Abstract
Objective
To analyze the complex relationship between various social indicators that contribute to socioeconomic status and healthcare barriers.
Design
Cluster analysis of historical patient data obtained from inpatient visits.
Setting
Inpatient rehabilitation unit in a large, urban university hospital.
Participants
Adult patients receiving acute inpatient care, predominantly for closed head injury.
Interventions
Not applicable
Main outcome measures
We examined the membership of TBI patients in various “vulnerable group” (VG) clusters (e.g., homeless, unemployed, racial/ethnic minority) and characterized the rehabilitation outcomes of the patients (e.g., duration of stay, changes in Functional Independence Measure [FIM] scores between admission to inpatient stay and discharge).
Results
Analysis revealed four major clusters (i.e., Clusters A-D) separated by VG memberships, with distinct durations of stay and FIM gains during their stay. Cluster B, the largest cluster and also consisting of mostly racial/ethnic minorities, had the shortest duration of hospital stay and one of the lowest FIM improvements among the four clusters despite higher FIM scores at admission. In cluster C, also consisting of mostly ethnic minorities with multiple SES vulnerabilities, patients were characterized by low cognitive FIM scores at admission and the longest duration of stay, and they showed good improvement in FIM scores.
Conclusions
Application of clustering techniques to inpatient data identified distinct clusters of patients who may experience differences in their rehabilitation outcome due to their membership in various “at-risk” groups. Results identified patients (i.e., cluster B, with minority patients and Cluster D, with elderly patients) who attain below-average gains in brain injury rehabilitation. Results also suggested that systemic (e.g., duration of stay) or clinical service improvements (e.g., staff’s language skills, ability to offer substance abuse therapy, provide appropriate referrals or liaise with intensive social work services or plan subacute rehabilitation phase) could be beneficial for acute settings. Stronger recruitment, training and retention initiatives for bilingual and multiethnic professionals may also be considered to optimize gains from acute inpatient rehabilitation following traumatic brain injury.
Keywords: Rehabilitation, diversity, Inpatient care, Socio-economic status, at-risk and vulnerable groups, minorities
For brain-injury-related diagnoses, prevalence studies suggest increased risk for various non-White populations. Incidence of traumatic brain injury (TBI) is also higher in young adult males. A study of pediatric TBI patients demonstrated higher incidence of TBI in young African-American children under age five. Among health risk factors associated with stroke (e.g., obesity, hypertension, heart disease, cardiovascular disease), Mexican Americans and Black women had higher prevalence of obesity, while Blacks and Pacific Islanders were more likely to have hypertension1. Consequently, patients from racial/ethnic and linguistic minority backgrounds, hereafter referred to as “Minorities,” are likely to make up the majority population for rehabilitation facilities in inner cities.
Despite the prevalence of diverse populations within rehabilitation settings, there is a service gap (e.g. lower utilization or provision), as well as general unavailability of evidence-based assessment and treatment for Minorities2–5. For Minorities who overcome barriers to access health care, research still suggests disparities in quality6,7 (e.g., duration and intensity of care are lower for non-Whites). Minority patients are less likely to engage in successful community participation after injury and are more likely to be “lost to follow-up” compared to Whites8.
This brief report presents a cluster analysis of inpatient data to refine our understanding of health care barriers faced by Minorities. We analyze archival demographic and clinical data from an urban public hospital and examine co-occurring membership of TBI patients in various “vulnerable groups” (e.g., homeless, unemployed, linguistic/racial/ethnic minority), using statistically robust clusters obtained from patient-level data. We illustrate defining characteristics of each patient cluster and compare rehabilitation outcomes.
