Abstract
Objective
Traditional measures for assessing functioning with adult patients with schizophrenia have been shown to be insufficient for assessing the issues that occur in adolescents and young adults at clinical high risk (CHR) for psychosis. The current study provides an expanded validation of the Global Functioning: Social (GF:Social) and Role (GF:Role) scales developed specifically for use with CHR individuals and explores the reliability and accuracy of the ratings, the validity of the scores in comparison to other established clinical measures, stability of functioning over a 2-year period, and psychosis predictive ability.
Methods
Seven hundred fifty-five CHR individuals and 277 healthy control (HC) participants completed the GF:Social and Role scales at baseline as part of the North American Prodrome Longitudinal Study (NAPLS2).
Results
Inter-rater reliability and accuracy were high for both scales. Correlations between the GF scores and other established clinical measures demonstrated acceptable convergent and discriminant validity. In addition, GF:Social and Role scores were unrelated to positive symptoms. CHR participants showed large impairments in social and role functioning over 2-years, relative to the HCs, even after adjusting for age, IQ, and attenuated positive symptoms. Finally, social decline prior to baseline was more pronounced in CHR converters, relative to non-converters.
Conclusions
The GF scales can be administered in a large-scale multi-site study with excellent inter-rater reliability and accuracy. CHR individuals showed social and role functioning impairments over time that were not confounded by positive symptom severity levels. The results of this study demonstrate that social decline is a particularly effective predictor of conversion outcome.
Keywords: Prodromal, Adolescent, NAPLS, CHR, scale validation, Global Functioning: Social, Global Functioning: Role
Early intervention and prevention research in the psychosis prodrome has recently evolved in scope by broadening the outcome of interest to include not only transition to schizophrenia and/or other psychotic disorders, but also poor functioning.1–8 This has occurred for several reasons, but chief among them is the increasing awareness that functional disability, not positive symptoms,9–13 overwhelmingly accounts for the large personal and financial burden of the illness.14 Studying functioning prior to the onset of psychosis, when individuals are less impaired and at a point where social, academic, and occupational skills are acquired and generalized,15,16 may, therefore, provide a critical window of opportunity to limit long-term functional difficulties. In this context, functioning refers to 2 primary behavioral constructs: social skills (ie, interpersonal interactions/activities) and role performance (ie, academic/work achievement). Two scales were specifically designed to measure each construct independently in prodromal youth and were initially shown cross-sectionally to have good psychometric characteristics and potential to predict psychosis. The present study aims to longitudinally validate the Global Functioning: Social (GF:Social) and Role (GF:Role)17 scale rating system on a large sample of adolescents and young adults at clinical high risk (CHR) for psychosis, and, in turn, provide information about the involvement of both functional domains in predicting illness.
Functional disability has long been associated with chronic schizophrenia.18,19 However, at the outset of prodromal research, traditional functional measures were rapidly discovered to be insufficient for assessing at-risk behaviors which are more subtle than difficulties observed in adult patients with chronic illness. For example, adult functioning scales do not address the distinct functional issues that occur in adolescence and young adulthood (eg, peer interactions, dating, school settings, etc.). Moreover, one of the most widely used adult measures, the Global Assessment of Functioning (GAF) is psychometrically problematic and associated more with psychiatric symptoms than actual functioning.20–22 Recognizing this gap, Cornblatt and colleagues designed the GF scales to provide brief and easy to use clinician ratings, account for age and phase of illness, detect changes over time, avoid confounding with psychiatric symptoms, and disentangle the social and role functional domains.17 Each scale is extensively anchored to reflect comparable success/failure, so that, for example, a score of 6 (scale from 1 to 10) indicates the same level of impairment on both scales.
In the initial validation study, Cornblatt et al17 demonstrated high inter-rater reliability for both scales and preliminary data supported construct and discriminant validity. Ratings of social and role functioning were independent of attenuated positive, disorganized, and general symptoms as rated by the Scale of Prodromal Symptoms (SOPS23–25), IQ and parental education. In addition, relative to healthy controls, CHR individuals displayed impaired social and role functioning at baseline. These early findings supported the inclusion of both GF scales across the 3 phases of the multi-site North American Prodrome Longitudinal Study (NAPLS).
In addition to consistent functional deficits, a decline in functioning, specifically in the social domain, has been found to predict transition to psychosis in several studies.26–29 Most recently, the NAPLS study included social decline as measured by the GF:Social scale in the online Psychosis Risk Calculator, which along with select positive symptoms, neurocognitive deficits, and other demographic information (eg, age) was found to significantly predict psychosis.27 Further, apart from positive symptoms, social decline was found to have the largest impact on the overall accuracy of the model when removed.27 Collectively, these findings demonstrate the robust ability of the GF scales to detect functional impairments in CHR youth and sensitivity to predict transition to psychosis.
Since the initial validation,17 the 2 scales have been used nationally and internationally in a variety of settings and contexts, including several wide-scale multi-site CHR studies,30–34 studies with young adults in their first episode of psychosis35–37 and schizophrenia.38,39 In addition, the scales have been used in several clinical trials,33,36,38,40–50 and have been translated into Italian, German, Dutch, Chinese, Danish, and Korean.34,51,52 Therefore, it is critical to provide a continual demonstration of the reliability, accuracy, and predictive performance of the scales in different studies.
The present study provides an expanded validation of the GF scales in a large sample of CHR individuals collected as part of NAPLS2. The initial validation study only included 2 sites, the Recognition and Prevention (RAP) program at The Zucker Hillside Hospital53 and the University of California Los Angeles (UCLA). The main goals are to: (1) evaluate the inter-rater agreement of the GF ratings collected at the different NAPLS2 sites; (2) examine the stability of functioning over 2 years in healthy controls and CHR subjects; (3) demonstrate convergent and discriminant validity by comparing GF:Social and Role scores to other established clinical measures; and (4) evaluate the ability of functioning scores to predict transition to psychosis and explore the range of decline amongst the CHR cases who did (ie, converters) and did not (ie, non-converters) develop psychosis.
Methods
Participants
Data was collected as part of NAPLS2 (N = 1042), an 8-site prospective study funded by the National Institute of Mental Health.32 The NAPLS2 sample consists of 764 clinical high-risk (CHR) subjects and 278 healthy control (HC) participants. Seven hundred fifty-five CHR individuals and 277 HCs completed the GF:Social and Role scales at baseline. Subjects were collected at Emory University, Harvard University, University of Calgary, UCLA, UCSD, UNC at Chapel Hill, Yale University, and the Zucker Hillside Hospital in New York. Recruitment efforts varied at the 8 sites and primarily resulted from direct referrals, referrals from community professionals, and advertising in the community and the internet.31
CHR subjects met criteria for 1 of the 3 prodromal syndromes derived from the SOPS23–25: (1) attenuated positive symptom syndrome: the presence of one or more moderate, moderately severe, or severe attenuated positive symptoms (scores of 3, 4, or 5 on the SOPS, on a scale of 0–6); (2) genetic risk and deterioration syndrome: genetic risk for psychosis coupled with deterioration in functioning; or (3) brief intermittent psychotic syndrome: intermittent psychotic symptoms that are recent, brief in duration, and not seriously disorganizing or dangerous. CHR and HCs between the ages of 12–35 were eligible to participate.
