Abstract
Background
Motivational interviewing, as a counseling approach, could promote not only behavioral changes but also individuals' psychological adaptation. Previous studies provide evidence that motivational interviewing focused on increasing physical activity decreases the risk of metabolic syndrome in women. Its effects on sedentary behaviors, depressive symptoms, and health-related quality of life (HRQL) remain unknown.
Objectives
The aim of this study was to evaluate whether a 12-week motivational counseling program reduces sedentary behaviors and depressive symptoms and improves HRQL in Taiwanese women.
Methods
A randomized controlled study was conducted. Participants (n = 115) were randomly assigned into 3 groups: experimental group (received a brochure on lifestyle modification combined with 12 weeks of motivational counseling), comparison group (received a lifestyle modification brochure), and usual care group (UCG). Outcome variables were measured at baseline and at 12 weeks post intervention by the International Physical Activity Questionnaire, Beck Depression Inventory, and Medical Outcomes Short Form-36 Health Survey. Generalized estimating equations were applied to analyze the intervention effects of groups by interaction of group and time.
Results
Women in the experimental group not only reduced (P < .001) weekly sitting time by 374 minutes but also decreased (P < .05) depressive symptoms, as well as had greater overall HRQL including 8 subscales as compared with the UCG. As compared with the UCG, the women in the comparison group had no change in sedentary behaviors, but they had reduced depressive symptoms and improvement on some HRQL subscales.
Conclusions
Motivational counseling that incorporates behavioral change principles is effective in reducing sedentary behaviors and depressive symptoms and improving HRQL for women with metabolic syndrome.
KEY WORDS: depression, health-related quality of life, motivational interviewing, sedentary behavior, women
There is substantial evidence to support the high prevalence of metabolic syndrome (MetS) and its associated health consequences (ie, diabetes, cardiovascular disease, mortality from coronary heart disease).1–3 Despite proposed effective treatment modalities to reverse the trajectory of MetS,4,5 people with MetS continue to experience negative mood state (ie, depressive symptoms) and poor health-related quality of life (HRQL).6,7 Therefore, it is important to implement strategies that improve psychological health and HRQL for this population.
Active lifestyles contribute to better HRQL and less depressive symptoms.8–10 Unfortunately, most people with MetS, particularly middle-aged and older women, do not consistently adhere to the recommended guidelines for modifying their lifestyles and tend to maintain sedentary lifestyles.11–13 There is limited research on whether strategies focused on decreasing sedentary behaviors and depressive symptoms and improving HRQL are effective in adults with MetS. In a previous report of an individualized, 12-week, behavior-based motivational interviewing program, we described the effectiveness of this intervention on increasing physical activity and reducing metabolic risks in middle-aged and older Taiwanese women.14 However, because physical activity is not synonymous with sedentary behavior, in this study, we tested the effects of the motivational interviewing intervention on sedentary behaviors. At the same time, we further examined the impact of the intervention on depressive symptoms and HRQL in this population with MetS.
People with MetS are at an increased risk for having depression;15 middle-aged people with MetS who at baseline are not depressed are twice as likely at 7-year follow-up to report depression.16 Among middle-aged women, depressive symptoms can predict MetS.15,17 This suggests that the relationship between MetS and depression is bidirectional.
People with MetS who have multiple cardiovascular risk factors carry an increased physical and psychological burden, leading to impaired HRQL.6,18 The US National Health and Nutrition Examination Survey indicated that adults with MetS experience worse HRQL than those without MetS after adjusting for sociodemographic covariates and smoking status.7 Although the reason is unknown, women have lower HRQL as compared with men.19–21 Bingefors and Isacson19 found that one possible contributing factor is that women have a higher prevalence of somatic pain and pain-related conditions. This may account for the lower HRQL reported by women.18,20,21 Because of the multiple family and social roles of women in Taiwan,13 middle-aged and older women with MetS may experience further reductions in psychological health and HRQL.
