Abstract
Objective:
To characterize and compare ambulatory antibiotic prescribing for children in U.S. pediatric and non-pediatric Emergency Departments (EDs).
Methods:
A cross-sectional retrospective study of patients aged 0–17 years discharged from U.S. EDs was conducted using the 2009–2014 National Hospital Ambulatory Medical Care Survey ED data. We estimated the proportion of ED visits resulting in antibiotic prescriptions, stratified by antibiotic spectrum, class, diagnosis, and ED type (pediatric defined as >75% of visits by patients aged 0–17 years, versus non-pediatric). Multivariable logistic regression was used to determine factors independently associated with first-line, guideline-concordant prescribing for acute otitis media, pharyngitis, and sinusitis.
Results:
In 2009–2014, of the 29 million mean annual ED visits by children, 14% (95% CI: 10–20%) occurred at pediatric EDs. Antibiotics overall were prescribed more frequently in non-pediatric than pediatric ED visits (24% versus 20%, p<0.01). Antibiotic prescribing frequencies were stable over time. Of all antibiotics prescribed, 44% (95% CI: 42–45%) were broad-spectrum, and 32% (95% CI: 30–34%, 2.1 million per year) were generally not indicated. Compared to pediatric EDs, non-pediatric EDs had a higher frequency of prescribing of macrolides (18% versus 8%, p<0.0001) and lower frequency of first-line, guideline-concordant prescribing for the respiratory conditions studied (77% versus 87%, p<0.001).
Conclusions:
Children are prescribed almost 7 million antibiotic prescriptions in EDs annually, primarily in non-pediatric EDs. Pediatric antibiotic stewardship efforts should expand to non-pediatric EDs nationwide, particularly regarding avoidance of antibiotic prescribing for conditions for which antibiotics are not indicated, reducing macrolide prescriptions, and increasing first-line, guideline-concordant prescribing.
Introduction
Approximately 18% of U.S. children visited an Emergency Department (ED) in 2012.1 Children in EDs often receive antibiotics, which are estimated to be prescribed in 15–20% of the >26 million annual pediatric visits to U.S. EDs.2–5 Respiratory conditions account for >70% of antibiotic prescriptions for children in the ambulatory setting.4 Previous work shows that the majority of antibiotics prescribed to children in ambulatory settings are broad-spectrum and approximately 30% are not in accordance with national guidelines.6–9
The National Action Plan for Combating Antibiotic-Resistant Bacteria aims to reduce inappropriate antibiotic use by 50% in ambulatory settings, including EDs, by 2020.10,11 However, formal antibiotic stewardship efforts specific to ambulatory and ED settings are lacking nationally.12,13
Over 80% of pediatric visits to an ED occur in non-academic EDs or general (i.e., non-pediatric) EDs.2,14,15 Children with asthma, bronchitis, and croup receive higher quality of care and fewer unnecessary chest x-rays when treated at a pediatric ED compared to a non-pediatric ED.16 Previous work has demonstrated lower frequency of antibiotic prescribing for children with febrile respiratory illness visits in pediatric EDs compared to non-pediatric EDs.17 However, an understanding of the overall landscape of antibiotic prescribing for children presenting to pediatric and non-pediatric EDs nationally is both lacking and necessary to guide efforts to improve antibiotic prescribing for children in EDs.
We aimed to provide a comprehensive characterization of antibiotic use for children in pediatric and non-pediatric EDs nationally by the type of agent prescribed, the diagnoses associated with antibiotic visits, and concordance with national guideline recommendations for first-line treatment of common respiratory infections.
Methods
Study Design and Data Source
We performed a cross-sectional retrospective study using the National Hospital Ambulatory Medical Care Survey (NHAMCS) ED public-use data files from 2009–2014 (the most recent available data at study onset).18 NHAMCS is conducted annually by the National Center for Health Statistics from a sample of non-federal hospital-based EDs, including representation from freestanding pediatric facilities.19 The survey uses a multistage probability sampling design in selecting participating hospitals and patient visits across the U.S. Data for sampled visits are collected during a 4-week reporting period, weighted to produce national estimates, and classified by U.S. Census Region.20 Participating centers had an unweighted ED survey response rate of 75.5–92.0% over the study period.
Survey variables used included demographics (age, gender, and race), insurance status (private versus non-private), provider type (physician versus advanced practice provider), U.S. Census Region, ED metropolitan statistical area (MSA) status, discharge diagnosis, and medications administered, prescribed or continued at ED visits. MSA is defined by the Office of Management and Budget as geographical regions with high population densities. Diagnoses were determined by International Classification of Diseases, 9th revision (ICD-9) codes. Duration of therapy and route of medication administration were unavailable; medications available only in topical formulations were omitted. For consistency across all included survey years, the first 3 diagnosis fields and 8 medications were considered.
Study Participants and Setting
Visits for all patients aged 0–17 years discharged from the ED were included. Antibiotic visits were defined as ED visits in which systemic (oral or parenteral) antibiotics were mentioned as continued, administered, or prescribed. Civilian non-institutionalized population data from the U.S. Census Bureau21 were used to determine antibiotic visits per 1000 U.S. population. We estimated each ED’s proportion of pediatric visits by calculating the weighted proportion of visits by children out of total ED visits. The ED type was then defined as pediatric if >75% of all visits to that ED were by patients aged 0–17 years, or non-pediatric otherwise, a definition used for classifying pediatric EDs previously.2,22,23 A histogram of the proportion of weighted pediatric visits by ED (Supplemental Figure 1) indicates most EDs defined as pediatric had >90% of visits by children; thus our definition appears to accurately differentiate pediatric EDs from others.
