Abstract
Patient: Male, 43
Final Diagnosis: Boerhaave’s syndrome
Symptoms: Dyspnoea • epigastric pain • vomiting
Medication: —
Clinical Procedure: Over-the scope-clip and pleurodesis
Specialty: Gastroenterology and Hepatology
Objective:
Rare disease
Background:
The diagnosis of Boerhaave’s syndrome is often missed or delayed. This subsequently leads to a high mortality rate, which could be greatly reduced if treatment is instituted early, within 24 hours of perforation. Treatment ranges from conservative management to operative intervention depending on the time of presentation and the patient’s clinical condition. Endoscopic intervention in the form of over-the-scope clip (OTSC) application is gaining popularity with very promising results.
Case Report:
A 43-year-old male was diagnosed with Boerhaave’s syndrome and treated initially by insertion of bilateral chest drainage, intravenous broad-spectrum antibiotics, and total parenteral nutrition. He was transferred to our facility 9 days later. Upper gastrointestinal endoscopy revealed a 1.5 cm deep longitudinal ulcer involving the distal esophagus and extending to the Z-line. Due to the perforation site, a size 12 OTSC clip was used. Application of a second clip was needed to achieve complete closure of the perforation site. Contrast swallow was done 4 days later showed no leak. The patient was started on oral intake and was discharged home in good general condition after a hospital stay of 16 days.
Conclusions:
Delayed presentation of Boerhaave’s syndrome can be treated safely by an over-the-scope clip. This endoscopic method hastens recovery and shortens the hospital stay.
MeSH Keywords: Endoscopy, Gastrointestinal; Esophageal Diseases; Esophageal Perforation; Pleurodesis
Background
Boerhaave’s syndrome is spontaneous perforation of the esophagus; most commonly the distal part, as a result of forceful emesis. The classical triad of sub-xiphoid retrosternal pain, vomiting, and subcutaneous emphysema is present in a small number of patients, posing a formidable diagnostic challenge [1]. The management option depends on the time of perforation. Early presentation (within 24 hours) is commonly managed surgically, but delayed presentation is managed conservatively, especially if the perforation is confined and the clinical condition of the patient is stable. However, delayed presentation and treatment is associated with inferior outcome [1]. In recent years, endoscopic options are gaining popularity in the management of Boerhaave’s syndrome. Such options include endoscopic stenting and over-the-scope clipping (OTSC) of the perforation [2,3]. We report here a case of successful management by the OTSC system of a patient with Boerhaave’s syndrome who presented more than 9-days after the perforation.
Case Report
A 43-year-old male was admitted to a nearby secondary hospital after episodes of repeated forceful vomiting following alcohol ingestion. He complained of severe epigastric, sub-xiphoid pain, and shortness of breath. An initial chest x-ray followed by computerized tomography (CT) scan of the chest showed left-sided hydropneumothorax, pneumo-mediastinum, and para-aortic and para-esophageal air-fluid collections (Figure 1). The oral contrast at that time showed communication to both pleural cavities. The picture was diagnostic of esophageal perforation and hence the patient was initially managed by insertion of bilateral chest tubes which brought purulent drainage, intravenous broad-spectrum antibiotics, and total parenteral nutrition (TPN). The patient condition became stable and he was transferred to our facility for further management at 9 days after his initial presentation.
Figure 1.
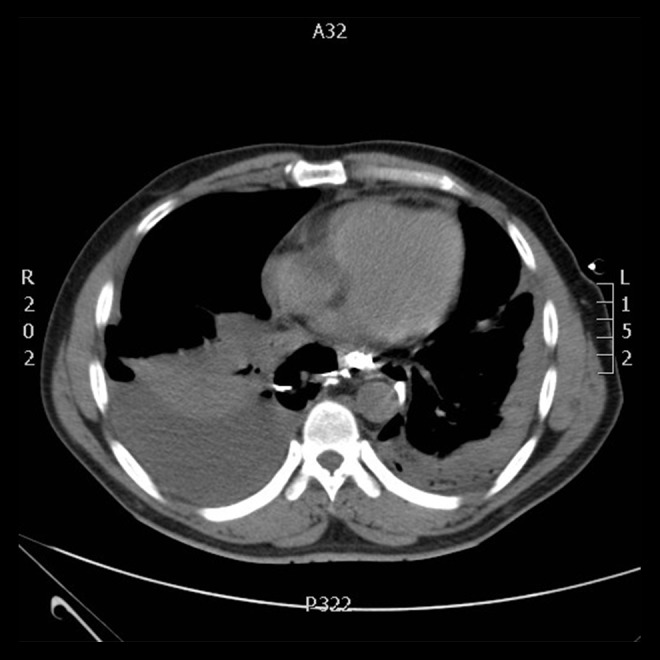
Chest computed tomography scan showing bilateral oral contrast extravasation from esophagus into the pleural cavity.
