Abstract
Objectives:
This study of loneliness across adult lifespan examined its associations with sociodemographics, mental health (positive and negative psychological states and traits), subjective cognitive complaints, and physical functioning.
Design:
Secondary analysis of cross-sectional data
Participants:
340 community-dwelling adults in San Diego, California, mean age 62 (SD = 18) years, range 27–101 years, who participated in three community-based studies
Measurements:
Loneliness measures included UCLA Loneliness Scale Version 3 (UCLA-3), 4-item Patient-Reported Outcomes Measurement Information System (PROMIS) Social Isolation Scale, and a single-item measure from the Center for Epidemiologic Studies Depression (CESD) scale. Other measures included the San Diego Wisdom Scale (SD-WISE) and Medical Outcomes Survey- Short form 36.
Results:
The different measures of loneliness were highly correlated. 76% of subjects had moderate-high levels of loneliness on UCLA-3, using standardized cut-points. Loneliness was correlated with worse mental health and inversely with positive psychological states/traits. Even moderate severity of loneliness was associated with worse mental and physical functioning. Loneliness severity and age had a complex relationship, with increased loneliness in the late-20s, mid-50s, and late-80s. There were no sex differences in loneliness prevalence, severity, and age relationships. The best-fit multiple regression model accounted for 45% of the variance in UCLA-3 scores, and three factors emerged with small-medium effect sizes: wisdom, living alone and mental well-being.
Conclusions:
The alarmingly high prevalence of loneliness and its association with worse health-related measures underscore major challenges for society. The non-linear age-loneliness severity relationship deserves further study. The strong negative association of wisdom with loneliness highlights the potentially critical role of wisdom as a target for psychosocial/behavioral interventions to reduce loneliness. Building a wiser society may help us develop a more connected, less lonely, and happier society.
INTRODUCTION
Loneliness has been considered the latest global health epidemic, with serious health implications. According to Vivek Murthy, the former US Surgeon General, the reduction in life span associated with loneliness is similar to that caused by smoking 15 cigarettes a day, and is greater than that due to obesity (McGregor, 2017). The UK government recently established a Ministry of Loneliness to address psychosocial and health needs of lonely people. Issues regarding loneliness have also drawn attention of the private sector, as shown by a recent study exploring how businesses and governments can partner to address loneliness in the aging population (Myers and Palmarini, 2017). In China, loneliness levels in older adults increased from 1995 to 2011 by more than one standard deviation (Yan et al., 2014).
Loneliness has been linked to poor mental health [e.g., depression, hopelessness, substance use, and cognitive impairment], as well as worse physical health [e.g., malnutrition, worse motor function, hypertension, disrupted sleep, frailty], and higher mortality (Aanes et al., 2011; Boss et al., 2015; Cacioppo et al., 2002; Tabue Teguo et al., 2016; Yu et al., 2016). Biological mechanisms such as dysregulated hypothalamic-pituitary-adrenal axis function and dysregulated immune function have been proposed to mediate the link between loneliness and these poor health outcomes (Cacioppo et al., 2002; van Beljouw et al., 2014).
Loneliness is defined as distress resulting from a discrepancy between actual and desired social relationships (Hawkley and Cacioppo, 2010). Loneliness may be considered a personality trait associated with negative states (anxiety, depression) and negative traits (lack of optimism, lack of resilience) (Ben-Zur, 2012; Zebhauser et al., 2014). Most personality traits are relatively stable with roughly 35%−50% heritability, though they are also modifiable. According to van Roekel et al. (2016), loneliness may have both trait and state characteristics; however, persistence of loneliness can lead to negative health consequences. Loneliness is distinct from living alone, solitude, and social isolation; though they may be interrelated. Reported psychosocial risk factors for loneliness include having few close relationships, being single (widowed, divorced, or never married), worsening physical health, and lower socioeconomic status (Cohen-Mansfield et al., 2016; Jakobsson and Hallberg, 2005); all of these factors may increase social isolation.
The reported prevalence of loneliness in the US ranges from 17% to 57% in the general population and is higher in people with physical and mental illnesses including heart disease, depression, anxiety and dementia (Musich et al., 2015). The differing prevalence rates may be related to varied definitions of loneliness, differences in loneliness measures used, and specific subpopulation studied.
Relationships of loneliness severity with age and sex are not clear. Studies have reported increased loneliness during adolescence (Rokach, 2000), middle age (Luhmann and Hawkley, 2016; Wilson and Moulton, 2010), and older age (Ernst and Cacioppo, 1999; Fees et al., 1999; Jylha, 2004). The relationship between loneliness and age is confounded by greater prevalence of certain risk factors for loneliness in older age, e.g., chronic physical illnesses, disability, and loss of relationships (Penninx et al., 1997; Tijhuis et al., 1999). Findings about sex differences are also mixed, with reports of greater loneliness in women (Jakobsson and Hallberg, 2005; Pinquart and Sorensen, 2001; Victor and Bowling, 2012), men (Djukanovic et al., 2015), or neither (Jylha, 2004; Nicolaisen and Thorsen, 2014a). Such inconsistent findings might reflect sex-related differences in loneliness risk factors, reporting biases, and divergent constructs of loneliness (Arber and Ginn, 1994; De Jong Gierveld and Van Tilburg, 2010; Tornstam, 1992).
Assessments of loneliness can be broadly grouped into 1) multiple-item scales that do not explicitly use the words “lonely” or “loneliness” and 2) single-item measures that directly ask subjects to rate frequency/severity of “feeling lonely.” Commonly used multiple-item scales include the uni-dimensional UCLA Loneliness Scale Version 3 (UCLA-3) (Russell, 1996) and the multi-dimensional De Jong Gierveld Loneliness Scale that assesses social and emotional loneliness (de Jong-Gierveld and Kamphuis, 1985). Single-item measures include item #14 from the Center for Epidemiologic Studies Depression (CESD) scale (Radloff, 1977) as well as other similar inquires of “Did you feel lonely much of the time over the past week?” Multiple-item scales assess a specific conceptualization of loneliness and address the problem of potential underreporting due to stigma associated with loneliness as identified by single-item measures. This stigma may disproportionately affect male participants (de Jong Gierveld et al., 2006). Nicolaisen and colleagues examined both a multiple-item scale (De Jong Gierveld Loneliness Scale) and a single-item measure of loneliness in participants aged 18–81 years, and found that women were more lonely to report loneliless on the direct question while men appeared more lonely on the multiple-item scale, though only in the younger age groups (Nicolaisen and Thorsen, 2014b).
Though the relationships of loneliness with resilience and optimism have been examined (Ben-Zur, 2012; Zebhauser et al., 2014), the association between loneliness and wisdom has not been investigated. Wisdom is an important but understudied entity. Discussed in religious and philosophical literature since ancient times, wisdom has only been examined empirically during the last four decades. Published studies including literature reviews, an expert consensus panel, and examination of an ancient scripture suggest that wisdom is a complex human trait with specific components- i.e., emotional regulation, self-reflection, pro-social behaviors such as empathy and compassion, decisiveness, social advising, tolerance of divergent values, and spirituality (Jeste and Lee, 2018; Jeste et al., 2010; Jeste and Vahia, 2008; Meeks and Jeste, 2009). These components have been shown to map onto specific regions of the brain – i.e., prefrontal cortex (dorsolateral and ventromedial), anterior cingulate, and limbic striatum – to forma putative neurocircuitry of wisdom (Meeks and Jeste, 2009). Based on these neurobiological foundations, our group developed a self-report scale for measuring wisdom based on those six components of wisdom, labeled San Diego Wisdom (SD-WISE) scale.
To our knowledge, there has been no study of loneliness using multiple measures of this construct in a well-characterized sample with a broad age range covering the adult lifespan, that has examined the relationships of loneliness with various negative and positive psychological traits and states, especially wisdom, as well as subjective cognitive and physical functioning. The present study examined the severity and prevalence of loneliness using three published measures of loneliness.