Diagnoses for Antibiotic Visits
The NHAMCS dataset does not link medications with diagnoses. Based on a previously published classification system informed by national guideline recommendations, we assigned the top 3 listed diagnoses to one of three tiers: diagnoses for which antibiotics were (1) almost always indicated (e.g., bacterial pneumonia), (2) may be indicated (e.g., pharyngitis), or (3) generally not indicated (e.g., bronchiolitis/bronchitis).5 Each visit was assigned a single diagnosis, with priority given hierarchically to tier 1 diagnoses, then tier 2 diagnoses, then tier 3 diagnoses. If a visit had multiple diagnoses from a single tier, the first-listed diagnosis was assigned.
Because >70% of ambulatory pediatric antibiotic prescribing is for acute respiratory tract infection (ARTI), we evaluated prescribing for ARTIs.4 We defined ARTI to include pneumonia, acute otitis media (AOM), non-suppurative otitis media, sinusitis, pharyngitis (including viral and streptococcal), non-specific upper respiratory tract infection, bronchitis/bronchiolitis, and influenza.5
Classification of Antibiotic Spectrum and First-Line, Guideline-Concordant Prescribing
Antibiotic types were classified by their generic components and therapeutic classes using Multum Lexicon® Drug Database. Antibiotics included: penicillins, cephalosporins, macrolides, quinolones, lincomycin derivatives, tetracyclines, sulfonamides, urinary anti-infectives (e.g., nitrofurantoin), aminoglycosides, carbapenems, linezolid, and vancomycin. The general class of antibiotics (e.g. penicillins) and sub-classes (e.g. 1st generation cephalosporins) were determined using Multum Level 2 and Level 3 categories, respectively. The following antibiotics and antibiotic classes were considered narrow-spectrum: penicillin, amoxicillin, 1st generation cephalosporins, sulfonamides, and nitrofurantoin. All other antibiotics, including macrolides and combination beta-lactam/beta-lactamase inhibitors such as amoxicillin-clavulanate, were considered broad-spectrum.
The diagnoses of AOM, pharyngitis, and sinusitis are common respiratory illnesses, and have evidence-based clinical practice guidelines that recommend specific and primarily narrow-spectrum antibiotic options as first-line therapy.24–26 Based on national guidelines, we defined first-line, guideline-concordant antibiotic use as amoxicillin or amoxicillin-clavulanate for AOM and sinusitis, and penicillin or amoxicillin for pharyngitis. Amoxicillin-clavulanate was included as first-line for AOM due to recommendations to use it first-line for selected patients, e.g., for children with concurrent conjunctivitis.
Analysis
We studied three main outcomes. First, using NHAMCS-provided patient visit weights, we estimated the proportion and mean annual number of ED visits resulting in an antibiotic prescription, called antibiotic visits. We stratified antibiotic visits by patient demographic characteristics, patient insurance type, provider type, U.S. Census Region, ED MSA status, and ED type. Six years of survey data were combined to increase sample size for analyses stratified by age. Second, we compared the proportion of antibiotic visits and antibiotic classes for ARTI, urinary tract infection (UTI), skin and soft tissue infection (SSTI) and diagnostic tier by pediatric and non-pediatric EDs. All pediatric age groups were combined for the analysis of antibiotic use by diagnosis to increase the sample size and produce reliable estimates as suggested in the NHAMCS use files.27 We assessed trends in proportion of antibiotic classes over time using logistic regression in 2-year increments (2009–10, 2011–12, and 2013–14) as the predictor variable and percent of antibiotics by class as the outcome. Finally, based on previous work in ambulatory settings demonstrating factors associated with antibiotic prescribing,4,28–30 we used multivariable logistic regression, adjusting for patient demographic characteristics, patient insurance type, provider type, U.S. Census Region, ED type, and diagnoses, to determine factors independently associated with the outcome of first-line, guideline-concordant prescribing for AOM, pharyngitis, and sinusitis. Odds ratio estimates for first-line guideline-concordant prescribing by MSA were also determined. Data on MSA were not publicly available in 2012; therefore, odds ratio estimates for MSA were determined using a separate model that adjusted for all other variables, but excluded observations from 2012.
We performed statistical analyses using STATA 14® (STATA Corp, College Station, TX) accounting for the complex survey design, including patient visit weights, strata, and primary sampling unit design variables. Estimates were not calculated if based on <30 visits or if the relative standard error was <0.3, as recommended by NHAMCS standards for reliability and precision.27 Antibiotic prescribing proportions were compared using chi-square tests for heterogeneity. Ninety-five percent confidence intervals (CI) were calculated for all estimates. Significance was considered at 2-sided P value ≤0.05. NHAMCS data sets used in this analysis are de-identified and publically available and thus were determined non-human subjects by the Human Subjects Advisor at the National Center for Emerging and Zoonotic Infectious Diseases.
Results:
Characteristics of Pediatric Visits to EDs
In 2009–2014, an average 29 million (95% CI: 27–32 million) ED visits by children occurred annually, of which 23% (95% CI: 22–24%) were antibiotic visits, accounting for an estimated 6.7 million (95% CI: 6.1–7.5 million) antibiotic visits annually (Table 1). Fourteen percent (95% CI: 10–20%) of ED visits occurred in pediatric EDs. The percentage of ED visits resulting in an antibiotic prescription was significantly higher in non-pediatric EDs (24%, 95% CI: 23–25%) compared to pediatric EDs (20%, 95% CI: 17–22%, p<0.01).