The development of MetS is multifactorial. Genetics and lifestyle factors are clear contributors.22 A sedentary lifestyle is considered a risk factor for cardiovascular morbidity and mortality, after adjusting for performance of moderate and vigorous physical activity.23,24 A sedentary lifestyle is defined as more hours of behaviors such as lying down, sitting, watching television, and using the computer and other forms of screen-based entertainment than hours of physical activity including exercise during waking hours.25 Sedentary behaviors can be quantified as “sitting time” and can be measured using objective and subjective approaches, such as accelerometers and questionnaires.26 Evidence is accumulating about the relationship between sedentary behaviors and health outcomes.27–30 In a study of Swedish middle-aged women, Frisman and Kristenson18 found that the observed association between MetS and HRQL was lost after adjustment for lifestyles (level of physical activity). Reducing sedentary behaviors or promoting physical activity level for middle-aged and older women with MetS may increase HRQL.8–10,30
Although programs to promote active lifestyles have become popular in primary care settings, low adherence has been reported,31 particularly among women.32 Motivational interviewing as a counseling approach, first proposed by Miller,33 has been widely applied as an effective method in promoting behavior changes such as smoking cessation, problem drinking, diabetes management, and engagement of active lifestyles.34–36 Motivational counseling places emphasis on encouraging people to consider their current behaviors and to explore them in relation to their values, interests, aspirations, and self-efficacy.37 On the basis of a systematic review of 72 randomized controlled trials in patients with obesity/diabetes/asthma/mental illness, individuals with alcohol abuse/drug addiction, or those who smoke, motivational counseling was found to have a significant and clinically relevant effect on both physical and psychological health.38 When applying motivational counseling in brief encounters of 15 minutes, more than half of the studies (64%) showed a positive effect, and more than 1 individualized encounter with the patients confirmed the effectiveness of motivational counseling.38 In studies that included an estimated median follow-up period of 12 months (range, 2 months to 4 years), the positive benefits of motivational counseling persisted.38 We previously described that a motivational interviewing program aimed at lifestyle modification had positive benefits, namely, increased physical activity and reduced the percentage of middle-aged and older women in the sample who met the criteria for MetS.14 Women with MetS increased their physical activity amount by 283 MET-min/wk after the 12-week program.
An increase in physical activity does not necessarily equate to a reduction in sedentary behaviors. As shown by Grontved and Hu23 (2011) and Ford and Caspersen24 (2012), a reduction in sedentary behavior has positive health benefits, such as decreases in cardiometabolic morbidity and mortality, after adjustment for physical activity. Yet, evidence is limited that examines the effectiveness of motivational counseling on reduction of sedentary behaviors and depressive symptoms and improvement of HRQL among middle-aged and older women with MetS after controlling for physical activity.
Using our previously described cohort, we examined the effectiveness of a 12-week, individually tailored, motivational counseling–based lifestyle modification intervention on sedentary behaviors, depressive symptoms, and HRQL, compared with a single brief lifestyle modification counseling session plus an educational brochure, and usual care for middle-aged and older women with MetS after adjusting for physical activity.
Method
Study Design
A randomized controlled trial with a 3 parallel intervention group design was conducted in northern Taiwanese women to compare the differences in effectiveness on weekly sitting time, depressive symptoms, and HRQL among experimental group (EG), comparison group (CG), and usual care group (UCG) participants. Eligible women were randomly assigned to 3 parallel groups: (1) EG, received a brochure on lifestyle modification, combined with individual 12-week motivational counseling; (2) CG, received only the lifestyle modification brochure; and (3) UCG, received usual care with regular outpatient follow-up. Sealed, opaque envelopes were used, following computer-generated random serial numbers. Sedentary behaviors (ie, weekly sitting time), depressive symptoms, and HRQL were compared among the 3 groups at baseline and after 12 weeks.
Participants and Setting
A purposive sample of urban-dwelling middle-aged and older women (older than 40 years) in northern Taiwan was recruited from an urban community health center. Those potentially eligible women who agreed to participate and gave their informed consent were then referred to an endocrinology/metabolism physician at the local medical center for screening for eligibility before randomization. Inclusion criteria were able to speak and understand Mandarin; without a history of cancer, end-stage renal disease with dialysis, or confirmed psychiatric diseases; and able to walk without assistance. Of those initially approached (N = 328), 115 eligible women with confirmed MetS were randomly assigned: 38 (33%) to the EG, 38 (33%) to the CG, and 39 (34%) to the UCG. MetS is defined as having 3 or more of the following 5 risk factors for women according to the National Cholesterol Education Program Adult Treatment Panel III: (1) elevated fasting plasma glucose of 100 mg/dL or use of antidiabetic medicines, (2) elevated blood pressure of 130/85 mm Hg or higher or use of antihypertensive medicines, (3) elevated triglyceride level of 150 mg/dL or higher, (4) reduced high-density lipoprotein cholesterol level less than 50 mg/dL, and (5) central obesity, with a waist circumference of 80 cm or greater.39 Exclusion criteria included not meeting the criteria for MetS, declining to participate, and having a history of cancer, confirmed psychiatric disease, and moderate to severe physical disability. All eligible participants, approached consecutively for 4 months, were given thorough information about participation, and written informed consent was obtained before final inclusion. The 12-week follow-up assessments were conducted by a research nurse blinded to group assignment. Ethical approval (reference number: 1-101-05-073) was obtained from the institutional review board of the local medical center.