Based on the published literature, we hypothesized that loneliness would increase with age, but would not differ between women and men. We also hypothesized that loneliness would be associated directly with measures of worse mental, cognitive and physical functioning; and inversely with levels of wisdom, optimism, resilience, and well-being. Lastly, we explored which factors were associated with loneliness when entered into a multivariate model.
METHODS
Study Participants
The current report is based on secondary analyses from a combined dataset of three study cohorts (total N=340), described below. All three cohorts had several similar inclusion and exclusion criteria: 1) community-dwelling adults, 2) provision of written informed consent to participate in the study, 3) fluency in English, 4) physical and mental abilities to complete the study assessments, 5) no known diagnosis of dementia, and 6) completion of the UCLA-3 measure of loneliness. Additional selection criteria for specific studies are described below.
UCSD Successful AGing Evaluation or SAGE cohort (age 21 −100 years, Lifespan or LS): This study sample has been previously described (Jeste et al., 2013; Thomas et al., 2016). Briefly, it included 190 community-dwelling residents of San Diego County who met the following additional inclusion criteria: 1) aged 25–100 years, and 2) had a telephone line within the home. Persons who lived in nursing homes or required daily skilled nursing care, or had a terminal illness, were excluded. Participants were recruited using list-assisted random digit dialing in the San Diego area.
Healthy comparison subjects from a study of aging and mental illness (age 26–65 years, Young and Middle-aged Adults or YMA): This study cohort has also been described previously (Joseph et al., 2015; Lee et al., 2016a; Lee et al., 2016b; Lee et al., 2018). Participants (n=96) were recruited from the greater San Diego area via advertisements for the parent study. Additional exclusion criteria were: 1) past or present major neuropsychiatric illness as screened by the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998), 2) alcohol or other non-tobacco substance abuse or dependence within 3 prior months, and 3) diagnosis of intellectual disability disorder or a major neurological disorder.
Subjects from a Retirement Community study (age 65+ years, Old Age adults or OA): The OA study cohort includes 54 residents of a senior living community in San Diego County. This is the first published report from this study cohort. Additional inclusion criteria were: 1) 65+ years of age, and 2) residence in an independent living facility. Participants were recruited within the facility, using fliers and scripted presentations.
All the study protocols were individually approved by the UC San Diego Human Research Protections Program (HRPP) and all participants provided written informed consent prior to study participation. This secondary analysis of the combined dataset was reviewed and approved by the UC San Diego HRPP. The data were collected over a period from November 2015 though June 2018.
Sociodemographic and clinical characteristics
Trained study staff conducted structured interviews with the participants and gathered sociodemographic information on age, sex, education level, race/ethnicity, current marital status, living situation, and income. Self-administered standardized assessments were completed for depression (Patient Health Questionnaire-9 or PHQ-9) (Kroenke et al., 2001), anxiety (Brief Symptom Inventory – Anxiety subscale) (Derogatis and Melisaratos, 1983), perceived stress (Perceived Stress Scale) (Cohen et al., 1983), resilience (Connor Davidson Resilience Scale or CD-RISC) (Connor and Davidson, 2003), optimism (Life Orientation Test – Revised or LOTR) (Scheier et al., 1994), satisfaction with life (Satisfaction with Life Scale or SWLS) (Diener et al., 1985), and wisdom (San Diego Wisdom Scale or SD-WISE) (Thomas et al., 2017). Shortly after its development, SD-WISE was included in the study assessments from July 2017 onward.
Physical and mental health assessments included physical functioning and mental well-being based on the component scores from the Medical Outcomes Survey - Short Form 36 (SF-36) (Ware and Sherbourne, 1992).
Self-reported Cognitive Complaints
The assessment of subjective cognitive complaints included the Cognitive Failures Questionnaire that measures forgetfulness, distractibility, and false triggering (Broadbent 1982, Rast 2008). Please note that this is not an objective measure of cognitive function.
Loneliness Measures
The 20-item UCLA Loneliness Scale (Version 3) or UCLA-3 is the most commonly used measure, with strong test-retest reliability, high internal consistency, and validity. While the word “lonely” is never used explicitly, participants rate the frequency of several experiences (e.g., “How often do you feel in tune with others around you?” or “How often do you feel left out?”) on a 4-point Likert scale (options: “I never feel this way”, “I rarely feel this way”, “I sometimes feel this way”, and “I often feel this way.”) The cut-offs for loneliness severity on the UCLA-3 scale were adapted from Cacioppo and Patrick (2008) (Cacioppo and Patrick, 2008) and include: Total score < 28 = No/Low Loneliness, Total score 28 – 43 = Moderate Loneliness, and Total score >43 = High Loneliness.
The 4-item Patient-Reported Outcomes Measurement Information System (PROMIS) Social Isolation scale was also used. The items overlap with the UCLA-3 (items #11, 13, 14, 18) though they are scored on a 5-point Likert scale (options: “Never”, “Rarely”, “Sometimes”, “Usually”, and “Always.”). The PROMIS items include: “I feel left out,” “I feel that people barely know me,” “I feel isolated from others,” “I feel that people are around me, but not with me.” All items assess perceived social isolation, with the first item specifically addressing distress from perceived social isolation. The scores were interpreted as being lonely if the overall score was greater than 8 (i.e., participants rated “sometimes” or higher on any of the four items.)
In order to compare the multiple-item measures with a single-item measure of loneliness, item #14 from the Center for Epidemiologic Studies Depression Scale (CESD) was completed. This item asks participants to rate the frequency of “I felt lonely” over the preceding week with the following answer options: “Rarely or none of the time,” “Some or a little of the time (1–2 days)”, “Occasionally or moderate amount of time (3–4 days)” and “Most or all of the time (5–7 days)” (Radloff, 1977). The scores were interpreted as being lonely if the subject rated feeling lonely “some or a little of the time” or more frequently.
Of note, the UCLA-3 and PROMIS Social Isolation scale do not inquire about a specific time period for these items, while the CESD #14 item inquires about loneliness over the past week. This could be a critical need for development of future loneliness scales as acute loneliness may be an adaptive social-motivating response, whereas sustained/persistent loneliness is likely maladaptive, and associated with deleterious psychosocial and biological effects (Hawkley and Cacioppo, 2004).
Statistical Analyses
Variables were assessed for violation of distribution assumptions (skew and kurtosis) and were log-transformed as necessary. The three study cohorts (LS, YMA, and OA) were first compared by age group. The 25–65 year old participants from the LS study were compared with the YMA cohort and the 65+ year old participants from the LS study were compared to the OA cohort. The compared samples were similar in proportion of women and loneliness scores; therefore, they were combined for subsequent analyses.
One-Way ANOVA with post-hoc Least Significant Difference (LSD) testing or Pearson’s Chi-square tests with post-hoc Chi-square testing were used to assess differences in sociodemographic factors, psychological traits/states, subjective cognitive complaints, physical functioning, and loneliness measures by subgroup of loneliness severity and by sex. However, recent studies show that this two-step procedure may miss between-group differences; it is possible that there is a significant difference between two groups, while the F test is nonsignificant (Chen et al., 2018).
Though prevalence of loneliness was assessed using all three measures of loneliness described above, given its broad use in the literature and excellent psychometric properties, the UCLA-3 was employed as the primary measure of loneliness severity and used in the multivariate data analyses. We used locally weighted scatterplot smoothing (LOWESS) curve fitting, a nonparametric method to fit the potential non-linear relationship between loneliness severity and age. We then modeled such relationship using a parametric cubic-spline function, which requires specification of knot/break points for the function, akin to two points to anchor a linear relationship. While the LOWESS suggests potential forms of non-linear relationship, the cubic-spline function allows for formal testing of the suggested non-linear relationship.