Table 1:
Characteristics of visits to EDs by children 0–17 years of age, United States, 2009–2014.
| Characteristic | Average annual number of visits by children, in millions (95% CI) | Percentage of visits by children that resulted in an antibiotic prescription (95% CI) |
|---|---|---|
| Total | 29 (27–32) | 23% (22–24%) |
| Age (years) | ||
| <1 | 3.6 (3.2–4.0) | 22% (20–24%) |
| 1–4 | 9.6 (8.6–10.5) | 29% (27–30%) |
| 5–12 | 9.4 (8.5–10.3) | 23% (22–24%) |
| 13–17 | 6.7 (6.0–7.3) | 17% (16–19%) |
| Gender | ||
| Male | 15.3 (13.9–16.7) | 22% (22–23%) |
| Female | 13.9 (12.6–15.2) | 24% (23–25%) |
| Race | ||
| White | 20.2 (18.2–22.1) | 23% (22–24%) |
| Black | 7.7 (6.6–8.8) | 24% (23–26%) |
| Other | 1.4 (1.1–1.6) | 20% (17–23%) |
| Insurance Status | ||
| Private | 8.7 (7.8–9.6) | 20% (19–21%) |
| Non-private | 18.8 (16.9–20.7) | 25% (24–26%) |
| US Census Region+ | ||
| Northeast | 4.6 (3.9–5.3) | 19% (17–20%) |
| Midwest | 6.5 (5.3–7.6) | 24% (22–25%) |
| South | 12.0 (10.0–14.0) | 25% (24–27%) |
| West | 6.1 (5.0–7.2) | 22% (20–24%) |
| Metropolitan Statistical Area (MSA)* | ||
| Non-MSA | 5.0 (3.2–6.9) | 27% (25–29%) |
| MSA | 24.7 (21.5–27.8) | 23% (22–24%) |
| Type of ED | ||
| Non-Pediatric | 25.1 (22.8–27.3) | 24% (23–25%) |
| Pediatric | 4.1 (2.6–5.7) | 20% (17–22%) |
| Advanced Practice Practitioner Present at ED Visit | ||
| No | 23.7 (21.4–26.0) | 23% (22–24%) |
| Yes | 5.3 (4.6–6.0) | 26% (24–28%) |
U.S. Census Regions defined by the U.S. Census Bureau20
Data on MSA were not publicly available in 2012; therefore, estimates exclude observations from 2012.
Diagnoses Associated with Antibiotic Visits
ARTIs accounted for the majority of diagnoses among antibiotic visits (55%, 95% CI: 54–57%), followed by SSTI (9%, 95% CI: 8–10%) and UTI (7%, 95% CI: 6–8%). AOM and pharyngitis accounted for 45% (95% CI: 42–47%) and 25% (95% CI: 23–27%) of all ARTI antibiotic visits, respectively. Pediatric and non-pediatric EDs had similar proportion of antibiotic visits for ARTI, SSTI, and UTI (Table 2).
Table 2:
Percent of ED visits and antibiotic visits by diagnosis category and tier*, stratified by ED type, United States, 2009–2014.
| Percent of visits in which the diagnosis category or tier was used, among all visits involving children | Percent of antibiotic visits in which the diagnosis category or tier was used, among all antibiotic visits | |||||
|---|---|---|---|---|---|---|
| Diagnosis Category | Non-pediatric ED (95% CI) | Pediatric ED (95% CI) | p (χ2) | Non-pediatric ED (95% CI) | Pediatric ED (95% CI) | p (χ2) |
| ARTI | 26% (25–27%) | 28% (26–31%) | 0.16 | 55% (53–57%) | 57% (51–62%) | 0.55 |
| SSTI | 2% (2–2%) | 2% (1–2%) | 0.38 | 9% (8–10%) | 9% (6–12%) | 0.39 |
| UTI | 3% (3–3%) | 3% (2–4%) | 0.43 | 7% (6–8%) | 8% (6–10%) | 0.99 |
| Other Conditions | 69% (68–70%) | 67% (64–70%) | 0.31 | 29% (28–31%) | 27% (22–32%) | 0.34 |
| Diagnosis Tier* | Non-pediatric ED (95% CI) | Pediatric ED(95% CI) | p (χ2) | Non-pediatric ED (95% CI) | Pediatric ED (95% CI) | p (χ2) |
| Antibiotics always indicated | 10% (9–10%) | 11% (9–12%) | 0.28 | 16% (15–18%) | 17% (14–20%) | 0.02 |
| Antibiotics may be indicated | 23% (22–24%) | 24% (22–27%) | 51% (49–53%) | 57% (52–62%) | ||
| Antibiotics generally not indicated | 67% (66–68%) | 65% (62–68%) | 33% (31–34%) | 26% (21–31%) | ||
ARTI: acute respiratory tract infection;
SSTI: skin and soft tissue infection;
UTI: urinary tract infection
Classification of diagnosis tier is based on a previously published hierarchical system informed by national guideline recommendations (Fleming-Dutra 2016).
Of antibiotic visits for children in EDs nationally, 32% (95% CI: 30–34%; 2.1 million/year) were for conditions for which antibiotics are generally not indicated. There were no significant differences in the proportion of visits in each diagnostic tier (antibiotics almost always, may be, or generally not indicated) for children in pediatric versus non-pediatric EDs (Table 2). However, non-pediatric EDs had significantly more antibiotic visits for diagnoses for which antibiotics are generally not indicated (33%, 95% CI: 31–34%) compared to pediatric EDs (26%, 95% CI: 21–31%, p=0.02).