Sample size estimation was based on a previous study with a medium-to-small effect size.40 With an α of .05 and a power of 0.8, each group required at least 34 participants.41
Study Intervention
Among the EG, participants were given individually tailored, 12-week, telephone-based motivational counseling for modifying lifestyles that focused on decreasing sedentary activities including sitting, watching television, and using mobile devices, computers, or other forms of screen-based entertainment and increasing the frequencies of breaks in those sedentary behaviors, except for physical activity promotion.14 In addition, the EG also received an educational brochure about lifestyle modification and stress coping. The CG received the educational material similar to the EG, whereas the UCG only underwent routine outpatient clinical follow-up. The intervention consisted of individualized promotion of active physical activity behaviors and enhancement of self-efficacy32,42 based on the principles of motivational interviewing and aimed to reduce participants' sedentary behaviors. The telephone-based motivational counseling was delivered by an experienced nurse in a medical center at Taipei city in northern Taiwan, details of which were previously reported.14
Measures
Sedentary Behaviors
Sedentary behaviors can be referred to as “sitting time.”25 The sedentary behaviors in this study presented as weekly sitting time (minutes per week)26 were assessed for the past 7 days at pre and post 12-week intervention by the International Physical Activity Questionnaire-Short Form, which has well-established reliability and validity.43 Participants with more weekly sitting time had more sedentary behaviors.
Depressive Symptoms
The Beck Depression Inventory, with good reported reliability and validity in various populations,44,45 was used to measure depressive symptoms. This 21-item scale, scored from 0 to 63, comprising emotional, cognitive, and somatic categories, measured participants' depressive symptoms.46 Higher scores on the Beck Depression Inventory represented more depressive symptoms. The total scores were used to screen depressive symptoms: none to minimal (0–9) and mild to severe (10–63).
Health-Related Quality of Life
Health-related quality of life was assessed by the well-validated and reliable Medical Outcomes Short Form-36 Health Survey, a widely used scale, with scores ranging from 0 to 100, composed of 36 self-administered items and 8 subscales: physical function, role function limits due to physical problem (role-physical), role function limits due to emotional problem (role-emotional), social functioning, bodily pain, vitality, mental health, and general health.47,48 Higher scores reflect higher HRQL.
Data Analysis
Data were collected at baseline and after the 12-week intervention. Analysis of variance and χ2 test were used to compare the background variables including sociodemographic characteristics, lifestyle covariates (ie, alcohol consumption, smoking status, weekly amounts of physical activity, and dietary patterns presented as habit of weekly breakfast and late-night snack), and preintervention and postintervention. The intervention effects were evaluated after adjusting for sociodemographic characteristics and lifestyle covariates by generalized estimating equations. Differences of interventional effect between groups were analyzed and presented via the interaction variables (group × time).
Results
Baseline Characteristics
Of the 115 randomized participants, 100 (87%) completed the study: 34 in the EG, 32 in the CG, and 34 in the UCG. During the study, 1 participant withdrew and 14 were lost to follow-up at the 12-week assessment. An intention-to-treat analysis was used. A flow diagram with this sample was previously published.14 The participants' sociodemographic characteristics (age, educational level, married status, employment, menopausal status) and lifestyle patterns (alcohol consumption, smoking status, physical activity, dietary patterns) were similar in the 3 groups, as shown in previous study.14
Outcome Evaluation
Table 1 shows the weekly sitting time, depressive symptoms, and HRQL of the 3 groups at baseline and at 12 weeks. The mean differences between baseline and 12 weeks within the EG, CG, and UCG were significantly (P < .001) different for weekly sitting time, depressive symptoms, HRQL, and all of the 8 HRQL subscales. Weekly sitting time decreased in the EG, whereas it increased in the UCG and remained unchanged in the CG. Participants in the EG had reduced depressive symptoms and improved HRQL at 12 weeks, whereas those in the UCG had more depressive symptoms and worse HRQL.