We conducted bivariate correlational analysis with UCLA-3 scores as the dependent variables and other sociodemographic and clinical variables as independent variables. The Fisher r-to-z transformation was performed to compare the correlations of loneliness with other factors in women and men. Then we performed multiple regression analyses, aided by least absolute shrinkage and selection operator (LASSO) variable selection, to identify the best multivariable model of loneliness. Missing data were imputed according to the method of chained equations. There were no missing data for age, sex, and race/ethnicity. The following measures had missing data for fewer than 3% of the participants: living situation, income, depression, anxiety, perceived stress, resilience, optimism, and mental well-being. Education level and current marital status had missing data for 4–5%. The SD-WISE total score had the highest level of missing data at 36% - a direct result of this scale having been developed and added to the assessment battery only recently (Thomas, et al., 2017). Thus, study that started earlier (YMA) tended to have more subjects with missing SD-WISE, whereas the LS and OA subjects were more likely to have SD-WISE scores. We formally assessed this proposition by modeling missingness of SD-WISE using a logistic regression, and found that age did predict missing SD-WISE. We included age in all regression analyses to control for potential bias due to missing SD-WISE.
In the multiple regression analysis, regression coefficients were made commensurate by standardizing each variable. Independent variables were ranked by the order in which they entered the LASSO regression. LASSO overcomes various limitations of classic variable selection procedures such as multicollinearity to provide reliable selection of independent variables (Chen et al., 2016). As LASSO does not attempt to maximize R2, the R2 value is a less-biased indicator of the variance explained by the resulting model. Independent variables selected by LASSO were entered into linear model for further trimming using backwards elimination. The model presented is the final trimmed model such that only the independent variables that are statistically significant remain in the model. We used this approach rather than the forward or stepwise selection as the backward method provides the most reliable approach for trimming statistical models (Wang et al., 2017). All analyses were carried out in R.
We present effect sizes and p-values for all of these statistical tests, and interpret small-medium effect sizes (i.e., Cohen’s d > .20 or r ≥ .30) as meaningful. Significance was defined as Type I error alpha = 0.05 (two-tailed) for all analyses, and False Discovery Rate (FDR) was used to account for multiple comparisons to ensure overall Type 1 error at alpha = 0.05.
RESULTS
Prevalence of Loneliness across Measures
The total sample included 340 subjects, mean age 62 (SD = 18) years, ranging from 27–101 years. Fifty percent of the participants were women. The prevalence rates varied depending on the measure of loneliness. On the UCLA-3, 76% of all subjects reported moderate to high level of loneliness, while only 38% and 8.6% of subjects reported feeling lonely on the PROMIS and CESD, respectively. The PROMIS Social Isolation scale scores were highly correlated with the UCLA-3 total score (Spearman’s rho = 0.76, p < 0.001) and the UCLA-3 subscore excluding the four PROMIS items (Spearman’s rho =0.64, p<0.001). We did not examine loneliness prevalence by age group due to the small numbers.
This sample included 96 subjects from our group’s previous work that reported on loneliness in a non-psychiatric comparison group (Eglit et al., 2018), which comprised the YMA cohort in the present study. Mean UCLA-3 scores were similar between the Eglit cohort [34.7 (SD = 10.4)] and the current sample [35.9 (SD = 10.7); t200=−0.8, p = 0.2, d = −0.12.]
Comparison by severity of loneliness
The subjects were compared by severity of loneliness, as defined by the UCLA-3 scores (Table 1). The three subgroups (No/Low vs. Moderate vs. High Loneliness) were similar in age, sex, race and educational attainment. The high loneliness group was more likely to be single, live alone, and have personal income <$35,000. Across the subgroups, high loneliness was associated with greater depression, anxiety, and perceived stress; less resilience, optimism, mental well-being, wisdom; and greater cognitive complaints. Of note, the subgroup with a moderate level of loneliness also had worse psychological traits/states (i.e., depression, anxiety, perceived stress, resilience, optimism, mental well-being, wisdom) and subjective cognition compared to the No/low loneliness group. Although there was no significant difference in mean scores of physical functioning across all three groups on ANOVA, there was a significant difference between No/Low and Moderate Loneliness (t263 = 2.2, p = 0.03, d = 0.30) and no significant difference between Moderate and High Loneliness (t252 = −0.71, p = 0.48, d = −0.10).
Table 1.
Comparison of Study Participants by Severity of Loneliness*
| No / Low Loneliness (A) | Moderate Loneliness (B) | High Loneliness (C) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | F or X2 | p | Post-hoc Significant Comparisons | |
| Number (%) | 82 (24%) | 184 (54%) | 74 (22%) | |||||||||
| Sociodemographic | ||||||||||||
| Age (years) | 82 | 60.0 | 178.0 | 184 | 63.0 | 18.0 | 74 | 59.8 | 19.0 | 1.26 | 0.28 | |
| Sex (% Female) | 82 | 56.1% | 184 | 47.3% | 74 | 50.0% | 1.76 | 0.41 | ||||
| Race (% Caucasian) | 82 | 76.8% | 184 | 80.4% | 74 | 77.0% | 0.63 | 0.73 | ||||
| Education attainment | 79 | 176 | 71 | 2.99 | 0.56 | |||||||
| High school and below | 8.9% | 9.7% | 7.0% | |||||||||
| Some college | 59.5% | 52.3% | 63.4% | |||||||||
| Graduate school/higher | 31.6% | 38.1% | 29.6% | |||||||||
| Marital status (% single) | 79 | 29.1% | 176 | 36.9% | 71 | 53.5%a | 9.87 | 0.007 | ||||
| Living alone (%) | 82 | 9.8%a | 177 | 20.3% | 73 | 34.2%a | 14.1 | 0.001 | ||||
| Personal income | 79 | 170 | 70 | 25.9 | <0.001 | |||||||
| Less than $35,000 | 31.6% | 24.7%a | 55.7%a | |||||||||
| $35,000 to $49,999 | 12.7% | 14.1% | 15.7% | |||||||||
| $50,000 to $74,999 | 16.5% | 21.2% | 12.9% | |||||||||
| $75,000 or more | 39.2% | 40.0% | 15.7%a | |||||||||
| Negative psychological traits/states | ||||||||||||
| Depression (PHQ-9) | 79 | 1.1 | 1.8 | 181 | 2.2 | 2.8 | 72 | 4.6 | 4.4 | 26.6 | <0.001 | A < B < C |
| Anxiety (BSI) | 81 | 0.67 | 1.8 | 183 | 1.3 | 1.8 | 74 | 2.3 | 2.8 | 12.1 | <0.001 | A < B < C |
| Perceived Stress (PSS) | 80 | 7.9 | 4.8 | 181 | 10.9 | 4.4 | 72 | 15.3 | 5.7 | 45.6 | <0.001 | A < B < C |
| Positive psychological traits/states | ||||||||||||
| Resilience (CD-RISC) | 82 | 26.3 | 3.2 | 180 | 24.1 | 3.6 | 74 | 21.4 | 4.4 | 34.1 | <0.001 | A < B < C |
| Optimism (LOTR) | 80 | 34.9 | 4.8 | 180 | 31.3 | 5.4 | 74 | 27.4 | 6.5 | 35.7 | <0.001 | A < B < C |
| Mental Well-being (SF-36) | 82 | 57.8 | 4.5 | 183 | 55.0 | 7.0 | 71 | 47.7 | 9.5 | 41.5 | <0.001 | A < B < C |
| Wisdom (SD-WISE) | 48 | 4.26 | 0.42 | 122 | 3.93 | 0.35 | 47 | 3.62 | 0.39 | 34.6 | <0.001 | A < B < C |
| Subjective Cognition | ||||||||||||
| Cognitive Complaints (CFQ) | 81 | 18.3 | 10.5 | 176 | 27.4 | 12.8 | 72 | 31.1 | 13.1 | 22.9 | <0.001 | A < B < C |
| Physical health | ||||||||||||
| Physical functioning (SF-36) | 82 | 50.6 | 9.5 | 183 | 47.6 | 10.3 | 71 | 48.6 | 9.2 | 2.5 | 0.083 | |
| Loneliness measures | ||||||||||||
| UCLA-3 | 82 | 23.9 | 2.2 | 184 | 34.7 | 4.6 | 74 | 51.9 | 6.8 | 675.0 | <0.001 | A < B < C |
| PROMIS Social Isolation | 53 | 39.3 | 4.6 | 136 | 45.9 | 5.5 | 54 | 56.8 | 7.1 | 131.0 | <0.001 | A < B < C |
| CESD Item #14 | 81 | 0.09 | 0.28 | 181 | 0.26 | 0.54 | 74 | 1.01 | 0.99 | 50.3 | <0.001 | A < B < C |
For all measures (except the Cognitive complaints score, loneliness scales, depression, anxiety, and perceived stress), lower scores suggest worse functioning.