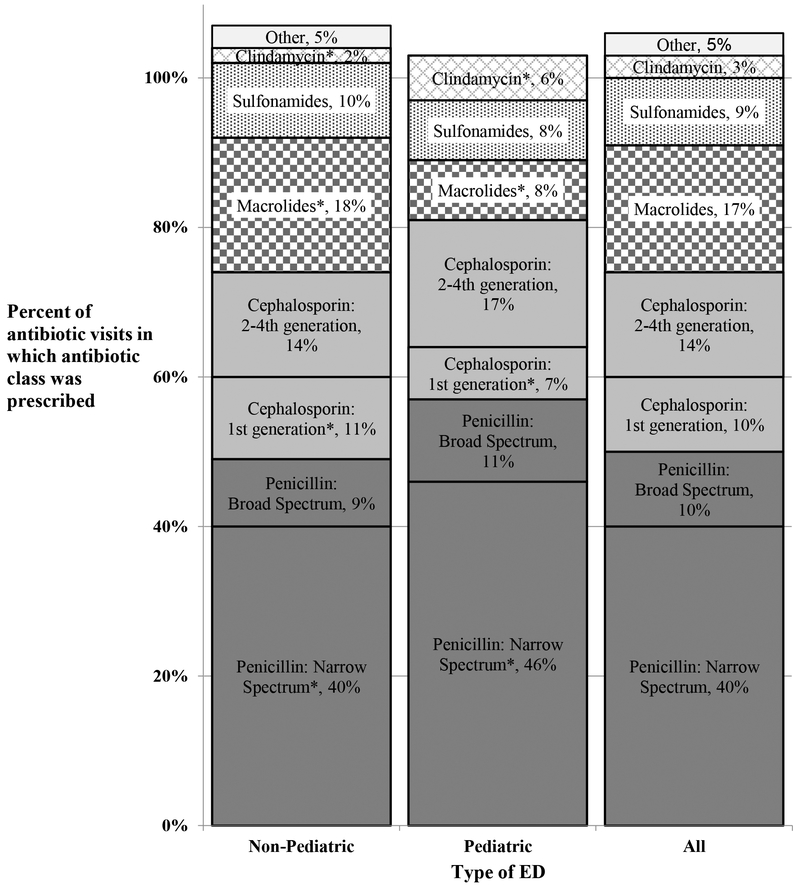
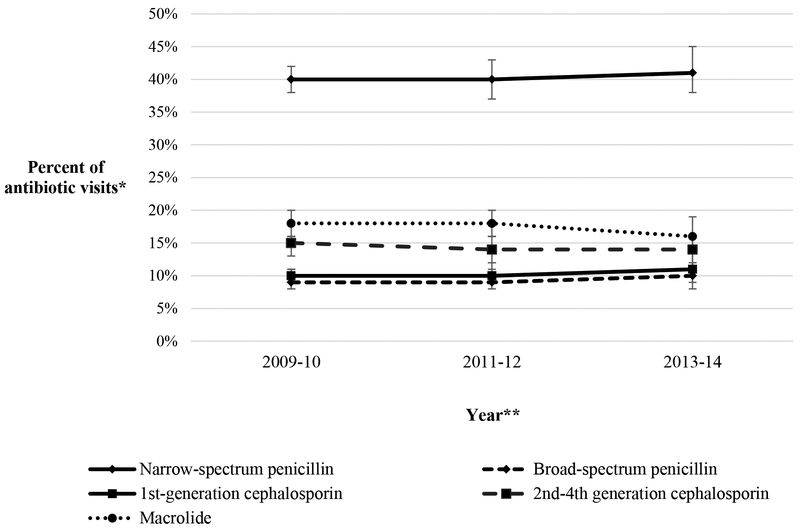
Antibiotic Classes Prescribed at ED Visits
Narrow-spectrum penicillins were the most commonly prescribed antibiotic class in visits to both pediatric and non-pediatric EDs, followed by cephalosporins, macrolides, sulfonamides, and lincomycin derivatives (clindamycin) (Figure 1). Fluoroquinolones comprised 2% (95% CI: 2–3%) and tetracyclines, urinary anti-infectives, and aminoglycosides together comprised 3% (95% CI: 3–3%) of antibiotic prescriptions in all EDs; prescribing estimates for these agents in pediatric EDs did not meet NHAMCS standards for reliability or precision due to sample size. There was no significant change over time in the percent of any one antibiotic class of all antibiotics prescribed (Figure 2).
Figure 1: Percent of antibiotic visits by antibiotic class for ED visits by children, by ED type, United States, 2009–2014.
Shading represents antibiotic class: dark grey are penicillins, light grey are cephalosporins, grey/white checkered are macrolides, black/white dotted are sulfonamides, white/grey diamonds are clindamycin (lincomycin derivative), and lightest grey are all other antibiotics. *P≤0.05 in comparison of non-pediatric versus pediatric ED. **Percentages sum to >100% because of co-prescribing at some visits.
Figure 2: Percent of antibiotic visits by antibiotic class for ED visits by children over time, United States, 2009–2014.
*Antibiotic visits were defined as visits in which antibiotics were mentioned as continued, administered, or prescribed. **2-year increments used to assess change in antibiotic prescriptions over time. No significant change in percentages over the study period.
Macrolides were prescribed in 17% (95% CI: 16–19%; 1.1 million) of all visits to EDs in which antibiotics were prescribed. Among antibiotic visits, the diagnoses most frequently associated with macrolides included AOM (17%, 95% CI: 14–20%), non-viral pneumonia (14%, 95% CI: 12–17%), pharyngitis/tonsillitis (12%, 95% CI: 10–14%), bronchitis/bronchiolitis (11%, 95% CI: 9–13%), and upper respiratory tract infection (10%, 95% CI: 8–13%). Of all ED macrolide prescribing to children, 44% (95% CI: 41–47%; 500,000 annually) were for diagnoses for which antibiotics are generally not indicated. Macrolides were prescribed at a significantly higher frequency in non-pediatric EDs (18%, 95% CI: 17–20%) compared to pediatric EDs (8%, 95% CI: 6–10%, p<0.0001, Figure 1).
Broad-spectrum antibiotics were prescribed in 44% (95% CI: 42–45%) of antibiotic visits by children in EDs nationally, with no difference between non-pediatric (44%, 95% CI: 42–45%) versus pediatric (44%, 95% CI: 40–48%, p=0.91) EDs.