Methods
Data collection was approved by our medical center’s Institutional Review Board. We used patient-level data (N = 148) collected through retrospective chart review. Inclusion and exclusion criteria followed TBIMS National Database9 guidelines, available online. Binary information denoting membership in 11 vulnerable groups were used as the basis of cluster analysis: homelessness, past incarceration, undocumented status, elderly, minority status, non-English speaking, psychiatric history, history of mental institute stays, history of severe medical problems, substance abuse history, and other. A data-driven, two-step cluster approach with log-linear distances (capped at 8 clusters) was used10. K-means approach was adopted for the 4-cluster solution11. Fit of alternative solutions (e.g., furthest neighbor, 2–4 cluster solutions; resorted and dropped variables) were compared using Akaike Information Criterion obtained from the Two-Step Cluster outputs. Demographic and psychosocial information; length of hospital stay (acute only); FIM score change from admission to discharge were compared using appropriate parametric or nonparametric statistics. A data point indicating a length of stay greater than 5 months was excluded from relevant group-wise statistics with no effect on clustering analysis.
Results
Vulnerable group membership was defined along eleven categories, in line with our group’s past work in this domain12. Prevalence of vulnerabilities across these groups were as follows: substance abuse history (35.8%), psychiatric history (20.9%), medical history (19.6%), history of psychiatric institutionalization (8.8%), English as a second language (ESL)/non-English speaking (18.2%), racial/ethnic minority (58.1%), elderly (27%), undocumented status (8.8%), history of incarceration (12.2%), history of homelessness (17.6%) and other vulnerabilities (2.7%). Two of the four patients in the “other” vulnerability group sustained injuries from being assaulted with a blunt instrument; one was a homeless male with complex medical and psychiatric history admitted after a fall, the other was a non-English speaking young male admitted after a biking accident with unknown immigration status.
Clustering analysis revealed four main clusters that were stable across 2-step and k-means approaches. Final cluster sizes and characteristics (i.e., cluster centers) are provided in Table 1. Significant group differences were found for the 4-cluster solution (all p’s < .05) in all variables except for “other vulnerability.” Largest F-values were obtained for substance abuse history (F=76.71), medical history (F=45.73), elderly (F=38.25), psychiatric history (F = 33.12), homelessness (F = 27.09), and minority status (F = 18.82), where all p’s < .001. Given the small size of undocumented status and other vulnerability groups, we repeated the analysis with only nine vulnerability groups and still obtained a four cluster solution that highlights cluster differences in terms of minority group membership.
Table 1.
Cluster analysis results and outcomes by cluster
Above half shows cluster centers for each input variable that was used for the clustering analysis. Top defining variables for each cluster are shaded in dark gray. Bottom half shows the breakdown of rehabilitation outcomes for each cluster.
| Cluster Name
|
|||||
|---|---|---|---|---|---|
| A | B | C | D | ||
| INPUT variables | |||||
| ethnic/racial minority | .25 | .72 | .95 | .24 | |
| significant medical hx | .04 | .01 | .45 | .72 | |
| elderly | .07 | .17 | .10 | .92 | |
| homelessness hx | .29 | .05 | .70 | .00 | |
| substance abuse hx | .82 | .11 | 1.00 | .08 | |
| incarceration hx | .18 | .05 | .30 | .12 | |
| ESL/Non-English Sp | .07 | .21 | .40 | .04 | |
| institutionalization hx | .18 | .00 | .30 | .08 | |
| psychiatric hx | .71 | .03 | .10 | .28 | |
| undocumented | .00 | .12 | .20 | .00 | |
| other | .04 | .04 | .00 | .00 | |
|
| |||||
| ANALYSIS variables | |||||
| Duration of Stay (days)* | 21.39 | 15.95 | 27.00 | 18.24 | |
| FIM gains (Total) | 39.61 | 27.86 | 34.74 | 26.40 | |
| FIM gains (Cog)* | 10.9286 | 7.7571 | 9.3158 | 5.2400 | |
| FIM gains (Motor) | 28.6786 | 21.3784 | 25.4211 | 21.1600 | |
| Discharge Location (χ2 = 12.66, p = .049, n = 148) | |||||
| Home | 32.1% | 56.0% | 35.0% | 36.0% | |
| Acute / Subacute Care | 53.6% | 42.7% | 55.0% | 60.0% | |
| Other | 14.3% | 1.3% | 10.0% | 4.0% | |
| Primary person at d/c (χ2 = 8.10, p = .231, n = 148) | |||||
| Self / Alone / Other | 6.6% | 5.0% | 4.0% | ||
| Family / Friends | 32.1% | 49.3% | 30.0% | 32.0% | |
| Facility Care | 67.9% | 44.0% | 65.0% | 64.0% | |
indicates significant group differences between clusters based on omnibus ANOVAs, p < .05.