Exclusion criteria for all participants included: (1) any axis I schizophrenia-spectrum diagnosis; (2) non-English speaking; (3) a medical or neurological disorder; (4) estimated IQ < 70; (5) significant head injury; or (6) severe substance abuse. HCs were additionally excluded if they had a first-degree relative with a diagnosed axis I psychotic disorder. All procedures were approved by the Institutional Review Board (IRB) at each site. Written informed consent (with assent from participants <18) was obtained from all participants.
Measures
Details of the comprehensive baseline clinical assessment have been reported previously.32 Axis I diagnoses were assessed by the Structured Clinical Interview for DSM-IV (SCID-I54). Prodromal symptoms were assessed by the Structured Interview for Prodromal Syndromes (SIPS) and the companion SOPS.23–25 Total scores for each subscale (Positive, Negative, Disorganized, General) were calculated. The Calgary Depression Scale for Schizophrenia (CDSS55–57) assessed depressive symptoms. Premorbid functioning was measured with the Premorbid Adjustment Scale (PAS58). The PAS is a semi-structured interview that asks individuals to describe their social and role adjustment in childhood, early adolescence, and late adolescence. Social and role functioning were assessed with the GF:Social and GF:Role scales.17 The GF:Social scale assesses peer relationships, peer conflict, age-appropriate intimate relationships, and family involvement. The GF:Role scale rates performance and amount of support needed in one’s specific role (ie, school, work).17 Each GF scale generates 3 scores: (1) current level, (2) highest, and (3) lowest level of functioning in the past year prior to the assessment.
GF Training Procedures
To establish inter-rater reliability across the 8 sites, 8 written cases, based on de-identified case reports, were distributed to 48 raters. The 8 written cases were based on cases presented on consensus calls and the HC pool at ZHH. Prior to scoring the 8 cases, all raters received training on the administration and guidelines for scoring the GF scales by A.M.A. The raters were blind to group membership. Each case generated 6 scores (current, lowest, and highest for both social and role), for a total of 48 scores per rater.
Statistical Analyses
All analyses were conducted using SPSS 20.0 (SPSS Inc.). Comparisons of demographic and clinical characteristics were performed with Student’s t-tests for continuous variables, Pearson Chi-square for categorical variables (2-tailed, P < .05).
The reliability, accuracy, and validity of the GF scales was explored with the following procedures: (1) inter-rater reliability and the agreement between raters across the sites was assessed with intraclass correlations (ICC, 2-way mixed-effects model with absolute agreement)59; (2) accuracy of the ratings was assessed by correlations between the ratings at each site with the gold-standard rating.60 The gold standard rating was a consensus rating between 3 Hillside raters (A.M.A., Rita Barsky, and Stephanie Snyder); (3) convergent and discriminant validity were determined by examining correlations between the GF:Social and Role scales and scores on the: (a) SOPS Attenuated Positive, Negative, Disorganized, and General Symptom scales, (b) GAF, (c) CDSS, and (d) PAS. In addition, in order to determine the relative contribution of other potential nonpsychiatric confounders, we examined the relationships between the GF scales and baseline age, education, and current IQ.
Linear mixed-effects models for repeated measures were used to evaluate group differences between the HC vs CHR groups in social and role functioning over the course of the study.61–64 GF:Social and Role scores at each visit (Baseline, 6 mo, 1 y, 18 mo, and 2 y) were used as the primary dependent variables. Fixed effects were group and time (5 visits) and the group and time interaction. The subjects were entered as a random effect. Restricted maximum likelihood estimation and type III tests of fixed effects were used, with an autoregressive (1) covariance structure. Follow-up analyses adjusted the comparisons between HCs and CHRs for age, education, and positive symptom severity at the assessment.
Decline in social and role functioning at baseline was defined as: Decline = Highest level – Current functioning.17,27,65 These analyses were conducted using data for subjects who had either developed a psychotic disorder (N = 94) or who had been followed at least 24 months without developing psychosis (N = 272).66
Results
Baseline Characteristics
Table 1 summarizes baseline demographic and clinical characteristics of the study sample. HCs and CHR subjects did not differ significantly on race, ethnicity, or the proportion of subjects enrolled as students (table 1). However, HCs were older and had more years of education compared to the CHR group. In addition, HCs had higher estimated premorbid and current IQ scores. The CHR group had a slightly higher proportion of males (P = .05).
Table 1.
Demographic and Clinical Characteristics of the Healthy Controls and CHR Subjects
| Healthy Controls (N = 277) | CHR (N = 755) | P Value | |
|---|---|---|---|
| Age, y | 19.74 (4.68) | 18.50 (4.25) | <.001 |
| Education, y | 12.68 (3.58) | 11.27 (2.82) | <.001 |
| Sex, male, N (%) | 139 (50.4) | 431 (57.3) | .05 |
| Race, White, N (%) | 151 (54.7) | 430 (57.2) | .48 |
| Ethnic origin, Hispanic, N (%) | 50 (18.1) | 142 (18.9) | .86 |
| Premorbid IQ | 108.50 (16.44) | 105.18 (16.39) | .006 |
| Current IQ | 111.05 (14.24) | 103.71 (15.32) | <.001 |
| Enrolled as student, N (%) | 224 (81.2) | 617 (82.3) | .71 |
| Scale of prodromal symptoms | |||
| Positive | 1.04 (1.62) | 11.89 (3.81) | <.001 |
| Negative | 1.42 (2.22) | 11.91 (6.07) | <.001 |
| Disorganized | 0.64 (1.17) | 5.16 (3.16) | <.001 |
| General | 1.33 (2.15) | 9.09 (4.28) | <.001 |
| GAF Score | 83.70 (10.35) | 48.31 (10.68) | <.001 |
| Global functioning: Social Scale | 8.86 (0.92) | 6.19 (1.57) | <.001 |
| Global functioning: Role Scale | 8.56 (1.34) | 5.95 (2.14) | <.001 |
Note: CHR, clinical high risk; GAF, Global Assessment of Functioning.
CHR subjects had significantly higher levels of SOPS rated attenuated positive, negative, disorganized, general symptoms, and CDSS scores, and lower GAF scores compared to the HCs. The CHR group also demonstrated significant impairments in social and role functioning in comparison to HCs (table 1).
