Abstract
The Public Health Agency of Canada (PHAC) has modernized its approach to physical activity surveillance by broadening its scope to include sedentary behaviour and sleep. The first step was to develop a conceptual framework which covers the full spectrum of physical movement from moderate-to-vigorous intensity physical activity (MVPA) and light intensity physical activity (LPA) to sedentary behaviour and sleep. The framework accounts for the environments in which these behaviours take place (home, work/school, transportation, and community), and applies a socioecological approach to incorporate individual factors and broader built, social, and societal environmental indicators. A visual model of the conceptual framework was created to aid dissemination.
Keywords: motor activity, sedentary behaviour, sleep, framework
Highlights
The Public Health Agency of Canada (PHAC) has modernized its approach to physical activity surveillance to include all aspects of daily movement from moderate-to-vigorous intensity physical activity (MVPA) and light intensity physical activity (LPA) to sedentary behaviour and sleep.
The new approach accounts for the environments where these behaviours take place (home, work/ school, transportation, and community) and the socioecological model.
To guide this process, the PHAC has developed a conceptual framework and visual model.
Canada has a long series of physical activity surveillance data1 which have received international recognition.2 Canada’s physical activity surveillance system has traditionally focused on measures of leisure-time physical activity. In recent years, there has been a growth in research identifying the independent effects of prolonged sedentary behaviour (e.g., time spent sitting, lying or reclining while awake at a low energy expenditure)3 and inadequate sleep4,5 on chronic disease.6,7 Further, at the international level, there has been a move away from measuring physical activity through the single lens of leisuretime physical activity and instead examining physical activity behaviours/indicators from across domains of physical activity, such as home, work/school, transportation, and community.8 Finally, a number of scientific systematic reviews and key research papers have been published outlining a broad range of individual, social and environmental correlates or dimensions for physical activity, sedentary behaviour and sleep that were important for consideration with an evidence based surveillance system.9-17 Drawing on these developments, the Public Health Agency of Canada (PHAC) modernized its physical activity surveillance system.
To support the identification and selection of a set of surveillance indicators that would form the foundation of the PHAC’s Physical Activity, Sedentary behaviour and Sleep (PASS) surveillance system, a conceptual framework was developed.18 The conceptual framework included three core components (i.e., behaviours, settings, socioecological approach) and the 24-hour movement spectrum (i.e., physical activity [light, moderate and vigorous], sedentary behaviour and sleep). The first component identified the behaviours of interest: moderate-to-vigorous intensity physical activity (MVPA), light intensity physical activity (LPA), sedentary behaviour, and sleep. The second component looked to incorporate a domain approach to the conceptual framework8 by recognizing the settings in which these behaviours take place including: home; work/school; transportation; and, community. The final component is the use of a socioecological approach recognizing the importance of indicators across multiple levels of influence including: the individual (e.g., age, sex, ethnicity, socioeconomic status); the family/social environment (e.g., intrapersonal relationships, social norms, crime, neighbourhood demographics); and, the built environment (e.g., roadways, buildings, parks, playgrounds, public transit).
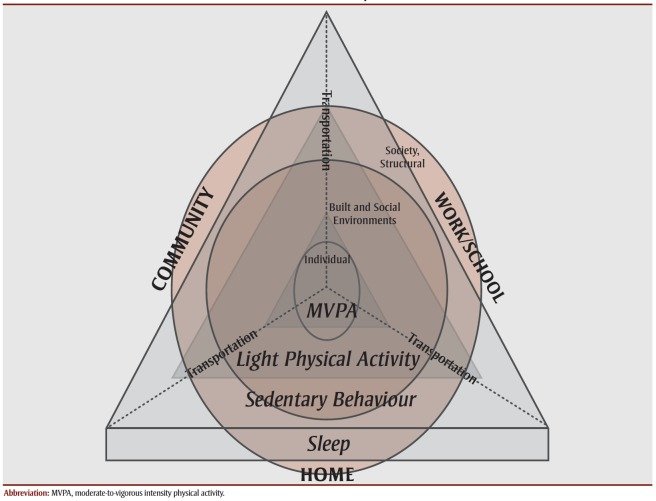
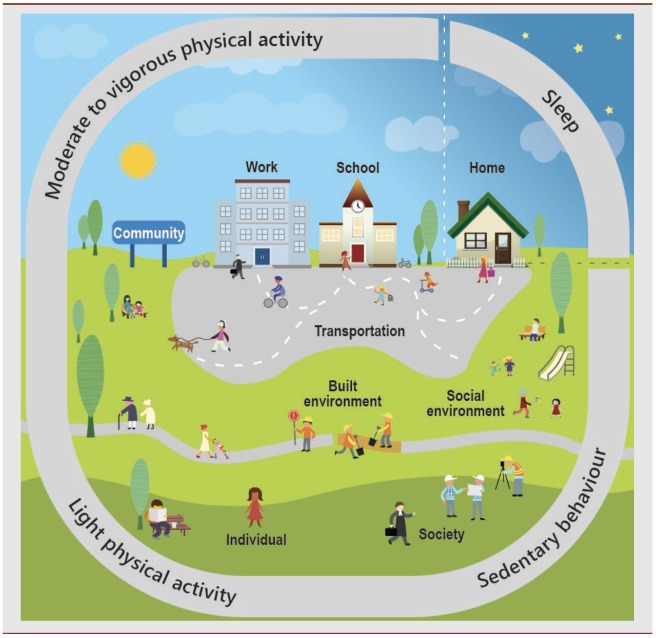
To quickly and easily describe the components of the conceptual framework, a visual model was created (Figure 1). This initial visual model, which displayed the components of the conceptual framework using a pyramid format, was presented to experts in the fields of physical activity, sedentary behaviour and sleep, who broadly agreed that it was consistent with current knowledge, and it was used during the selection of the PASS surveillance indicators at a meeting in Ottawa on June 24, 2014.18 This initial framework lacked descriptions of the types of activities which the indicators were intended to illustrate. Further, the sense of hierarchy in the outcomes implied by the use of a pyramid was not its intended purpose. As a result, a second, visual model (Figure 2) was developed and has been adopted for use alongside the PASS Indicators.18 The revised visual model includes illustrative examples of the components of the PASS Indicators.
