The NiV and HeV henipaviruses are BSL-4 pathogens transmitted from bats. NiV and HeV often lead to human death and animal diseases. The formation of multinucleated cells (syncytia) is a hallmark of henipaviral infections and is caused by fusion of cells coordinated by interactions of the viral attachment (G) and fusion (F) glycoproteins. We found via various assays that viral entry and syncytium formation depend on the viral origin of the glycoproteins, with HeV F and NiV G promoting higher membrane fusion levels than their counterparts. This is important knowledge, since both viruses use the same bat vector species and potential coinfections of these or subsequent hosts may alter the outcome of disease.
KEYWORDS: Hendra, Nipah, entry, fusion, henipaviral, henipavirus, heterologous, homologous, paramyxovirus, virus
ABSTRACT
Nipah and Hendra viruses (NiV and HeV) exhibit high lethality in humans and are biosafety level 4 (BSL-4) paramyxoviruses in the growing genus Henipavirus. The attachment (G) and fusion (F) envelope glycoproteins are both required for viral entry into cells and for cell-cell fusion, which is pathognomonic of henipaviral infections. Here, we compared the fusogenic capacities between homologous and heterologous pairs of NiV and HeV glycoproteins. Importantly, to accurately measure their fusogenic capacities, as these depend on glycoprotein cell surface expression (CSE) levels, we inserted identical extracellular tags to both fusion (FLAG tags) or both attachment (hemagglutinin [HA] tags) glycoproteins. Importantly, these tags were placed in extracellular sites where they did not affect glycoprotein expression or function. NiV and HeV glycoproteins induced comparable levels of homologous HEK293T cell-cell fusion. Surprisingly, however, while the heterologous NiV F/HeV G (NF/HG) combination yielded a hypofusogenic phenotype, the heterologous HeV F/NiV G (HF/NG) combination yielded a hyperfusogenic phenotype. Pseudotyped viral entry levels primarily corroborated the fusogenic phenotypes of the glycoprotein pairs analyzed. Furthermore, we constructed G and F chimeras that allowed us to map the overall regions in G and F that contributed to these hyperfusogenic or hypofusogenic phenotypes. Importantly, the fusogenic phenotypes of the glycoprotein combinations negatively correlated with the avidities of F-G interactions, supporting the F/G dissociation model of henipavirus-induced membrane fusion, even in the context of heterologous glycoprotein pairs.
IMPORTANCE The NiV and HeV henipaviruses are BSL-4 pathogens transmitted from bats. NiV and HeV often lead to human death and animal diseases. The formation of multinucleated cells (syncytia) is a hallmark of henipaviral infections and is caused by fusion of cells coordinated by interactions of the viral attachment (G) and fusion (F) glycoproteins. We found via various assays that viral entry and syncytium formation depend on the viral origin of the glycoproteins, with HeV F and NiV G promoting higher membrane fusion levels than their counterparts. This is important knowledge, since both viruses use the same bat vector species and potential coinfections of these or subsequent hosts may alter the outcome of disease.
INTRODUCTION
Nipah and Hendra viruses (NiV and HeV) are single-stranded RNA viruses that belong to the Henipavirus genus in the family Paramyxoviridae. These two biosafety level 4 (BSL-4) pathogens have mortality rates in humans ranging from 40% to 100%, varying by outbreak (1, 2, 61). Although some vaccine strategies have been explored, none have been approved for use in humans (3–5). The Coalition for Epidemic Preparedness Innovations (CEPI) has made it one of its top priorities to develop vaccines against Nipah virus and two other emergent viruses, Middle East respiratory syndrome and Lassa viruses (6). Recently, at least 19 new virus species in the genus Henipavirus have been found in Africa, demonstrating a greater genetic diversity in this genus than previously known (7). Because of their high mortality rates in humans and their wide global distribution, the study of henipaviruses is critical.
The paramyxoviral attachment (HN/H/G) and fusion (F) glycoproteins are necessary and sufficient for virus-cell or cell-cell membrane fusion during viral entry or syncytium formation, respectively. The henipaviral G and F glycoproteins are also major targets for virus-neutralizing antibodies (8–14). Cell-cell membrane fusion results in the formation of multinucleated cells (syncytia) and is believed to be important for both pathogenicity and viral spread (15). HN/H/G and F execute membrane fusion via highly coordinated efforts. In the past, there have been two proposed models for paramyxoviral fusion-promoted glycoprotein-glycoprotein interactions, which appear to correlate with the type of cellular receptors utilized. In the association or provocateur model, the attachment and fusion glycoproteins do not interact (at least significantly) until receptor binding occurs (16). Paramyxoviruses that bind sialic acid generally appear to conform to this model (16–20). Conversely, paramyxoviruses that bind protein receptors, such as henipaviruses and morbilliviruses, appear to conform to the dissociation or clamp model, in which the attachment glycoprotein G or H, respectively, interacts with F prior to receptor binding (17, 21). More recently the “safety-catch” model was described for the morbilliviruses (22). In this model, the attachment glycoprotein H and the F precursor F0 tightly assemble in the endoplasmic reticulum, mainly through the F head and the H stalk domain. In this model, the strength of H and F interactions is reduced for proteolytically cleaved F (F1 + F2) in the late Golgi compartments while presumably still blocking premature F triggering (Ftrig). This safety-catch interaction is released at the target membrane upon receptor binding. Regardless of these models, however, several aspects of the core molecular mechanism for membrane fusion appear to be conserved among paramyxoviruses (23, 24).
For the henipaviruses, G tetramers bind the ubiquitous cellular receptor ephrinB2 (9) or ephrinB3 (25) before undergoing a series of conformational changes we uncovered, ultimately resulting in the triggering of the metastable F trimer to execute membrane fusion (10). The henipaviral F glycoprotein exists in various forms. The precursor F0 is first transported to the cell surface and then endocytosed and cleaved by cathepsin L into the mature fusogenic subunits F1 and F2. These subunits, held together by a disulfide bond, are then recycled back to the cell surface, where this complex exists as trimers and hexamers of trimers, implicated in fusion pore formation and expansion (26). Upon F triggering, the fusion peptide located at the N terminus of F1 is inserted into the neighboring cell membrane, forming a prehairpin intermediate (PHI). Further conformational changes bring together two highly conserved heptad repeat regions located in F1 (HR1 and HR2) into a six-helix bundle (6HB) after fusion conformation. These conformational changes in F drive fusion of the virus-host cell or cell-cell membranes. HR1- or HR2-derived peptides have been successfully used to lock the PHI conformation into place and to help study the F-triggering process (27).
Chimeric henipaviral and paramyxoviral glycoproteins have been used to help us understand the mechanisms of glycoprotein-mediated membrane fusion processes (28–30). For example, an attachment glycoprotein chimera harboring the NiV G-derived globular head domain and the Newcastle disease virus (NDV) HN-derived stalk, transmembrane (TM), and cytoplasmic tail (CT) domains was able to trigger NDV F to promote cell-cell fusion, whereas the reciprocal chimera was not (28). This result showed for the first time that a paramyxovirus F protein can be triggered by an attachment protein that binds a different class of receptor, and that the G stalk is a determinant of specificity of F triggering. A subsequent study using measles virus (MeV) and NDV glycoprotein chimeras also showed that the stalk of the attachment glycoprotein determines the specificity of F activation (31). Further, for some paramyxoviruses, such as NiV, parainfluenza virus 5 (PIV5), and MeV, the attachment glycoprotein head domain is entirely dispensable for fusion activation, corroborating that the stalk domain triggers F (10, 32, 33). These studies also indicate that the G/H/HN head has a role in blocking F triggering until the receptor binding event, providing the spatiotemporal framework for the membrane fusion process. Fusion protein chimeric constructs have also further elucidated the role of the fusion protein in regulating membrane fusion. A study showed that switching an ∼45-amino-acid residue region in canine distemper virus (CDV) F to that of a homologous MeV F region resulted in fusion when triggered by MeV H (34). In a similar study, the substitution of a different region, a central pocket, from MeV F to CDV F also induced fusion when triggered by MeV H (35).
With the goal of elucidating how henipaviral G glycoproteins trigger F-mediated membrane fusion, in the present study we compare the membrane fusion capacities of the NiV and HeV G and F glycoproteins and define the areas in G or F important for homo- or heterotypic fusion activation. The G and F glycoproteins are highly conserved between the two viruses, with the G proteins sharing 79% and the F proteins 89% amino acid identity. Heterotypic functional activities of the NiV and HeV glycoproteins have been observed in vitro and in a reverse genetics system (36, 37). However, since cell-cell fusion is highly dependent on G and F cell surface expression (CSE) levels, a quantitative comparison between NiV and HeV homo- and heterotypic fusion levels is only possible if CSE levels can be quantified and compared (11, 38). We accomplished this by adding extracellular hemagglutinin (HA) tags to both NiV and HeV G and FLAG tags to both NiV and HeV F glycoproteins, since it is uncertain whether any of the available anti-G or anti-F antibodies are able to detect the glycoproteins of the two viral species equally (9, 11, 39). Although extracellular tags (HA) have been used for henipavirus Gs, they have not been described for the F glycoproteins (8). Here, we created well-expressed and fully functional extracellularly FLAG-tagged NiV F and HeV F at locations similar to those recently reported for members of the closely related Morbillivirus genus (35, 40, 41). Our results revealed equal homologous but unequal heterologous glycoprotein F-triggering capabilities. To enhance our mechanistic understanding of these results, we performed functional assays to determine the levels of F-G interactions, F triggering, and viral entry capabilities of wild-type (WT) and chimeric glycoprotein pairs to map the henipaviral glycoprotein bioactivities.
RESULTS
FLAG tag insertions at the extracellular domains of the NiV and HeV F fusion proteins do not alter their fusogenic capacities.
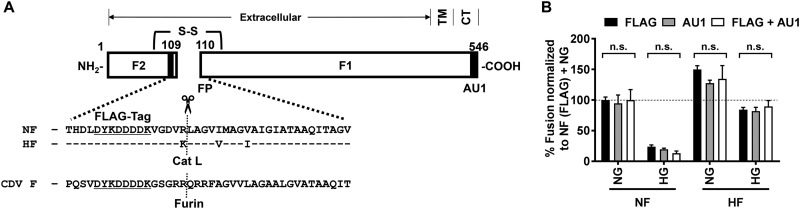
The NiV F (NF) and HeV F (HF) glycoproteins are class I viral fusion proteins with an N-terminal extracellular domain, a transmembrane domain, and a C-terminal intracellular domain (Fig. 1A). Intracellular F1 C-terminal tags (AU1) have been widely used in previous studies to detect henipavirus F glycoproteins and have not been shown to affect the functions of these proteins (Fig. 1A) (8, 10, 19). However, henipaviral F proteins with identical extracellular tags that allow quantitative comparisons of cell surface expression (CSE) and fusion levels have not been described. Such constructs are necessary because cell-cell fusion is highly dependent on glycoprotein CSE (11). Although polyclonal antisera against NiV F have been previously used to detect F (i.e., rabbit 834) (9, 19), it is uncertain whether HeV and NiV Fs could be equally detected by these or any other antisera or monoclonal antibodies.