Reliability and Accuracy
For the GF:Social scale, a measurement of intraclass correlation (ICC) indicated an overall correlation between raters of 0.956 (95% CI = 0.904–0.989) for the current level, 0.954 (95% CI = 0.899–0.989) for the highest level in the past year, and 0.926 (95% CI = 0.843–0.981) for the lowest level of functioning in the past year. For the GF:Role scale, there was an overall correlation between raters of 0.926 (95% CI = 0.844–0.981) for the current level, 0.926 (95% CI = 0.844–0.981) for the highest level in the past year, and 0.933 (95% CI = 0.857–0.983) for the lowest level in the past year. The ICC between raters at each of the 8 sites ranged between 0.944 and 1.0 for GF:Social and between 0.913 and 1.0 for GF:Role, suggesting excellent agreement between raters across the 8 sites.
In addition to determining the reliability of the ratings across sites on the 8 cases, the accuracy of the ratings was examined by comparing each rater to the gold standard rating. Overall, the accuracy of the ratings was excellent. The average correlations across the sites ranged from 0.904 to 0.973, overall suggesting that the raters were able to rate the cases reliably and accurately.
Discriminant and Convergent Validity
As seen in table 2, both the GF:Social and Role scales showed small-to-no correlations with item and total scores on the SOPS Positive, Disorganized, General Symptoms scales, and CDSS, within the CHR group, indicating that the GF measures avoid confounding levels of functioning with psychiatric symptoms. The GF:Social scale showed small cross-domain correlations with the SOPS N6 item of Occupational Functioning (r = −.297, P < .001) and the PAS current role functioning domain score (r = −.282, P < .001). Similarly, the GF:Role scale showed weak correlations with the SOPS N1 item of Social Anhedonia (r = −.160, P < .001) and PAS current social functioning domain score (r = −.141, P < .001) (table 2), further suggesting that social and role functioning are separate domains. Indeed, a moderate correlation was observed between the GF:Social and Role Scales (r = .362, P < .001).
Table 2.
Divergent and Convergent Validity of the GF: Social and Role Scales
| GF: Social | GF: Role | |
|---|---|---|
| Age | −0.016 | 0.054 |
| Education level | 0.031 | 0.143*** |
| IQ (WASI) | 0.067 | 0.234*** |
| SOPS positive symptoms total | −0.054 | −0.037 |
| P1. Unusual thought content | −0.039 | −0.052 |
| P2. Suspiciousness | −0.117** | 0.063 |
| P3. Grandiosity | −0.004 | −0.005 |
| P4. Perceptual abnormalities | 0.140*** | 0.046 |
| P5. Disorganized communication | −0.122** | −0.135*** |
| SOPS negative symptoms total | −0.526*** | −0.473*** |
| N1. Social anhedonia | −0.660*** | −0.160*** |
| N2. Avolition | −0.253*** | −0.386*** |
| N3. Decreased expression of emotion | −0.311*** | −0.133*** |
| N4. Decreased experience of emotions and self | −0.149*** | −0.058 |
| N5. Decreased ideational richness | −0.184*** | −0.218*** |
| N6. Occupational functioning | −0.297*** | −0.663*** |
| SOPS disorganized symptoms total | −0.229*** | −0.230*** |
| D1. Odd behavior or appearance | −0.222*** | −0.128** |
| D2. Bizarre thinking | −0.106** | −0.036 |
| D3. Trouble with focus and attention | −0.075* | −0.218*** |
| D4. Impairment in personal hygiene | −0.222*** | −0.214*** |
| SOPS total general symptoms total | −0.161*** | −0.149*** |
| G1. Sleep disturbances | −0.089* | −0.180*** |
| G2. Dysphoric mood | −0.177*** | −0.093* |
| G3. Motor disturbances | −0.073* | −0.085* |
| G4. Impaired tolerance to normal stress | −0.123** | −0.079* |
| GAF | 0.407*** | 0.505*** |
| Calgary Depression Scale, Total | −0.242*** | −0.059 |
| Premorbid Adjustment Scale, Current Score, Social | −0.562*** | −0.141*** |
| Premorbid Adjustment Scale, Current Score, Role | −0.282*** | −0.535*** |
Note: GAF, Global Assessment of Functioning; SOPS, Scale of Prodromal Symptoms.
*P < .05; **P < .01; ***P < .001.
In terms of convergent validity, the GF:Social scale was strongly correlated with the SOPS N1 item of Social Anhedonia (r = −.660, P < .001) and PAS current social functioning domain score (r = −.562, P < .001). The GF:Role scale was strongly correlated with the SOPS N6 item of Occupational Functioning (r = −.663, P < .001) and PAS current role functioning domain score (r = −.535, P < .001).
As expected both GF scales were moderately correlated with GAF scores (GF:Social, r = .407, P < .001; GF:Role, r = .505, P < .001). However, while the GAF measures functioning, it also measures symptom severity, as shown through moderate correlations with the SOPS Negative (r = −.495, P < .001) and General symptom scales (r = −.351, P < .001), and CDSS (r = −.308, P < .001).
Finally, both GF scales showed small-to-no correlations with baseline age (GF:Social, r = −.016, P = .660; GF:Role, r = .054, P = .138), education (GF:Social, r = .031, P = .392; GF:Role, r = .143, P < .001), and current IQ (GF:Social, r = .067, P = .08; GF:Role, r = .234, P < .001) (table 2).