Characteristics of First-Line, Guideline-Concordant Therapy
Among children with AOM, sinusitis, or pharyngitis, the proportion of antibiotic visits during which patients received first-line, guideline-concordant therapy was 78% (95% CI: 76–80%) and was higher in pediatric EDs (87%, 95% CI: 82–90%) than non-pediatric EDs (77%, 95% CI: 75–79%, p<0.001, Table 3). This difference persisted in the multivariable model for the percent of AOM, pharyngitis, or sinusitis visits prescribed first-line, guideline-concordant therapy with an adjusted odds ratio (aOR) of 2.01 (95% CI: 1.38–2.92) for pediatric EDs compared to non-pediatric EDs. First-line, guideline-concordant antibiotic prescribing was also significantly more likely in visits by black children (aOR 1.56, 95% CI: 1.15–2.11) compared to visits by white children. First-line, guideline-concordant antibiotic prescribing was significantly lower in the Midwest (aOR 0.51, 95% CI: 0.34–0.77), South (aOR 0.46, 95% CI: 0.32–0.67) and West (aOR 0.55, 95% CI: 0.35–0.87) when compared to the Northeast region (Table 3). Patients with sinusitis and pharyngitis had lower adjusted odds of receiving first-line antibiotic treatment (aOR 0.51, 95% CI: 0.32–0.82 and aOR 0.72, 95% CI: 0.53–0.96, respectively) compared to patients with AOM. The percent of AOM, sinusitis, and pharyngitis visits with first-line, guideline-concordant prescribing did not change over the study period (Supplemental Figure 2a).
Table 3:
Factors associated with first-line, guideline-concordant antibiotic prescribing for acute otitis media, sinusitis, and pharyngitis in ED visits by children, United States, 2009–2014.
| Characteristic* | Percentage of visits in which first-line, guideline-concordant antibiotics were prescribed, among all visits in which antibiotics were prescribed (95% CI) | p(χ2) | Adjusted Odds Ratio (95% CI) for first-line, guideline-concordant prescribing |
|---|---|---|---|
| Age (years) | 0.12 | ||
| <1 | 80% (74–85%) | 1.00 | |
| 1–4 | 80% (76–83%) | 1.07 (0.68–1.70) | |
| 5–12 | 78% (74–81%) | 1.11 (0.68–1.82) | |
| 13–17 | 72% (66–77%) | 0.92 (0.49–1.72) | |
| Sex | 0.89 | ||
| Male | 78% (75–81%) | 1.00 | |
| Female | 78% (75–81%) | 1.01 (0.78–1.30) | |
| Race | <0.01 | ||
| White | 76% (73–79%) | 1.00 | |
| Black | 81% (75–85%) | 1.56 (1.15–2.11) | |
| Insurance status | 0.08 | ||
| Private | 75% (70–79%) | 1.00 | |
| Non-private | 79% (76–82%) | 1.32 (0.99–1.76) | |
| US Census Region+ | 0.04 | ||
| Northeast | 86% (83–89%) | 1.00 | |
| Midwest | 78% (74–83%) | 0.51 (0.34–0.77) | |
| South | 76% (72–80%) | 0.46 (0.32–0.67) | |
| West | 77% (72–82%) | 0.55 (0.35–0.87) | |
| Advanced Practice Practitioner present at ED Visit | 0.58 | ||
| No | 78% (75–80%) | 1.00 | |
| Yes | 79% (75–83%) | 1.08 (0.84–1.39) | |
| Type of ED | <0.001 | ||
| Non-Pediatric | 77% (75–79%) | 1.00 | |
| Pediatric | 87% (82–90%) | 2.01 (1.38–2.92) | |
| Diagnosis | <0.01 | ||
| Acute Otitis Media | 81% (78–84%) | 1.00 | |
| Sinusitis | 70% (60–78%) | 0.51 (0.32–0.82) | |
| Pharyngitis | 74% (71–78%) | 0.72 (0.53–0.96) | |
| Modeled using 2009–11 and 2013–14 | |||
| Metropolitan Statistical Area (MSA) | <0.001 | ||
| Non-MSA | 71% (68–75%) | 1.00 | |
| MSA | 79% (75–80%) | 1.26 (0.99–1.60) | |
Data on MSA were not publicly available in 2012. The main model to determine the odds ratio estimates for each variable included all listed variables other than MSA. Odds ratio estimates for MSA are from a separate model that adjusted for all other variables, but excluded observations from 2012.
U.S. Census Regions defined by the U.S. Census Bureau20
Discussion:
This study provides a comprehensive overview of antibiotic use among visits involving children in U.S. EDs. Non-pediatric EDs care for >85% of pediatric ED patients (over 25 million visits annually), and consequently prescribe antibiotics in >6 million annual pediatric visits — nearly 10% of all pediatric outpatient antibiotic prescriptions.9 Compared to visits in pediatric EDs, clinicians in non-pediatric EDs prescribe antibiotics more frequently for conditions for which antibiotics are likely unnecessary, are more likely to select macrolides, and are less likely to select first-line, guideline-recommended antibiotics for children with common respiratory illnesses.
While the proportion of children with viral infections receiving unnecessary antibiotics has been as low as 2.5% in selected, large, academic pediatric EDs,31 we evaluated all ED visits nationally, and found 26% of antibiotic visits at pediatric EDs were for conditions for which antibiotics were generally not indicated. Our finding mirrors previous work on antibiotic prescribing for children with ARTI in the ambulatory and ED setting.4,32 In comparison, we found that 33% of antibiotic visits at non-pediatric EDs were for conditions for which antibiotics were generally not indicated, accounting for an estimated 2 million unnecessary pediatric antibiotic prescriptions annually. Antibiotic prescribing for these conditions provides no benefit to patients, puts them at unnecessary risk for adverse events, and should be a target for quality improvement in EDs nationally, particularly in non-pediatric EDs.
