environment only, or exclusively included children and/or adolescents were excluded. Upon checking the analysis and results of included studies, those which did not adjust for any covariates (i.e., via statistical controls, matching, or stratification) in estimated associations between the built environment and health were also excluded. The reference lists of articles meeting the inclusion criteria, similar literature reviews, and key Canadian peerreviewed journals (Canadian Journal of Public Health, Health Promotion and Chronic Disease Prevention in Canada, Canadian Medical Association Journal, and Canadian Journal of Urban Research) were also screened for relevant articles. After full-text assessment, 55 were included in the review and underwent data extraction and synthesis. We applied the PRISMAScR checklist36 to guide reporting of article inclusion and exclusion for our scoping review and to improve rigor and replicability (Figure 1).
Figure 1. PRISMA-ScR flow chart of included and excluded studies.
Data extraction and synthesis
Relevant data extracted from reviewed articles included author, first-author institution, publication year, study design, geographical location, sample design, basic sample characteristics, data collection and measures (built environment and health), findings, and funding or sponsor details. One reviewer (RL) led article data extraction, tabulation, and synthesis, with a second (AB) and a third reviewer (GRM) tasked with ensuring the accuracy of the data extracted and summary of findings reported. We extracted and synthesized statistically significant positive and negative associations (based on either reported p-values or confidence intervals) from the most fully or final covariate-adjusted (including statistical controls, matching, or stratification) model reported in the study. Extracted article data were entered and organized in an electronic database (Microsoft Excel). Summaries of article findings were broadly categorized based on the eleven health outcomes informed by the CDIF and the broad groupings of conceptually similar built characteristics informed by previous frameworks.12,13 We undertook a narrative qualitative description of study differences and similarities in terms of their types of built environment exposures, types of chronic disease and injury outcomes, study populations, methods, geographical contexts, journal types, funding sources, and findings.
Results
Study contexts
Fifty-five articles were included in this review. Articles were published between 1998 and 2017, although most (n = 52) were published after 2008. Eleven articles included national or multi-province samples (e.g., Ontario and British Columbia). Most single province studies were undertaken in Ontario (n = 22) followed by Quebec (n = 12), Alberta (n = 7), British Columbia (n = 2), and Nova Scotia (n = 1). Notably, other Canadian provinces and territories were not represented in the included articles. Forty-six studies declared some type of research funding (program, project, or salary support), with most studies supported by funding from Canadian Institutes of Health Research (n = 32), provincial government (n = 26), national government (n = 13), and the Heart and Stroke Foundation (n = 11). All but 5 articles were principal authored by someone affiliated with a Canadian university, institute or other organization. Based on first-author affiliations, affiliation from which multiple articles were published included McGill University (n = 8), Li Ka Shing Knowledge Institute, Toronto (n = 5), University of Calgary (n = 4),University of Alberta (n = 3), Child Health Evaluative Sciences, Toronto (n = 3), Institute for Clinical Evaluative Sciences, Toronto (n = 3), University of Toronto (n = 3), University of British Columbia (n = 3), Université de Montreal (n = 3), University of Ottawa (n = 2), Simon Fraser University (n = 2), and University of Western Ontario (n = 2). Studies were typically published in international and national public health or medical journals (e.g., British Medical Journal, BMC Public Health, Health Reports, Canadian Journal of Public Health, American Journal of Preventive Medicine, American Journal of Public Health) environment and health journals (e.g., Health and Place, Social Science and Medicine, Journal of Environmental and Public Health, International Journal of Environmental Research and Public Health, Journal of Epidemiology and Community Health, Geospatial Health), injury-related journals (e.g., Injury Prevention, Accident Analysis and Prevention, Traffic Injury Prevention), or land use or transportation journals (e.g., Land Use Policy, Transportation Research Board).
Study and sample design
Cross-sectional studies (individual-level and ecological) were the most common study type (n = 36) with the remainder including a mix of prospective and retrospective cohort, longitudinal, case-control, casecrossover, time series, and quasi-experimental study designs. Twenty-nine studies reported using a probability sampling strategy to recruit participants. Among studies that reported sample size, samples ranged from 160 to over 1.4 million. Further, among studies providing response rates, rates were as low as 8% and as high as 94.4%. All but one study included men and women. Most studies included samples aged 18 to 64 years, although three included samples aged 30 to 64 years, and one study included a sample aged 60 years and older.
Twenty-seven studies included self-reported health outcomes alone or in combination with a clinician-diagnosed, administrative or other objective measure of health. Twenty-eight studies reported on clinician- diagnosed or administrative database reported health outcomes only. Among those studies reporting use of existing data, nineteen studies undertook secondary analysis using the National Population Health Survey or the Canadian Community Health Survey, ten studies used ambulance dispatch or hospital data, and the remainder used other sources (e.g., traffic data, police reports, disease registries and surveillance databases, municipal, provincial and other administrative databases) (summary of findings available on request).
Study approaches for measuring the health outcomes varied for injury (n = 19; 18 with objective and 1 with self-reported injury), weight status (n = 19; all selfreported), cardiovascular disease (n = 5; 3 with objective and 2 self-reported CVD), depression/anxiety (n = 5; all selfreported), diabetes (n = 5; all objectively measured), mortality (n = 4; all objectively measured), self-rated health (n = 2; all self-reported), metabolic conditions (n = 2; 1 with objectively measured and 1 self-reported conditions), quality of life (n = 1; self-reported), cancer (n = 1, objectively measured), and aggregate chronic conditions (n = 2; all self-reported). Two studies included “aggregate chronic conditions”, one combined cancer, migraines, asthma, and arthritis37 and another38 combined asthma, fibromyalgia, high blood pressure, migraines, chronic bronchitis, emphysema or chronic obstructive pulmonary disease, diabetes, heart disease, angina, cancer, ulcers, bowel disorders, and Alzheimer’s disease into a single health outcome, in addition to a separate measure of self-reported general health.