Stability
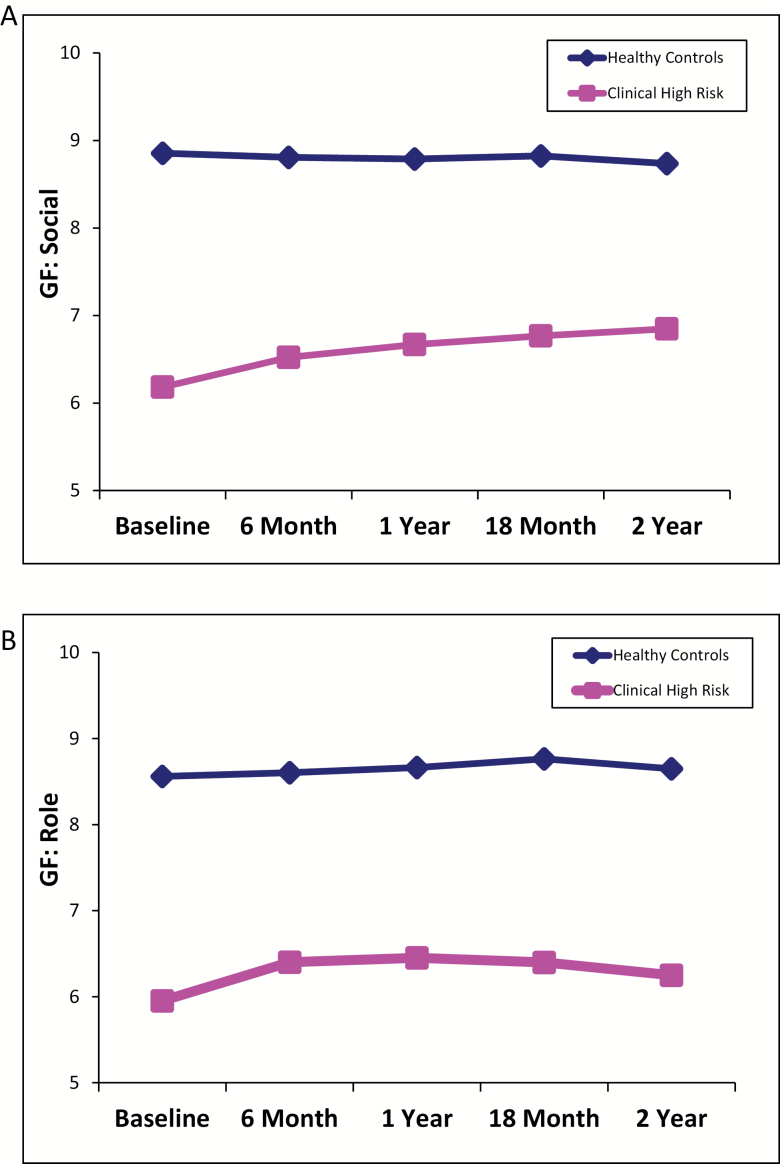
As shown in figures 1A and 1B, compared to HCs, CHR subjects showed a consistent impairment over time in social (P < .001) and role (P < .001) functioning. The linear mixed-models for repeated measures also revealed significant time effects for both social (P < .001) and role (P < .001), as well as group × time interactions (Social, P < .001 and Role, P = .03). There was a significant improvement in functioning levels for the overall CHR group in both social and role. However, the overall CHR group did not approach HC levels by the 2nd year (supplementary table S1). Follow-up analyses adjusting for age, positive symptom severity, and education levels showed similar results, with significant group differences between HCs and CHR subjects in social (P < .001) and role (P < .001) functioning, as well as significant effects of time for both scales (Social, P = .001, Role, P = .004). However, while the significant group x time interaction was not affected for social (P < .001), the interaction was not significant for role functioning (P = .285), after adjusting for age, positive symptoms, and education (see supplementary methods and results for more details).
Fig. 1.
Current (A) Social and (B) Role functioning at each assessment over 2 years for healthy controls and clinical high-risk subjects. Mean GF scores are estimated marginal means derived from the linear mixed models for repeated measures.
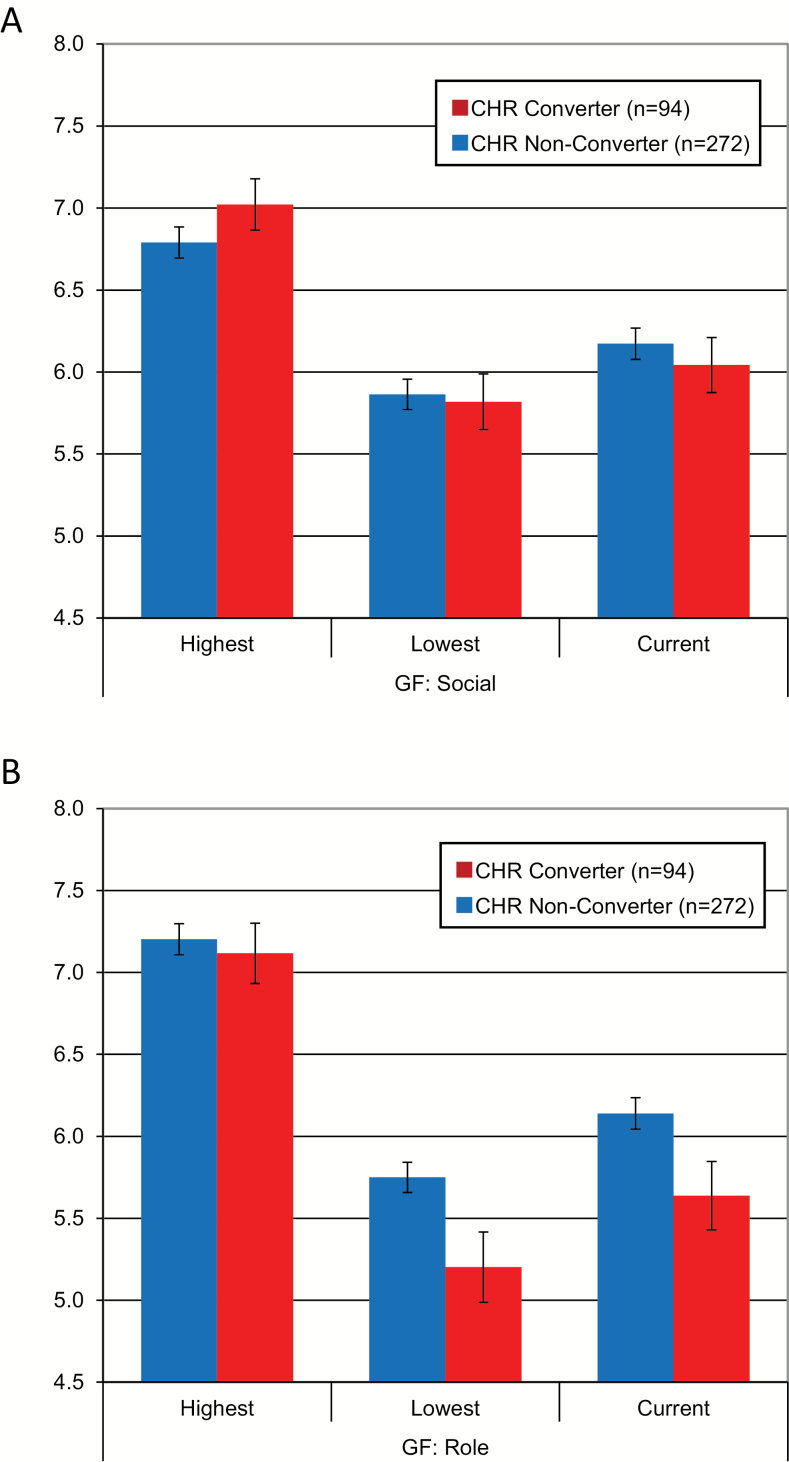
Predictive Ability—Functional Decline
Figures 2A and 2B display the current, highest and lowest GF:Social and Role scores at baseline for the CHR converters and non-converters. At baseline, there were no significant differences between converters and non-converters for current (P = .492), highest (P = .214), or lowest (P = .810) social functioning. For role functioning, there was a trend difference (P = .051) between converters and non-converters for the current level of role functioning at baseline and a significant difference for the lowest level of role functioning in the past year (P = .032). There was no difference in the highest level of role functioning in the past year (P = .686).