The clusters in the main analysis were characterized as follows: Cluster A – higher likelihood of problematic substance use and psychiatric history; Cluster B – racial and ethnic minority group membership and somewhat increased incidence of ESL; Cluster C – substance use, incarceration, homelessness history in predominantly minority and ESL group; Cluster D – elderly patients with complex medical comorbidities (see Figure 1 for relative incidences of membership in each cluster). Clusters B (n = 75) and C (n = 20), both defined by ethnic/minority membership, comprised more than half the sample (N = 148). Patients with psychiatric histories were more likely to be in Clusters A and C; those with significant medical histories were more likely to be in Clusters C and D. Age was significantly higher for Cluster D (M = 76), compared to the other clusters, where average age per cluster ranged from 43 to 49.
Figure 1. Clusters of VG Membership.
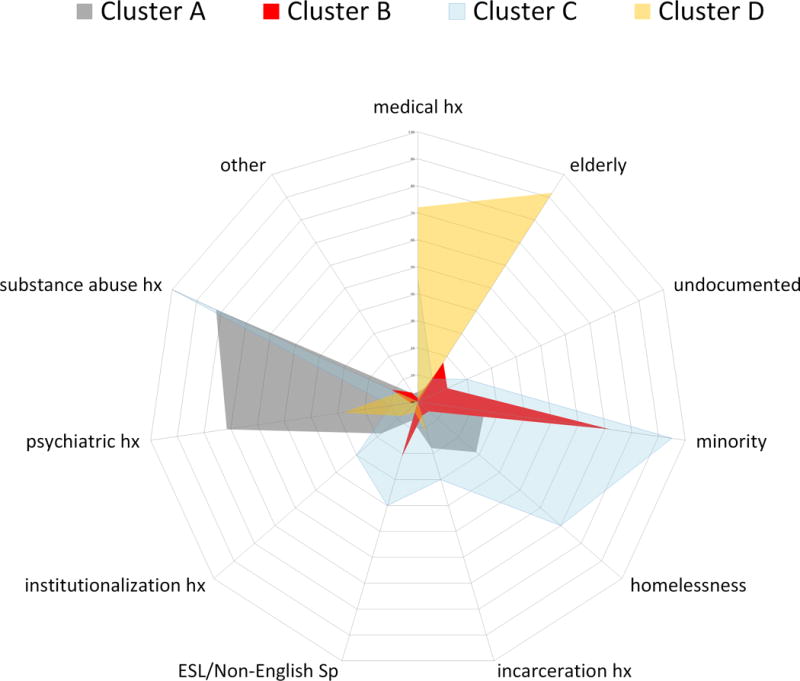
Radial axes represent the percent of patients belonging to each vulnerability group within each cluster. Different shaded areas connect the percentages that define each cluster. For example, cluster C is shown in light blue, characterized by the high incidence of minority status, substance abuse history and minority status in the cluster.
Analyses of rehabilitation outcomes revealed significant differences between clusters in duration of stay (p = .012) and cognitive FIM score change from admission to discharge, (p = .014). Pairwise comparisons, using least-significance difference to correct for multiple comparisons, indicated statistically significant differences between Clusters B and C in duration of stay; and differences in FIM cognitive gains between Clusters A vs. D, A vs. B and C vs. D. Though not statistically significant, large differences in FIM total score and FIM motor score change were also observed between Clusters A and B in pairwise comparisons.
Chi-squared tests on discharge disposition, χ2 (6, N = 148) = 12.657, p = .049, and primary person at discharge, χ2 (6, N = 148) = 8.103, p = .231, showed large but statistically insignificant group differences between clusters when using a more stringent cut-off due to multiple comparisons (α = .01).