On arrival to our hospital, the patient looked reasonably well with no distress and his vital signs were normal (pulse 85 beats per minute, blood pressure 139/92 mmHg, and temperature 36.7°C). His O2 saturation was 94% on 2 L of oxygen via nasal cannula and he had bilateral chest tubes which were draining purulent discharge. The rest of the general examination was unremarkable except for decreased air entry and dullness in both lung fields. The initial blood tests showed hemoglobin 9.3 g/dL (normal range, 13–18 g/dL), white cell count 11.9×103/μL, platelets 581×103/μL, albumin 19 g/dL (normal range, 23–50 g/dL), and the liver and renal panels were normal.
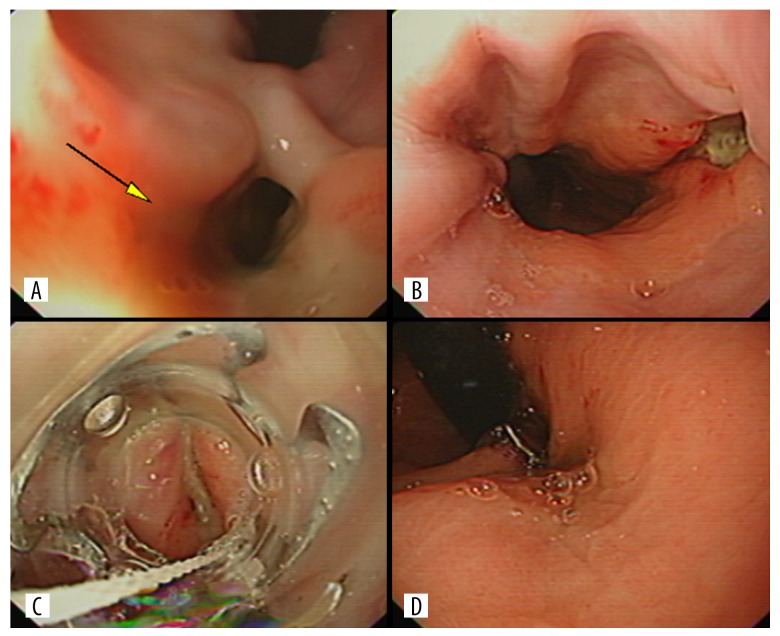
On the following day, he underwent an upper gastrointestinal endoscopy with fluoroscopic setup in place. This revealed a 1.5 cm deep longitudinal ulcer involving the lower esophagus and extending to the Z-line (Figure 2A). The ulcer had a necrotic base seen clearly at retroversion (Figure 2B). Due to the perforation site and delayed presentation, an over-the-scope clip (OTSC) system was preferred rather than endoscopic stenting.
Figure 2.
Endoscopic views of the esophago-gastroscopy. (A) Retroversion view looking at lower esophagus showing deep ulcer which was seen like a hole (yellow arrow). (B) Forward view showing deep ulcer with necrotic base at lower esophagus. (C) The ulcer being centered into the OTSC cylinder prior to clipping. (D) The ulcer after the application of the first OTSC clip. OTSC, over-the-scope clipping.