Measurement of urban form
Geographical information systems (GIS) with spatial databases represented the most common approach for estimating built environment characteristics (n = 37 studies), followed by use of Walk Score® (n = 4 studies), in-person or virtual (e.g., via Google Street View®) street audits (n = 4 studies), and other approaches (i.e., police reports, street classifications, census data). Studies evaluated the built environment characteristics at or within a specific distance of an intersection or collision site (e.g., between motor vehicle and pedestrian), along transportation routes and streets, within activity spaces (e.g., geographical areas estimated based on mobility, travel patterns, and origin and destination locations), within administrative boundaries (e.g., census tracts, dissemination areas or blocks, postal code polygons, neighbourhoods), and within researcher-defined buffers of various sizes (i.e., 150m to 1600m) and types (e.g., network, line-based, or radial) typically estimated in relation to a geo-located residential postal code or household address (summary of findings available on request).
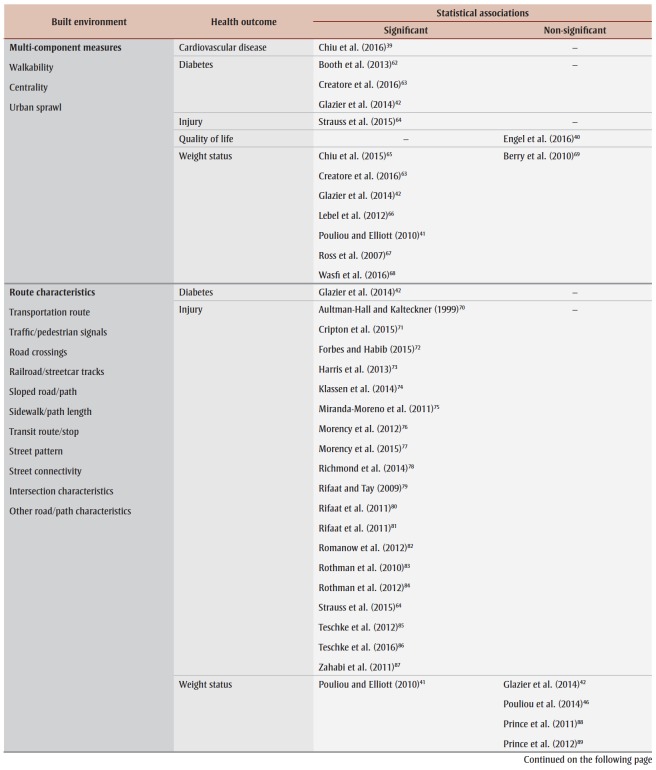
Aggregate-built environment indicators and health
There was consistent support for an association between aggregate or overall built environment indicators (e.g., walkability, Walk Scores®, centrality, and sprawl), diabetes and weight status (Table 2). One study also found an increase in walkability to be associated with a decreased risk of hypertension.39 All significant associations were in the expected direction (summary of findings available on request). The one study estimating the relation between walkability and quality of life reported a statistically non-significant association only.40 No studies reviewed estimated associations between aggregate built environment indicators and depression/ anxiety, self-rated health, cancer, metabolic or aggregate chronic conditions, or mortality.
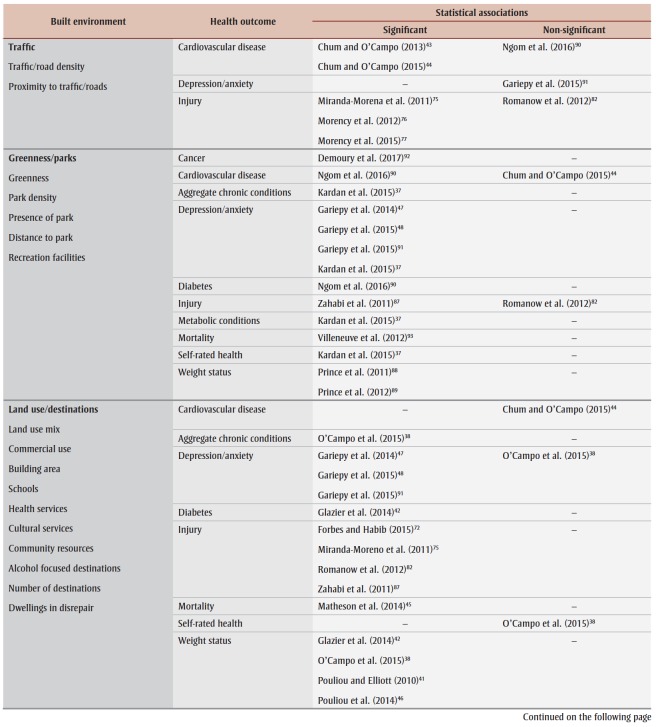
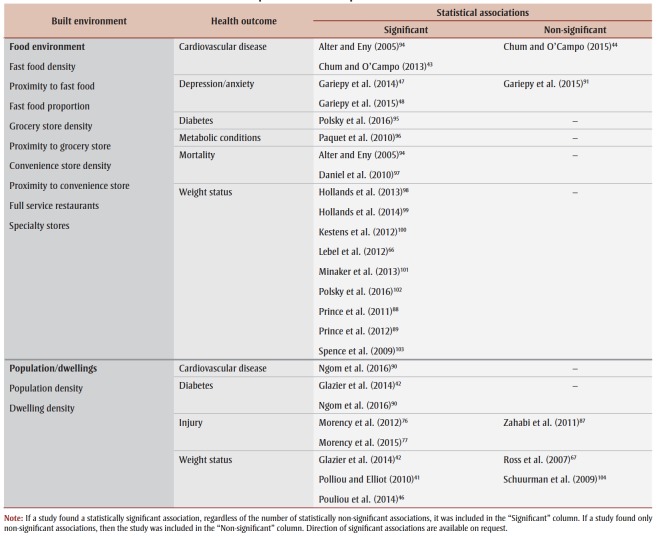
Table 2. Associations between objectively-measured built environment variables and health outcomes reported in Canadian quantitative studies published 1998-2017.