FIG 1.
FLAG tag insertion in the F2 ectodomain and fusion phenotypes. (A) Schematic representation of the proteolytically cleaved NiV and HeV F (NF and HF). F1 and F2 subunits are held together by a disulfide bond. A FLAG tag was inserted just N terminal to the cathepsin L cleavage site (Cat L) located at the C terminus of F2, an extracellular portion of the F head domain. An AU1 tag, inserted at the intracellular C terminus of F (type I transmembrane protein), has been previously used for the detection of NF and HF (8, 11, 12, 19). FP depicts the location of the fusion peptide inserted into the target cell membrane during membrane fusion. The comparative sequences surrounding the cleavage site are shown for NiV, HeV, and CDV F glycoproteins. The N and C termini (NH2- and -COOH, respectively), transmembrane (TM), and cytoplasmic tail (CT) domains are indicated. (B) HEK293T cells were transfected with NF or HF expression plasmids in combination with either NG or HG. F expression constructs harbored an extracellular FLAG tag, an intracellular AU1 tag, or both (FLAG plus AU1). Sixteen to 20 hpt, cells were fixed with 1% paraformaldehyde and nuclei inside syncytia were counted (4 or more nuclei per multinucleated cell were considered a syncytium). Syncytial nuclei were counted and added within each microscopic field (200×), and five microscopic fields were counted for each transfection. The results were normalized to NF (FLAG)-NG fusion, which was set at 100% (dotted line). A one-way ANOVA statistical analysis was performed, followed by a Tukey pairwise multiple-comparison test. The data represent averages ± SEM from at least five independent experiments. Statistical significance is indicated. A P value of >0.05 is shown as nonsignificant (n.s.).
An insertion of a FLAG tag in the F ectodomain of the related morbilliviruses canine distemper virus (CDV) and measles virus (MeV) does not significantly modulate their bioactivity (40, 41). In those studies, the FLAG tag was inserted in the F2 subunit close to the furin cleavage site (Fig. 1A). The henipaviral Fs are processed by cathepsin L and not furin, and the sequences surrounding the protease cleavage site are very conserved among henipaviruses but much less conserved between henipaviruses and morbilliviruses (i.e., CDV F) (Fig. 1A). To test whether an insertion of a FLAG tag near the C terminus of the F2 subunit would alter the bioactivity of NF or HF, we constructed NiV and HeV Fs that harbor either a C-terminal intracellular AU1 tag, an extracellular FLAG tag, or both (FLAG plus AU1) (Fig. 1A). We then compared the fusion capacities of the single (FLAG or AU1)- or double (FLAG plus AU1)-tagged F constructs in combination with HA-tagged NiV G (NG) or HeV G (HG) constructs (Fig. 1B). HEK293T cells were transfected with F and G expression plasmids, and fusion levels were determined 16 to 20 h posttransfection (hpt) by counting nuclei inside syncytia per field (200× field; five fields for each combination, n ≥ 4 independent experiments) and normalizing the fusion levels to that of the wild-type NiV fusion (FLAG NF and NG, set to 100%). Neither the sequence, position of the tag, nor the presence of both tags (FLAG plus AU1) significantly altered the fusogenic capacity of the fusion protein significantly (P > 0.05 by one-way analysis of variance [ANOVA] followed by a Tukey pairwise multiple-comparison test) (Fig. 1B). Therefore, we continued utilizing FLAG-tagged F constructs in subsequent experiments unless otherwise noted to allow us to quantify and compare henipaviral F glycoprotein cell surface expression levels.
Notably, while homologous NiV and HeV F and G pairs yielded similar levels of cell-cell fusion, we observed fusion levels significantly lower than those of the wild type for the NF/HG pair (23.7%; P < 0.0001) and greater than wild-type fusion levels for the HF/NG pair (150.2%; P < 0.001) (Fig. 1B).
HeV and NiV glycoproteins induce comparable homologous but distinct heterologous fusion phenotypes.
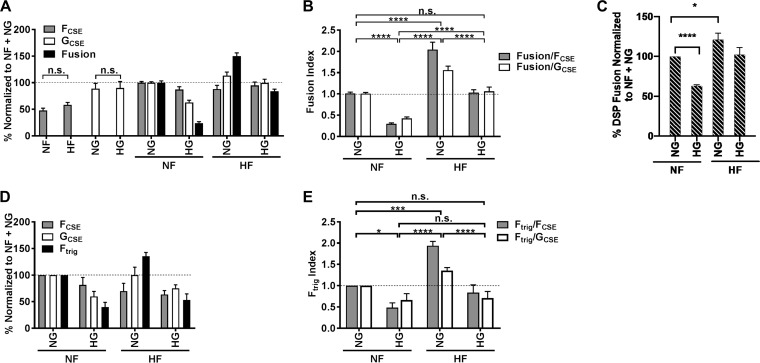
To quantitatively compare HeV and NiV fusion phenotypes, we determined the relative CSE levels on HEK293T cells. Cells were transfected with F and G expression plasmids as described above and harvested 16 to 20 hpt with ice-cold 10 mM EDTA in phosphate-buffered saline (PBS). CSE levels were determined by flow cytometry using monoclonal mouse anti-FLAG and/or rabbit anti-HA antibodies (FCSE and/or GCSE), followed by fluorescently labeled secondary antibodies (see Materials and Methods). The CSE expression levels were all normalized to NF/NG levels (CSE set to 100%). When the glycoproteins were expressed alone, we observed that the heterologous NF and HF (FCSE, 47.9% and 58.4%, respectively) and the heterologous NG and HG (GCSE, 88.9% and 90.1%, respectively) were expressed similarly on the cell surface (P > 0.05) (Fig. 2A). Interestingly, the F proteins were expressed at higher levels in the presence of G proteins. Further, homologous combinations of glycoproteins (NF/NG versus HF/HG) displayed equivalent CSE levels (Fig. 2A). However, GCSE levels appeared to be affected by the F glycoprotein expressed. For example, HG CSE levels increased in the presence of HF (99.5%) compared to that in the presence of NF (63.0%) (P < 0.0001). As CSE levels are known to affect cell-cell fusion levels, we calculated fusion indices (FIs) as the ratio of normalized cell-cell fusion levels to normalized CSE levels. A prior study for simian virus 5 (SV5) showed that F-mediated fusion was dependent on the surface density of the F protein but not the HN protein and that there is no linear correlation for both paramyxovirus glycoproteins (42). However, we previously showed for henipaviral glycoproteins that when transfecting with the amounts of DNA used in the current study, there is a linear correlation between cell surface expression and syncytium formation (11). To add rigor to our study, fusion indices were determined by taking both FCSE and GCSE into account (Fig. 2B). The FI for the NF/NG combination was set to 1.0; thus, levels significantly greater than 1.0 would be considered hyperfusogenic and those significantly lower than 1.0 would be hypofusogenic fusion phenotypes. To determine statistical significance, we performed a one-way ANOVA followed by a Tukey pairwise multiple-comparison test (Fig. 2B). In this analysis we used mean FIs (FIMean) for each glycoprotein combination, which is the combined mean for FIs calculated with GCSE and FCSE. Homotypic fusion resulted in comparable FIs (FIMean for NF/NG and HF/HG, 1.00 and 1.05, respectively) (Fig. 2B). However, heterotypic fusion yielded a hypofusogenic phenotype for the NF/HG pair (FIMean, 0.36; P < 0.0001) and a hyperfusogenic phenotype for the HF/NG pair (FIMean, 1.81; P < 0.0001). This result suggested that NiV-G is capable of triggering HeV-F more efficiently than the homologous HeV-G.
FIG 2.
NiV and HeV glycoproteins induce similar homologous but distinct heterologous fusion and F-triggering phenotypes. (A) HEK293T cells were transfected with NF, HF, NG, or HG expression constructs alone or in combination. Cells were harvested 16 to 20 hpt, and F and/or G cell surface expression (FCSE and GCSE) was determined by flow cytometry using a mouse anti-FLAG or rabbit anti-HA antibody, respectively. CSE levels were normalized to NF/NG CSE levels, set at 100% (dotted line). Cell-cell fusion levels were determined and normalized as described in the legend to Fig. 1B. (B) Fusion indices (FIs) were determined from results obtained for panel A by calculating the ratio of fusion to CSE levels (fusion/FCSE and fusion/GCSE). FIs were normalized to the FI of the NF/NG combination, set at 1.0 (dotted line). (C) Dual-split protein fusion assay. Effector HEK293T cells were transfected with DSP1 and NiV and HeV WT or chimeric fusion and attachment glycoproteins. Target HEK293T cells were transfected with ephrinB2 and DSP2. Twelve h posttransfection, cells were collected and incubated in the presence of EnduRen substrate and read at 8 h on a Tecan plate reader. Data shown are averages of percent normalized NF plus NG fusion from 4 experiments ± SEM. (D) F-triggering assay. HEK293T cells were transfected, and CSE levels (FCSE and GCSE) were measured as described above. CSE and F-triggering levels were determined at 10 hpt, a time point at which syncytia begin to be microscopically visible. F-triggering levels (Ftrig) were determined by flow cytometry using a Cy5-labeled HR2 peptide as outlined in Materials and Methods. Ftrig levels were normalized to the Ftrig levels of the NF/NG combination, set at 100% (dotted line). (E) F-triggering indices (FtrigIs) were determined from results obtained in panel C by calculating the ratio of Ftrig to CSE levels (Ftrig/FCSE and Ftrig/GCSE). FtrigIs were normalized to the FtrigI of the NF/NG combination, set at 1.0 (dotted line). For panels B and E, a one-way ANOVA statistical analysis was performed, followed by a Tukey pairwise multiple-comparison test. For panel C, a t test comparing each combination to the NF/NG pair was performed. Statistical significance is indicated. A P value of >0.05 is shown as nonsignificant (n.s.). *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001; ****, P ≤ 0.0001.