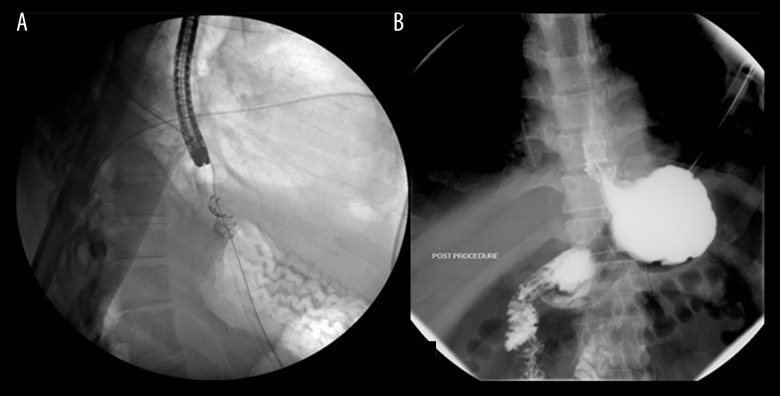
After the perforation site was assessed, a 12-mm OTS clip (OTSC; Ovesco Endoscopy, Tübingen, Germany) was preloaded over a transparent cap attached to the scope tip. The perforation was centralized, and the edges of the perforation were approximated by applying full suction through the cap to pull the tissue into the cap. A clip was then released by rotating the wheel attached to the shaft of the endoscope (Figure 2C). As only three-fourth of the perforation was closed by the first clip (Figure 2D), a second clip was applied to get a complete closure (Figure 3). Contrast x-rays that were done post-clipping revealed no leak (Figure 4A, 4B).
Figure 3.

Endoscopic views of the esophago-gastroscopy showing the 2 clips (OTSC) which were placed to close the site of the perforation. OTSC, over-the-scope clipping.
Figure 4.
Post-clipping contrast x-rays (A) lateral view, (B) supine position) showing no leak at the lower esophagus.
On the fourth day after clipping, a contrast swallow showed no leak and he was started on oral intake with gradual discontinuation of TPN. On the fifth day after clipping, a chest x-rays revealed presence of a fluid level in the left pleural cavity, so a CT scan was done showing features suggestive of empyema (Figure 5), which was managed non-operatively by interventional radiology using pig tail drains. The output, which was initially purulent, gradually became serous over the following 4 days. Bilateral chemical pleurodesis with bleomycin was later done and the chest tubes were removed.
Figure 5.
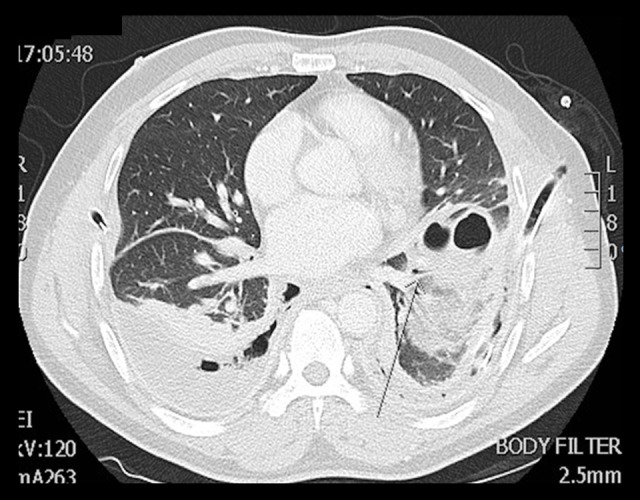
Computed tomography scan of the chest showing features of empyema.
Outcome and follow-up
The patient’s condition improved, and he was discharged home on day 16 after admission. The patient was seen in the out-patient clinic 14 days after discharge. He was well and tolerating full diet with no other complications. A chest x-ray was done at that time was normal (Figure 6). He remained well at 6-month follow-up.
Figure 6.
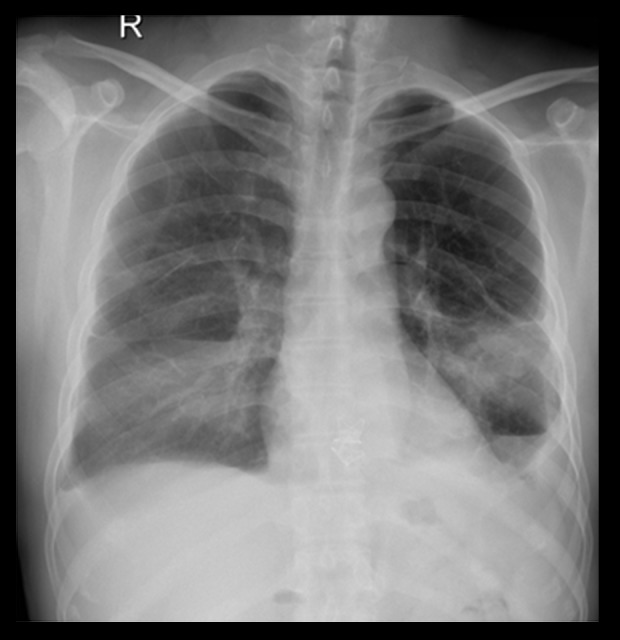
Posteroanterior chest x-ray at 2-week follow-up showing small air fluid level at left.