Connectivity and route features and health
There was consistent evidence for an association between connectivity and route features (e.g., transportation route, traffic and pedestrian signals, tracks, trails, pathways, and sidewalks, street pattern, connectivity and intersections, road and path characteristics) and injury (Table 2). Connectivity and route features both increased and decreased the risk of pedestrian and cyclist injury (summary of findings available on request). One study found higher street connectivity significantly associated with lower weight status;41 however, four other studies reported no significant association. Higher street connectivity was also significantly associated with a decrease in diabetes risk in one study.42 Among the studies reviewed, none estimated associations between connectivity or route features and cardiovascular conditions, metabolic and aggregate chronic conditions, cancer, depression/ anxiety, self-rated health, or quality of life.
Traffic features and health
Five studies found significant associations between traffic features (e.g., traffic and road density, proximity to traffic) and cardiovascular conditions and injury (Table 2). For example, Chum and colleagues43,44 found proximity to traffic to be positively associated with self-reported cardiovascular disease. Three studies also reported only statistically non-significant associations between traffic features and objectively determined cardiovascular disease, injury, and self-reported depression. Among the reviewed studies, associations between traffic features and other health outcomes were not estimated.
Green space, parks, and recreation features and health
Greenspace, parks and recreation features (e.g., park density, park proximity) were significantly associated with a range of health outcomes including cancer, depression/ anxiety, metabolic conditions, selfrated health, weight status, cardiovascular related disease outcomes, aggregate chronic conditions, diabetes, injury, and mortality (Table 2). Notably, the direction of association (protective vs. risk factor) between greenspace, parks, and recreational facilities was mixed (summary of findings available on request). Among the studies that investigated greenspace and park features, none estimated the association with quality of life.
Land use and destination features and health
Non-food related land use and destination features (e.g., mix and proximity to general and specific land uses and destinations) were significantly associated with a range of health outcomes including aggregate chronic conditions, depression/anxiety, diabetes, injury, weight status, and mortality (Table 2). For example, increased access to alcohol outlets (among men and women) and cheque cashing destinations (among men only) increased the likelihood of allcause mortality,45 land use mix was associated with better weight status,41,46 and access to health and cultural services was associated with lower odds of self-reported depression.47,48 One study reported statistically non-significant associations between community resources and depression, anxiety, and self-rated health, but found significant associations between community resources and aggregate chronic conditions and weight status38 (summary of findings available on request).
Food environment features and health
Food environment features, such as proximity to and density of healthy and unhealthy food destinations, were significantly associated with a range of health outcomes (Table 2). Proximity and access to fast food was associated with mortality, depression, cardiovascular conditions, and weight status. Access and proximity to grocery or healthy food stores were supportive of health (e.g., depression and weight status). Two studies only found no association between the food environment and cardiovascular conditions and anxiety and depression. Among the reviewed food environment studies, none investigated cancer, self-reported health, quality of life, aggregate chronic conditions, or injury.
Population and dwelling density and health
Eight studies reported significant associations between population and dwelling density and health outcomes (i.e., cardiovascular conditions, diabetes, injury, and weight status). Despite this, statistically non-significant associations between population/ dwelling density and injury and weight status were also found (Table 2). None of the included population/dwelling density studies estimated associations with cancer, depression/anxiety, self-rated health, quality of life, mortality, metabolic or aggregate chronic conditions.
Discussion
Our scoping review findings support those of previous systematic reviews that suggest urban form is associated with weight status,14,15 blood pressure,15 metabolic syndrome, 15 diabetes,15,16 cardiovascular outcomes, 15 injury risk17-19 and mental health.11,22 Built characteristics related to land use patterns, urban design features, and transportation systems were found to be important correlates of chronic health conditions and injury in the Canadian context. Moreover, among Canadian studies on urban form and health, most have focussed on injury (primarily transportrelated) and weight status outcomes. This focus may reflect the significant preventable burden both transport-related injury49 and excess weight50 place on the Canadian healthcare system. Despite some evidence elsewhere showing relations between the urban form or built environment and falls in the older adult population,20,21 this evidence appears to be scant within the Canadian context. There is a recognized need for evidence in relation to the impact of urban form on the health of older Canadian adults, including the enablers and barriers to ‘aging in place’.51,52 This context-specific understanding of the relationship between urban form and health is needed to develop and expand policy and interventions that can promote wellbeing and accommodate the health and social needs of adults, including infrastructure that allows adults to remain mobile and active across the life-span.53
Our study is novel, as previously no single source had attempted to systematically review and articulate all Canadian evidence on urban form and chronic health outcomes and injury. Thus, the findings of this review are specific and relevant to the current Canadian research and policy context. As suggested from our review findings, there are built environment features that might be important for specific health outcomes that have yet to be studied. For instance, published studies have not provided evidence about the associations between objectively-measured walkability indices and mental health and pedestrian or cyclist injury outcomes, although components of walkability have been found to be important correlates. Similarly, there is still a range of built environment features (e.g., aesthetics and appeal, personal safety and incivilities) to be examined even for the most investigated health outcomes in this literature (e.g., weight status, injury, and cardiovascular outcomes). The findings from the review suggest more research, especially longitudinal and quasi-experiment studies, is needed in relation to urban form, mental health and quality of life. Despite its subjectivity, health related quality of life (HRQOL) is strongly associated with the type, number, and pattern of physical and mental health conditions54,55 as well as mortality risk.56 Only two Canadian studies have examined the relationship between quality of life and urban form; however, because HRQOL summarises a wide range of health states into a comprehensive measure, future research on the built environment and its impact on HRQOL would be useful.