In addition, we performed a quantitative fusion pore formation assay based on a dual-split green fluorescent protein (GFP)/luciferase reporter protein. Effector HEK293T cells were transfected with DSP1 and NiV and HeV WT or chimeric fusion and attachment glycoproteins. Target HEK293T cells were transfected with ephrinB2 and DSP2. The trends of fusion pore formation levels were generally similar to those of cell-cell fusion phenotypes observed from syncytium counting (Fig. 2B and C), with the NF/HG pair reducing and the HF/NG pair increasing fusion pore formation (P ≤ 0.05) (Fig. 2C). Notably, the phenotypes measured by the DSP and syncytium assays are not identical. The DSP quantitative assay measures fusion pore formation, as cells only need a pore between them big enough for the DSP protein fractions to pass by and allow DSP1/DSP2 activity. In contrast, syncytium counts measure nuclei inside cell-cell fusion events that result in four or more nuclei per cell, which require full fusion pore expansion and movement of nuclei between cells, which are later events in the fusion process.
We next asked whether the hyper- and hypofusogenic fusion phenotypes directly correlated with differences in the ability of G to trigger F. We developed an NiV F-triggering assay that measures the amount of Cy5-labeled HR2 peptide that binds to triggered F. We used a protocol slightly modified from that of Aguilar et al. (27). We transfected HEK293T cells with just NiV-G (negative control) or both F and G. Briefly, prior to significant syncytium formation (∼10 hpt), F/G-expressing HEK293T cells were incubated at 4°C to synchronize receptor binding (receptors are present in HEK293T cells), and subsequently cells were allowed to undergo F triggering at 37°C for 30 min (27). Importantly, the NiV F HR2 peptide sequence differs from the HeV F HR2 sequence by two residues, but the peptide’s binding area in the HR1 region is identical between NiV F and HeV F (43). Thus, we found that the NiV F HR2 peptide could trap both NiV- and HeV-triggered F by binding the HR1 region in the F prehairpin intermediate (PHI) conformation at the cell surface. Besides Ftrig, we simultaneously measured F and G CSE at the same early time point. The relative amount of Ftrig roughly corresponded to the relative amount of fusion for each protein combination (compare Fig. 2D and E, and A). To account for differences in CSE levels, we determined an Ftrig index (FtrigI) by calculating the ratio of normalized Ftrig levels to normalized FCSE or GCSE levels (Ftrig/FCSE or Ftrig/GCSE) (Fig. 2E). A statistical analysis was performed as described above using the combined mean FtrigI (FtrigIMean; combined mean for Ftrig/FCSE and Ftrig/GCSE). F triggering with homologous glycoprotein combinations resulted in no significant differences between NF/NG and HF/HG (FtrigIMean, 1.00 and 0.77, respectively; P > 0.05). However, F triggering with heterologous glycoprotein pairs was increased for the HF/NG combination (FtrigIMean, 1.65; P < 0.001) and decreased for the NF/HG combination (FtrigIMean, 0.58; P < 0.05). These results indicate that F triggering is directly proportional to the cell-cell fusion capabilities of the respective glycoprotein pairs; thus, syncytium formation levels are likely due to membrane fusion steps prior to or coincident with F triggering.
The HG stalk and NF head are critical to achieve cell-cell fusion phenotypes.
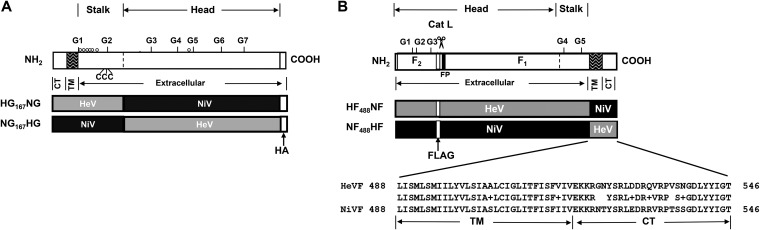
To elucidate which domains in the attachment glycoprotein G or the fusion glycoprotein F are important for the different heterologous fusion phenotypes observed, we created chimeric HeV and NiV G and F glycoproteins by swapping functional domains (Fig. 3A and B). We previously showed that a headless NG consisting of the cytoplasmic, transmembrane, and stalk domains (NG167) was sufficient to trigger NF to execute cell-cell fusion, suggesting that the G stalk triggers F (10). We therefore created NG167 with an HeV head (NG167HG) or HG167 with an NiV head (HG167NG) (Fig. 3A).
FIG 3.
Schematic representation of Nipah virus and Hendra virus G and F chimeras. (A) G chimeras were constructed by exchanging the head domain between the two viral G glycoproteins. HeV G with an NiV G head domain (HG167NG) and NiV G with an HeV G head domain (NG167HG) were constructed by overlapping PCR mutagenesis. (B) F chimeras were constructed by exchanging the transmembrane domain (TM) and the cytoplasmic tail (CT) between NiV and HeV F glycoproteins. The TM and CT domains in F are strongly conserved between the two viruses and have previously been implicated in viral budding (44, 45). HeV F with an NiV F TM/CT domain (HF488NF) and NiV F with an HeV F TM/CT domain (NF488HF) were constructed by overlapping PCR mutagenesis. Protein modifications, including N-glycosylation (in G, G1 to G7; in F, G1 to G5) and O-glycosylation (o) sites, as well as the cathepsin L cleavage site in F (Cat L), are depicted in G (A) and/or F (B).
For henipaviral Fs, both the transmembrane (TM) and cytoplasmic tail (CT) domains have been implicated as being important for membrane fusion as well as virus-like particle (VLP) formation (19, 44, 45). To understand the roles of these domains in heterologous fusion and budding, we created HF and NF chimeras with swapped transmembrane/cytoplasmic tail domains (TM/CT; amino acids 488 to 546). The resulting chimeras, NF488HF and HF488NF, were constructed with FLAG tags in their ectodomains, as described above (Fig. 3B).
Given that receptor binding to the attachment glycoprotein G is important in triggering F and fusion formation, we examined ephrinB2 binding to WT and chimeric G and measured their CSE levels (Fig. 4A). By calculating the ratio of ephrinB2 binding and CSE levels, we show that WT and chimeric G bind ephrinB2 roughly equally. We also compared oligomerization patterns of WT and chimeric G, since differences in G oligomerization patterns might affect cell surface expression levels and fusion (8, 46–48). Wild-type NiV and HeV G and their chimeras all displayed similar tetramer/dimer oligomerization ratios (one-way ANOVA followed by a Tukey pairwise multiple-comparison test) (Fig. 4B).
FIG 4.
Characterization of ephrinB2 binding and oligomerization. (A) Cell surface expression and ephrinB2 binding levels. EphrinB2 binding was further divided by CSE to account for differences in CSE between Gs. (B) The indicated wild-type or chimeric NiV and HeV G proteins were expressed in HEK293Ts, and lysates were collected at 24 h posttransfection. Lysates were then analyzed under reducing or nonreducing conditions. Proteins were detected using a PE-conjugated anti-HA antibody (1:1,000). One-way ANOVA statistical analysis was performed in GraphPad Prism, followed by a Tukey pairwise multiple-comparison test. Statistical significance is indicated. P > 0.05, nonsignificant (n.s.).
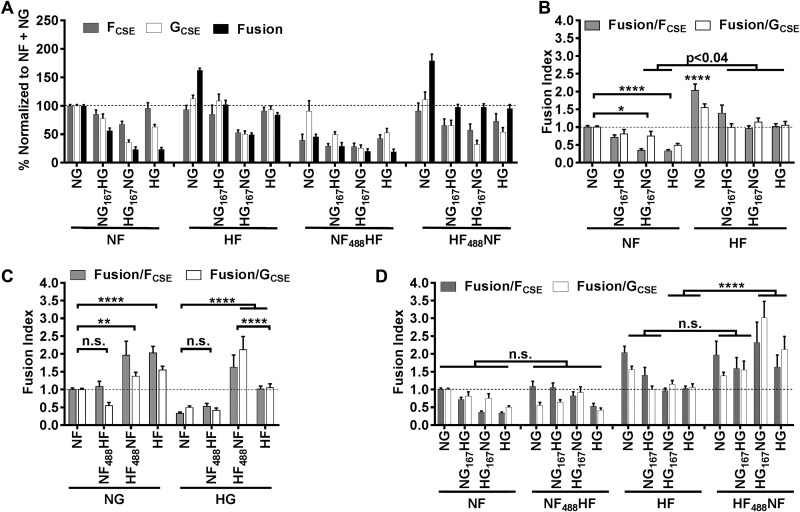
We then examined the fusogenic capacities of NF or HF in combination with the G chimeras (NG167HG or HG167NG) and determined the fusion indexes for these protein pairs (Fig. 5A and B; also see Fig. 7A). We observed a hypofusogenic phenotype for the NF/HG167NG combination similar to that for the NF/HG combination (FIMean, 0.56 and 0.42, respectively) (Fig. 5B; also see Fig. 7A). The FIs for both combinations were significantly lower than the FI for the NF/NG combination (P < 0.05), which indicates that the HG N-terminal (stalk-containing) domain confers the hypofusogenic phenotype. In contrast, for the HF combinations we found no G chimera that was sufficient to confer the hyperfusogenic phenotype of the HF/NG pair. This result suggests that both the head- and stalk-containing domains of NG contribute to inducing the hyperfusogenic phenotype of the HF/NG combination (Fig. 5B).
FIG 5.
Cell-cell fusion activities of wild-type and chimeric HeV and NiV F and G glycoproteins. (A) Cell surface expression (CSE) and cell-cell syncytium fusion levels are shown. (B to D) Fusion indices (FIs) were calculated for all combinations of F or F chimeras with G or G chimeras. CSE, fusion levels, and FIs were determined as outlined in the legend to Fig. 2, and a one-way ANOVA was performed as described in the legend to Fig. 2 The data represent averages ± SEM from at least four independent experiments.
FIG 7.
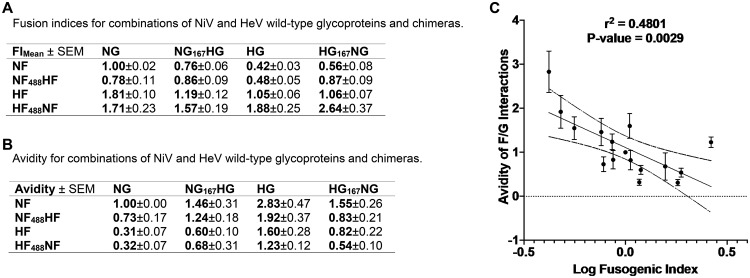
Negative correlation between fusogenicity and avidities of F-G interactions. (A) Fusion indices for combinations of NiV and HeV wild-type glycoproteins and chimeras. FIMean ± SEM is the fusion index (FI), the ratio of normalized fusion levels to normalized CSE levels. Fusion indices were determined by taking both FCSE and GCSE into account (FIMean), and the SEM were calculated. (B) Avidity of F-G interactions from Fig. 6 for combinations of NiV and HeV wild-type glycoproteins and chimeras. The ratios of coimmunoprecipitated G and F (GIP and FIP) as well as G in the cell lysate (lysate, α-HA) was calculated to determine the binding avidities for all F-G interactions [GIP/(GLys × FIP)]. The SEM are shown for each averaged value. (C) Avidity of F-G interactions from panel B plotted against the fusion index scores from panel A. Pearson correlation analysis was performed using GraphPad Prism.