Fig. 2.
Mean (±Standard Error of the Mean) highest in the past year, lowest in the past year, and current (A) GF: Social and (B) role scores for converters and non-converters at baseline.
For social decline, converters (mean = 0.98, SD = 1.15) showed a larger drop from the highest level of functioning to the current level at baseline, compared to non-converters (mean = 0.62, SD = 0.94, P = .007). Levels of role decline showed a trend-level difference between converters (mean = 1.48, SD = 1.75) and non-converters (mean = 1.07, SD = 1.61, P = .05).
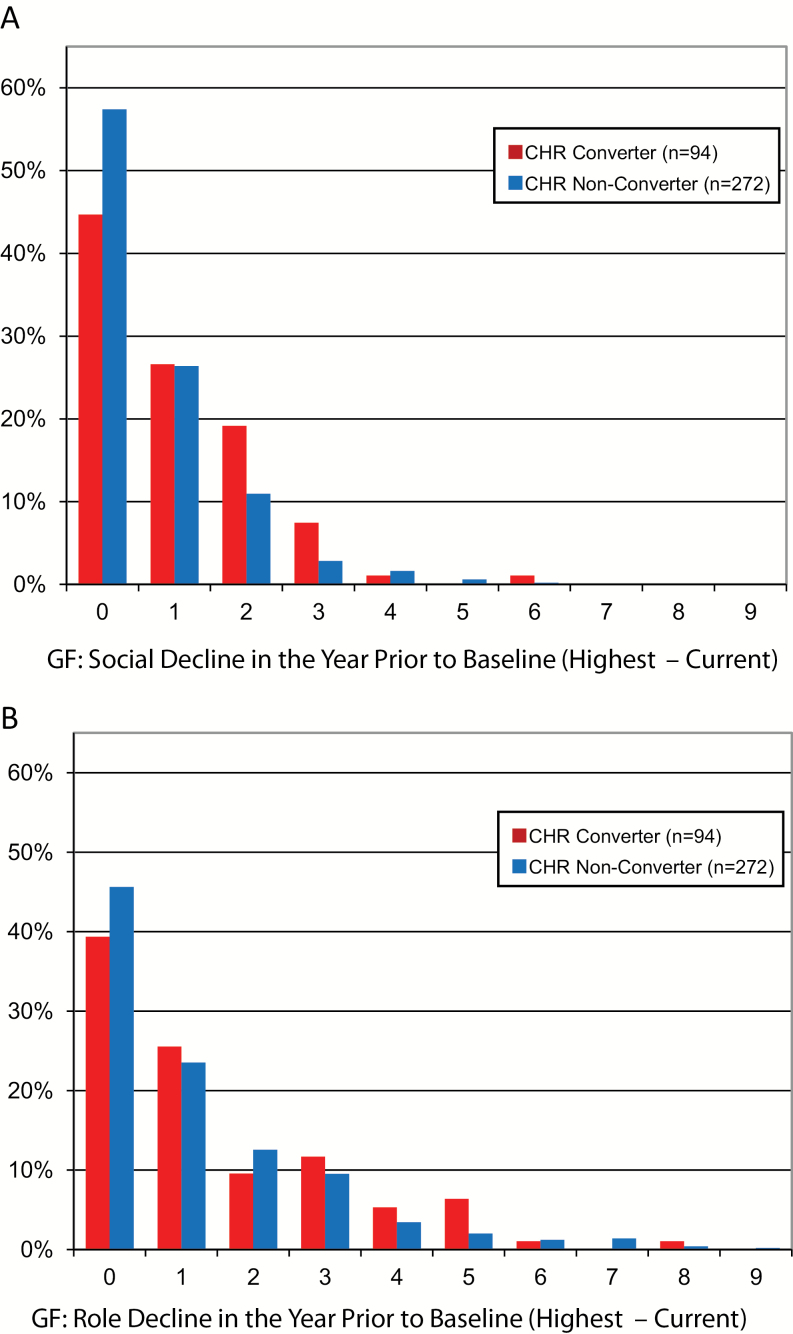
As shown in figure 3A, in terms of the distribution of social decline, a majority of the non-converters (57.4%) showed no social decline (ie, GFS decline = 0). By contrast, a significantly lower proportion of converters (44.7%, P = .010), showed no social decline. This indicates that the converters showed greater levels of decline when compared to the non-converters (figure 3A).
Fig. 3.
Distribution of (A) Social and (B) Role decline in the year prior to baseline (highest – current) for converters and non-converters.
For example, 55.3% of the converters had a decline of 1 point or greater compared to 40.4% of the non-converters. Likewise, 28.7% of the converters had a social decline of 2 points or greater compared to 16.2% of the non-converters (see figure 3A for more details). Compared to social functioning, the distribution of role decline was broader and not significantly different between converters and non-converters (P = .143).
As shown in figure 3B, for role decline, 45.6% of the non-converters showed no decline, compared to 39.4% of the converters. Sixty-one percent of the converters had a decline ≥1 point compared to 54.4% of the non-converters. Thirty-five percent of the converters had a role decline ≥2 points or greater compared to 30% of the non-converters.
Discussion
In previous research with patients with schizophrenia, a variety of measures have been used to assess social and role functioning. However, these scales are commonly fraught with psychometric issues and are not appropriate for use with CHR youth. Building on the findings from the preliminary validation study,17 the current study demonstrated that the GF scales can be administered in a large-scale multi-site study with excellent reliability and accuracy amongst raters. In addition, functioning levels were not confounded by symptom severity and CHR individuals showed stable impairments, relative to healthy controls, over 2 years. Finally, social decline prior to baseline was more pronounced in CHR converters, further supporting its placement in the NAPLS Psychosis Risk Calculator.27,65
Consistent with previous findings,17 the ratings collected across the sites on the written cases were highly reliable, with ICCs for the both GF scales above .90. This suggests that different raters within each site can derive consistent scores with each other. In terms of accuracy, the ratings were very closely related to the gold standard ratings, establishing that the raters can score the GF scales correctly. To date, a few studies have used the GF scales without training or training with a limited set of vignettes. However, this report strongly suggests that training should be implemented prior to its use in order to maximize their effectiveness. As a result, a training package has been developed for standardizing training, especially in multi-site studies. The training package includes a background on scale development, validation and prediction findings, scale descriptions, a broader, more complex array of training vignettes and reviews of the scores and interview prompts. Preliminary data has found this training to be critical for promoting reliability, accuracy, and validity multi-site studies.