Based on the published scientific literature, there has been a steady increase in Canadian studies on urban form and health outcomes since 2008. Notably, not all provinces or territories were represented in the studies reviewed and those included were heterogeneous in terms of their methodology, thus making direct comparison of results impossible. While this increase in the quantity of studies is encouraging, more causal evidence is needed to better inform local policy and urban planning decisions in all Canadian provinces and territories. Within the Canadian context, associations between some built environment characteristics and health outcomes have been established; however, some of this evidence is mixed. Further, the few studies published reporting statistically non-significant associations only could suggest publication bias, thus overemphasizing the apparent impact of the built environment might have on health. Notably, statistical significance is affected by other factors (e.g., aggregation of data, delay between exposure and health outcome, reliability of measures, sample exposure and outcome variation) and may not necessarily mean no actual association exists. Future highquality primary studies and systematic reviews investigating urban form and health should consider in more detail (beyond this scoping review) the reasons for these non-significant associations. Most of the evidence to date has been derived from observational, primarily cross-sectional, studies that allow only weak causal inferences to be drawn. Given the large amount of resources and time and the potential short- and long-term social and economic impact associated with urban planning decisions, rigorous evidence from scientifically robust study designs (e.g., longitudinal studies, natural and quasi-experiments, cluster randomized designs where feasible) is desperately needed. Increasing the use of existing Canadian longitudinal data sources, such as the National Population Health Survey (1994 to 2010)57 and the Canadian Longitudinal Study on Aging,58 and longitudinal linked health administrative data,59 can contribute to enhancing the evidence base in a timely manner. In addition to the mostly cross-sectional nature of the current Canadian evidence, studies in our review typically did not take into consideration the intensity and duration of built environment exposure needed to result in a clinically relevant influence on health.
We acknowledge several limitations with our review that impact the findings. Our scoping review allowed for a large body of evidence to be synthesized; however, given the breadth of urban form and health outcomes, we did not formally critique the scientific quality, and internal and external validity of individual studies— a strategy typically used in systematic reviews. The implicit aim of our scoping review was to identify knowledge trends and gaps that could inform future primary studies and systemic reviews and to provide an overview of the research on this topic. Our inclusion of published peer-review evidence only could mean that relevant, yet unpublished findings are missing from our review. Despite scanning the reference lists of the included studies to identify other additional sources, it is possible that peer-reviewed studies not indexed in our search databases may have been omitted. Several health studies were excluded as they did not include health outcomes in alignment with the CDIF.60 For example, one excluded study found associations between satellite-determined greenery (i.e., Normalized Difference Vegetation Index) and indicators of perinatal health (such as birth weight, likelihood of preterm birth).60 Hence, we acknowledge that the effect of the built environment on health likely goes beyond the specific health outcomes presented in this scoping review. Furthermore, our inclusion of studies that undertook steps to control for confounding could have resulted in the exclusion of relevant descriptive studies, including those exploring relations between spatial variation in urban form and health.
Conclusion
It is important for practitioners and policymakers to use the best available evidence. Evidence elsewhere demonstrating plausible pathways linking urban form with health (e.g., via physical activity, sedentary behaviour, diet, the stress process61 and social interactions)5-11 support our findings. Notably, not all statistically significant associations between the built environment and health outcomes were in an expected harm-reducing or health-promoting direction. Health promotion strategies might be required where urban form has some unavoidable negative impact on a health outcome. Our review findings show that in Canada, associations exist between urban form and health outcomes, but causal evidence is lacking.
Acknowledgements
Funding supporting this study was obtained from a makeCalgary Network pilot grant (University of Calgary), the Public Health Agency of Canada, and a Canadian Institutes for Health Research (CIHR) Foundations Scheme Grant. Gavin McCormack was supported by a CIHR New Investigator Award (MSH-130162). We appreciate the guidance provided by Lorraine Toews (Health Sciences Librarian, University of Calgary).
Conflicts of interest
Heather Orpana is affiliated with the Public Health Agency of Canada, which oversees the production and publication of the Health Promotion and Chronic Disease Prevention in Canada (HPCDPIC). Gavin McCormack and Heather Orpana are Associate Scientific Editors for HPCDPIC. Orpana and McCormack were blinded from the peer review process and editorial decision- making associated with the publication of this manuscript. The Public Health Agency of Canada provided funding support to undertake the scoping review. The authors declare there are no other conflicts of interest regarding the publication of this article.
Authors’ contributions and statement
GRM, NK, and JC conceived the study aim and overall design. All authors contributed to the method design and the review and interpretation of results. GRM, RL, and AB conducted the scoping review with input from NK, JC, HO, and SG. All authors contributed to the manuscript drafting and approved the final manuscript. The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- The Ottawa Charter for health promotion. Health Promotion International. 1986 [Google Scholar]