BSI = Brief Symptom Inventory – Anxiety subscale; measure of anxiety (Derogatis and Melisaratos, 1983)
CD-RISC = Connor Davidson Resilience Scale; measure of resilience (Connor and Davidson, 2003)
CESD = Center for Epidemiologic Studies Depression Scale; measure of loneliness (Radloff 1977)
CFQ = Cognitive Failures Questionnaire; measure of forgetfulness, distractibility and false triggering (Broadbent 1982, Rast 2008)
LOTR = Life Orientation Test – Revised; measure of optimism (Scheier 1994)
PHQ-9 = Patient Health Questionnaire-9; measure of depression (Kroenke 2001)
PROMIS = Patient-Reported Outcomes Measurement Information System
PSS = Perceived Stress Scale; measure of perceived stress (Cohen 1983)
SD-WISE = San Diego Wisdom Scale; measure of wisdom (Thomas 2017)
SF-36 = Medical Outcomes Survey - Short Form 36; measure of mental and physical functioning (Ware and Sherbourne 1992)
UCLA-3 = UCLA Loneliness Scale (Version 3); measure of loneliness (Russell 1996)
Cutoff for loneliness
UCLA-3 Total score < 28 = No/Low Loneliness
UCLA-3 Total score 28 – 43 = Moderate Loneliness
UCLA-3 Total score >43 = High Loneliness
Post-hoc Chi-square tests were significantly different at the Bonferroni-corrected p-value level
The women and men were similar in mean age and age distribution, education attainment, and number of children. Women and men also did not differ on depression, mental well-being, overall wisdom scores, or cognitive complaints. However, women were more likely to be currently single, live alone, as well as have lower personal incomes, worse physical functioning, greater anxiety and perceived stress, and less resilience than men (data not shown). Women and men had similar mean scores of loneliness on the UCLA-3 (35.7 (SD = 10.8) and 36.1 (SD = 10.7), respectively) and PROMIS measures (8.0 (SD = 3.5) and 8.0 (SD = 3.4), respectively), though women had slightly higher mean scores on the CESD single-item question (0.47 (SD = 0.78) and 0.29 (SD = 0.62), respectively, t334 = 2.33, p = 0.02). Women and men were similar in prevalence of loneliness across all three measures: UCLA-3 (73% and 79%), PROMIS (40% and 36%) and CESD (11% and 7%).
Loneliness severity was worse in the late-20s, mid-50s and late-80s:
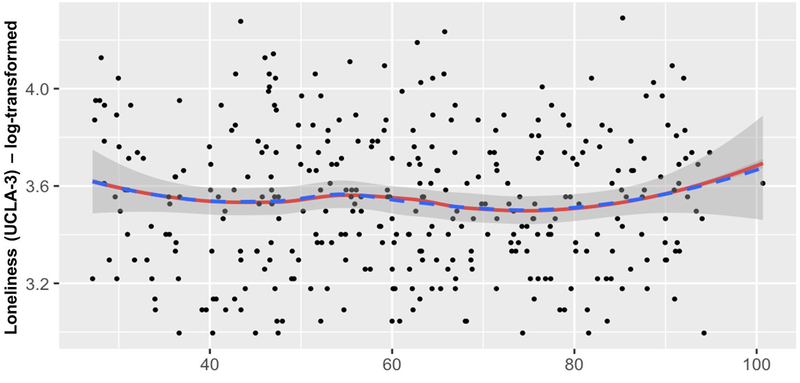
The relationship between loneliness severity (UCLA-3) and age was plotted and fitted with a spline model in Figure 1. As there was no significant age x sex interaction for loneliness, the data are shown for the entire sample. The data highlight higher levels of loneliness at three different age-points: young adulthood (late-20s), middle-age (mid-50s), and old-old (late-80s). We first examined potential non-linear relationship between loneliness severity and age using the non-parametric LOWESS curve method. We then modeled the suggested non-linear pattern using a parametric cubic-spline function, which requires specification of a knot/break point to join the two cubic functions. Thus, there is one cubic function between 20 and 53 and another cubic function between 53 and 90. When tested against the null of a linear relationship, p-value = 0.019, which is statistically significant, ruling out random fluctuations.
Figure 1: Relationship between Loneliness severity and Age(N=340).
Blue dotted line: LOESS curve fit, Red solid line: Linear spline model using age 53 year knot/break point
UCLA-3 = UCLA Loneliness Scale (Version 3); measure of loneliness (Russell 1996)
The linear spline model significantly differs from linear age effect (Wald statistic = 7.93, p = 0.019)
Loneliness was associated with negative states and traits:
Loneliness (UCLA-3) correlated with several negative states and traits. People who were more lonely also had worse depression, anxiety, perceived stress, and cognitive complaints (Table 2).