TABLE 1.
Comparison of Weekly Sitting Time, Depressive Symptoms, and Health-Related Quality of Life Between Baseline and 12-Week Follow-up
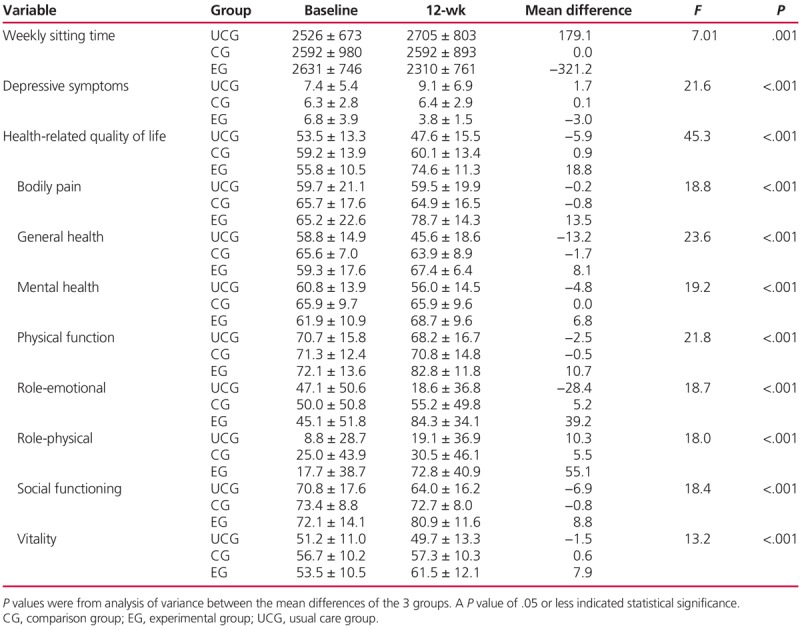
Table 2 shows the generalized estimating equation analyses and adjustment for sociodemographic characteristics and lifestyle covariates for the effectiveness of the motivational interviewing on weekly sitting time, depression, and HRQL. The significant group × time interaction for weekly sitting time revealed that women in the EG had a greater decrease in weekly sitting time at 12 weeks than did those in the UCG (ß = −374, P < .001) and CG (ß = −272, P = .013); however, there was no difference between women in the CG and UCG. Women in the EG and CG had less depressive symptoms compared with those in the UCG at 12 weeks (ß = −4.21, P < .001, and ß = −1.36, P = .037, respectively). Women in the EG also had less depressive symptoms compared with those in the CG (ß = −2.8, P < .001).
TABLE 2.
Evaluation of the Intervention's Effectiveness on Weekly Sitting Time, Depressive Symptoms, and Health-Related Quality of Life Based on Generalized Estimating Equation Analysis
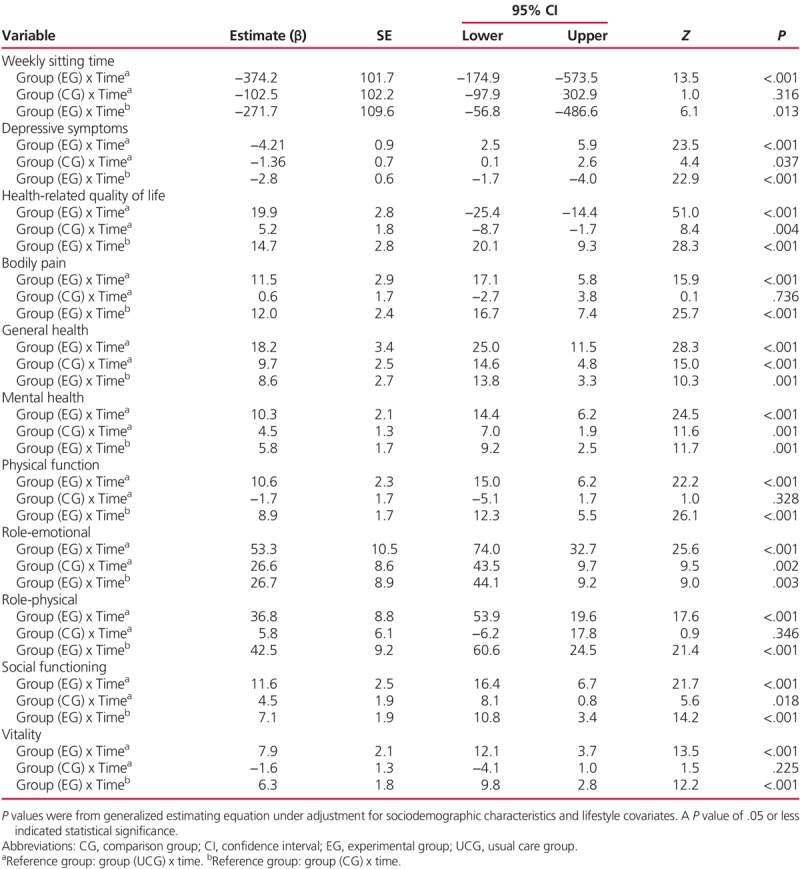
Women in the EG had a greater increase in mean HRQL scores (ß = 19.9, P < .001) and all 8 subscales than did those in the UCG. However, women in the CG improved only in the HRQL mean scores, general health, mental health, role-emotional, and social function, as compared with the UCG. As compared with women in the CG, those in the EG also had a greater increase in mean scores of the HRQL (ß = 14.7, P < .001) and all 8 subscales at 12 weeks.
Discussion
A tailored lifestyle modification intervention based on a motivational interviewing strategy had significant beneficial effects on reduction of weekly sitting time and depressive symptoms, and improved HRQL scores for middle-aged and older Taiwanese women with MetS after controlling for changes in physical activity. Our intervention facilitated successful health promotion for this population of Taiwanese middle-aged and older women from an urban community.
Our study results reveal that overall weekly sitting time was reduced by 12.2% in the EG as compared with the UCG. Women in the CG also had reduced weekly sitting time; however, this difference did not reach significance when compared with those in the UCG. We found a greater reduction (12.2%) in sitting time as compared with a previous study (2.9%) conducted with 166 sedentary community-dwelling Danish adults that used 4 