- Public Health Agency of Canada. Ottawa(ON): 2005. The Integrated Pan-Canadian Healthy Living Strategy [Internet] Available from: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/ipchls-spimmvs/pdf/ipchls-spimmvs-eng.pdf. [Google Scholar]
- Global strategy on diet, physical activity and health [Internet] WHO. 2004 Available from: http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf. [Google Scholar]
- Frumkin H, Frank L, Jackson R, et al. Island Press. Washington(USA): 2004. Urban sprawl and public health. [Google Scholar]
- Durand CP, Andalib M, Dunton GF, Wolch J, Pentz MA, et al. A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obes Rev. 2011;12((5)):e173–e82. doi: 10.1111/j.1467-789X.2010.00826.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack G, Shiell A, et al. In search of causality: a systematic review of the relationship between the built environment and physical activity among adults. Int J Behav Nutr Phys Act. 2011;8((1)):125–e82. doi: 10.1186/1479-5868-8-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Reed JL, McFetridge C, Tremblay MS, Reid RD, et al. Correlates of sedentary behaviour in adults: a systematic review. Obes Rev. 2013;18((8)):915–35. doi: 10.1111/obr.12529. [DOI] [PubMed] [Google Scholar]
- Owen N, Salmon J, Koohsari MJ, Turrell G, Giles-Corti B, et al. Sedentary behaviour and health: mapping environmental and social contexts to underpin chronic disease prevention. Br J Sports Med. 2014;48((3)):174–7. doi: 10.1136/bjsports-2013-093107. [DOI] [PubMed] [Google Scholar]
- Caspi CE, Sorensen G, Subramanian SV, Kawachi I, et al. The local food environment and diet: a systematic review. The local food environment and diet: a systematic review. Health & Place. 2012;18((5)):1172–87. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyden KM, et al. Social capital and the built environment: the importance of walkable neighborhoods. Am J Public Health. 2003;93((9)):1546–51. doi: 10.2105/ajph.93.9.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis J, Giles-Corti B, Wood L, Knuiman M, et al. Neighbourhood influences on mental health in master planned estates: a qualitative study of resident perspectives. Health Promot J Austr. 2014;25((3)):186–92. doi: 10.1071/HE14036. [DOI] [PubMed] [Google Scholar]
- Northridge M, Sclar E, Biswas P, et al. Sorting out the connections between the built environment and health: a conceptual framework for navigating pathways and planning healthy cities. J Urban Health. 2003;80((4)):556–68. doi: 10.1093/jurban/jtg064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank LD, Engelke PO, Schmid TL, et al. Island Press. Washington(USA): 2003. Health and community design. [Google Scholar]
- Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC, et al. The built environment and obesity. Epidemiol Rev. 2007;29((1)):129–43. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- Malambo P, Kengne AP, Villiers A, Lambert EV, Puoane T, et al. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLOS ONE. 2016;11((11)):e0166846–43. doi: 10.1371/journal.pone.0166846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dendup T, Feng X, Clingan S, Astell-Burt T, et al. Environmental risk factors for developing type 2 diabetes mellitus: a systematic review. Int J Environ Res Public Health. 2018 doi: 10.3390/ijerph15010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CC, Harris MA, Teschke K, Cripton PA, Winters M, et al. The impact of transportation infrastructure on bicycling injuries and crashes: a review of the literature. Environ Health. 2009 doi: 10.1186/1476-069X-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoker P, Garfinkel-Castro A, Khayesi M, et al, et al. Pedestrian safety and the built environment: a review of the risk factors. Journal of Planning Literature. 2015;30((4)):377–92. [Google Scholar]
- Ewing R, Dumbaugh E, et al. The built environment and traffic safety: a review of empirical evidence. Journal of Planning Literature. 2009;23((4)):347–67. [Google Scholar]
- Nicklett EJ, Lohman MC, Smith ML, et al. Neighborhood environment and falls among community-dwelling older adults. Int J Environ Res Public Health. 2017 doi: 10.3390/ijerph14020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chippendale T, Boltz M, et al. The neighborhood environment: perceived fall risk, resources, and strategies for fall prevention. Gerontologist. 2015;55((4)):575–83. doi: 10.1093/geront/gnu019. [DOI] [PubMed] [Google Scholar]
- Gong Y, Palmer S, Gallacher J, Marsden T, Fone D, et al. A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environ Int. 2016:48–57. doi: 10.1016/j.envint.2016.08.019. [DOI] [PubMed] [Google Scholar]
- Renalds A, Smith TH, Hale PJ, et al. A systematic review of built environment and health. Fam Community Health. 2010;33((1)):68–78. doi: 10.1097/FCH.0b013e3181c4e2e5. [DOI] [PubMed] [Google Scholar]
- Mazumdar S, Learnihan V, Cochrane T, Davey R, et al. The built environment and social capital: a systematic review. Environ Behav. 2017;50((2)):119–58. [Google Scholar]
- The 2017 Canadian Chronic Disease Indicators. Health Promot Chronic Dis Prev Can. 2017;37((8)):248–51. doi: 10.24095/hpcdp.37.8.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerin E, Cain KL, Conway TL, et al, et al. Neighborhood environments and objectively measured physical activity in 11 countries. Med Sci Sports Exerc. 2014;46((12)):2253–64. doi: 10.1249/MSS.0000000000000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams MA, Frank LD, Schipperijn J, et al, et al. International variation in neighborhood walkability, transit, and recreation environments using geographic information systems: the IPEN adult study. International Journal of Health Geographics. 2014:43–64. doi: 10.1186/1476-072X-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pucher J, Buehler R, et al. Making cycling irresistible: lessons from the Netherlands, Denmark and Germany. Transport Reviews. 2008;28((4)):495–528. [Google Scholar]
- Mertens L, Compernolle S, Deforche B, et al, et al. Built environmental correlates of cycling for transport across Europe. Built environmental correlates of cycling for transport across Europe. Health & Place. 2017:35–42. doi: 10.1016/j.healthplace.2017.01.007. [DOI] [PubMed] [Google Scholar]