The GF scores were not related to age, education level, and IQ, further supporting their use in studying developmental mechanisms. Correlations between the GF scores and other established measures demonstrated acceptable construct validity. In terms of discriminant validity, GF scores were not meaningfully related to the SOPS Positive, Disorganized, General subscales, or depressive symptoms. The GF:Social and Role scores were moderately related to the GAF, providing convergent validity. Additionally, GF:Social scores were strongly related to PAS Social scores and Social Anhedonia (SOPS N1) and GF: Role scores were strongly related to PAS Role scores and Occupational Functioning (SOPS N6) and cross-domain correlations were low. These findings re-confirm that the 2 scales are not impacted by symptom severity and are assessing domain (social and role) specific functioning.
CHR individuals showed impairments in social and role functioning, relative to healthy controls, over a 2-year period. Previous findings from NAPLS1 and the RAP Program also demonstrated longitudinal impairments on the GF:Social and Role scales.67 Similarly, in the current report, while the overall CHR group shows improvements over time in both social and role, functioning levels never reach those seen in the HCs. These findings add to a growing body of evidence that CHR criteria are associated with persistent functional impairments,2,4,7,67–72 suggesting that these individuals are additionally at-risk for long-term functional disability. Moreover, these findings highlight that the GF measures are uniquely appropriate for the prodromal phase of psychosis, in that social and role functioning can be assessed separately, but can be directly compared with each other because the scales have parallel anchor points.
CHR converters showed greater social decline in the year prior to baseline, compared to non-converters, adding to the mounting evidence that impairments in social functioning may be a marker of underlying vulnerability to the illness.69,73 Although there was no relationship between current functioning and age, recent findings suggest a complex association between social decline and age in CHR converters. For example, the social decline variable entered in the NAPLS Psychosis Risk Calculator was measured as decline in the past year prior to baseline.27,65 By contrast, Cornblatt and colleagues74 found that social decline over follow-up significantly predicted psychosis. While there might be other explanatory factors, the average age of the CHR cohorts (16-y-old for RAP and 18-y-old for NAPLS2), suggests that mid-adolescence may be a particularly critical period for a decline in social skills in true-positive prodromal patients. Indeed, this developmental period (16- to 18-y-old) coincides with an elevated risk period of developing schizophrenia.75,76 Collectively, these findings indicate that it is critical to take the age of the CHR sample into consideration when examining social decline.
Compared to social decline, the distribution of role decline prior to baseline was more variable and not associated with psychosis onset. This is consistent with previous findings that have shown that role, compared to social impairments, are not as predictive of psychosis.26,77–79 Poor role functioning may be more susceptible to environmental determinants, such as economic factors and access to educational resources80 and may not serve as a direct premorbid marker of psychosis. Moreover, impaired role functioning has been found to be a core aspect of long-term disability.19
Our findings should be considered in the context of certain limitations. First, the current study did not examine the impact of treatment, especially with medication, on changes in functioning over time. Future studies should explore whether different medication classes are related to the longitudinal improvements seen in the CHR group. Second, the GF scales produce 2 independent global functioning scores, rather than producing a single overall score. However, combining social and role is likely to cloud the relative contributions of each domain to the prediction of psychosis and long-term disability. In fact, our findings support separating the domains, as they are differentially related to psychosis onset. Third, the GF scales do not allow the parsing of functionally-relevant components (eg, number of friends), which may be preferred in certain contexts. However, the GF scales were constructed to produce a single score for both domains that are reliable and stable over time, and therefore, more suitable for studying the prediction of psychosis. Finally, a substantial proportion of the conversions occurred prior to the 6-month assessment, thereby making it difficult to examine functional changes over 2-years. The third phase of NAPLS may be better suited to address this question as the functional assessments are spaced closer together (ie, every 2 mo).
Funding
Supported by grants from the National Institute of Mental Health: U01 MH081984 to J.A.; U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to L.J.S.; R01 MH60720, U01 MH082022, and K24 MH76191 to K.S.C.; U01 MH081902 to T.D.C.; P50 MH066286 (Prodromal Core) to C.E.B.; grant U01 MH082004 to D.O.P.; U01 MH081988 to E.F.W.; RO1 MH076989-01 to D.H.M.; U01 MH082022 to S.W.W.; U01 MH081857 and MH61523 to B.A.C.; the Zucker Hillside Hospital NIMH Advanced Center for Intervention and Services Research for the Study of Schizophrenia MH 074543-01 to John M. Kane, M.D. REC received funding from the Brain and Behavior Research Foundation (NARSAD): Young Investigator Grant 19740 and the Let the Sun Shine Run/Walk, Cold Spring, MN. No funding agency had any role in the collection, analysis, and interpretation of data, in the writing of the report, and in the decision to submit the article for publication.
Supplementary Material
Acknowledgment
Dr. Cannon has served as a consultant for the Los Angeles County Department of Mental Health and Boehringer-Ingelheim Pharmaceuticals. The other authors report no conflicts of interest.