Table 2:
Spearman’s Correlations of Loneliness in Women and Men
| Total | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| N | rho | N | rho | N | rho | Z | p | |
| Sociodemographic Measures | ||||||||
| Age | 340 | −0.01 | 170 | 0.03 | 170 | −0.06 | 0.82 | 0.41 |
| Race/Ethnicitya | 340 | −0.02 | 170 | −0.02 | 170 | −0.01 | −0.09 | 0.93 |
| Educationb | 326 | −0.03 | 164 | −0.09 | 164 | 0.01 | −0.9 | 0.37 |
| Current marital statusc | 326 | 0.17*** | 164 | 0.12 | 164 | 0.24** | −1.1 | 0.27 |
| Living aloned | 332 | −0.21*** | 165 | −0.18* | 165 | −0.28*** | 0.95 | 0.34 |
| Personal Incomee | 319 | −0.19** | 168 | −0.15* | 168 | −0.21** | 0.56 | 0.58 |
| Negative psychological traits/states | ||||||||
| Depression (PHQ-9) | 332 | 0.43*** | 169 | 0.45*** | 164 | 0.40*** | 0.55 | 0.58 |
| Anxiety (BSI) | 338 | 0.32*** | 170 | 0.33*** | 168 | 0.33*** | <0.01 | 0.99 |
| Perceived Stress (PSS) | 333 | 0.49*** | 166 | 0.53*** | 168 | 0.49*** | 0.49 | 0.62 |
| Positive psychological traits/states | ||||||||
| Resilience (CD-RISC) | 334 | −0.47*** | 168 | −0.55*** | 167 | −0.38*** | −1.98 | 0.05 |
| Optimism (LOTR) | 336 | −0.46*** | 169 | −0.45*** | 167 | −0.48*** | 0.35 | 0.73 |
| Mental well-being (SF-36) | 336 | −0.46*** | 167 | −0.44*** | 167 | −0.47*** | 0.34 | 0.74 |
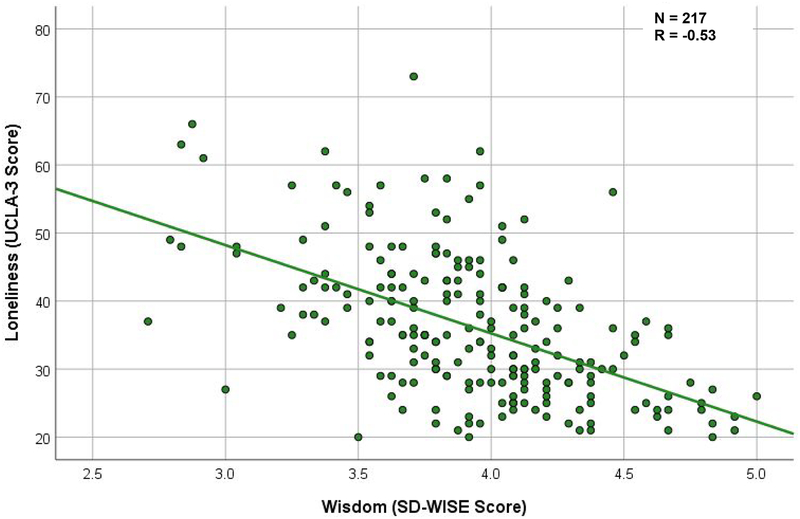
| Wisdom (SD-WISE) | 217 | −0.53*** | 104 | −0.51*** | 113 | −0.56*** | 0.51 | 0.61 |
| Subjective Cognition | ||||||||
| Cognitive complaints (CFQ) | 329 | 0.38*** | 170 | 0.43*** | 166 | 0.27*** | 1.66 | 0.10 |
| Physical health | ||||||||
| Physical Functioning (SF-361) | 336 | −0.12* | 169 | −0.16* | 167 | −0.09 | −0.65 | 0.52 |
BSI = Brief Symptom Inventory – Anxiety subscale; measure of anxiety (Derogatis and Melisaratos, 1983)
CD-RISC = Connor Davidson Resilience Scale; measure of resilience (Connor and Davidson, 2003)
CFQ = Cognitive Failures Questionnaire; measure of forgetfulness, distractibility and false triggering (Broadbent 1982, Rast 2008)
LOTR = Life Orientation Test – Revised; measure of optimism (Scheier 1994)
PHQ-9 = Patient Health Questionnaire-9; measure of depression (Kroenke 2001)
PSS = Perceived Stress Scale; measure of perceived stress (Cohen 1983)
SD-WISE = San Diego Wisdom Scale; measure of wisdom (Thomas 2017)
SF-36 = Medical Outcomes Survey - Short Form 36; measure of mental and physical functioning (Ware and Sherbourne 1992)
Race/Ethnicity is coded as: 101 = Caucasian, 102 = Non-Caucasian
Education is coded as 101 = High school and below, 102 = Some College to Bachelor’s Degree, 103 = Post-Graduate Degree
Current marital status is coded as: 101 = Currently Married/Cohabitating, 102 = Currently Single
Living alone is coded as: 0 = Lives alone, 1 = Lives with someone
Personal Income is coded as: 1 = Less than $10,000, 2 = $10,000 to $19,999, 3 = $20,000 to $34,999, 4 = $35,000 to $49,999, 5 = $50,000 to $74,999, 6 = $75,000 to $99,999, 7 = $100,000 to $149,999, 8 = $150,000 or more.
= p < 0.05,
= p < 0.01;
= p < 0.001
Loneliness was inversely associated with positive states, especially wisdom:
Loneliness was also associated with several positive states/traits. People who were more lonely had lower resilience, optimism, and mental well-being (Table 2). The highest negative correlation of loneliness was with wisdom (see Figure 2). There was no statistically significant difference by sex, so the data are plotted for all subjects. Persons who were wiser were less lonely. Interestingly, very few individuals were lonely and wise, or not lonely and unwise.
Figure 2: Wisdom and Loneliness.
SD-WISE = San Diego Wisdom Scale; measure of wisdom (Thomas 2017)
UCLA-3 = UCLA Loneliness Scale (Version 3); measure of loneliness (Russell 1996)
Multivariate Analysis:
The best multiple regression model achieved with all the variables as potential correlates of loneliness is shown in Table 3a. This model accounted for 45% of the variance. The first step of LASSO identified age, sex, education, living alone, income, depression, perceived stress, cognitive failures (subjective cognitive complaints), optimism, mental well-being, and wisdom. These factors were then entered into a multiple linear model and the following were found to be significant: wisdom, living alone, mental well-being as well as age, sex, perceived stress, optimism, and subjective cognitive complaints. Thus, while we did not find interactive effects, we did find independent additive effects in multiple regression analyses. The factor with the largest effect size was wisdom, followed by living alone, and then mental well-being. As age was retained in both steps, these models also controlled for potential bias due to missing SD-WISE, although power was reduced because of reduced sample size.
Table 3:
Multiple Regression Model of Loneliness
| Table 3a: Loneliness Model in Total Sample (N=340) | ||||
|---|---|---|---|---|
| Variable | B | SE | FDR- adjusted p | Cohen’s d |
| Age | −0.001 | 0.0007 | 0.04 | 0.11 |
| Sex | 0.05 | 0.02 | 0.03 | 0.12 |
| Living alone | 0.13 | 0.03 | 0.0001 | 0.24 |
| Perceived Stress | 0.008 | 0.003 | 0.02 | 0.14 |
| Optimism | −0.01 | 0.004 | 0.004 | 0.17 |
| Mental well-being | −0.007 | 0.002 | 0.0004 | 0.21 |
| Wisdom | −0.17 | 0.03 | <0.0001 | 0.29 |
| Cognitive complaints | 0.002 | 0.0009 | 0.03 | 0.12 |
| Table 3b: Loneliness Model in Each Sex | ||||
| Women (N=170) | ||||
| Variable | B | SE | FDR- adjusted p | Cohen’s d |
| Age | −0.02 | 0.03 | 0.57 | 0.05 |
| Living alone | 0.13 | 0.04 | 0.003 | 0.26 |
| Perceived Stress | 0.008 | 0.004 | 0.11 | 0.16 |
| Optimism | −0.009 | 0.004 | 0.12 | 0.15 |
| Mental well-being | −0.009 | 0.003 | 0.002 | 0.28 |
| Wisdom | −0.19 | 0.04 | 0.0004 | 0.32 |
| Cognitive complaints | 0.002 | 0.001 | 0.24 | 0.11 |
| Men (N=170) | ||||
| Variable | B | SE | FDR- adjusted p | Cohen’s d |
| Age | −0.06 | 0.03 | 0.15 | 0.14 |
| Living alone | 0.15 | 0.05 | 0.01 | 0.24 |
| Perceived Stress | 0.007 | 0.005 | 0.18 | 0.11 |
| Optimism | −0.02 | 0.006 | 0.04 | 0.20 |
| Mental well-being | −0.004 | 0.003 | 0.15 | 0.12 |
| Wisdom | −0.15 | 0.05 | 0.01 | 0.24 |
| Cognitive complaints | 0.002 | 0.001 | 0.15 | 0.12 |
Perceived stress measured with the Perceived Stress Scale (Cohen 1983)
Optimism measured with the Life Orientation Test – Revised (Scheier 1994)
Mental well-being measured with the Medical Outcomes Survey - Short Form 36 (Ware and Sherbourne 1992)
Wisdom measured with the San Diego Wisdom Scale (Thomas 2017)
Cognitive complaints measured with the Cognitive Failures Questionnaire (Broadbent 1982, Rast 2008)
The linear models were also run in women and men separately to assess if the factors associated with loneliness differed by sex (Table 3b). In women, loneliness was associated with less wisdom, living alone, and poorer mental well-being. In men, loneliness was associated with less wisdom, living alone, and less optimism.