- Dyck D, Cerin E, Conway TL, et al, et al. Perceived neighborhood environmental attributes associated with adults' transport-related walking and cycling: findings from the USA, Australia and Belgium. Int J Behav Nutr Phys Act. 2012 doi: 10.1186/1479-5868-9-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdeaudhuij I, Dyck D, Salvo D, et al, et al. International study of perceived neighbourhood environmental attributes and body mass index: IPEN adult study in 12 countries. Int J Behav Nutr Phys Act. 2015:62–42. doi: 10.1186/s12966-015-0228-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz M, Romppel M, Grande G, et al. Built environment and health: a systematic review of studies in Germany. Built environment and health: a systematic review of studies in Germany. J Public Health (Oxf) 2016;40((1)):8–15. doi: 10.1093/pubmed/fdw141. [DOI] [PubMed] [Google Scholar]
- Politis CE, Mowat DL, Keen D, et al. Pathways to policy: lessons learned in multisectoral collaboration for physical activity and built environment policy development from the Coalitions Linking Action and Science for Prevention (CLASP) initiative. Can J Public Health. 2017;108((2)):e192–8. doi: 10.17269/CJPH.108.5758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, Malley L, et al. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005;8((1)):19–32. [Google Scholar]
- Betancourt MT, Roberts KC, Bennett TL, Driscoll ER, Jayaraman G, Pelletier L, et al. Monitoring chronic diseases in Canada: the Chronic Disease Indicator Framework. Chronic Dis Inj Can. 2014;34((Suppl 1)):1–30. [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, et al, et al. Prisma extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169((7)):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Kardan O, Gozdyra P, Misic B, et al, et al. Neighborhood greenspace and health in a large urban center. Scientific Reports. 2015 doi: 10.1038/srep11610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo P, Wheaton B, Nisenbaum R, Glazier RH, Dunn JR, Chambers C, et al. The Neighbourhood Effects on Health and Well-being (NEHW) study. The Neighbourhood Effects on Health and Well-being (NEHW) study. Health & Place. 2015:65–74. doi: 10.1016/j.healthplace.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Chiu M, Maclagan LC, et al, et al. Moving to a highly walkable neighborhood and incidence of hypertension: a propensity-score matched cohort study. Environmental Health Perspectives. 2016;124((6)):754–60. doi: 10.1289/ehp.1510425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel L, Chudyk AM, Ashe MC, McKay HA, Bryan S, et al. Older adults' quality of life - exploring the role of the built environment and social cohesion in community-dwelling seniors on low income. Soc Sci Med. 2016:1–11. doi: 10.1016/j.socscimed.2016.07.008. [DOI] [PubMed] [Google Scholar]
- Pouliou T, Elliott SJ, et al. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Health & Place. 2010;16((2)):389–98. doi: 10.1016/j.healthplace.2009.11.011. [DOI] [PubMed] [Google Scholar]
- Glazier RH, Creatore MI, Weyman JT, Fazli G, Matheson FI, et al. Density, destinations or both. PLOS ONE. 2014;9((3)):e85295–98. doi: 10.1371/journal.pone.0085295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chum A, Campo P, et al. Contextual determinants of cardiovascular diseases: overcoming the residential trap by accounting for non-residential context and duration of exposure. Contextual determinants of cardiovascular diseases: overcoming the residential trap by accounting for non-residential context and duration of exposure. Health & Place. 2013:73–9. doi: 10.1016/j.healthplace.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Chum A, Campo P, et al. Cross-sectional associations between residential environmental exposures and cardiovascular diseases. BMC Public Health. 2015;15((1)):438–9. doi: 10.1186/s12889-015-1788-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Creatore MI, Gozdyra P, Park AL, Ray JG, et al. A population-based study of premature mortality in relation to neighbourhood density of alcohol sales and cheque cashing outlets in Toronto, Canada. BMJ Open. 2014;4((12)):e006032–9. doi: 10.1136/bmjopen-2014-006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouliou T, Elliott SJ, Paez A, Newbold KB, et al. Building obesity in Canada: understanding the individual- and neighbourhood-level determinants using a multi-level approach. Geospatial Health. 2014;9((1)):45–55. doi: 10.4081/gh.2014.5. [DOI] [PubMed] [Google Scholar]
- Gariepy G, Blair A, Kestens Y, Schmitz N, et al. Neighbourhood characteristics and 10-year risk of depression in Canadian adults with and without a chronic illness. Neighbourhood characteristics and 10-year risk of depression in Canadian adults with and without a chronic illness. Health & Place. 2014:279–86. doi: 10.1016/j.healthplace.2014.10.009. [DOI] [PubMed] [Google Scholar]
- Gariepy G, Thombs BD, Kestens Y, Kaufman JS, Blair A, Schmitz N, et al. The neighbourhood built environment and trajectories of depression symptom episodes in adults: a latent class growth analysis. PLOS ONE. 2015;10((7)):e0133603–86. doi: 10.1371/journal.pone.0133603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parachute. Toronto(ON): 2015. The cost of injury in Canada [Internet] Available from: http://www.parachutecanada.org/downloads/research/Cost_of_Injury-2015.pdf. [Google Scholar]
- Tran BX, Nair AV, Kuhle S, Ohinmaa A, Veugelers PJ, et al. Cost analyses of obesity in Canada: scope, quality, and implications. Cost Eff Resour Alloc. 2013;11((1)):3–86. doi: 10.1186/1478-7547-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra R, Siva H, Kehler M, et al. Walk-friendly suburbs for older adults. J Aging Stud. 2015:10–9. doi: 10.1016/j.jaging.2015.07.002. [DOI] [PubMed] [Google Scholar]
- Dupuis-Blanchard S, Gould ON, Gibbons C, Simard M, thier S, Villalon L, et al. Strategies for aging in place: the experience of language-minority seniors with loss of independence. Glob Qual Nurs Res. 2015 doi: 10.1177/2333393614565187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowledge translation on ageing and health: a framework for policy development 2012 [Internet] World Health Organization. 2012 [Google Scholar]