References
- 1. Cornblatt BA, Carrión RE. Deconstructing the psychosis risk syndrome: moving the field of prevention forward. JAMA Psychiatry. 2016;73:105–106. [DOI] [PubMed] [Google Scholar]
- 2. Carrión RE, McLaughlin D, Goldberg TE, et al. . Prediction of functional outcome in individuals at clinical high risk for psychosis. JAMA Psychiatry. 2013;70:1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lin A, Wood SJ, Nelson B, Beavan A, McGorry P, Yung AR. Outcomes of nontransitioned cases in a sample at ultra-high risk for psychosis. Am J Psychiatry. 2015;172:249–258. [DOI] [PubMed] [Google Scholar]
- 4. Lin A, Wood SJ, Nelson B, et al. . Neurocognitive predictors of functional outcome two to 13 years after identification as ultra-high risk for psychosis. Schizophr Res. 2011;132:1–7. [DOI] [PubMed] [Google Scholar]
- 5. Michel C, Ruhrmann S, Schimmelmann BG, Klosterkötter J, Schultze-Lutter F. Course of clinical high-risk states for psychosis beyond conversion. Eur Arch Psychiatry Clin Neurosci. 2018;268:39–48. [DOI] [PubMed] [Google Scholar]
- 6. Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, et al. . EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry. 2015;30:388–404. [DOI] [PubMed] [Google Scholar]
- 7. Fusar-Poli P, Rocchetti M, Sardella A, et al. . Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry. 2015;207:198–206. [DOI] [PubMed] [Google Scholar]
- 8. Cotter J, Drake RJ, Bucci S, Firth J, Edge D, Yung AR. What drives poor functioning in the at-risk mental state? A systematic review. Schizophr Res. 2014;159:267–277. [DOI] [PubMed] [Google Scholar]
- 9. Jungbauer J, Wittmund B, Dietrich S, Angermeyer MC. The disregarded caregivers: subjective burden in spouses of schizophrenia patients. Schizophr Bull. 2004;30:665–675. [DOI] [PubMed] [Google Scholar]
- 10. Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30:279–293. [DOI] [PubMed] [Google Scholar]
- 11. Ohaeri JU. The burden of caregiving in families with a mental illness: a review of 2002. Curr Opinion Psychiatry. 2003;16:457–465. [Google Scholar]
- 12. Perlick DA, Rosenheck RA, Kaczynski R, Swartz MS, Cañive JM, Lieberman JA. Components and correlates of family burden in schizophrenia. Psychiatr Serv. 2006;57:1117–1125. [DOI] [PubMed] [Google Scholar]
- 13. Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. PharmacoEcon. 2008;26:149–162. [DOI] [PubMed] [Google Scholar]
- 14. Cloutier M, Aigbogun MS, Guerin A, et al. . The Economic Burden of Schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77:764–771. [DOI] [PubMed] [Google Scholar]
- 15. Neumann CS, Walker EF. Developmental origins of interpersonal deficits in schizophrenia. In: Mueser KT, Tarrier N, eds. Handbook of Social Functioning in Schiophrenia. Boston, MA: Allyn & Bacon, Inc; 1998:121–133. [Google Scholar]
- 16. Henry AD, Coster WJ. Predictors of functional outcome among adolescents and young adults with psychotic disorders. Am J Occup Ther. 1996;50:171–181. [DOI] [PubMed] [Google Scholar]
- 17. Cornblatt BA, Auther AM, Niendam T, et al. . Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007;33:688–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harvey PD. Disability in schizophrenia: contributing factors and validated assessments. J Clin Psychiatry. 2014;75(Suppl 1):15–20. [DOI] [PubMed] [Google Scholar]
- 19. Harvey PD, Heaton RK, Carpenter WT Jr, Green MF, Gold JM, Schoenbaum M. Functional impairment in people with schizophrenia: focus on employability and eligibility for disability compensation. Schizophr Res. 2012;140:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moos RH, McCoy L, Moos BS. Global assessment of functioning (GAF) ratings: determinants and role as predictors of one-year treatment outcomes. J Clin Psychol. 2000;56:449–461. [DOI] [PubMed] [Google Scholar]
- 21. Skodol AE, Link BG, Shrout PE, Horwath E. The revision of axis V in DSM-III-R: should symptoms have been included?Am J Psychiatry. 1988;145:825–829. [DOI] [PubMed] [Google Scholar]
- 22. Bacon SF, Collins MJ, Plake EV. Does the global assessment of functioning assess functioning?J Ment Health Couns. 2002;24:202. [Google Scholar]
- 23. Miller TJ, McGlashan TH, Rosen JL, et al. . Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. [DOI] [PubMed] [Google Scholar]
- 24. Miller TJ, McGlashan TH, Rosen JL, et al. . Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. [DOI] [PubMed] [Google Scholar]
- 25. Miller TJ, McGlashan TH, Woods SW, et al. . Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70:273–287. [DOI] [PubMed] [Google Scholar]
- 26. Cannon TD, Cadenhead K, Cornblatt B, et al. . Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cannon TD, Yu C, Addington J, et al. . An individualized risk calculator for research in prodromal psychosis. Am J Psychiatry. 2016;173:980–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cornblatt BA, Carrión RE, Auther A, et al. . Psychosis prevention: a modified clinical high risk perspective from the Recognition and Prevention (RAP) Program. Am J Psychiatry. 2015;172:986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Velthorst E, Zinberg J, Addington J, et al. . Potentially important periods of change in the development of social and role functioning in youth at clinical high risk for psychosis. Dev Psychopathol. 2018;30:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Addington J, Cadenhead KS, Cannon TD, et al. ; North American Prodrome Longitudinal Study North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr Bull. 2007;33:665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Addington J, Cadenhead KS, Cornblatt BA, et al. . North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophr Res. 2012;142:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Addington J, Liu L, Buchy L, et al. . North American Prodrome Longitudinal Study (NAPLS 2): the prodromal symptoms. J Nerv Ment Dis. 2015;203:328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McFarlane WR, Levin B, Travis L, et al. . Clinical and functional outcomes after 2 years in the early detection and intervention for the prevention of psychosis multisite effectiveness trial. Schizophr Bull. 2015;41:30–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Markulev C, McGorry PD, Nelson B, et al. . NEURAPRO-E study protocol: a multicentre randomized controlled trial of omega-3 fatty acids and cognitive-behavioural case management for patients at ultra high risk of schizophrenia and other psychotic disorders. Early Interv Psychiatry. 2017;11:418–428. [DOI] [PubMed] [Google Scholar]
- 35. Bachman P, Niendam TA, Jalbrzikowski M, et al. . Processing speed and neurodevelopment in adolescent-onset psychosis: cognitive slowing predicts social function. J Abnorm Child Psychol. 2012;40:645–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fowler D, Hodgekins J, French P, et al. . Social recovery therapy in combination with early intervention services for enhancement of social recovery in patients with first-episode psychosis (SUPEREDEN3): a single-blind, randomised controlled trial. Lancet Psychiatry. 2018;5:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Piskulic D, Addington J, Auther A, Cornblatt BA. Using the global functioning social and role scales in a first-episode sample. Early Interv Psychiatry. 2011;5:219–223. [DOI] [PubMed] [Google Scholar]