More frequent unnecessary and guideline-discordant antibiotic prescribing by clinicians in non-pediatric EDs may reflect differences in clinical experiences during training. The American Academy of Pediatrics has published multiple evidence-based clinical practice guidelines for common pediatric conditions, created with multidisciplinary expert consensus, including representation from pediatric emergency medicine. ARTIs constitute the majority of antibiotic visits for children in EDs nationally, as is the case among outpatients seen by pediatric clinicians.4,33 Pediatric-trained clinicians are more likely to work in pediatric EDs compared to non-pediatric EDs,34,35 and might thereby have increased familiarity and compliance with pediatric-specific guidelines, which could contribute to differences in quality of antibiotic prescribing between pediatric and non-pediatric EDs. Previous work shows children are more likely to receive unnecessary antibiotics for upper respiratory tract infections in EDs or family practitioner offices compared to pediatrician offices.36 Increased exposure of emergency medicine clinicians to pediatric-focused guidelines and antibiotic stewardship initiatives is an important strategy to improve antibiotic prescribing quality in non-pediatric EDs.
We found that broad-spectrum antibiotics constitute almost half (47%) of all antibiotics prescribed to children in the ED. Previous work has shown similar rates of broad-spectrum antibiotic prescribing for children in other ambulatory settings and in the ED with respiratory tract infections specifically.4,32 In our study, macrolides accounted for 17% of all antibiotics prescribed to children in EDs, and non-pediatric EDs prescribed macrolides significantly more often than pediatric EDs (18% vs. 8%, respectively). Our work adds to a growing body of literature demonstrating that non-pediatric healthcare centers and clinicians prescribe macrolides more frequently than pediatric healthcare centers and clinicians.37–40 In our study, macrolides were most commonly prescribed for AOM; however, macrolides are not recommended for AOM treatment.24 Streptococcus pneumoniae is the most common cause of AOM and sinusitis, yet41 approximately 30% of U.S. invasive S. pneumoniae isolates are resistant to macrolides,42 so macrolides represent a suboptimal treatment choice for these conditions. Bronchitis/bronchiolitis and upper respiratory tract infections, diagnoses for which antibiotics are not recommended,43–46 constituted 21% of all macrolide use in our study. Inappropriate macrolide use should be a target for improvement in antibiotic prescribing for children in EDs, and non-pediatric EDs in particular.
The Centers for Disease Control and Prevention’s Core Elements of Outpatient Antibiotic Stewardship47 offers a framework for implementing antibiotic stewardship in outpatient settings, including EDs. Additionally, EDs can improve their antibiotic prescribing through standardized clinical pathways for guideline-concordant antibiotic prescribing and quality of care, clinical decision support tools, and clinical justification for non-recommended antibiotic use.47,48
We acknowledge several possible limitations to this study. First, our study period from 2009–2014 captured the most recent survey data available at the time of the analysis. Although prescribing patterns could have changed in the interim, the trend in antibiotic prescribing did not change significantly during the study period (Supplemental Figure 2b). Second, indications for antibiotics were based on the three diagnosis codes available in the NHAMCS dataset, which were not directly linked to medications mentioned during the visit. The hierarchical classification system used was designed to categorize the most likely diagnosis for which the antibiotic was prescribed. However, it is possible that a small proportion of antibiotic visits grouped as ‘generally not indicated’ might still warrant antibiotic prescribing, such as visits among patients with sickle-cell disease and fever. Third, patient allergies to medications are not captured in the NHAMCS dataset, which could influence the antibiotic class prescribed. However, patient antibiotic allergies would be expected to occur at similar rates in pediatric and non-pediatric EDs. Fourth, longitudinal patient data were not available, nor were data on provider specialty. Finally, although our definition of pediatric EDs has been used previously2,22,23 and is likely quite specific (Supplemental Figure 1), some large non-pediatric EDs might have a specific pediatric subsection that constitutes the minority of visits but is nonetheless staffed by pediatric specialists.
In summary, in this nationally representative study of all ED visits by children, we found the vast majority of pediatric visits and antibiotics ordered or prescribed to children occur in non-pediatric EDs, highlighting the important role of non-pediatric emergency medicine practitioners in improving the quality of antibiotic prescribing for children nationally. Pediatric antibiotic stewardship efforts in non-pediatric EDs have the potential to eliminate over 2 million unnecessary antibiotic prescriptions annually and increase the rates of guideline-concordant antibiotic use among children seen in this setting. Macrolides are frequently and inappropriately prescribed for children in EDs, and non-pediatric EDs in particular. Antibiotic stewardship efforts should expand to EDs nationwide, particularly regarding avoidance of antibiotic prescribing for treatment of conditions for which antibiotics are not indicated, reducing macrolide use, and increasing first line, guideline-concordant prescribing for children, especially in non-pediatric EDs.
Supplementary Material
Supplemental Figure 1: Proportion of visits by children by EDs in NHAMCS, United States, 2009–2014. ED type was defined as pediatric if >75% of all visits to that ED were by patients aged 0–17 years, or non-pediatric otherwise (Bourgeois & Shannon, 2007; Neuman et al., 2013; Bekmezian et al. 2011).
Supplemental Figure 2: (2a) Percent of antibiotic visits prescribing first-line guideline-concordant antibiotics for acute otitis media, pharyngitis, and sinusitis in ED visits by children; and (2b) Percent of ED visits by children prescribed an antibiotic in the United States from 2009–2014.
*First-line, guideline-concordant prescribing defined as amoxicillin or amoxicillin-clavulanate for AOM and sinusitis; penicillin or amoxicillin for pharyngitis. **Change in antibiotic prescriptions over time assessed in 2-year increments. +Antibiotic visits defined as visits in which antibiotics were continued, administered, or prescribed.
#Population denominators based on the 2009 – 2014 set of estimates of the civilian, noninstitutionalized population of the United States, as developed by the Population Division, US Census Bureau.21 No significant change in percentages over study period.