individual theory-based motivational interviewing sessions without physical activity promotion included.49 Several demographic characteristics may account for the differences between samples. Our sample was older (63.1 vs 52.2 years), and Taiwanese, and had a lower percentage of employment (9% vs 60%) and perhaps more leisure time, increased baseline weekly sitting time (2631.0 vs 2229.6 min/wk), and a decreased follow-up period (3 vs 6 months) assessment.49
Several authors of recent intervention studies have tested strategies to reduce sedentary behaviors.49–51 None of them used a randomized controlled trial approach. On average, they found a 2.9% to 4.3% reduction of objectively (ie, accelerometer-derived, activPAL, ActiGraphy) measured sitting time among older adults or adults who are overweight/obese.49–51 Authors of other studies only used 1 face-to-face counseling session50,51 or 4 individual theory-based counseling sessions with at least 30 minutes per session,49 with either a 7-day50,51 or 6-month follow-up.49 We postulate that a 12-week, nurse-led, individually tailored motivational counseling program with a weekly telephone call for 15 to 30 minutes has a greater impact on reducing sitting time.
In our study, we used a self-reported questionnaire (International Physical Activity Questionnaire-Short Form), to assess participants' sitting times instead of an objective accelerometer-based device as applied in the study by Aadahl et al49 (2014). Although there is potential for subjective bias, we selected the International Physical Activity Questionnaire-Short Form because it can be used for global comparisons across different geographic populations.12 In addition, our subjective assessment was found to have similar results with the objective measures of a triaxial accelerometer-based device among adults with 63% women aged 52.2 years in the previous study by Aadahl et al.49 Self-report of sedentary behaviors might serve as an easier and simpler instrument for evaluating participants' sedentary behaviors in a clinic population.
In the current study of middle-aged and older Taiwanese women with MetS, the intervention improved depression and HRQL scores. It may be that effectively tailored approaches are better remembered and perceived as more credible compared with nontailored communication.52 Granger et al9 (2011) found that enhanced counseling increases participants' confidence and self-efficacy in their self-care, resulting in less depressive symptoms, better health status, and an overall HRQL.