The NiV F TM/CT domain can enhance the fusogenicity of HF.
We next examined the fusogenic capacities of wild-type or chimeric G glycoproteins in combination with the F chimeric glycoprotein NF488HF or HF488NF (Fig. 4A) and determined their FIs (Fig. 5C and D; also see Fig. 7A).
Interestingly, HF with the TM/CT domain of NiV F (HF488NF) yielded a significantly hyperfusogenic phenotype when combined with either wild-type or chimeric G glycoproteins, while wild-type HF induced hyperfusogenicity only in combination with wild-type NG (Fig. 5C and D; also see Fig. 7A). This indicates that the NF TM/CT domain is capable of enhancing the fusogenic properties of HeV F. In contrast, NF with the TM/CT domain of HeV F (NF488HF) did not significantly affect the fusogenic properties of NiV F, yielding fusion indices similar to those of wild-type NF for all G combinations (P > 0.05) (Fig. 5D; also see Fig. 7A). This indicates that the TM/CT domain of henipaviral Fs influences membrane fusion phenotypes in the context of the rest of the F glycoprotein, supporting our proposed inside-out signaling model for henipaviral F (19).
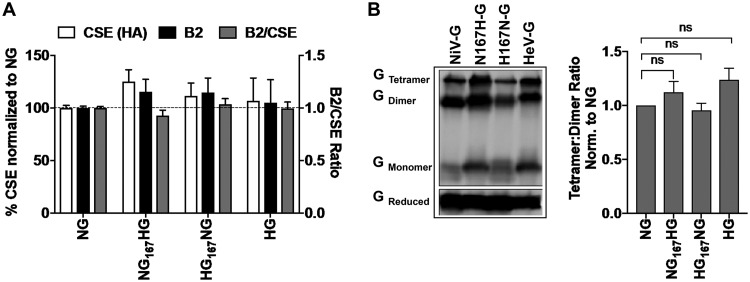
Avidities of F/G interactions inversely correlate with fusogenicities of F/G pairs.
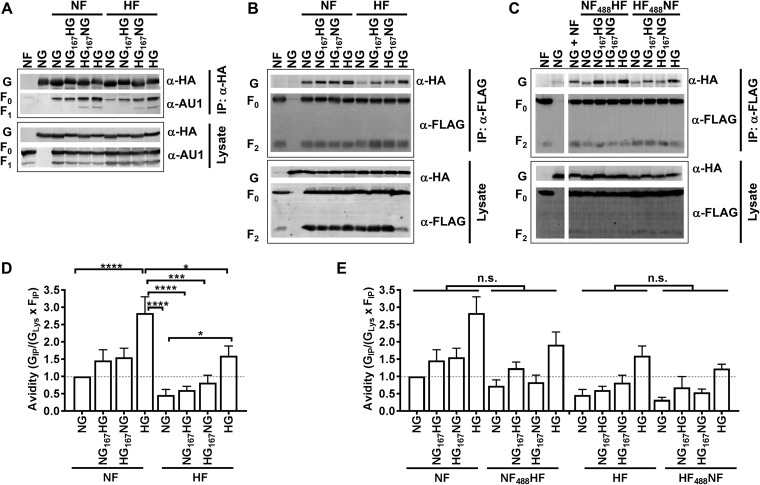
To analyze the binding avidities of the F-G interactions for the various F/G combinations, we performed coimmunoprecipitation (co-IP) assays from lysates of F/G-expressing HEK293T cells. Affinity purification was directed against either the HA tag in the attachment glycoprotein G or the FLAG tag in the fusion glycoprotein F. Importantly, only F that directly associated with G (IP, α-HA) or only G that directly associated with F (IP, α-FLAG) was coimmunoprecipitated (Fig. 6A to C). We used μMACS anti-HA or anti-FLAG magnetic beads to specifically bind HA-tagged G or FLAG-tagged F proteins. Viral G and F proteins were detected from total cell lysates or from the IP fractions by immunoblotting using rabbit anti-HA and mouse anti-AU1 or anti-FLAG antibodies (Fig. 6A to C). The detection of F2 by anti-FLAG immunoblotting of anti-HA immunoprecipitates was weak (data not shown), possibly due to masking of the FLAG epitope in the F2 subunit. Therefore, we first utilized AU1-tagged F constructs in G pulldown experiments (IP, α-HA) and compared the coimmunoprecipitated F (α-AU1) with coimmunoprecipitated G (α-HA) from F pulldown experiments (IP, α-FLAG) (Fig. 6A and B, respectively). Generally, the coimmunoprecipitated F (α-AU1; F0 + F1) showed a pattern for band intensities by Western blotting similar to that of the coimmunoprecipitated G for the same F-G combinations (Fig. 6A and B, respectively). We concluded from this observation that F/G binding avidities are similar whether F or G is pulled down and therefore continued performing F pulldown experiments (IP, α-FLAG) to determine the avidity of F-G interactions (Fig. 6C). We next determined the levels of coimmunoprecipitated G and F (GIP and FIP) as well as the G expression levels in the cell lysate (lysate, α-HA) from our fluorescence-based semiquantitative Western blots. We then determined the binding avidities for all F-G interactions as GIP/(GLys × FIP) to account for differences in G or F expression or pulldown efficiencies, as previously described (11, 19). To facilitate the comparison between different F-G interaction avidities, we normalized the values for each F and G combination to the value of NF/NG, set to 1 (Fig. 6D to E and 7B).
FIG 6.
Avidities of HeV and NiV F and G interactions. (A to C) HEK293T cells were transfected with the indicated combinations of wild-type or chimeric F and G expression constructs. Sixteen to 20 hpt cells were lysed, and viral glycoproteins were immunoprecipitated from the cell lysates using μMACS. Anti-HA (IP, α-HA) (A) or anti-FLAG (IP, α-FLAG) (B and C) magnetic beads were used. Total cell lysates (lysate) and immunoprecipitated proteins were separated by 10% SDS-PAGE and immunoblotted with mouse α-AU1 or α-FLAG (F detection) or rabbit α-HA (G detection) specific antibodies. Proteins were detected using fluorescent secondary antibodies to increase the quantitative aspect of our measurements. Cell lysates from cells transfected with F only or G only served as controls. (D and E) The amounts of immunodetected glycoproteins were measured by densitometry using Image Lab software. The obtained values were used to determine the binding avidities for all G and F combinations [GIP/(GLys × FIP)]. Binding avidity levels were normalized to the levels of NF/NG, set as 1.00 (Fig. 5D and E, dotted line). Statistical analysis was performed as outlined in the legend to Fig. 2. The data represent averages ± SEM from at least three independent experiments, and statistical analysis was performed as outlined in the legend to Fig. 2.
We found that the strongly hypofusogenic NF/HG combination had a significantly higher binding avidity than the NF/NG combination (avidities, 2.83 and 1.00, respectively; P < 0.0001) (Fig. 6A, B, and D and 7B). We also observed a significantly higher binding avidity for the HF/HG combination than for the hyperfusogenic HF/NG combination (avidities, 1.60 and 0.31, respectively; P < 0.05). These results indicate that HG binds more strongly than NG to either NF or HF. It is interesting that HG has a stronger binding avidity to NF than its cognate HF (avidity, 2.83 and 1.60, respectively). The F chimeras (NF488HF and HF488NF) yielded avidities with G and G chimeras similar to those of the corresponding wild-type Fs (P > 0.05, not significant), indicating that the origin of the TM/CT domain in F does not significantly affect the F-G binding avidities. In general, we observed a significant inverse correlation between fusogenicity levels and F-G avidities, similar to what we previously observed for HeV and NiV N-glycan mutants (P < 0.01) (Fig. 7A and C) (8, 11).
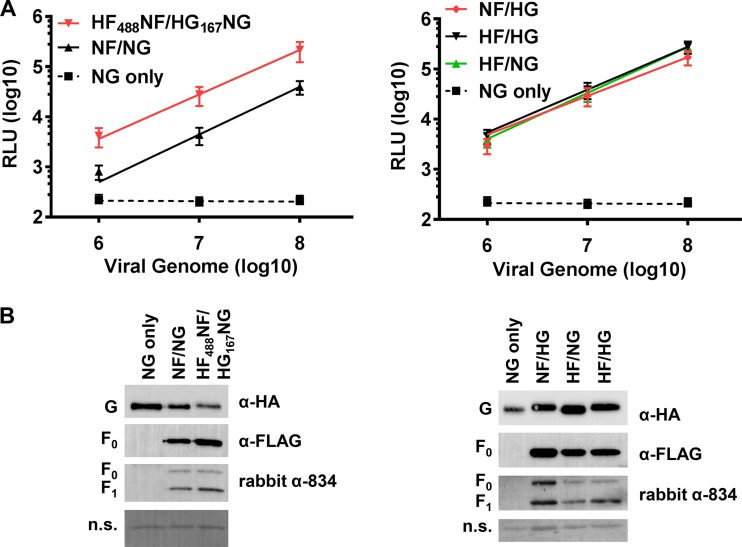
Viral entry is enhanced by the strongly hyperfusogenic glycoprotein combination HF488NF/HG167NG.
It is thought that the mechanism of viral entry (virus-cell membrane fusion) is generally closely related to the mechanism of cell-cell membrane fusion (49), although we have reported that the two processes do not always correlate (10, 50). Thus, we asked whether the highly hyperfusogenic combination HF488NF/HG167NG (2.6-fold above wild-type levels) (Fig. 7A) would yield increased levels of viral entry. To do so, we made use of our previously established BSL-2 pseudotyped viral entry assay. Briefly, HeV or NiV F or G wild-type or chimeric proteins were pseudotyped onto vesicular stomatitis virus (VSV) that lacks its own glycoprotein but contains the Renilla luciferase reporter gene in lieu of the VSV G gene (VSVΔG-rLuc) (11, 19). Pseudotyped virus carrying NiV G but lacking F (NG only) was used as a negative-control virus to control for nonspecific entry of virions via non-virus-cell membrane fusion mechanisms.