What’s Known on This Subject:
Children are often prescribed antibiotics in EDs. Previous work has examined antibiotic prescribing in EDs for particular diagnostic conditions (e.g., pneumonia), but a comprehensive national evaluation of all antibiotic prescribing for children in pediatric and non-pediatric EDs is lacking.
What This Study Adds:
Children are prescribed over 2 million antibiotics annually in non-pediatric EDs that are likely unnecessary. Compared to pediatric EDs, non-pediatric EDs prescribe more macrolides and fewer guideline-concordant antibiotics for common illnesses. Pediatric antibiotic stewardship efforts are needed in EDs nationwide.
Acknowledgments
Financial Source: Funding for this study was provided by the Centers for Disease Control and Prevention through IPA number 171IPA1708452.
Financial Disclosure: All authors have no financial relationships relevant to this article to disclose.
Abbreviations:
- ED
emergency department
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- MSA
metropolitan statistical area
- ARTI
acute respiratory tract infection
- AOM
acute otitis media
- SSTI
skin and soft tissue infection
- UTI
urinary tract infection
- CI
confidence interval
- aOR
adjusted odds ratio
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References:
- 1.Gindi RM, Jones LI. Reasons for Emergency Room Use Among U.S. Children: National Health Interview Survey, 2012. Vol Data Brief No. 160: NCHS July 2014. [PubMed] [Google Scholar]
- 2.Bourgeois FT, Shannon MW. Emergency care for children in pediatric and general emergency departments. Pediatr Emerg Care. 2007;23(2):94–102. [DOI] [PubMed] [Google Scholar]
- 3.Raofi S, Schappert SM. Medication therapy in ambulatory medical care: United States, 2003–04. Vital Health Stat 13 2006(163):1–40. [PubMed] [Google Scholar]
- 4.Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–1061. [DOI] [PubMed] [Google Scholar]
- 5.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA. 2016;315(17):1864–1873. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chemother. 2014;69(1):234–240. [DOI] [PubMed] [Google Scholar]
- 7.Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Danziger LH. A national evaluation of antibiotic expenditures by healthcare setting in the United States, 2009. J Antimicrob Chemother. 2013;68(3):715–718. [DOI] [PubMed] [Google Scholar]
- 8.Hicks LA, Chien YW, Taylor TH, Haber M, Klugman KP, Team ABCSA. Outpatient antibiotic prescribing and nonsusceptible Streptococcus pneumoniae in the United States, 1996–2003. Clin Infect Dis. 2011;53(7):631–639. [DOI] [PubMed] [Google Scholar]
- 9.Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis. 2015;60(9):1308–1316. [DOI] [PubMed] [Google Scholar]
- 10.The White House. National action plan for combating antibiotic-resistant bacteria. 2015.
- 11.Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol. 2012;33(4):322–327. [DOI] [PubMed] [Google Scholar]
- 12.Mistry RD, Newland JG, Gerber JS, et al. Current State of Antimicrobial Stewardship in Children’s Hospital Emergency Departments. Infect Control Hosp Epidemiol. 2017;38(4):469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mistry RD, Dayan PS, Kuppermann N. The battle against antimicrobial resistance: time for the emergency department to join the fight. JAMA Pediatr. 2015;169(5):421–422. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Monuteaux MC, Bachur RG. Variation in Pediatric Care Between Academic and Nonacademic US Emergency Departments, 1995–2010. Pediatr Emerg Care. 2017. doi: 10.1097/PEC.0000000000001036 [DOI] [PubMed] [Google Scholar]
- 15.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304(6):664–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knapp JF, Simon SD, Sharma V. Variation and trends in ED use of radiographs for asthma, bronchiolitis, and croup in children. Pediatrics. 2013;132(2):245–252. [DOI] [PubMed] [Google Scholar]
- 17.Shah S, Bourgeois F, Mannix R, Nelson K, Bachur R, Neuman MI. Emergency Department Management of Febrile Respiratory Illness in Children. Pediatr Emerg Care. 2016;32(7):429–434. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics. Ambulatory Health Care Data. Datasets and Documentation. https://www.cdc.gov/nchs/ahcd/datasets_documentation_related.htm. Accessed March 11, 2018.
- 19.Centers for Disease Control and Prevention, National Center for Health Statistics. Ambulatory Health Care Data. Data Products. https://www.cdc.gov/nchs/ahcd/new_ahcd.htm. Accessed March 31, 2017, 2017.
- 20.U.S. Department of Commerce Economics and Statistics Administration, U.S. Census Bureau. Census Regions and Divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed May 25, 2018.
- 21.U.S. Department of Commerce Economics and Statistics Administration, U.S. Census Bureau, Population Division. Monthly Population Estimates for the Unites States. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed May 31, 2018.