Discussion
Spontaneous esophageal rupture (Boerhaave’s syndrome) is rarely encountered and hence its diagnosis is either missed or delayed leading to a high mortality rate that approaches 60% if time to theatre is delayed beyond 48 hours. However, the overall mortality in cases managed early, within 24 hours of presentation, is much lower at 20% [4]. In addition to the delay in diagnosis and treatment, another major prognostic factor in determining mortality is the site of the injury.
It is recommended that all septic patients with esophageal perforation should be treated surgically, and conservative treatment is reserved for patients presenting early without sepsis. Conservative treatment is also advocated for those with delayed presentations but without sepsis. The recovery of such patients can be hastened by minimally invasive endoscopic means [2].
The hospital stay of our patient was 16 days; this was much shorter than that reported by others for delayed Boerhaave’s syndrome treated by OTSC [5]. There is no doubt that the combined non-operative interventional radiology drainage of septic collection and the minimally invasive OTSC greatly contributed to the rapid recovery and short hospital stay. This combined management strategy emphasizes the importance of a multi-disciplinary team approach for the management of this condition to minimize morbidity and mortality, and to achieve good outcomes.
In recent years, an increasing number of patients with esophageal perforations are being managed by non-operative endoscopic measures such as placement of covered self-expanding stents, over-the-scope clipping, or both a clip and a stent [6]. A covered self-expanding stent can achieve sealing of a leak in up to 50% of cases, and placement of a second stent in failed cases is not usually successful in sealing the leak [1]. The OTSC system is a clipping method for mechanical compression of tissues in the gastrointestinal tract. It was first designed for the management of bleeding, perforation, and fistula [7], and hence, OTSC can be appropriately employed in the treatment of esophageal perforation [3,5,8]. It has been demonstrated that standard clips might not be as effective as OTSC as a primary therapy in sealing gastrointestinal bleeding [9]. In comparison to the conventional clips, OTSC has a greater compressive force and is more effective in achieving superior grip of fibrotic tissue, as in this case of delayed perforation. Moreover, OTSC offers easy application and maneuvering in tight anatomical positions. However, there is no clinical study to date that compares OTSC versus conventional clips, except one prospective randomized study that confirmed superiority of OTSC over standard methods used to control recurrent ulcer bleeding (not perforation) in term of technical and clinical success [10].
Our case presented late (9 days after perforation) to our facility and the size of the perforation was 1.5 cm. Due to the site of the perforation, OTSC rather than stenting was applied with success. However, the closure could not be achieved by one clip and therefore, a second clip was applied. The residual thoracic sepsis was treated by tube drainage and later by pleurodesis after clearance of sepsis. A review of the literature for cases of delayed Boerhaave’s syndrome treated by OTSC revealed 3 similar cases. The first successful endoscopic use of the OTSC in a delayed presentation (7 days after admission) of Boerhaave’s syndrome with mediastinitis was reported in 2013 by Ramhamadany et al. in a case of a 69-year-old patient. During endoscopy, the defect was visualized and successfully closed using OTSC, which resulted in a favorable outcome [3]. Bona et al. reported a case of a 36-year-old male patient referred with a delayed diagnosis of Boerhaave’s syndrome (12 days), which was successfully treated by OTSC application followed by lung decortication [5]. Kircheva and Vigneswaran reported a case of a 53-year-old male patient who had failed OTSC followed by endoscopic stenting after failure of OTSC to seal the leak. Despite stenting, the leak persisted necessitating a primary surgical repair 14 days after perforation [11]. This case confirms that combining OTSC and stenting does not guarantee success and does not avert the need for surgery in some cases. It also indicates that successful primary repair can be done in delayed perforations (as late as 2 weeks after the diagnosis) and after failure of the endoscopic management [11].