Discussion
Using cluster analysis to explore the relationship between inpatient rehabilitation outcomes and binary socioeconomic categories, health histories, and demographics, we found complex, multivariate associations between vulnerability factors that impact acute TBI rehabilitation outcomes. Results demonstrated four distinct, relatively stable clusters. Cluster A contained primarily White patients with significant substance abuse and psychiatric histories. Cluster B, the largest cluster, was marked by patients who belonged to a racial/ethnic minority group, with often limited English proficiency. Cluster C was comprised of minority patients with substance abuse, incarceration, and homelessness histories. Cluster D was marked by elderly patients with complex medical comorbidities, and the cluster’s average FIM gains suggest that their functional gains may not be fully optimized during the acute stay window and are likely to continue during their prolonged stay at another acute/subacute facility. Duration of inpatient stay was shortest for patients in Cluster B, who were also likely to make smaller total and cognitive FIM gains, and more likely to be discharged home than any other cluster. Cluster A and C both appeared to respond well to acute rehabilitation with higher FIM gains, which may, in part, also explain the longer duration of stay observed for these groups on average.
Study Limitations
Our study has two main limitations. First, our diverse, urban data from one of the most ethnically diverse metropolitan regions in the U.S., may not be entirely representative of different U.S. regions that are more homogenous demographically. Second, cluster analyses’ micro-level results are often sensitive to type, number and definition of input variables used. That said, our overall results appear consistent with our group’s earlier SES analyses and identifies a complex, cautionary relationship between clusters of vulnerable groups and rehabilitation outcomes that can be replicated by other sites. Indeed, simplistic univariate analyses has produced counter-intuitive or null results by washing-out significant outcome differences of latent groups13. In contrast, we challenge the notion of equity in terms of access to services and outcomes in the acute rehabilitation landscape.
Conclusions
Our findings suggest that hospital policy changes (e.g., duration of stay) or improvements in service provision may be needed to address disparities in rehabilitation services rooted in complex SES relationships. Programs that augment staff’s language skills, ability to offer substance abuse therapy, systematically provide appropriate referrals or liaise with intensive social work services may be beneficial in addressing the identified gap in service provision to minority patients14. Similarly, increased recruitment, training, and retention options for bilingual and multiethnic professionals may be considered to optimize gains from acute inpatient TBI rehabilitation.
Highlight.
Simultaneous co-occurrence (i.e., clustering) of some demographic and clinical variables may affect the acute rehabilitation outcomes of patients with TBI, rendering ethic/racial minority and elderly groups particularly vulnerable to shorter stays despite small gains in functional variables.
Acknowledgments
Work conducted with support from the Administration for Community Living, National Institute on Disability, Independent Living and Rehabilitation Research, Advanced Rehabilitation Research Training (PI: Dr. Rath) and TBI Model Systems (PI: Dr. Bushnik) grants, nos. 90AR5014 and 90DP0047. Information presented in the manuscript has been partially presented orally and/or as a scientific poster at the APA Div. 22 conference (NM, 2017) and at the ACRM (GA, 2017). The manuscript represents original work, has not been published elsewhere and is not submitted for review to any other journal before. Authors report no conflict of interest.