- 22.Neuman MI, Shah SS, Shapiro DJ, Hersh AL. Emergency department management of childhood pneumonia in the United States prior to publication of national guidelines. Acad Emerg Med. 2013;20(3):240–246. [DOI] [PubMed] [Google Scholar]
- 23.Bekmezian A, Hersh AL, Maselli JH, Cabana MD. Pediatric emergency departments are more likely than general emergency departments to treat asthma exacerbation with systemic corticosteroids. J Asthma. 2011;48(1):69–74. [DOI] [PubMed] [Google Scholar]
- 24.Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964–999. [DOI] [PubMed] [Google Scholar]
- 25.Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(10):1279–1282. [DOI] [PubMed] [Google Scholar]
- 26.Wald ER, Applegate KE, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262–280. [DOI] [PubMed] [Google Scholar]
- 27.McCaig LF, Burt CW. Understanding and interpreting the National Hospital Ambulatory Medical Care Survey: key questions and answers. Ann Emerg Med. 2012;60(6):716–721. e711. [DOI] [PubMed] [Google Scholar]
- 28.Fleming-Dutra KE, Shapiro DJ, Hicks LA, Gerber JS, Hersh AL. Race, otitis media, and antibiotic selection. Pediatrics. 2014;134(6):1059–1066. [DOI] [PubMed] [Google Scholar]
- 29.Hersh AL, Fleming-Dutra KE, Shapiro DJ, Hyun DY, Hicks LA, Workgroup OAUT-S. Frequency of First-line Antibiotic Selection Among US Ambulatory Care Visits for Otitis Media, Sinusitis, and Pharyngitis. JAMA Intern Med. 2016;176(12):1870–1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanchez GV, Hersh AL, Shapiro DJ, Cawley JF, Hicks LA. Outpatient Antibiotic Prescribing Among United States Nurse Practitioners and Physician Assistants. Open Forum Infect Dis. 2016;3(3):ofw168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goyal MK, Johnson TJ, Chamberlain JM, et al. Racial and Ethnic Differences in Antibiotic Use for Viral Illness in Emergency Departments. Pediatrics. 2017;140(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehrotra A, Gidengil CA, Setodji CM, Burns RM, Linder JA. Antibiotic prescribing for respiratory infections at retail clinics, physician practices, and emergency departments. Am J Manag Care. 2015;21(4):294–302. [PubMed] [Google Scholar]
- 33.Hasegawa K, Tsugawa Y, Cohen A, Camargo CA Jr. Infectious Disease-related Emergency Department Visits Among Children in the US. Pediatr Infect Dis J. 2015;34(7):681–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vu TT, Hampers LC, Joseph MM, et al. Job market survey of recent pediatric emergency medicine fellowship graduates. Pediatr Emerg Care. 2007;23(5):304–307. [DOI] [PubMed] [Google Scholar]
- 35.Dharmar M, Marcin JP, Romano PS, et al. Quality of care of children in the emergency department: association with hospital setting and physician training. J Pediatr. 2008;153(6):783–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nadeem Ahmed M, Muyot MM, Begum S, Smith P, Little C, Windemuller FJ. Antibiotic prescription pattern for viral respiratory illness in emergency room and ambulatory care settings. Clin Pediatr (Phila). 2010;49(6):542–547. [DOI] [PubMed] [Google Scholar]
- 37.Saleh EA, Schroeder DR, Hanson AC, Banerjee R. Guideline-concordant antibiotic prescribing for pediatric outpatients with otitis media, community-acquired pneumonia, and skin and soft tissue infections in a large multispecialty healthcare system. Clin Res Infect Dis. 2015;2(1). [PMC free article] [PubMed] [Google Scholar]
- 38.Fleming-Dutra KE, Demirjian A, Bartoces M, Roberts RM, Taylor TH, Hicks LA. Variations in Antibiotic and Azithromycin Prescribing for Children by Geography and Specialty - United States, 2013. Pediatr Infect Dis J. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez GV, Shapiro DJ, Hersh AL, Hicks LA, Fleming-Dutra KE. Outpatient Macrolide Antibiotic Prescribing in the United States, 2008–2011. Open Forum Infect Dis. 2017;4(4):ofx220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yaeger JP, Temte JL, Hanrahan LP, Martinez-Donate P. Roles of Clinician, Patient, and Community Characteristics in the Management of Pediatric Upper Respiratory Tract Infections. Ann Fam Med. 2015;13(6):529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bradley JS, Byington CL, Shah SS, et al. Executive summary: the management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):617–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Streptococcus pneumoniae, 2015. Active Bacterial Core Surveillance Report, Emerging Infections Program Network 2015; https://www.cdc.gov/abcs/reports-findings/survreports/spneu15.html. Accessed May 1, 2018.
- 43.Ralston SL, Lieberthal AS, Meissner HC., et al. Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. Pediatrics. 2014;134(5):e1474–e1502. [DOI] [PubMed] [Google Scholar]
- 44.Snow V, Mottur-Pilson C, Gonzales R, et al. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults. Ann Intern Med. 2001;134(6):487–489. [DOI] [PubMed] [Google Scholar]
- 45.Hersh AL, Jackson MA, Hicks LA, Diseases AAoPCoI. Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics. 2013;132(6):1146–1154. [DOI] [PubMed] [Google Scholar]
- 46.Irwin RS, Baumann MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):1S–23S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sanchez GV, Fleming-Dutra KE, Roberts KB, Hicks L. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep. 2016. November 11;65(6):1–12. doi: 10.15585/mmwr.rr6506a1 [DOI] [PubMed] [Google Scholar]
- 48.May L, Cosgrove S, L’Archeveque M, et al. A call to action for antimicrobial stewardship in the emergency department: approaches and strategies. Ann Emerg Med. 2013;62(1):69–77 e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Proportion of visits by children by EDs in NHAMCS, United States, 2009–2014. ED type was defined as pediatric if >75% of all visits to that ED were by patients aged 0–17 years, or non-pediatric otherwise (Bourgeois & Shannon, 2007; Neuman et al., 2013; Bekmezian et al. 2011).
Supplemental Figure 2: (2a) Percent of antibiotic visits prescribing first-line guideline-concordant antibiotics for acute otitis media, pharyngitis, and sinusitis in ED visits by children; and (2b) Percent of ED visits by children prescribed an antibiotic in the United States from 2009–2014.
*First-line, guideline-concordant prescribing defined as amoxicillin or amoxicillin-clavulanate for AOM and sinusitis; penicillin or amoxicillin for pharyngitis. **Change in antibiotic prescriptions over time assessed in 2-year increments. +Antibiotic visits defined as visits in which antibiotics were continued, administered, or prescribed.
#Population denominators based on the 2009 – 2014 set of estimates of the civilian, noninstitutionalized population of the United States, as developed by the Population Division, US Census Bureau.21 No significant change in percentages over study period.