To accurately compare viral entry levels, we determined pseudotyped VSV genome concentrations by using quantitative reverse transcription-PCR (see Materials and Methods), as we previously established (11). We normalized recombinant VSV-rLuc (rVSV) virions to equal viral genome copy numbers and used 10-fold serial dilutions to infect Vero cells. Target Vero cells were lysed 20 to 24 h postinfection and monitored for luciferase activity, a direct measurement of viral entry. Equal copy numbers of rVSV were separated by 10% PAGE and analyzed by Western blot analysis for F and G glycoproteins using anti-F (mouse α-FLAG, rabbit 834) and anti-G (rabbit α-HA) specific antibodies. Overall, we found that the glycoprotein incorporation rates for NF/NG and HF488NF/HG167NG combinations were much lower than those of the NF/HG, HF/NG, and HF/HG combinations. Therefore, we decided to only compare the combinations with the lower G incorporation rate (NF/NG and HF488NF/HG167NG) to each other and the combinations with the higher G incorporation rate (NF/HG, HF/NG, and HF/HG) to one another (Fig. 8, left versus right, respectively). G and F incorporation into VSV virions was roughly similar for NF/NG and HF488NF/HG167NG (Fig. 8B, left) and for NF/HG, HF/NG, and HF/HG (Fig. 8B, right). Since F2 was very difficult to detect by Western blot analysis using an anti-FLAG antibody, we also used F-specific polyclonal antiserum (rabbit 834) to show that F was efficiently processed. The hyperfusogenic combination (HF488NF/HG167NG) showed 5- to 6-fold greater viral entry levels than the wild-type NF/NG combination, which correlated with the hyperfusogenic phenotype (FIMean, 2.64) (Fig. 7A and 8A, left). However, the hyperfusogenic HF/NG (FIMean, 1.81) and hypofusogenic NF/HG (FIMean, 0.42) combinations showed viral entry levels similar to that of the HF/HG combination (Fig. 8A, right). Recently, we also observed for various NiV and HeV glycoprotein N-glycan mutants that viral entry and cell-cell fusion mechanisms do not always correlate, as previously thought (8, 11, 12). Generally, however, here and in prior studies we have observed that viral entry appears to be enhanced for hyperfusogenic glycoprotein mutants to fuse cells above a certain threshold.
FIG 8.
Viral entry of the hyperfusogenic HF488NF/HG167NG protein pair is enhanced compared to that of the NF/NG combination. (A and B) Viral entry (A) and viral glycoprotein incorporation (B) levels are shown. Vero cells were infected with serial dilutions of HNV/VSV-rLuc pseudotyped virions containing either WT (NF/NG) or chimeric G and F (HF488NF/HG167NG) (A, left) or WT (HF/HG) or the heterotypic combinations NF/HG or HF/NG (A, right). VSV-rLuc carrying NG only is unable to enter cells efficiently and therefore was used as a negative control (NG only). Cells were lysed 20 to 24 h postinfection, and relative light units (RLU) were quantified and plotted against the number of viral genomes/ml. Data shown are averages ± SEM from at least four independent experiments. (B) Equivalent amount of viruses (4 × 1010 viral particles) used in panel A were separated by 10% SDS-PAGE and immunoblotted with G (rabbit α-HA) or F (mouse α-FLAG or rabbit α-834) specific antibodies; one representative experiment out of four is shown.
DISCUSSION
Glycoprotein pairs from different viruses (heterotypic) are mostly either unable to mediate fusion or mediate fusion at a considerably lower level than homotypic glycoprotein pairs (36, 51, 52). However, efficient heterotypic fusion has been reported among morbilliviruses, using measles virus H and strain-specific canine distemper F combinations (29). In such a study, four key amino acids in the N-terminal region of F were critical for a productive interaction with measles virus H. Interestingly, we found that heterotypic fusion with HeV and NiV glycoproteins occurs with relatively high efficiency (36, 37). Bossart et al. observed that the homologous HeV glycoproteins fused relatively more efficiently than the NiV glycoproteins using a vaccinia T7 expression system (36). Heterotypic cell-cell fusion was observed, and Bossart et al. speculated that the fusion potency correlates with the fusogenicity of the F protein. However, that study did not quantify the glycoprotein CSE levels, which is crucial, as we and others have shown that membrane fusion levels are highly dependent on glycoprotein CSE levels (11, 38).
Our study, which takes into account glycoprotein CSE levels, indicates that homotypic HeV or NiV glycoproteins promote comparable levels of cell-cell fusion (Fig. 2B and 7A). Additionally, the membrane fusion capacities of heterotypic glycoprotein combinations varied and were dependent on both the F and the G glycoproteins (Fig. 2B and 7A). Further, a recent study that utilized a reverse genetics system to construct recombinant NiV (rNiV-mCherry) showed that both HeV glycoproteins in the context of Nipah virus (rNiV-mCherry HeV F/G) induced lower levels of cell-cell fusion than wild-type rNiV-mCherry but similar levels of viral entry (37). However, the reciprocal rHeV-mCherry system was not analyzed in that study; thus, it is possible that a match between the F/G pairs and other viral proteins is necessary to achieve optimal fusion levels. Nonetheless, neither the vaccinia T7 system nor the rNiV-mCherry system allowed for normalization of the different glycoproteins’ CSE levels. We created a system that allows for direct comparison of NiV and HeV membrane fusion capacities by the glycoproteins by normalizing glycoprotein CSE levels between the two viruses without affecting glycoprotein function. We found that the HeV G glycoprotein is less fusogenic in both homo- and heterotypic F glycoprotein combinations than NiV G. Further, we found that HeV F bearing homo- and heterotypic G glycoprotein combinations resulted in enhanced fusion levels compared to those of NiV F combinations (Fig. 7A). In conclusion, heterotypic fusion was highly increased or decreased depending on the viral origin of the glycoproteins. In somewhat of a contrast, for the morbilliviruses the importance between heterotypic fusion and the origin of the attachment protein was shown (35).
Both cell-cell fusion and coimmunoprecipitation experiments revealed that HeV and NiV glycoproteins are able to efficiently interact structurally and functionally. All F interactions with HeV G showed stronger binding avidities than those with NiV G, which can be attributed to both the head and the stalk domains in HeV G (Fig. 7B). Generally, the binding avidities inversely correlated with the respective potencies of fusogenicity, similar to what has been observed for many NiV glycoprotein mutants, including N-glycosylation mutants (Fig. 7C) (8, 11, 19). This provides evidence for a G/F dissociation model not only for NiV but also for the henipaviral genus, whereby G/F dissociation is crucial for the fusion process even for heterologous henipaviral glycoprotein pairs, although this model may be part of a more comprehensive safety-catch model. We find it remarkable that HG displayed a stronger binding avidity to NF than to its cognate HF (avidity, 2.83 and 1.60, respectively; P < 0.0001). Whether the relatively stronger avidity of HG and NF binding is due to protein residues and/or N- or O-glycan differences remains to be determined. Interestingly, our F-triggering studies further revealed that syncytium levels were likely a result of membrane fusion steps prior to or coincident with F triggering, as F-triggering levels correlated with the final cell-cell fusion phenotypes (Fig. 2D). This is important in our understanding of the role of the G-F interactions in the process of henipaviral membrane fusion triggering.
Henipaviruses are unique within the paramyxovirus family in that G and F are believed to traffic independently within the cell and do not interact with each other prior to initial cell surface transport (53). Interestingly, we observed that the hypofusogenic NF/HG combination appeared to show slightly lower G and F CSE levels than the homotypic NF/NG combination (Fig. 2A) but similar cellular lysate levels (Fig. 6A). It is unclear whether the relative intracellular retention observed is due to the stronger NF-HG interactions within the cell prior to cell surface transport. The reduced cell surface transport may be partially responsible for the hypofusogenic NF/HG phenotype, although for proper interpretation fusion levels were normalized to CSE levels. If NF and HG do not interact at all prior to cell surface transport, then it is conceivable that the glycoproteins affect each other during the endosomal recycling process necessary for the activation of F by cathepsin L cleavage.
We and others have reported the importance of the G/H/HN stalk domain in promoting membrane fusion (10, 32, 33). One of our studies showed that chimeras containing the NiV-G head domain and the NDV HN stalk domain could bind ephrinB2 and trigger fusion mediated by NDV F (28). In the present study, to elucidate the protein elements responsible for the fusion phenotypes observed, we created G chimeras in which we exchanged the CT/TM/stalk (residues 1 to 167) or head (residues 168 to 604) domain between HeV and NiV G. Functional properties of the cytoplasmic, stalk, and head domains of G have been described somewhat (54–57). Our G chimeras revealed that the CT/TM/stalk domain of HeV G is a main determinant of the hypofusogenic NF/HG phenotype and that this may in part be attributed to a stronger binding avidity of the HG CT/TM/stalk domain to NF. In contrast, we could not identify a specific region within NG that was solely responsible for its hyperfusogenic properties, as both the head and the stalk domains appeared to be important. Notably, the exchange in functional domains did not affect CSE levels or budding efficiencies of chimeric Gs from the cell surface when expressed in the absence of F (data not shown). Recently, Herren et al. described the importance of the connector/linker residues between the head and stalk domains of MeV H and CDV H for the formation of stable H dimers of dimers and receptor-induced F triggering (47). Since the homologous connector domain in NiV and HeV is identical in both henipaviruses, it may not play as important a role, as oligomerization patterns were not significantly different between NG, HG, NG167HG, and HG167NG (Fig. 4B). Sawatsky et al. showed that CDV H containing a NiV-G CT domain maintained stable cell surface expression and fusion capabilities (55). In contrast, NiV-G containing the CDV H CT domain had abrogated expression and fusion activity. In the present study, we aimed to determine whether differences in fusion were attributed to either the head or stalk regions of the attachment glycoprotein. However, future studies may further define the glycoprotein regions involved by targeting relatively more conserved domains downstream of the stalk, such as the transmembrane or cytoplasmic tail regions.
To elucidate the regions in HeV F that may be responsible for the enhanced fusion observed in homo- and heterotypic G glycoprotein combinations, we created chimeras by exchanging the TM/CT domains between the HeV and NiV F glycoproteins. We found that the viral origin of the F head domain dominantly determined the membrane fusion phenotypes. Additionally, the NiV F TM/CT domain was able to enhance the ability of HeV F to induce cell-cell fusion (Fig. 5, HF488NF). Avila et al. showed that inserting the MeV F central region into the CDV F protein resulted in less stable prefusion F conformations, allowing for the heterotypic MeV H and CD46 receptor to induce fusion (35). However, the homologous central regions in NiV and HeV are very conserved and likely do not account for the observed differences in fusion.