Although the CG did not change their sedentary behaviors, they did report improvements in depressive symptoms and some domains of HRQL, as compared with the UCG. As such, the brief lifestyle counseling with educational material does seem to have beneficial effects on depressive symptoms and HRQL in women with MetS. This is consistent with the findings of Marshall et al53 in their study among Australian adults. However, significant differences in depressive symptoms and HRQL between the CG and the UCG may be because women in the CG had similar scores in depressive symptoms and HRQL between baseline and 12 weeks. This suggests that brief lifestyle counseling with educational material may stabilize psychological health and HRQL in Taiwanese women with MetS. Whether these effects would have persisted remains unknown.
The low-cost, generalizable intervention in the CG can be a practical and population-based health promotion strategy, as compared with the multisession EG intervention. However, more intensive coaching with weekly follow-up, particularly via technology (ie, mobile apps, internet-delivered approaches), might still be recommended, because only the women in the EG increased physical activity14 and reduced their sedentary behaviors. Thus, when adding telephone reminders based on motivational interviewing, this individual intensive strategy may ensure its effectiveness on active lifestyles, and depressive symptoms and HRQL, as it did in our study population.10 A larger study of community-based clinics is needed to support the implementation of such an intervention.
Whether the improvement of depressive symptoms and HRQL is because of the reduction of sedentary behaviors, we cannot make this conclusion using our study results. However, to deepen the understanding of the role of sedentary behaviors in this hypothesis, we have used Pearson correlation analysis to evaluate the relationships between sedentary behavior (weekly sitting time), depressive symptoms, and HRQL, and found that weekly sitting time did positively correlate with depressive symptoms and negatively associated with HRQL. Therefore, we postulate that reducing weekly sitting time may lead to reduced depressive symptoms and improved HRQL. Further research testing whether reducing sedentary behaviors is a mediator of interventions that result in improvement of depressive symptoms and HRQL is required.
Generalizability of our findings is limited because of (1) a short-term (12-week) follow-up, (2) a selection bias caused by a lack of randomization in the selection of participants, and (3) a sample only from a single geographical region of Taiwan. However, strengths exist in this study, including a random allocation and a relatively low dropout rate (13%). Furthermore, multiple comparisons with 3 groups, as used in this study, provide considerations for future designs of health promotion interventions and strategies to increase patients' adherence to lifestyle behavioral changes. In the future, more rigorous sampling strategies with larger samples from multiple sites are recommended. Further studies are suggested to investigate the long-term effect of adherence to active lifestyles and psychological health as well as HRQL among middle-aged and older women with MetS. Important mediators such as self-efficacy and family or peer support that may influence women's participation in active lifestyles and contribute to improved psychological health and HRQL should be identified. In addition, the testing of this intervention with other geographically diverse groups is suggested for future study.
Conclusion
A 12-week motivational counseling strategy, incorporating lifestyle modification, is effective for behavioral changes to reduce sedentary behaviors and improve depressive symptoms as well as HRQL for middle-aged and older Taiwanese women with MetS. It could be an effective model for community-based approaches to promote health among middle-aged and older women with other chronic health conditions including obesity, type 2 diabetes, and cardiovascular disease. Future studies are required to examine the effects of this intervention among other geographically diverse groups and patients with different chronic conditions.
What's New and Important
Motivational counseling incorporated with behavioral change in lifestyle modification programs can be an effective model to significantly reduce weekly sitting time for middle-aged and older women with MetS.
Individualized, telephone-based, motivational counseling to reduce sedentary behaviors is effective for improving depression and HRQL among middle-aged and older women with MetS.
Acknowledgment
We thank all of the participating women in this study funded by the Tri-Service General Hospital (TSGH-C102-138) and the Ministry of Science and Technology (MOST107-2314-B016-068), Taipei, Taiwan.
Footnotes
L.-C.C. and S.-L.C. contributed equally to the study.
The authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28:629–636. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005;28:1769–1778. [DOI] [PubMed] [Google Scholar]
- 3.Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. [DOI] [PubMed] [Google Scholar]
- 4.Steckhan N, Hohmann CD, Kessler C, et al. Effects of different dietary approaches on inflammatory markers in patients with metabolic syndrome: a systematic review and meta-analysis. Nutrition. 2016;32:338–348. [DOI] [PubMed] [Google Scholar]
- 5.Lemes IR, Turi-Lynch BC, Cavero-Redondo I, et al. Aerobic training reduces blood pressure and waist circumference and increases HDL-c in metabolic syndrome: a systematic review and meta-analysis of randomized controlled trials. J Am Soc Hypertens. 2018;12:580–588. [DOI] [PubMed] [Google Scholar]
- 6.Corica F, Corsonello A, Apolone G, et al. Metabolic syndrome, psychological status and quality of life in obesity: the QUOVADIS Study. Int J Obes (Lond). 2008;32(1):185–191. [DOI] [PubMed] [Google Scholar]
- 7.Ford ES, Li C. Metabolic syndrome and health-related quality of life among U.S. adults. Ann Epidemiol. 2008;18:165–171. [DOI] [PubMed] [Google Scholar]
- 8.Martin CK, Church TS, Thompson AM, et al. Exercise dose and quality of life: a randomized controlled trial. Arch Intern Med. 2009;169:269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Granger CL, McDonald CF, Berney S, Chao C, Denehy L. Exercise intervention to improve exercise capacity and health related quality of life for patients with non-small cell lung cancer: a systematic review. Lung Cancer. 2011;72(2):139–153. [DOI] [PubMed] [Google Scholar]
- 10.Mammen G, Faulkner G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am J Prev Med. 2013;45:649–657. [DOI] [PubMed] [Google Scholar]
- 11.Lin CH, Chiang SL, Yates P, Tzeng WC, Lee MS, Chiang LC. Influence of socioeconomic status and perceived barriers on physical activity among Taiwanese middle-aged and older women. J Cardiovasc Nurs. 2017;32(4):321–330. [DOI] [PubMed] [Google Scholar]
- 12.Bauman A, Bull F, Chey T, et al. The International Prevalence Study on Physical Activity: results from 20 countries. Int J Behav Nutr Phys Act. 2009;6:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Im EO, Chang SJ, Ko Y, et al. A national internet survey on midlife women's attitudes toward physical activity. Nurs Res. 2012;61:342–352. [DOI] [PubMed] [Google Scholar]
- 14.Lin CH, Chiang SL, Heitkemper MM, et al. Effects of telephone-based motivational interviewing in lifestyle modification program on reducing metabolic risks in middle-aged and older women with metabolic syndrome: a randomized controlled trial. Int J Nurs Stud. 2016;60:12–23. [DOI] [PubMed] [Google Scholar]
- 15.Pan A, Keum N, Okereke OI, et al. Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koponen H, Jokelainen J, Keinänen-Kiukaanniemi S, et al. Metabolic syndrome predisposes to depressive symptoms: a population-based 7-year follow-up study. J Clin Psychiatry. 2008;69:178–182. [DOI] [PubMed] [Google Scholar]
- 17.Raikkonen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women: a comparison of World Health Organization, Adult Treatment Panel III, and International Diabetes Foundation definitions. Diabetes Care. 2007;30:872–877. [DOI] [PubMed] [Google Scholar]
- 18.Frisman GH, Kristenson M. Psychosocial status and health related quality of life in relation to the metabolic syndrome in a Swedish middle-aged population. Eur J Cardiovasc Nurs. 2009;8:207–215. [DOI] [PubMed] [Google Scholar]
- 19.Bingefors K, Isacson D. Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain—a gender perspective. Eur J Pain. 2004;8(5):435–450. [DOI] [PubMed] [Google Scholar]
- 20.Chedraui P, Hidalgo L, Chavez D, et al. Quality of life among postmenopausal Ecuadorian women participating in a metabolic syndrome screening program. Maturitas. 2007;56:45–53. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. [DOI] [PubMed] [Google Scholar]
- 22.Edwardson CL, Gorely T, Davies MJ, et al. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS One. 2012;7:e34916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305:2448–2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ford ES, Caspersen CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41:1338–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pate RR, O'Neill JR, Lobelo F. The evolving definition of "sedentary.". Exerc Sport Sci Rev. 2008;36:173–178. [DOI] [PubMed] [Google Scholar]
- 26.Craig CL, Marshall AL, Sjöström M, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. [DOI] [PubMed] [Google Scholar]