DISCUSSION
We examined positive and negative psychological traits/states as well as cognitive and physical functioning as correlates of loneliness in community-dwelling individuals across adult lifespan. We found a surprisingly high prevalence of loneliness (76%) using a commonly used comprehensive scale with excellent psychometric properties (the 20-item UCLA-3) and lower prevalence using other scales: 38% with a 4-item scale (PROMIS) and 8% with a single-item measure (CESD). Opposed to our a priori hypotheses, we found a non-linear relationship between loneliness severity and age, that showed increased loneliness among persons in their late-20s, mid-50s and late-80s. While we did not find sex differences in the mean UCLA-3 and PROMIS scores, women were slightly more likely to report feeling lonely on a single-item question about loneliness. Loneliness was consistently correlated with negative psychological states and traits, and inversely correlated with positive psychological states and traits, especially wisdom. The best multivariate model of loneliness included: lower levels of wisdom, living alone and worse mental well-being.
Seventy-six percent prevalence of loneliness found in this study is higher than found in most published studies of community-based samples. We examined if this higher prevalence was an artifact of sample characteristics, measures used, and severity of loneliness. 1) Our sample was community-based, with more than half of the participants being randomly selected (using random-digit dialing) and excluding institutionalized and severely medically ill persons, in whom loneliness might be even more common and severe. 2) This study used the comprehensive UCLA-3 scale. Other studies using the UCLA-3 have reported mean scores of their sample between 31 and 49 (Kong et al., 2015; Russell, 1996; Springer et al., 2003; Theeke and Mallow, 2013). The mean UCLA-3 score of the current study (35.9 (SD = 10.7)) falls within this range, consistent with different studies. 3) In calculating prevalence of loneliness, we categorized persons with low levels of loneliness as not being lonely. We found that even moderate levels of loneliness were associated with worse negative and positive psychological traits and states as well as worse physical functioning. We did not find a difference in physical functioning between people with moderate versus high levels of loneliness, which might be due to the exclusion of individuals with clinically significant mental or physical disabilities that might interfere with participation. The relationship between loneliness and more severe levels of disability could not be examined. Thus, our findings might be representative of moderate-severe loneliness, atleast in the San Diego Community.
Loneliness prevalence may vary by measure due to different constructs of loneliness measured, reporting biases, and scale sensitivity. Single-item measures of loneliness have reported loneliness 10–39% of subjects (Beutel et al., 2017; Nicolaisen and Thorsen, 2014b; Theeke, 2009; Victor and Bowling, 2012), while 3- to 6-item measures have reported loneliness in 24–55% of subjects (Musich et al., 2015; Nicolaisen and Thorsen, 2014b; Simon et al., 2014). Multiple-item scales (that do not explicitly use the word “loneliness”) were based on specific conceptualizations of loneliness, while single-item measures relied on the respondent’s own concept of and willingness to report loneliness. Individuals might underreport loneliness due to stigma or social desirability bias, and this bias might be worse with the single-item measure. The lower prevalence of loneliness on PROMIS and CESD single-item in our study might reflect lower sensitivity of these brief measures compared to the more comprehensive UCLA-3 (Nicolaisen and Thorsen, 2014b). Alternatively, it is possible that the UCLA-3 scale also captures conditions that are not loneliness. Furthermore, the scales differed over the time period over which loneliness was assessed (single-item: past week, PROMIS and UCLA-3: no specific time period.)
The observed association of loneliness severity with age was consistent with some, but not all of the existing studies with broad age ranges. One study reported a U-shaped relationship between loneliness and age, such that the adolescents/young adults and oldest old were the most lonely (Luhmann and Hawkley, 2016). Other cross-sectional studies have reported greater loneliness among the oldest old (65+ to 80+ year olds) (Dykstra et al., 2005; Perlman and Peplau, 1984; Pinquart and Sorensen, 2001; Victor and Yang, 2012). Some studies suggest that individuals of all ages overestimate the extent and impact of loneliness among older adults – than the older adults themselves report (Abramson and Silverstein, 2006; Dykstra, 2009). Loneliness varies by country and societal structure (Dykstra, 2009; Fokkema et al., 2012). Longitudinal studies have reported age-related increased loneliness in older individuals, especially among the old-old (80+ years) (Dahlberg et al., 2015; Houtjes et al., 2014; Jylha, 2004; Samuelsson et al., 1998; Tijhuis et al., 1999). Many of the large population-based studies were predominantly conducted in Europe, and used single-item measures of loneliness which, as mentioned above, may underestimate prevalence of loneliness.
The relationship between age and loneliness in the present study appeared to be complex and multi-faceted. While no age group seemed to be immune to loneliness, different sociodemographic variables may affect loneliness throughout the lifespan. There is also a paradox of aging: physical health declines but mental health tends to improve with age (Jeste et al., 2013).
The correlations between loneliness and negative/positive psychosocial traits and states were consistent with other studies examining relationships with depression, anxiety, resilience, and optimism (Ben-Zur, 2012; Zebhauser et al., 2014). These findings may reflect interrelationships between loneliness and personality traits and affective states. As these negative/positive psychosocial traits and states are themselves intercorrelated, this highlights the consistency of the loneliness findings. It may be argued that certain components of wisdom such as pro-social behaviors and social advising involve good social relationships and therefore, the inverse correlation between wisdom and loneliness may be a mere tautology. We do not believe that is the case as pro-social behaviors and social advising are not necessarily related to close social relationships or networks. A compassionate person who offers advice when approached by someone else, need not be a socially engaged individual. For example, there are compassionate priests who give sound advice to a parishioner, but do not have personal networks of friends. Likewise, people with sizable social networks may not be compassionate or known for giving wise advice to others.
The multiple regression model highlighted the importance of three factors that emerged with small-medium effect sizes. Wisdom had the largest impact on loneliness, followed by living alone and mental well-being. The influence of wisdom, as measured by SD-WISE, was present in both women and men. Positive psychological traits such as wisdom may be potentially modifiable targets for novel interventions for loneliness. Studies are needed to determine if increasing an individual’s wisdom would reduce his or her loneliness and enhance well-being, and vice versa. They may buffer the negative influences of less modifiable factors such as older age with its associated physical and psychosocial stressors. Living alone is intercorrelated with social isolation, though it is distinct (Holt-Lunstad et al., 2015). The relationship of living alone (and the other factors) with loneliness might be bi-directional, i.e., living alone might increase loneliness and loneliness might, in turn, increase social isolation.
Strengths of this study include consideration of the entire adult lifespan as well as a well-characterized cohort of persons with multiple assessments of loneliness, psychological traits and states, and health. Furthermore, all the participants were community-dwelling individuals. We used three different measures of loneliness, allowing for comparison across measures. This study also examined the relationships of loneliness with wisdom, an understudied personality trait.
Our study also had some important limitations. This was a cross-sectional study; so causality cannot be inferred. Loneliness and other psychological traits were assessed via self-reported measures, which could result in a social desirability response bias as participants may underreport negative traits. However, it should be noted that, by definition, loneliness is a subjective experience that is partially independent of the actual social network size. Loneliness measures differed over the time period of assessment. This study did not include measures of objective cognitive performance or biomarkers, which could elucidate underlying biological mechanisms mediating the relationships between loneliness and health consequences. The sample was comprised primarily of educated Caucasians, which may limit the generalizability of the findings to lower SES and/or minority populations. The SD-WISE (Thomas et al., 2017) total score had a high level of missing data at 36% - a result of this scale having been developed and added to the assessment battery only recently. Age was found to be a significant predictor of missing SD-WISE data. Therefore, to control for potential bias due to missing SD-WISE, age was included in all regression analyses.