Endoscopic stenting alone is another viable option even in delayed cases [12]. Aloreidi et al. reported effective endoscopic stent treatment in 6 patients (4 males and 2 females) with Boerhaave’s syndrome. They attributed satisfactory results in patients presenting with sepsis to urgent interventional radiology-guided fluid drainage [12]. This again highlights the importance of a multidisciplinary team approach in the management of this condition to secure good and favorable outcomes. Other minimally invasive mean of treating delayed esophageal rupture is by T-tube drainage using video-assisted thoracoscopic surgery (stay 46 days) [13].
Conclusions
OTSC of esophageal perforation in Boerhaave’s syndrome presenting late is safe and effective. Moreover, OTSC hastens recovery and shortens the hospital stay in cases suitable for conservative treatment.
References:
- 1.Glatz T, Marjanovic G, Kulemann B, et al. Management and outcome of esophageal stenting for spontaneous esophageal perforations. Dis Esophagus. 2017;30(3):1–6. doi: 10.1111/dote.12461. [DOI] [PubMed] [Google Scholar]
- 2.Darrien JH, Kasem H. Minimally invasive endoscopic therapy for the management of Boerhaave’s syndrome. Ann R Coll Surg Engl. 2013;95(8):552–56. doi: 10.1308/003588413X13629960049315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramhamadany E, Mohamed S, Jaunoo S, et al. A delayed presentation of Boerhaave’s syndrome with mediastinitis managed using the over-the-scope clip. J Surg Case Rep. 2013;(5) doi: 10.1093/jscr/rjt020. pii: rjt020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connelly CL, Lamb PJ, Paterson-Brown S. Outcomes following Boerhaave’s syndrome. Ann R Coll Surg Engl. 2013;95(8):557–60. doi: 10.1308/003588413X13629960049199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bona D, Aiolfi A, Rausa E, Bonavina L. Management of Boerhaave’s syndrome with an over-the-scope clip. Eur J Cardiothorac Surg. 2014;45(4):752–54. doi: 10.1093/ejcts/ezt363. [DOI] [PubMed] [Google Scholar]
- 6.González-Haba M, Ferguson MK, Gelrud A. Spontaneous esophageal perforation (Boerhaave syndrome) successfully treated with an over-the- scope clip and fully covered metal stent. Gastrointest Endosc. 2016;83:650. doi: 10.1016/j.gie.2015.09.032. [DOI] [PubMed] [Google Scholar]
- 7.Nasa M, Sharma ZD, Choudhary NS, et al. Over-the-scope clip placement for closure of gastrointestinal fistula, postoperative leaks and refractory gastrointestinal bleed. Indian J Gastroenterol. 2016;35(5):361–65. doi: 10.1007/s12664-016-0690-8. [DOI] [PubMed] [Google Scholar]
- 8.Musala C, Eisendrath P, Brasseur A, et al. Successful treatment of Boerhaave syndrome with an over-the-scope clip. Endoscopy. 2015;47(Suppl. 1) doi: 10.1055/s-0034-1390718. UCTN: E24–25. [DOI] [PubMed] [Google Scholar]
- 9.Brandler J, Baruah A, Zeb M, et al. Efficacy of over-the-scope clips in management of high-risk gastrointestinal bleeding. Clin Gastroenterol Hepatol. 2018;16(5):690–96. doi: 10.1016/j.cgh.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt A, Gölder S, Goetz M, et al. Over-the-scope clips are more effective than standard endoscopic therapy for patients with recurrent bleeding of peptic ulcers. Gastroenterology. 2018;155(3):674–86. doi: 10.1053/j.gastro.2018.05.037. [DOI] [PubMed] [Google Scholar]
- 11.Kircheva DY, Vigneswaran WT. Successful primary repair of late diagnosed spontaneous esophageal rupture: A case report. Int J Surg Case Rep. 2017;35:49–52. doi: 10.1016/j.ijscr.2017.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aloreidi K, Patel B, Ridgway T, et al. Non-surgical management of Boerhaave’s syndrome: A case series study and review of the literature. Endosc Int Open. 2018;6(1):E92–97. doi: 10.1055/s-0043-124075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Do YW, Lee CY, Lee S, et al. Successful management of delayed esophageal rupture with T-Tube drainage using video-assisted thoracoscopic surgery. Korean J Thorac Cardiovasc Surg. 2016;49(6):478–80. doi: 10.5090/kjtcs.2016.49.6.478. [DOI] [PMC free article] [PubMed] [Google Scholar]