- Hodek JM, Ruhe AK, Greiner W, et al. Relationship between health-related quality of life and multimorbidity. Gesundheitswesen. 2009;72((8-9)):455–65. doi: 10.1055/s-0029-1234121. [DOI] [PubMed] [Google Scholar]
- Mujica-Mota RE, Roberts M, Abel G, et al, et al. Common patterns of morbidity and multi-morbidity and their impact on health-related quality of life: evidence from a national survey. Qual Life Res. 2015;24((4)):909–18. doi: 10.1007/s11136-014-0820-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan MS, Berthelot JM, Feeny D, McFarland BH, Khan S, Orpana H, et al. The predictive validity of health-related quality of life measures: mortality in a longitudinal population-based study. Qual Life Res. 2007;16((9)):1539–46. doi: 10.1007/s11136-007-9256-7. [DOI] [PubMed] [Google Scholar]
- Tambay JL, Catlin G, et al. Sample design of the national population health survey. Health Rep. 1995;7((1)):29–38. [PubMed] [Google Scholar]
- Raina PS, Wolfson C, Kirkland SA, et al, et al. The Canadian Longitudinal Study on Aging (CLSA) Can J Aging. 2009;28((3)):221–9. doi: 10.1017/S0714980809990055. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. Ottawa(ON): 2017. Social Data Linkage Environment (SDLE) [Internet] [Google Scholar]
- Hystad P, Davies HW, Frank L, et al, et al. Residential greenness and birth outcomes: evaluating the influence of spatially correlated built-environment factors. Environ Health Perspect. 2014;122((10)):1095–102. doi: 10.1289/ehp.1308049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Rudenstine S, Wallace Z, Vlahov D, et al. Urban built environment and depression: a multilevel analysis. J Epidemiol Community Health. 2005;59((10)):822–7. doi: 10.1136/jech.2005.033084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth GL, Creatore MI, Moineddin R, et al, et al. Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care. 2013;36((2)):302–8. doi: 10.2337/dc12-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creatore MI, Glazier RH, Moineddin R, et al, et al. Association of neighborhood walkability with change in overweight, obesity, and diabetes. JAMA. 2016;315((20)):2211–20. doi: 10.1001/jama.2016.5898. [DOI] [PubMed] [Google Scholar]
- Strauss J, Miranda-Moreno LF, Morency P, et al. Mapping cyclist activity and injury risk in a network combining smartphone GPS data and bicycle counts. Accid Anal Prev. 2015:132–42. doi: 10.1016/j.aap.2015.07.014. [DOI] [PubMed] [Google Scholar]
- Chiu M, Shah BR, Maclagan LC, Rezai MR, Austin PC, Tu JV, et al. Walk score® and the prevalence of utilitarian walking and obesity among Ontario adults: a cross-sectional study. Health Rep. 2015;26((7)):3–10. [PubMed] [Google Scholar]
- Lebel A, Kestens Y, Pampalon R, Theriault M, Daniel M, Subramanian SV, et al. Local context influence, activity space, and foodscape exposure in two Canadian metropolitan settings: is daily mobility exposure associated with overweight. J Obesity. 2012 doi: 10.1155/2012/912645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross NA, Crouse D, Tremblay S, Khan S, Tremblay M, et al. Body mass index in urban Canada: neighborhood and metropolitan area effects. Am J Public Health. 2007;97((3)):500–8. doi: 10.2105/AJPH.2004.060954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasfi RA, Dasgupta K, Orpana H, Ross NA, et al. Neighborhood walkability and body mass index trajectories: longitudinal study of Canadians. Am J Public Health. 2016;106((5)):934–40. doi: 10.2105/AJPH.2016.303096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry T, Spence J, Blanchard C, Cutumisu N, Edwards J, Selfridge G, et al. A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. Int J Behav Nutr Phys Act. 2010;7((57)):1–11. doi: 10.1186/1479-5868-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aultman-Hall L, Kaltenecker MG, et al. Toronto bicycle commuter safety rates. Accid Anal Prev. 1999;31((6)):675–86. doi: 10.1016/s0001-4575(99)00028-7. [DOI] [PubMed] [Google Scholar]
- Cripton PA, Shen H, Brubacher JR, et al, et al. Severity of urban cycling injuries and the relationship with personal, trip, route and crash characteristics: analyses using four severity metrics. BMJ Open. 2015;5((1)):e006654–86. doi: 10.1136/bmjopen-2014-006654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes JJ, Habib MA, et al. Pedestrian injury severity levels in the Halifax regional municipality, Nova Scotia, Canada: hierarchical ordered probit modeling approach. Transp Res Rec. 2015:172–8. [Google Scholar]
- Harris MA, Reynolds CC, Winters M, et al, et al. Comparing the effects of infrastructure on bicycling injury at intersections and non-intersections using a case-crossover design. Injury Prevention. 2013;19((5)):303–10. doi: 10.1136/injuryprev-2012-040561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klassen J, El-Basyouny K, Islam MT, et al. Analyzing the severity of bicycle-motor vehicle collision using spatial mixed logit models: a city of Edmonton case study. Safety Science. 2014:295–304. [Google Scholar]
- Miranda-Moreno LF, Morency P, El-Geneidy AM, et al. The link between built environment, pedestrian activity and pedestrian-vehicle collision occurrence at signalized intersections. Accid Anal Prev. 2011;43((5)):1624–34. doi: 10.1016/j.aap.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Morency P, Gauvin L, Plante C, Fournier M, Morency C, et al. Neighborhood social inequalities in road traffic injuries: the influence of traffic volume and road design. Am J Public Health. 2012;102((6)):1112–9. doi: 10.2105/AJPH.2011.300528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morency P, Archambault J, Tremblay M, Plante C, et al. Major urban road characteristics and injured pedestrians: a representative survey of intersections in Montréal, Quebec. Can J Public Health. 2015;106((6)):e388–94. doi: 10.17269/CJPH.106.4821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond SA, Willan AR, Rothman L, et al, et al. The impact of pedestrian countdown signals on pedestrian-motor vehicle collisions: a reanalysis of data from a quasi-experimental study. Inj Prev. 2014;20((3)):155–8. doi: 10.1136/injuryprev-2012-040717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifaat SM, Tay R, et al. Effects of street patterns on injury risks in two-vehicle crashes. Transp Res Rec. 2009:61–7. [Google Scholar]