Viral entry levels overall were similar between the homotypic and one of the heterotypic F and G combinations, which matches the results of a recent study that found that swapping the glycoproteins between HeV and NiV using a reassortant NiV did not have any effect on viral replication but did have an effect on cell-cell fusion (37). However, with the highly hyperfusogenic combination HF488NF/HG167NG, we observed over half a log increase in viral entry (Fig. 8A, left). Whether the higher level of cell-cell hyperfusogenicity is relevant to the pathogenicity of the henipaviruses remains to be determined (58). According to a recent study coming from the related pneumovirus field, increased in vitro cell-cell fusion generally correlated with increased early viral loads but not increased levels of airway mucin expression, a marker for pathogenicity (59). It is possible that a certain level of cell-cell fusion has to be reached in order to observe an increase in viral entry. However, the relationship between cell-cell fusion activity and viral pathogenicity is complex and remains understudied.
Finally, the results in this study may have implications for improving henipavirus vaccine development. VLP-based henipaviral vaccines using the matrix (M) and the F and G glycoproteins recently have been shown to protect against NiV disease in a hamster model (3). Vaccine formulations composed of chimeric G or F glycoproteins or glycoproteins from two different henipaviruses may improve cross-protection against both HeV and NiV. Although neutralizing antibodies appear to be directed more heavily against the G glycoprotein than the F glycoprotein, F may also contribute to host immune responses. Further, VLP or pseudotyped rVSV cell entry can be enhanced by incorporating chimeric glycoproteins such as HF488NF/HG167NG. This may enhance vaccine efficiency by enhancing VLP or rVSV entry into cells for better presentation to the immune system, as, for example, dendritic cells have been shown to support a productive NiV infection (60).
MATERIALS AND METHODS
Expression plasmids and site-directed and overlapping PCR mutagenesis.
Codon-optimized HeV G and NiV G genes were cloned within the KpnI and XhoI restriction sites of the pcDNA3.1(+) vector (Invitrogen, NY). The codon-optimized NiV and HeV F genes were cloned within KpnI and XhoI restriction sites of the pCAGGS vector (8). The codon-optimized NiV G sequence was as described in the GenBank database (AAV80425.1), except that the nucleotides that code for the first glycine after the start codon were removed, since that glycine is not present in the virus. The removal of the glycine did not affect the fusogenic capacities of NiV G (data not shown). G proteins had a C-terminal HA tag (YPYDVPDYA) and F proteins had a C-terminal AU1 tag (DTYRYI), as previously described (8). Where indicated, F proteins with an internal FLAG tag (DYKDDDDK) were constructed and utilized.
FLAG tag insertion into the C-terminal region of NiV or HeV F2 was accomplished by site-directed mutagenesis using the QuikChange II XL site-directed mutagenesis kit from Agilent according to the manufacturer’s instructions. FLAG tag insertion into NiV F was accomplished with primer pair NiVF_FLAG_aa114-F (5′-CAACACCCACGACCTGGATTACAAGGATGACGACGATAAGGTGGGCGACGTGCGGCTG-3′) and NiVF_FLAG_aa114-R (5′-CAGCCGCACGTCGCCCACCTTATCGTCGTCATCCTTGTAATCCAGGTCGTGGGTGTTG-3′) and FLAG tag insertion into HeV F with primer pair HeVF_Flag_aa114-F (5′-TACAACAACAACACCCACGACCTGGATTACAAGGATGACGACGATAAGGTGGGCGACGTGAAGCTG-3′) and HeVF_FLAG_aa114-R (5′-CAGCTTCACGTCGCCCACCTTATCGTCGTCATCCTTGTAATCCAGGTCGTGGGTGTTGTTGTTGTA-3′).
The F chimeras (NF488HF and HF488NF) as well as the G chimeras (NG167HG and HG167NG) were constructed by overlapping PCR. To construct the F chimeras, we used NF488HF_F (5′-CTGTACGTGCTGAGCATCGCCGCCCTGTGTATCGGCCTGATC-3′) and HF488NF_F (5′-CTGTATGTGCTGTCCATCGCCAGCCTGTGCATCGGCCTGATC-3′) in combination with HeV or NiV F specific forward and reverse primers HeVF_KpnI-F (TTGGTACCGCCACCATGGCCACCCAGGAAGTG), NiVF_KpnI-F (5′-ATGGTACCGCCACCATGGTGGTGATCCTGGAC-3′), and HeVF/NiVF_XhoI-R (5′-AACTCGAGTCATCAGATGTACCGGTAGGTGTC-3′). To construct the G chimeras, we used NG167HG_F/HG167NG_F (5′-GCAAGTTCACCCTGCCCCCCCTGAAGATCCACGAG-3′) and NG167HG_R/HG167NG_R (5′-CTCGTGGATCTTCAGGGGGGGCAGGGTGAACTTGC-3′) in combination with HeV (HeVG-KpnI-F [5′-TTGGTACCGGCCGCATGATGGCCGACAGCAAGCTG-3′] and HeVG-XhoI-R [5′-AACTCGAGTCAGGCGTAATCGGGCACG-3′]) or NiV G specific primers (NiVG-KpnI-F [5′-TTGGTACCGGCCGCATGCCTGCCGAGAACAAGAAAGTG-3′] and NiVG-XhoI-R [5′-AACTCGAGTCAGGCGTAGTCGGGCACG-3′]).
The sequences of all constructs were verified by DNA sequencing (Eurofins, AL).
Cell lines.
HEK293T cells were maintained in Dulbecco’s modified Eagle medium (DMEM) and Vero cells were cultured in minimal essential medium (MEM), both supplemented with 10% fetal bovine serum (FBS), 50 IU of penicillin ml−1, 50 μg of streptomycin ml−1, and 2 mM glutamine.
Cell-cell fusion.
Six-well plates of HEK293T cells (70% to 80% confluence) were transfected with wild-type or mutant G and/or F expression plasmids (1.6 μg and/or 0.4 μg, respectively) in the presence of Lipofectamine 2000 according to the manufacturer’s recommendations (Invitrogen). Sixteen to 20 h posttransfection (hpt), cells were fixed with 1% paraformaldehyde and syncytial nuclei (4 or more nuclei per cell) were counted in each microscopic field (200×). Five microscopic fields were counted for each transfection, as previously established (10, 11).
Quantification of F and G cell surface expression and ephrinB2 binding by flow cytometry.
Six-well plates of 70% to 80% confluent HEK293T cells were transfected as described above (cell-cell fusion assay). Cells transfected with G or F only were transfected with the same amount of G and F as described above, and empty vector (pCAGGS or pcDNA3.1, respectively) was added to bring up the total DNA content to 2 μg. Sixteen to 20 h posttransfection, cells were collected in 10 mM ice-cold EDTA and washed twice with fluorescence-associated cell sorting (FACS) buffer (1% FBS in PBS). Transfected cells were incubated with rabbit anti-HA (1:400; Bethyl Laboratories, TX, USA) for the detection of G glycoproteins and with mouse anti-FLAG M2 (1:400; Millipore-Sigma, MO, USA) or mouse anti-AU1 (1:400; Bethyl Laboratories, TX, USA) for the detection of F glycoproteins at 4°C for 1 h. Cells were washed twice with FACS buffer (1% FBS in PBS) and incubated with fluorescently labeled anti-rabbit Alexa Fluor 647 and anti-mouse Alexa Fluor 488 antibodies (1:400; Life Technologies, NY) for 45 min at 4°C. Cells were washed twice as described above, fixed in 0.5% paraformaldehyde, and analyzed by flow cytometry (Guava easyCyte8 HT; EMD Millipore, MA).
For detection of ephrinB2 binding, HEK293T cells were transfected with 2 μg WT or chimeric NiV/HeV G expression plasmids and collected at 16 to 20 h posttransfection. Cells transfected with vector alone (pcDNA3.1) served as a negative control. Cells expressing WT or chimeric NiV/HeV G proteins were incubated with rabbit anti-HA (1:400) as a normalization control for cell surface expression or soluble recombinant mouse ephrinB2/human Fc chimera (10 nM; R&D Systems, MN) at 4°C for 1 h. Cells were washed twice with FACS buffer and incubated with fluorescently labeled anti-human Alexa Fluor 647 or anti-rabbit Alexa Fluor 488 antibodies (1:400; Life Technologies, NY) for 45 min at 4°C. Cells were washed, fixed, and analyzed as described above. Soluble mouse ephrinB2/human Fc chimera contains the ectodomain of mouse ephrinB2 (residues 27 to 227).
Reducing/nonreducing SDS-PAGE and immunoblotting.
HEK293T cells were transfected as described above and lysed in 1× radioimmunoprecipitation assay buffer (EMD Millipore, MA) supplemented with protease inhibitors (cOmplete Mini; Roche, IN) 16 to 24 hpt. Cell lysates or VSV-F and/or -G-rLuc pseudotyped virions were subjected to SDS-PAGE and immunoblotting. A total of 4 × 1010 virions (genome copies) were separated by reducing (10%) SDS-PAGE. G and F proteins were detected using rabbit anti-HA (1:2,000) and mouse anti-AU1 (1:500) or mouse anti-FLAG (1:500) antibodies. Fluorescently labeled secondary antibodies (1:2,000) were used as described above to increase the quantitative nature of our detection, and proteins were detected and quantitated using a ChemiDoc MP Imager system with Image Lab software (Bio-Rad, CA). For nonreducing SDS-PAGE, samples were neither treated with β-mercaptoethanol nor denatured by heat. Nonreducing SDS-PAGE samples were detected using phycoerythrin (PE)-conjugated anti-HA antibodies (1:1,000) (Miltenyi, Germany).
Coimmunoprecipitation.
Two μg (1.6 μg F and 0.4 μg G) of total DNA was transfected per well of a 6-well plate of HEK293T cells (∼90% confluence) using Lipofectamine 2000. Twenty-four hpt, cells from 3 wells were processed for each transfection condition. Cells were washed with PBS and resuspended in a total of 600 μl ice-cold lysis buffer provided with the μMACS epitope tag protein isolation kit (Miltenyi, Germany) and supplemented with proteinase inhibitor (Roche Mini). Cells were lysed on ice for 30 min with occasional mixing. Cells were centrifuged at 10,000 × g for 10 min at 4°C to remove cellular debris. A sixth of the lysate was set aside for immunoblot analysis and the rest was used for immunoprecipitation, as outlined by the manufacturer, with some minor modifications. Briefly, 40 μl of anti-tag beads was added to the lysate and incubated for 1 h at 4°C while rotating. μ Columns were prepared as described by the manufacturer. Lysate was run over the column, and beads were washed five times (350 μl four times and a final 100-μl washing step). Twenty μl preheated elution buffer (70°C) was added to the column before eluting the bound immunoprecipitated protein in 80 μl elution buffer. Forty μl of eluate was separated by 10% SDS-PAGE, and proteins were detected by immunoblotting.
Pseudotyped HeV and NiV/VSV-rLuc production, quantitative PCR, and viral entry quantification.