Notwithstanding these limitations, loneliness (as assessed by the UCLA-3) was found to be strikingly prevalent and with a significant association with negative mental and other health outcomes. Notably, loneliness also correlated strongly and inversely with wisdom. Wisdom may be a unique protective factor against loneliness. Intriguingly, recent genetics work has reported an association between loneliness and genes expressed in the prefrontal and anterior cingulate cortices (Abedellaoui et al., 2018) - areas that are also related to components of wisdom (Meeks and Jeste, 2009).
While living alone contributes to social isolation, wisdom may affect the quality of social relationships positively, and may offer a unique solution to loneliness, beyond external interventions such as support groups and facilitation of social interactions through technology and social media (Kharicha et al., 2018). The published studies of technology-based interventions to date have been small and limited. Loneliness interventions may be focused internally to influence components of wisdom (e.g., emotional regulation, pro-social behaviors) and well-being, using technology to widely disseminate evidence-based interventions with high fidelity. Though few studies have involved comprehensive wisdom interventions, several studies have reported improvement in wisdom subcomponents, e.g., mindfulness-based stress reduction to improve self-compassion in medical students (Erogul et al., 2014) and goal management training to improve emotion regulation in adults with acquired brain injuries (Tornas et al., 2016).
Conclusions
The loneliness epidemic presents major societal challenges. It is deeply concerning that three-fourths of this community-dwelling sample across the lifespan had moderate to high level of loneliness using a comprehensive measure of loneliness. This examination of loneliness identified increased loneliness at three key timepoints: young adulthood (late-20s), middle-age (mid-50s), and old-old age (late-80s). Loneliness was associated with poor mental health and negative psychological traits. At the same time, the strong negative association between loneliness and wisdom was particularly striking and may suggest a unique solution to loneliness. Thus, loneliness and overall well-being may be improved via increasing individuals’ wisdom, which includes ability to regulate emotions, self-reflect, be compassionate, tolerate opposing viewpoints, and be decisive. Thus, building a wiser society may help us build a more connected, less lonely, and happier society.
Footnotes
Conflict of interest declaration:
The authors have no conflicts of interest to report.
References
- Aanes MM, Hetland J, Pallesen S and Mittelmark MB (2011). Does loneliness mediate the stress-sleep quality relation? The Hordaland Health Study. Int Psychogeriatr, 23, 994–1002. [DOI] [PubMed] [Google Scholar]
- Abedellaoui A, et al. (2018). PHENOME-WIDE INVESTIGATION OF HEALTH OUTCOMES ASSOCIATED WITH GENETIC PREDISPOSITION TO LONELINESS Submitted. [DOI] [PMC free article] [PubMed]
- Abramson A and Silverstein M (2006). Images of Aging in America 2004. Washington, D.C.: AARP and the University of Southern California. [Google Scholar]
- Arber S and Ginn J (1994). Women and aging. Reviews in Clinical Gerontology, 4, 349–358. [Google Scholar]
- Ben-Zur H (2012). Loneliness, optimism, and well-being among married, divorced, and widowed individuals. J Psychol, 146, 23–36. [DOI] [PubMed] [Google Scholar]
- Beutel ME, et al. (2017). Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry, 17, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boss L, Kang DH and Branson S (2015). Loneliness and cognitive function in the older adult: a systematic review. Int Psychogeriatr, 27, 541–553. [DOI] [PubMed] [Google Scholar]
- Cacioppo J and Patrick W (2008). Loneliness: Human Nature and the Need for Social Connection. New York, NY: W.W. Norton & Company, Inc. [Google Scholar]
- Cacioppo JT, et al. (2002). Loneliness and health: potential mechanisms. Psychosom Med, 64, 407–417. [DOI] [PubMed] [Google Scholar]
- Chen T, et al. (2016). Variable selection for distribution-free models for longitudinal zero-inflated count responses. Stat Med, 35, 2770–2785. [DOI] [PubMed] [Google Scholar]
- Chen T, Xu M, Tu J, Wang H and Niu X (2018). Relationship between Omnibus and Post-hoc Tests: An Investigation of performance of the F test in ANOVA. Shanghai Arch Psychiatry, 30, 60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Mansfield J, Hazan H, Lerman Y and Shalom V (2016). Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr, 28, 557–576. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T and Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24, 385–396. [PubMed] [Google Scholar]
- Connor KM and Davidson JR (2003). Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety, 18, 76–82. [DOI] [PubMed] [Google Scholar]
- Dahlberg L, Andersson L, McKee KJ and Lennartsson C (2015). Predictors of loneliness among older women and men in Sweden: A national longitudinal study. Aging Ment Health, 19, 409–417. [DOI] [PubMed] [Google Scholar]
- de Jong-Gierveld J and Kamphuis F (1985). The development of a Rasch-type loneliness scale. Applied Psychological Measurement, 9, 289–299. [Google Scholar]
- De Jong Gierveld J and Van Tilburg T (2010). The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing, 7, 121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong Gierveld J, van Tilburg T and Dykstra PA (2006). Loneliness and Social Isolation In Vangelisti AL and Perlman D (Eds.) The Cambridge handbook of personal relationships (pp. 485–499, Chapter xxii, 891 Pages): Cambridge University Press, New York, NY. [Google Scholar]
- Derogatis LR and Melisaratos N (1983). The Brief Symptom Inventory: an introductory report. Psychol Med, 13, 595–605. [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ and Griffin S (1985). The Satisfaction With Life Scale. J Pers Assess, 49, 71–75. [DOI] [PubMed] [Google Scholar]
- Djukanovic I, Sorjonen K and Peterson U (2015). Association between depressive symptoms and age, sex, loneliness and treatment among older people in Sweden. Aging Ment Health, 19, 560–568. [DOI] [PubMed] [Google Scholar]
- Dykstra PA (2009). Older adult loneliness: myths and realities. Eur J Ageing, 6, 91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykstra PA, van Tilburg TG and de Jong Gierveld J (2005). Changes in Older Adult Loneliness: Results From a Seven-Year Longitudinal Study. Research on Aging, 27, 725–747. [Google Scholar]
- Eglit GML, Palmer BW, Martin AS, Tu X and Jeste DV (2018). Loneliness in schizophrenia: Construct clarification, measurement, and clinical relevance. PLoS One, 13, e0194021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst JM and Cacioppo JT (1999). Lonely hearts: Psychological perspectives on loneliness. Applied & Preventive Psychology, 8, 1–22. [Google Scholar]
- Erogul M, Singer G, McIntyre T and Stefanov DG (2014). Abridged mindfulness intervention to support wellness in first-year medical students. Teach Learn Med, 26, 350–356. [DOI] [PubMed] [Google Scholar]
- Fees BS, Martin P and Poon LW (1999). A model of loneliness in older adults. J Gerontol B Psychol Sci Soc Sci, 54, P231–239. [DOI] [PubMed] [Google Scholar]
- Fokkema T, De Jong Gierveld J and Dykstra PA (2012). Cross-national differences in older adult loneliness. J Psychol, 146, 201–228. [DOI] [PubMed] [Google Scholar]
- Hawkley LC and Cacioppo JT (2004). Stress and the aging immune system. Brain Behav Immun, 18, 114–119. [DOI] [PubMed] [Google Scholar]
- Hawkley LC and Cacioppo JT (2010). Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med, 40, 218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T and Stephenson D (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci, 10, 227–237. [DOI] [PubMed] [Google Scholar]