- Rifaat SM, Tay R, Barros A, et al. Effect of street pattern on the severity of crashes involving vulnerable road users. Accid Anal Prev. 2011;43((1)):276–83. doi: 10.1016/j.aap.2010.08.024. [DOI] [PubMed] [Google Scholar]
- Rifaat SM, Tay R, Barros AG, et al. Logistic model of injury risks in single vehicle crashes in urban neighborhoods. Rifaat SM, Tay R, de Barros AG. 2011;45((3)):186–95. [Google Scholar]
- Romanow NT, Couperthwaite AB, McCormack GR, Nettel-Aguirre A, Rowe BH, Hagel BE, et al. Environmental determinants of bicycling injuries in Alberta, Canada. J Environ Public Health. 2012:487681–95. doi: 10.1155/2012/487681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman L, Slater M, Meaney C, Howard A, et al. Motor vehicle and pedestrian collisions: burden of severe injury on major versus neighborhood roads. Traffic Inj Prev. 2010;11((1)):43–7. doi: 10.1080/15389580903452340. [DOI] [PubMed] [Google Scholar]
- Rothman L, Howard AW, Camden A, Macarthur C, et al. Pedestrian crossing location influences injury severity in urban areas. Inj Prev. 2012;18((6)):365–70. doi: 10.1136/injuryprev-2011-040246. [DOI] [PubMed] [Google Scholar]
- Teschke K, Harris M, Reynolds CC, et al, et al. Route infrastructure and the risk of injuries to bicyclists: a case-crossover study. Am J Public Health. 2012;102((12)):2336–43. doi: 10.2105/AJPH.2012.300762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teschke K, Dennis J, Winters M, Harris MA, et al. Bicycling crashes on streetcar (tram) or train tracks: mixed methods to identify prevention measures. BMC Public Health. 2016;16((1)):1–10. doi: 10.1186/s12889-016-3242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss J, Manaugh K, Miranda-Moreno LF, et al. Estimating potential effect of speed limits, built environment, and other factors on severity of pedestrian and cyclist injuries in crashes. Transp Res Rec. 2011:81–90. [Google Scholar]
- Prince SA, Kristjansson EA, Russell K, et al, et al. A multilevel analysis of neighbourhood built and social environments and adult self-reported physical activity and body mass index in Ottawa, Canada. Int J Environ Res Public Health. 2011;8((10)):3953–78. doi: 10.3390/ijerph8103953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Kristjansson EA, Russell K, et al, et al. Relationships between neighborhoods, physical activity, and obesity: a multilevel analysis of a large Canadian city. Obesity. 2012;20((10)):2093–100. doi: 10.1038/oby.2011.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngom R, Gosselin P, Blais C, Rochette L, et al. Type and proximity of green spaces are important for preventing cardiovascular morbidity and diabetes—a cross-sectional study for Quebec, Canada. Int J Environ Res Public Health. 2016;13((4)):423–100. doi: 10.3390/ijerph13040423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariepy G, Kaufman JS, Blair A, Kestens Y, Schmitz N, et al. Place and health in diabetes: the neighbourhood environment and risk of depression in adults with type 2 diabetes. Diabetic Medicine. 2015;32((7)):944–50. doi: 10.1111/dme.12650. [DOI] [PubMed] [Google Scholar]
- Demoury C, Thierry B, Richard H, Sigler B, Kestens Y, Parent ME, et al. Residential greenness and risk of prostate cancer: a case-control study in Montreal, Canada. Environ Int. 2017:129–36. doi: 10.1016/j.envint.2016.10.024. [DOI] [PubMed] [Google Scholar]
- Villeneuve PJ, Jerrett M, Su JG, et al, et al. A cohort study relating urban green space with mortality in Ontario, Canada. Environ Res. 2012:51–8. doi: 10.1016/j.envres.2012.03.003. [DOI] [PubMed] [Google Scholar]
- Alter DA, Eny K, et al. The relationship between the supply of fast-food chains and cardiovascular outcomes. Can J Public Health. 2005;96((3)):173–7. doi: 10.1007/BF03403684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky JY, Moineddin R, Glazier RH, Dunn JR, Booth GL, et al. Relative and absolute availability of fast-food restaurants in relation to the development of diabetes: a population-based cohort study. Can J Public Health. 2016;107((S1)):5312–7. doi: 10.17269/CJPH.107.5312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquet C, Gauvin L, Kestens Y, Daniel M, et al. Sense of mastery and metabolic risk: moderating role of the local fast-food environment. Psychosom Med. 2010;72((3)):324–31. doi: 10.1097/PSY.0b013e3181cdf439. [DOI] [PubMed] [Google Scholar]
- Daniel M, Paquet C, Auger N, Zang G, Kestens Y, et al. Association of fast-food restaurant and fruit and vegetable store densities with cardiovascular mortality in a metropolitan population. Eur J Epidemiol. 2010;25((10)):711–9. doi: 10.1007/s10654-010-9499-4. [DOI] [PubMed] [Google Scholar]
- Hollands S, Campbell MK, Gilliland J, Sarma S, et al. A spatial analysis of the association between restaurant density and body mass index in Canadian adults. Prev Med. 2013;57((4)):258–64. doi: 10.1016/j.ypmed.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Hollands S, Campbell MK, Gilliland J, Sarma S, et al. Association between neighbourhood fast-food and full-service restaurant density and body mass index: a cross-sectional study of Canadian adults. Can J Public Health. 2014;105((3)):e172–8. doi: 10.17269/cjph.105.4287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestens Y, Lebel A, Chaix B, et al, et al. Association between Activity space exposure to food establishments and individual risk of overweight. PLOS ONE. 2012;7((8)):e41418–8. doi: 10.1371/journal.pone.0041418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minaker LM, Raine KD, Wild TC, Thompson ME, Frank LD, et al. Objective food environments and health outcomes. Am J Prev Med. 2013;45((3)):289–96. doi: 10.1016/j.amepre.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Polsky JY, Moineddin R, Dunn JR, Glazier RH, Booth GL, et al. Absolute and relative densities of fast-food versus other restaurants in relation to weight status: does restaurant mix matter. Prev Med. 2016:28–34. doi: 10.1016/j.ypmed.2015.11.008. [DOI] [PubMed] [Google Scholar]
- Spence JC, Cutumisu N, Edwards J, et al, et al. Relation between local food environments and obesity among adults. BMC Public Health. 2009;9((1)):192–34. doi: 10.1186/1471-2458-9-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuurman N, Peters PA, Oliver LN, et al. Are obesity and physical activity clustered. Obesity. 2009;17((12)):2202–9. doi: 10.1038/oby.2009.119. [DOI] [PubMed] [Google Scholar]