- 38. Nahum M, Fisher M, Loewy R, et al. . A novel, online social cognitive training program for young adults with schizophrenia: a pilot study. Schizophr Res Cogn. 2014;1:e11–e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Woodberry KA, Serur RA, Hallinan SB, et al. . Frequency and pattern of childhood symptom onset reported by first episode schizophrenia and clinical high risk youth. Schizophr Res. 2014;158:45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nelson B, Amminger GP, Yuen HP, et al. . Staged Treatment in Early Psychosis: a sequential multiple assignment randomised trial of interventions for ultra high risk of psychosis patients. Early Interv Psychiatry. 2018;12:292–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fisher M, Loewy R, Carter C, et al. . Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia. Schizophr Bull. 2015;41:250–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Glenthøj LB, Fagerlund B, Randers L, et al. . The FOCUS trial: cognitive remediation plus standard treatment versus standard treatment for patients at ultra-high risk for psychosis: study protocol for a randomised controlled trial. Trials. 2015;16:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hides L, Kavanagh DJ, Daglish M, et al. . The Quik Fix study: a randomised controlled trial of brief interventions for young people with alcohol-related injuries and illnesses accessing emergency department and crisis support care. BMC Emerg Med. 2014;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Landa Y, Mueser KT, Wyka KE, et al. . Development of a group and family-based cognitive behavioural therapy program for youth at risk for psychosis. Early Interv Psychiatry. 2016;10:511–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Loewy R, Fisher M, Schlosser DA, et al. . Intensive auditory cognitive training improves verbal memory in adolescents and young adults at clinical high risk for psychosis. Schizophr Bull. 2016;42(Suppl 1):S118–S126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. McAusland L, Addington J. Biofeedback to treat anxiety in young people at clinical high risk for developing psychosis. Early Interv Psychiatry. 2018;12:694–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Miklowitz DJ, O’Brien MP, Schlosser DA, et al. . Family-focused treatment for adolescents and young adults at high risk for psychosis: results of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53:848–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schlosser DA, Miklowitz DJ, O’Brien MP, De Silva SD, Zinberg JL, Cannon TD. A randomized trial of family focused treatment for adolescents and young adults at risk for psychosis: study rationale, design and methods. Early Interv Psychiatry. 2012;6:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shashi V, Harrell W, Eack S, et al. . Social cognitive training in adolescents with chromosome 22q11.2 deletion syndrome: feasibility and preliminary effects of the intervention. J Intellect Disabil Res. 2015;59:902–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Uher R, Cumby J, MacKenzie LE, et al. . A familial risk enriched cohort as a platform for testing early interventions to prevent severe mental illness. BMC Psychiatry. 2014;14:344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lo Cascio N, Curto M, Pasqualetti P, et al. . Impairment in social functioning differentiates youth meeting ultra-high risk for psychosis criteria from other mental health help-seekers: a validation of the Italian version of the global functioning: social and global functioning: role scales. Psychiatry Res. 2017;253:296–302. [DOI] [PubMed] [Google Scholar]
- 52. Lee SJ, Kim KR, Lee SY, An SK. Impaired social and role function in ultra-high risk for psychosis and first-episode schizophrenia: its relations with negative symptoms. Psychiatry Investig. 2017;14:539–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Carrión RE, Correll CU, Auther AM, Cornblatt BA. A severity-based clinical staging model for the psychosis prodrome: longitudinal findings from the New York recognition and prevention program. Schizophr Bull. 2017;43:64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. First M, Spitzer R, Gibbon M, Williams JB.. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, NY: New York State Psychiatric Institute. Biometrics Research; 1995. [Google Scholar]
- 55. Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry Suppl. 1993(22):39–44. [PubMed] [Google Scholar]
- 56. Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res. 1992;6:201–208. [DOI] [PubMed] [Google Scholar]
- 57. Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res. 1990;3:247–251. [DOI] [PubMed] [Google Scholar]
- 58. Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8:470–484. [DOI] [PubMed] [Google Scholar]
- 59. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. [DOI] [PubMed] [Google Scholar]
- 60. Streiner DL, Norman GR, Cairney J.. Health Measurement Scales: A Practical Guide to Their Development and Use. New York, NY: Oxford University Press; 2015. [Google Scholar]
- 61. Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61:310–317. [DOI] [PubMed] [Google Scholar]
- 62. Mallinckrodt CH, Clark WS, David SR. Accounting for dropout bias using mixed-effects models. J Biopharm Stat. 2001;11:9–21. [DOI] [PubMed] [Google Scholar]
- 63. McCulloch CE, Searle SR. Generalized, linear, and mixed models. Technometrics. 2001;45:99. [Google Scholar]
- 64. Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. Springer Ser Stat. 2000;xxii:56. [Google Scholar]
- 65. Carrión RE, Cornblatt BA, Burton CZ, et al. . Personalized prediction of psychosis: external validation of the NAPLS-2 psychosis risk calculator with the EDIPPP project. Am J Psychiatry. 2016;173:989–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. McLaughlin D, Carrión RE, Auther AM, et al. . Functional capacity assessed by the map task in individuals at clinical high-risk for psychosis. Schizophr Bull. 2016;42:1234–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Addington J, Cornblatt BA, Cadenhead KS, et al. . At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011;168:800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Schlosser DA, Jacobson S, Chen Q, et al. . Recovery from an at-risk state: clinical and functional outcomes of putatively prodromal youth who do not develop psychosis. Schizophr Bull. 2012;38:1225–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Cornblatt BA, Carrión RE, Addington J, et al. . Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38:1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Meyer EC, Carrión RE, Cornblatt BA, et al. ; NAPLS group The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr Bull. 2014;40:1452–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Francesconi M, Minichino A, Carrión RE, et al. . Psychosis prediction in secondary mental health services. A broad, comprehensive approach to the “at risk mental state” syndrome. Eur Psychiatry. 2017;40:96–104. [DOI] [PubMed] [Google Scholar]
- 72. Minichino A, Francesconi M, Carrión RE, et al. . Prediction of functional outcome in young patients with a recent-onset psychiatric disorder: beyond the traditional diagnostic classification system. Schizophr Res. 2017;185:114–121. [DOI] [PubMed] [Google Scholar]
- 73. Addington J, Liu L, Perkins DO, Carrion RE, Keefe RS, Woods SW. The role of cognition and social functioning as predictors in the transition to psychosis for youth with attenuated psychotic symptoms. Schizophr Bull. 2017;43:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cornblatt BA, Carrion RE, Auther A, et al. . Psychosis prevention: a modified clinical high risk perspective from the Recognition and Prevention (RAP) Program. Am J Psychiatry. 2015;172:986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Häfner H, Maurer K, an der Heiden W. ABC Schizophrenia study: an overview of results since 1996. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1021–1031. [DOI] [PubMed] [Google Scholar]
- 76. Häfner H, Maurer K, Löffler W, et al. . Modeling the early course of schizophrenia. Schizophr Bull. 2003;29:325–340. [DOI] [PubMed] [Google Scholar]
- 77. Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. 2008;99:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Nieman DH, Ruhrmann S, Dragt S, et al. . Psychosis prediction: stratification of risk estimation with information-processing and premorbid functioning variables. Schizophr Bull. 2014;40:1482–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Alderman T, Addington J, Bearden C, et al. . Negative symptoms and impaired social functioning predict later psychosis in Latino youth at clinical high risk in the North American prodromal longitudinal studies consortium. Early Interv Psychiatry. 2015;9:467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Harvey PD, Helldin L, Bowie CR, et al. . Performance-based measurement of functional disability in schizophrenia: a cross-national study in the United States and Sweden. Am J Psychiatry. 2009;166:821–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.