Figure 1. Initial visual model of the conceptual framework.
Figure 2. Current physical activity, sedentary behaviour and sleep (PASS) visual model of the conceptual framework for surveillance in Canada.
The visual model illustrates the proposed depth and breadth of the PHAC’s modernized PASS surveillance system. Work to ensure data development and reporting are undertaken in such a way that all areas of the conceptual framework are meaningfully represented is part of the PHAC’s ongoing surveillance activities. In addition, both the visual model and the conceptual framework communicate the PHAC’s approach to PASS surveillance to other international and domestic governmental partners working in surveillance and policy, and to researchers for their contribution and critical appraisal.
Conflicts of interest
The authors declare no conflicts of interest.
Authors’ contributions and statement
GB, KR, EK, DR and GJ developed the concepts in the paper and GB and KR wrote the paper. BB, SP and WT reviewed the paper and offered advice, comments or refinements. The study was carried out under the management of WT and GJ.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
References
- Craig CL, Russell SJ, Cameron C, et al, et al. Twenty-year trends in physical activity among Canadian adults. Can J Public Health. 2004;95((1)):59–63. doi: 10.1007/BF03403636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellew B, eppe S, Bull FC, et al, et al. The rise and fall of Australian physical activity policy 1996 - 2006: a national review framed in an international context. Australia and New Zealand Health Policy. 2008:a national review framed in an international context–63. doi: 10.1186/1743-8462-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay MS, Aubert S, Barnes JD, et al, et al. Sedentary Behavior Research Network (SBRN) - Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14((1)):75–63. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay MS, Carson V, Chaput JP, et al, et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl Physiol Nutr Metab. 2016;41((6 Suppl 3)):S311–27. doi: 10.1139/apnm-2016-0203. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, et al, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1((4)):233–43. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Church TS, Craig CL, et al, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41((5)):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- Knutson KL, Cauter E, et al. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallal PC, Andersen LB, Bull FC, et al, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380((9838)):247–57. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Prochaska JJ, Taylor WC, et al. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32((5)):963–75. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- Trost SG, Owen N, Bauman AE, et al, et al. Correlates of adults' participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34((12)):1996–2001. doi: 10.1097/00005768-200212000-00020. [DOI] [PubMed] [Google Scholar]
- Owen N, Sugiyama T, Eakin EE, et al, et al. Adults' sedentary behavior: determinants and interventions. Am J Prev Med. 2011;41((2)):189–96. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- Prince SA, Reed JL, McFetridge C, et al, et al. Correlates of sedentary behaviour in adults: a systematic review. Obes Rev. 2017;18((8)):915–35. doi: 10.1111/obr.12529. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, et al. Sleep health: can we define it. Sleep. 2014;37((1)):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Gunn HE, et al, et al. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015:23–36. doi: 10.1016/j.smrv.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenthaler TI, Croft JB, Dort LC, et al, et al. Development of the National Healthy Sleep Awareness Project Sleep Health Surveillance Questions. J Clin Sleep Med. 2015;11((9)):1057–62. doi: 10.5664/jcsm.5026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterdt E, Liersch S, Walter U, Educ J, et al. Correlates of physical activity of children and adolescents: a systematic review of reviews. Health Educ J. 2014;73((1)):72–89. [Google Scholar]
- Sallis JF, Bauman A, Pratt M, et al. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15((4)):379–97. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]
- Roberts KC, Butler G, Branchard B, et al, et al. The physical activity, sedentary behaviour and sleep (PASS) indicator framework. Health Promot Chronic Dis Prev Can. 2017;37((8)):252–6. doi: 10.24095/hpcdp.37.8.04. [DOI] [PMC free article] [PubMed] [Google Scholar]