- 27.Ford ES, Kohl HW, 3rd, Mokdad AH, Ajani UA. Sedentary behavior, physical activity, and the metabolic syndrome among U.S. adults. Obesity. 2005;13(3):608–614. [DOI] [PubMed] [Google Scholar]
- 28.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369–371. [DOI] [PubMed] [Google Scholar]
- 29.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–132. [DOI] [PubMed] [Google Scholar]
- 30.Wu XY, Han LH, Zhang JH, et al. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: a systematic review. PLoS One. 2017;12:e0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Conn VS, Minor MA, Burks KJ, et al. Integrative review of physical activity intervention research with aging adults. J Am Geriatr Soc. 2003;51:1159–1168. [DOI] [PubMed] [Google Scholar]
- 32.Pavey T, Taylor A, Hillsdon M, et al. Levels and predictors of exercise referral scheme uptake and adherence: a systematic review. J Epidemiol Community Health. 2012;66:737–744. [DOI] [PubMed] [Google Scholar]
- 33.Miller W. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:26. [Google Scholar]
- 34.Lindson-Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2015; (3):CD006936. [DOI] [PubMed] [Google Scholar]
- 35.Phillips AS, Guarnaccia CA. Self-determination theory and motivational interviewing interventions for type 2 diabetes prevention and treatment: a systematic review. J Health Psychol. 2017. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 36.Appiah-Brempong E, Okyere P, Owusu-Addo E, et al. Motivational interviewing interventions and alcohol abuse among college students: a systematic review. Am J Health Promot. 2014;29:e32–e42. [DOI] [PubMed] [Google Scholar]
- 37.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: Guilford Press; 2012. [Google Scholar]
- 38.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- 39.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement: executive summary. Crit Pathw Cardiol. 2005;4(4):198–203. [DOI] [PubMed] [Google Scholar]
- 40.Lin CH, Chiang SL, Yates P, et al. Moderate physical activity level as a protective factor against metabolic syndrome in middle-aged and older women. J Clin Nurs. 2015;24(9-10):1234–1245. [DOI] [PubMed] [Google Scholar]
- 41.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 42.Da Costa D, Ireland K. Perceived benefits and barriers to leisure-time physical activity during pregnancy in previously inactive and active women. Women Health. 2013;53:185–202. [DOI] [PubMed] [Google Scholar]
- 43.Liou YM, Jwo CJ, Yao KG, Chiang LC, Huang LH. Selection of appropriate Chinese terms to represent intensity and types of physical activity terms for use in the Taiwan version of IPAQ. J Nurs Res. 2008;16(4):252–263. [DOI] [PubMed] [Google Scholar]
- 44.Tsay S-L, Healstead M. Self-care self-efficacy, depression, and quality of life among patients receiving hemodialysis in Taiwan. Int J Nurs Stud. 2002;39:245–251. [DOI] [PubMed] [Google Scholar]
- 45.Pulkki-Råback L, Elovainio M, Kivimäki M, et al. Depressive symptoms and the metabolic syndrome in childhood and adulthood: a prospective cohort study. Health Psychol. 2009;28:108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beck AT, Steer RA, Carbin MG. Psychometric properties of Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 47.Fuh J-L, Wang S-J, Lu S-R, et al. Psychometric evaluation of a Chinese (Taiwanese) version of the SF-36 health survey amongst middle-aged women from a rural community. Qual Life Res. 2000;9:675–683. [DOI] [PubMed] [Google Scholar]
- 48.Ware JE, Kosinski M. SF-36 Physical & Mental Health Summary Scales: A Manual for Users of Version 1. 2nd Ed. Lincoln, RI: QualityMetric Inc; 2012. [Google Scholar]
- 49.Aadahl M, Linneberg A, Moller TC, et al. Motivational counseling to reduce sitting time: a community-based randomized controlled trial in adults. Am J Prev Med. 2014;47:576–586. [DOI] [PubMed] [Google Scholar]
- 50.Gardiner PA, Eakin EG, Healy GN, et al. Feasibility of reducing older adults' sedentary time. Am J Prev Med. 2011;41:174–177. [DOI] [PubMed] [Google Scholar]
- 51.Kozey-Keadle S, Libertine A, Staudenmayer J, Freedson P. The feasibility of reducing and measuring sedentary time among overweight, non-exercising office workers. J Obes. 2012;2012:282–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford Press; 2002. [Google Scholar]
- 53.Marshall AL, Bauman AE, Owen N, et al. Population-based randomized controlled trial of a stage-targeted physical activity intervention. Ann Behav Med. 2003;25:194–202. [DOI] [PubMed] [Google Scholar]