Abbreviations
- TBI
Traumatic Brain Injury
- FIM
Functional Independence Measure
- SES
Socio-Economic Status
- VG
Vulnerable Group
- TBIMS
Traumatic Brain Injury Model Systems
- ESL
English as Second Language
- hx
history
- MCO
Managed Care Organization
- Cog
Cognitive
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
N. Erkut Kucukboyaci, Rusk Institute of Rehabilitation, NYU Langone, Dept. of Rehabilitation Medicine.
Coralynn Long, Rusk Institute of Rehabilitation, NYU Langone, Dept. of Psychology
Michelle Smith, Rusk Institute of Rehabilitation, NYU Langone, Dept. of Rehabilitation Medicine
Joseph F. Rath, Rusk Institute of Rehabilitation, NYU Langone, Dept. of Rehabilitation Medicine
Tamara Bushnik, Rusk Institute of Rehabilitation, NYU Langone, Dept. of Rehabilitation Medicine.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Writing Group Members, American Heart Association Statistics Committee, Stroke Statistics Subcommittee Heart Disease and Stroke Statistics-2016 Update: a report from the American Heart Association. Circulation. 2016;2016:133:e38–60. doi: 10.1161/CIR.0000000000000350. Accessed 2/17. [DOI] [PubMed] [Google Scholar]
- 2.Roebuck-Spencer T, Cernich A. Epidemiology and Societal Impact of Traumatic Brain Injury. In: Sherer M, Sander AM, editors. Handbook on the Neuropsychology of Traumatic Brain Injury. New York, NY: Springer New York; 2014. pp. 3–23. [Google Scholar]
- 3.Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: difference by race. J Head Trauma Rehabil. 2005;20(1):229–38. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Lequerica A, Krch D. Issues of cultural diversity in acquired brain injury (ABI) rehabilitation. NeuroRehabilitation. 2014;34(4):645–53. doi: 10.3233/NRE-141079. [DOI] [PubMed] [Google Scholar]
- 5.Pappadis MR, Sander AM, Struchen MA, Leung P, Smith DW. Common misconceptions about traumatic brain injury among ethnic minorities with TBI. J Head Trauma Rehabil. 2011;26(4):301–311. doi: 10.1097/HTR.0b013e3181e7832b. [DOI] [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality (AHRQ) (Publication#11-0005-3-EF).Disparities in Healthcare Quality Among Racial and Ethnic Minority Groups - Selected Findings From the 2010 National Healthcare Quality and Disparities Reports. https://archive.ahrq.gov/research/findings/nhqrdr/nhqrdr10/minority.html, Accessed 10/17.
- 7.Peterson-Besse JJ, Walsh ES, Horner-Johnson W, Goode TD, Wheeler B. Barriers to Health Care Among People With Disabilities Who are Members of Underserved Racial/Ethnic Groups: A Scoping Review of the Literature. Medical Care. 2014;52:S51–S63. doi: 10.1097/MLR.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 8.Arango-Lasprilla JC, Kreutzer JS. Racial and ethnic disparities in functional, psychosocial, and neurobehavioral outcomes after brain injury. J Head Trauma Rehabil. 2010;25(2):128–136. doi: 10.1097/HTR.0b013e3181d36ca3. [DOI] [PubMed] [Google Scholar]
- 9.TBIMS National Database Standard Operating Procedures. https://www.tbindsc.org/SOP.aspx, form 101a: Identification of Subjects. Accessed 10/17.
- 10.Anderberg MR. Cluster analysis for applications. New York: Academic Press and Hartigan, J. A.; 1973. [Google Scholar]
- 11.Zhang T, Ramakrishnon R, Livny M. Proceedings of the ACM SIGMOD Conference on Management of Data. Montreal, Canada: ACM; 1996. BIRCH: An efficient data clustering method for very large databases. [Google Scholar]
- 12.Glubo H, McDermott H, Smith-Wexler L, Long C, Rath JF, Bushnik T. Poster presented at the National Multicultural Conference and Summit. Atlanta, GA: 2015. Multiple jeopardy and disparities in functional outcomes due to TBI-related disability. [Google Scholar]
- 13.Corrigan JD, Cuthbert JP, Whiteneck GG, Dijkers MP, Coronado V, Graham JE. Representativeness of the Traumatic Brain Injury Model Systems National Database. J Head Trauma Rehabil. 2012;27(6):391–403. doi: 10.1097/HTR.0b013e3182238cdd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Snowden L, Masland M, Guerrero R. Federal civil rights policy and mental health treatment access for persons with limited English proficiency. Am Psychol. 2007;62:109–117. doi: 10.1037/0003-066X.62.2.109. [DOI] [PubMed] [Google Scholar]