Virus stocks were produced in HEK293T cells as described previously (8, 9). Briefly, two 15-cm dishes of HEK293T cells were each transfected in the presence of 33 μg polyethylenimine (Polysciences) with combinations of F and/or G expression plasmids (48 μg F and 12 μg G), as outlined in Results. Sixteen to 20 h later the transfected cells were infected with recombinant VSV-ΔG-rLuc. VSV-rLuc pseudotyped virions were purified and viral genome copy numbers were measured as described in detail previously (8).
To quantify viral entry, Vero cells were seeded in a 96-well plate and infected at roughly 50% confluence using 10-fold serial virus dilutions. Infections were done for 2 h in infection medium (PBS plus 1% FBS). Luciferase activity was measured in relative light units and plotted against genome copy numbers per ml in GraphPad Prism 7 as previously outlined (8).
F-triggering assay.
F-triggering assays were performed as previously described (27), with minor modifications for optimization. HEK293T cells were transfected with combinations of pCAGGS-NiV F (NF) or -HeV F (HF) and pcDNA3.1 NiV G (NG) or HeV G (HG) vectors in a 4:1 ratio (1.6 μg plus 0.4 μg). Cells were collected 10 h posttransfection, before transfected cells exhibited high levels of fusion. Cells were resuspended in PBS containing 1% bovine serum albumin and incubated at 4°C for 90 min in the presence of 1 μM HR2-Cy5 peptide (Cy5-KVDISSQISSMNQSLQQSKDYIKEAQRLLDTVNPSL). Subsequently, cells were placed at 37°C for ∼30 min to allow F triggering. Cells then were washed and fixed in 1% paraformaldehyde. HR2-Cy5 peptide bound to triggered NiV F was detected by flow cytometric analysis. Cells were split to detect both F triggering and cell surface expression of F and G (as described above).
DSP quantitative fusion assay.
Effector HEK293T cells were seeded into 96-well plates and transfected with wild-type or chimeric G and/or F expression plasmids and a dual-split protein (DSP1–7) plasmid. For negative controls, pcDNA and pCAGGS vectors were used along with dual-split protein (DSP1–7) plasmid. Target HEK293T cells were transfected with ephrinB2 plasmid and DSP8–11. Twelve hpt, cells were washed extensively with PBS. Subsequently, EnduRen (Promega) substrate was added according to the manufacturer’s instructions and target cells were lifted, mixed, and incubated with effector cells at a 1:1 ratio. After 8 h at 37°C, Renilla luciferase activity was measured using a Tecan Spark plate reader.
Statistical analysis.
Data were analyzed with GraphPad Prism 7 and 8, and statistical significance was determined by a one-way ANOVA statistical analysis followed by a Tukey pairwise multiple-comparison test. The data represent averages ± standard errors of the means (SEM) from multiple experiments as indicated.
ACKNOWLEDGMENTS
This study was supported by NIH/NIAID R01 grant AI109022 and R21 grant AI142377 to H.A.C. and by DARPA PREEMPT program Cooperative Agreement D18AC00031. The content of the information does not necessarily reflect the position or the policy of the U.S. government, and no official endorsement should be inferred.
We thank Richard Plemper from Georgia State University for providing us the GFP and luciferase dual-split protein expression plasmids.
REFERENCES
- 1.Ching PK, de los Reyes VC, Sucaldito MN, Tayag E, Columna-Vingno AB, Malbas FF Jr, Bolo GC Jr, Sejvar JJ, Eagles D, Playford G, Dueger E, Kaku Y, Morikawa S, Kuroda M, Marsh GA, McCullough S, Foxwell AR. 2015. Outbreak of henipavirus infection, Philippines, 2014. Emerg Infect Dis 21:328–331. doi: 10.3201/eid2102.141433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weatherman S, Feldmann H, de Wit E. 2018. Transmission of henipaviruses. Curr Opin Virol 28:7–11. doi: 10.1016/j.coviro.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walpita P, Cong Y, Jahrling PB, Rojas O, Postnikova E, Yu S, Johns L, Holbrook MR. 2017. A VLP-based vaccine provides complete protection against Nipah virus challenge following multiple-dose or single-dose vaccination schedules in a hamster model. NPJ Vaccines 2:21. doi: 10.1038/s41541-017-0023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broder CC, Xu K, Nikolov DB, Zhu Z, Dimitrov DS, Middleton D, Pallister J, Geisbert TW, Bossart KN, Wang LF. 2013. A treatment for and vaccine against the deadly Hendra and Nipah viruses. Antiviral Res 100:8–13. doi: 10.1016/j.antiviral.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geisbert TW, Mire CE, Geisbert JB, Chan YP, Agans KN, Feldmann F, Fenton KA, Zhu Z, Dimitrov DS, Scott DP, Bossart KN, Feldmann H, Broder CC. 2014. Therapeutic treatment of Nipah virus infection in nonhuman primates with a neutralizing human monoclonal antibody. Sci Transl Med 6:242ra282. doi: 10.1126/scitranslmed.3008929.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler D. 2017. Billion-dollar project aims to prep vaccines before epidemics hit. Nature 541:444–445. doi: 10.1038/nature.2017.21329. [DOI] [PubMed] [Google Scholar]
- 7.Drexler JF, Corman VM, Müller MA, Maganga GD, Vallo P, Binger T, Gloza-Rausch F, Cottontail VM, Rasche A, Yordanov S, Seebens A, Knörnschild M, Oppong S, Adu Sarkodie Y, Pongombo C, Lukashev AN, Schmidt-Chanasit J, Stöcker A, Carneiro AJB, Erbar S, Maisner A, Fronhoffs F, Buettner R, Kalko EKV, Kruppa T, Franke CR, Kallies R, Yandoko ERN, Herrler G, Reusken C, Hassanin A, Krüger DH, Matthee S, Ulrich RG, Leroy EM, Drosten C. 2012. Bats host major mammalian paramyxoviruses. Nat Commun 3:796. doi: 10.1038/ncomms1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradel-Tretheway BG, Liu Q, Stone JA, McInally S, Aguilar HC. 2015. Novel functions of hendra virus G N-glycans and comparisons to Nipah virus. J Virol 89:7235–7247. doi: 10.1128/JVI.00773-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Negrete OA, Levroney EL, Aguilar HC, Bertolotti-Ciarlet A, Nazarian R, Tajyar S, Lee B. 2005. EphrinB2 is the entry receptor for Nipah virus, an emergent deadly paramyxovirus. Nature 436:401–405. doi: 10.1038/nature03838. [DOI] [PubMed] [Google Scholar]
- 10.Liu Q, Stone JA, Bradel-Tretheway B, Dabundo J, Benavides Montano JA, Santos-Montanez J, Biering SB, Nicola AV, Iorio RM, Lu X, Aguilar HC. 2013. Unraveling a three-step spatiotemporal mechanism of triggering of receptor-induced Nipah virus fusion and cell entry. PLoS Pathog 9:e1003770. doi: 10.1371/journal.ppat.1003770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aguilar HC, Matreyek KA, Filone CM, Hashimi ST, Levroney EL, Negrete OA, Bertolotti-Ciarlet A, Choi DY, McHardy I, Fulcher JA, Su SV, Wolf MC, Kohatsu L, Baum LG, Lee B. 2006. N-glycans on Nipah virus fusion protein protect against neutralization but reduce membrane fusion and viral entry. J Virol 80:4878–4889. doi: 10.1128/JVI.80.10.4878-4889.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biering SB, Huang A, Vu AT, Robinson LR, Bradel-Tretheway B, Choi E, Lee B, Aguilar HC. 2012. N-glycans on the Nipah virus attachment glycoprotein modulate fusion and viral entry as they protect against antibody neutralization. J Virol 86:11991–12002. doi: 10.1128/JVI.01304-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Broder CC, Weir DL, Reid PA. 2016. Hendra virus and Nipah virus animal vaccines. Vaccine 34:3525–3534. doi: 10.1016/j.vaccine.2016.03.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guillaume V, Contamin H, Loth P, Georges-Courbot MC, Lefeuvre A, Marianneau P, Chua KB, Lam SK, Buckland R, Deubel V, Wild TF. 2004. Nipah virus: vaccination and passive protection studies in a hamster model. J Virol 78:834–840. doi: 10.1128/JVI.78.2.834-840.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang A, Dutch RE. 2012. Paramyxovirus fusion and entry: multiple paths to a common end. Viruses 4:613–636. doi: 10.3390/v4040613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connolly SA, Leser GP, Jardetzky TS, Lamb RA. 2009. Bimolecular complementation of paramyxovirus fusion and hemagglutinin-neuraminidase proteins enhances fusion: implications for the mechanism of fusion triggering. J Virol 83:10857–10868. doi: 10.1128/JVI.01191-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bossart KN, Fusco DL, Broder CC. 2013. Paramyxovirus entry. Adv Exp Med Biol 790:95–127. doi: 10.1007/978-1-4614-7651-1_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aguilar HC, Henderson BA, Zamora JL, Johnston GP. 2016. Paramyxovirus glycoproteins and the membrane fusion process. Curr Clin Microbiol Rep 3:142–154. doi: 10.1007/s40588-016-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguilar HC, Matreyek KA, Choi DY, Filone CM, Young S, Lee B. 2007. Polybasic KKR motif in the cytoplasmic tail of Nipah virus fusion protein modulates membrane fusion by inside-out signaling. J Virol 81:4520–4532. doi: 10.1128/JVI.02205-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plemper RK, Hammond AL, Gerlier D, Fielding AK, Cattaneo R. 2002. Strength of envelope protein interaction modulates cytopathicity of measles virus. J Virol 76:5051–5061. doi: 10.1128/JVI.76.10.5051-5061.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plemper RK, Hammond AL, Cattaneo R. 2001. Measles virus envelope glycoproteins hetero-oligomerize in the endoplasmic reticulum. J Biol Chem 276:44239–44246. doi: 10.1074/jbc.M105967200. [DOI] [PubMed] [Google Scholar]
- 22.Brindley MA, Chaudhury S, Plemper RK. 2015. Measles virus glycoprotein complexes preassemble intracellularly and relax during transport to the cell surface in preparation for fusion. J Virol 89:1230–1241. doi: 10.1128/JVI.02754-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bose S, Jardetzky TS, Lamb RA. 2015. Timing is everything: fine-tuned molecular machines orchestrate paramyxovirus entry. Virology 479:518–531. doi: 10.1016/j.virol.2015.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jardetzky TS, Lamb RA. 2014. Activation of paramyxovirus membrane fusion and virus entry. Curr Opin Virol 5:24–33. doi: 10.1016/j.coviro.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Negrete OA, Wolf MC, Aguilar HC, Enterlein S, Wang W, Muhlberger E, Su SV, Bertolotti-Ciarlet A, Flick R, Lee B. 2006. Two key residues in ephrinB3 are critical for its use as an alternative receptor for Nipah virus. PLoS Pathog 2:e7. doi: 10.1371/journal.ppat.0020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu K, Chan YP, Bradel-Tretheway B, Akyol-Ataman Z, Zhu Y, Dutta S, Yan L, Feng Y, Wang LF, Skiniotis G, Lee B, Zhou ZH, Broder CC, Aguilar HC, Nikolov DB. 2015. Crystal structure of the pre-fusion Nipah virus fusion glycoprotein reveals a novel hexamer-of-trimers assembly. PLoS Pathog 11:e1005322. doi: 10.1371/journal.ppat.1005322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aguilar HC, Aspericueta V, Robinson LR, Aanensen KE, Lee B. 2010. A quantitative and kinetic fusion protein-triggering assay can discern distinct steps in the Nipah virus membrane fusion cascade. J Virol 84:8033–8041. doi: 10.1128/JVI.00469-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mirza AM, Aguilar HC, Zhu Q, Mahon PJ, Rota PA, Lee B, Iorio RM. 2011. Triggering of the Newcastle disease virus fusion protein by a chimeric attachment protein that binds to Nipah virus receptors. J Biol Chem 286:17851–17860. doi: 10.1074/jbc.M111.233965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JK, Prussia A, Paal T, White LK, Snyder JP, Plemper RK. 2008. Functional interaction between paramyxovirus fusion and attachment proteins. J Biol Chem 283:16561–16572. doi: 10.1074/jbc.M801018200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miest TS, Yaiw KC, Frenzke M, Lampe J, Hudacek AW, Springfeld C, von Messling V, Ungerechts G, Cattaneo R. 2011. Envelope-chimeric entry-targeted measles virus escapes neutralization and achieves oncolysis. Mol Ther 19:1813–1820. doi: 10.1038/mt.2011.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Talekar A, Moscona A, Porotto M. 2013. Measles virus fusion machinery activated by sialic acid binding globular domain. J Virol 87:13619–13627. doi: 10.1128/JVI.02256-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bose S, Zokarkar A, Welch BD, Leser GP, Jardetzky TS, Lamb RA. 2012. Fusion activation by a headless parainfluenza virus 5 hemagglutinin-neuraminidase stalk suggests a modular mechanism for triggering. Proc Natl Acad Sci U S A 109:E2625–E2634. doi: 10.1073/pnas.1213813109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brindley MA, Suter R, Schestak I, Kiss G, Wright ER, Plemper RK. 2013. A stabilized headless measles virus attachment protein stalk efficiently triggers membrane fusion. J Virol 87:11693–11703. doi: 10.1128/JVI.01945-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wild TF, Fayolle J, Beauverger P, Buckland R. 1994. Measles virus fusion: role of the cysteine-rich region of the fusion glycoprotein. J Virol 68:7546–7548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Avila M, Alves L, Khosravi M, Ader-Ebert N, Origgi F, Schneider-Schaulies J, Zurbriggen A, Plemper RK, Plattet P. 2014. Molecular determinants defining the triggering range of prefusion F complexes of canine distemper virus. J Virol 88:2951–2966. doi: 10.1128/JVI.03123-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bossart KN, Wang LF, Flora MN, Chua KB, Lam SK, Eaton BT, Broder CC. 2002. Membrane fusion tropism and heterotypic functional activities of the Nipah virus and Hendra virus envelope glycoproteins. J Virol 76:11186–11198. doi: 10.1128/JVI.76.22.11186-11198.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yun T, Park A, Hill TE, Pernet O, Beaty SM, Juelich TL, Smith JK, Zhang LH, Wang YE, Vigant F, Gao JL, Wu P, Lee B, Freiberg AN. 2015. Efficient reverse genetics reveals genetic determinants of budding and fusogenic differences between Nipah and Hendra viruses and enables real-time monitoring of viral spread in small animal models of henipavirus infection. J Virol 89:1242–1253. doi: 10.1128/JVI.02583-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whitman SD, Dutch RE. 2007. Surface density of the Hendra G protein modulates Hendra F protein-promoted membrane fusion: role for Hendra G protein trafficking and degradation. Virology 363:419–429. doi: 10.1016/j.virol.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu Z, Dimitrov AS, Bossart KN, Crameri G, Bishop KA, Choudhry V, Mungall BA, Feng YR, Choudhary A, Zhang MY, Feng Y, Wang LF, Xiao X, Eaton BT, Broder CC, Dimitrov DS. 2006. Potent neutralization of Hendra and Nipah viruses by human monoclonal antibodies. J Virol 80:891–899. doi: 10.1128/JVI.80.2.891-899.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Avila M, Khosravi M, Alves L, Ader-Ebert N, Bringolf F, Zurbriggen A, Plemper RK, Plattet P. 2015. Canine distemper virus envelope protein interactions modulated by hydrophobic residues in the fusion protein globular head. J Virol 89:1445–1451. doi: 10.1128/JVI.01828-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ader N, Brindley M, Avila M, Orvell C, Horvat B, Hiltensperger G, Schneider-Schaulies J, Vandevelde M, Zurbriggen A, Plemper RK, Plattet P. 2013. Mechanism for active membrane fusion triggering by morbillivirus attachment protein. J Virol 87:314–326. doi: 10.1128/JVI.01826-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dutch RE, Joshi SB, Lamb RA. 1998. Membrane fusion promoted by increasing surface densities of the paramyxovirus F and HN proteins: comparison of fusion reactions mediated by simian virus 5 F, human parainfluenza virus type 3 F, and influenza virus HA. J Virol 72:7745–7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bossart KN, Mungall BA, Crameri G, Wang LF, Eaton BT, Broder CC. 2005. Inhibition of Henipavirus fusion and infection by heptad-derived peptides of the Nipah virus fusion glycoprotein. Virol J 2:57. doi: 10.1186/1743-422X-2-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnston GP, Contreras EM, Dabundo J, Henderson BA, Matz KM, Ortega V, Ramirez A, Park A, Aguilar HC. 2017. Cytoplasmic motifs in the Nipah virus fusion protein modulate virus particle assembly and egress. J Virol 91:e02150-16. doi: 10.1128/JVI.02150-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cifuentes-Munoz N, Sun W, Ray G, Schmitt PT, Webb S, Gibson K, Dutch RE, Schmitt AP. 2017. Mutations in the transmembrane domain and cytoplasmic tail of Hendra virus fusion protein disrupt virus-like-particle assembly. J Virol 91:e00152-17. doi: 10.1128/JVI.00152-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Behner L, Zimmermann L, Ringel M, Weis M, Maisner A. 2018. Formation of high-order oligomers is required for functional bioactivity of an African bat henipavirus surface glycoprotein. Vet Microbiol 218:90–97. doi: 10.1016/j.vetmic.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 47.Herren M, Shrestha N, Wyss M, Zurbriggen A, Plattet P. 2018. Regulatory role of the morbillivirus attachment protein head-to-stalk linker module in membrane fusion triggering. J Virol 92:e00679-18. doi: 10.1128/JVI.00679-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brindley MA, Takeda M, Plattet P, Plemper RK. 2012. Triggering the measles virus membrane fusion machinery. Proc Natl Acad Sci U S A 109:E3018–E3027. doi: 10.1073/pnas.1210925109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.White JM, Delos SE, Brecher M, Schornberg K. 2008. Structures and mechanisms of viral membrane fusion proteins: multiple variations on a common theme. Crit Rev Biochem Mol Biol 43:189–219. doi: 10.1080/10409230802058320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stone JA, Nicola AV, Baum LG, Aguilar HC. 2016. Multiple novel functions of henipavirus O-glycans: the first O-glycan functions identified in the Paramyxovirus family. PLoS Pathog 12:e1005445. doi: 10.1371/journal.ppat.1005445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bagai S, Lamb RA. 1995. Quantitative measurement of paramyxovirus fusion: differences in requirements of glycoproteins between simian virus 5 and human parainfluenza virus 3 or Newcastle disease virus. J Virol 69:6712–6719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nussbaum O, Broder CC, Moss B, Stern LB, Rozenblatt S, Berger EA. 1995. Functional and structural interactions between measles virus hemagglutinin and CD46. J Virol 69:3341–3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Whitman SD, Smith EC, Dutch RE. 2009. Differential rates of protein folding and cellular trafficking for the Hendra virus F and G proteins: implications for F-G complex formation. J Virol 83:8998–9001. doi: 10.1128/JVI.00414-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu Q, Bradel-Tretheway B, Monreal AI, Saludes JP, Lu X, Nicola AV, Aguilar HC. 2015. Nipah virus attachment glycoprotein stalk C-terminal region links receptor binding to fusion triggering. J Virol 89:1838–1850. doi: 10.1128/JVI.02277-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sawatsky B, Bente DA, Czub M, von Messling V. 2016. Morbillivirus and henipavirus attachment protein cytoplasmic domains differently affect protein expression, fusion support and particle assembly. J Gen Virol 97:1066–1076. doi: 10.1099/jgv.0.000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Porotto M, Doctor L, Carta P, Fornabaio M, Greengard O, Kellogg GE, Moscona A. 2006. Inhibition of Hendra virus fusion. J Virol 80:9837–9849. doi: 10.1128/JVI.00736-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palomares K, Vigant F, Van Handel B, Pernet O, Chikere K, Hong P, Sherman SP, Patterson M, An DS, Lowry WE, Mikkola HK, Morizono K, Pyle AD, Lee B. 2013. Nipah virus envelope-pseudotyped lentiviruses efficiently target ephrinB2-positive stem cell populations in vitro and bypass the liver sink when administered in vivo. J Virol 87:2094–2108. doi: 10.1128/JVI.02032-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dhondt KP, Horvat B. 2013. Henipavirus infections: lessons from animal models. Pathogens 2:264–287. doi: 10.3390/pathogens2020264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hotard AL, Lee S, Currier MG, Crowe JE Jr, Sakamoto K, Newcomb DC, Peebles RS Jr, Plemper RK, Moore ML. 2015. Identification of residues in the human respiratory syncytial virus fusion protein that modulate fusion activity and pathogenesis. J Virol 89:512–522. doi: 10.1128/JVI.02472-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mathieu C, Pohl C, Szecsi J, Trajkovic-Bodennec S, Devergnas S, Raoul H, Cosset FL, Gerlier D, Wild TF, Horvat B. 2011. Nipah virus uses leukocytes for efficient dissemination within a host. J Virol 85:7863–7871. doi: 10.1128/JVI.00549-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thakur N, Bailey D. Advances in diagnostics, vaccines and therapeutics for Nipah virus. Microbes Infect, in press. doi: 10.1016/j.micinf.2019.02.002. [DOI] [PubMed] [Google Scholar]