- Houtjes W, van Meijel B, van de Ven PM, Deeg D, van Tilburg T and Beekman A (2014). The impact of an unfavorable depression course on network size and loneliness in older people: a longitudinal study in the community. Int J Geriatr Psychiatry, 29, 1010–1017. [DOI] [PubMed] [Google Scholar]
- Jakobsson U and Hallberg IR (2005). Loneliness, fear, and quality of life among elderly in Sweden: a gender perspective. Aging Clin Exp Res, 17, 494–501. [DOI] [PubMed] [Google Scholar]
- Jeste D and Lee EE (2018). Emerging Empirical Science of Wisdom: Definition, Measurement, Neurobiology, Longevity, and Interventions. Harvard Review of Psychiatry, In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeste DV, Ardelt M, Blazer D, Kraemer HC, Vaillant G and Meeks TW (2010). Expert consensus on characteristics of wisdom: a Delphi method study. Gerontologist, 50, 668–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeste DV, et al. (2013). Association Between Older Age and More Successful Aging: Critical Role of Resilience and Depression. American Journal of Psychiatry, 170, 188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeste DV and Vahia IV (2008). Comparison of the conceptualization of wisdom in ancient Indian literature with modern views: focus on the Bhagavad Gita. Psychiatry, 71, 197–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph J, et al. (2015). Associations of high sensitivity C-reactive protein levels in schizophrenia and comparison groups. Schizophr Res, 168, 456–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylha M (2004). Old age and loneliness: cross-sectional and longitudinal analyses in the Tampere Longitudinal Study on Aging. Can J Aging, 23, 157–168. [DOI] [PubMed] [Google Scholar]
- Kharicha K, Manthorpe J, Iliffe S, Davies N and Walters K (2018). Strategies employed by older people to manage loneliness: systematic review of qualitative studies and model development. Int Psychogeriatr, 1–15. [DOI] [PubMed] [Google Scholar]
- Kong X, et al. (2015). Neuroticism and extraversion mediate the association between loneliness and the dorsolateral prefrontal cortex. Exp Brain Res, 233, 157–164. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL and Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EE, et al. (2016a). Elevated plasma F2-isoprostane levels in schizophrenia. Schizophr Res, 176, 320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EE, Hong S, Martin AS, Eyler LT and Jeste DV (2016b). Inflammation in Schizophrenia: Cytokine Levels and Their Relationships to Demographic and Clinical Variables. Am J Geriatr Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EE, Martin AS, Tu X, Palmer BW and Jeste DV (2018). Childhood Adversity and Schizophrenia: The Protective Role of Resilience in Mental and Physical Health and Metabolic Markers. J Clin Psychiatry, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann M and Hawkley LC (2016). Age differences in loneliness from late adolescence to oldest old age. Dev Psychol, 52, 943–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor J (2017). This former surgeon general says there’s a ‘loneliness epidemic’ and work is partly to blame. Washington Post. [Google Scholar]
- Meeks TW and Jeste DV (2009). Neurobiology of wisdom: a literature overview. Arch Gen Psychiatry, 66, 355–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich S, Wang SS, Hawkins K and Yeh CS (2015). The Impact of Loneliness on Quality of Life and Patient Satisfaction Among Older, Sicker Adults. Gerontol Geriatr Med, 1, 2333721415582119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers L and Palmarini N (2017). Loneliness: Findings from IBM’s Institute for Business Value 2017 Study on Loneliness in the Aging Population. Public Policy & Aging Report, 27, 158–159. [Google Scholar]
- Nicolaisen M and Thorsen K (2014a). Loneliness among men and women--a five-year follow-up study. Aging Ment Health, 18, 194–206. [DOI] [PubMed] [Google Scholar]
- Nicolaisen M and Thorsen K (2014b). Who are lonely? Loneliness in different age groups (18–81 years old), using two measures of loneliness. Int J Aging Hum Dev, 78, 229–257. [DOI] [PubMed] [Google Scholar]
- Penninx BW, van Tilburg T, Kriegsman DM, Deeg DJ, Boeke AJ and van Eijk JT (1997). Effects of social support and personal coping resources on mortality in older age: the Longitudinal Aging Study Amsterdam. Am J Epidemiol, 146, 510–519. [DOI] [PubMed] [Google Scholar]
- Perlman D and Peplau LA (1984). Loneliness reserach: A Survey of Empirical Findings In Peplau LA and Goldston SE (Eds.) Preventing the harmful consequences of severe and persistent loneliness Washington, D.C.: US Government Printing Office. [Google Scholar]
- Pinquart M and Sorensen S (2001). Gender differences in self-concept and psychological well-being in old age: a meta-analysis. J Gerontol B Psychol Sci Soc Sci, 56, P195–213. [DOI] [PubMed] [Google Scholar]
- Radloff L (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements, 385–401. [Google Scholar]
- Rokach A (2000). Loneliness and the life cycle. Psychol Rep, 86, 629–642. [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess, 66, 20–40. [DOI] [PubMed] [Google Scholar]
- Samuelsson G, Andersson L and Hagberg B (1998). Loneliness in relation to social, psychological and medical variables over a 13-year period: A study of the elderly in a Swedish rural district.
- Scheier MF, Carver CS and Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol, 67, 1063–1078. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, et al. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, 59 Suppl 20, 22–33;quiz 34–57. [PubMed] [Google Scholar]
- Simon MA, Chang ES, Zhang M, Ruan J and Dong X (2014). The prevalence of loneliness among U.S. Chinese older adults. J Aging Health, 26, 1172–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer MB, et al. (2003). Spirituality, depression, and loneliness among Jewish seniors residing in New York City. J Pastoral Care Counsel, 57, 305–318. [DOI] [PubMed] [Google Scholar]
- Tabue Teguo M, et al. (2016). Feelings of Loneliness and Living Alone as Predictors of Mortality in the Elderly: The PAQUID Study. Psychosom Med, 78, 904–909. [DOI] [PubMed] [Google Scholar]
- Theeke LA (2009). Predictors of loneliness in U.S. adults over age sixty-five. Arch Psychiatr Nurs, 23, 387–396. [DOI] [PubMed] [Google Scholar]
- Theeke LA and Mallow J (2013). Loneliness and quality of life in chronically ill rural older adults. Am J Nurs, 113, 28–37; quiz 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas ML, et al. (2017). A new scale for assessing wisdom based on common domains and a neurobiological model: The San Diego Wisdom Scale (SD-WISE). J Psychiatr Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas ML, et al. (2016). Paradoxical Trend for Improvement in Mental Health With Aging: A Community-Based Study of 1,546 Adults Aged 21–100 Years. J Clin Psychiatry, 77, e1019–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tijhuis MA, De Jong-Gierveld J, Feskens EJ and Kromhout D (1999). Changes in and factors related to loneliness in older men. The Zutphen Elderly Study. Age Ageing, 28, 491–495. [DOI] [PubMed] [Google Scholar]
- Tornas S, Lovstad M, Solbakk AK, Schanke AK and Stubberud J (2016). Goal Management Training Combined With External Cuing as a Means to Improve Emotional Regulation, Psychological Functioning, and Quality of Life in Patients With Acquired Brain Injury: A Randomized Controlled Trial. Arch Phys Med Rehabil, 97, 1841–1852.e1843. [DOI] [PubMed] [Google Scholar]
- Tornstam L (1992). Loneliness in marriage. Journal of Social and Personal Relationships, 9, 197–217. [Google Scholar]
- van Beljouw IM, et al. (2014). “Being all alone makes me sad”: loneliness in older adults with depressive symptoms. Int Psychogeriatr, 1–11. [DOI] [PubMed] [Google Scholar]
- van Roekel E, Verhagen M, Engels R, Scholte RHJ, Cacioppo S and Cacioppo JT (2016). Trait and State Levels of Loneliness in Early and Late Adolescents: Examining the Differential Reactivity Hypothesis. J Clin Child Adolesc Psychol, 1–12. [DOI] [PubMed] [Google Scholar]
- Victor CR and Bowling A (2012). A longitudinal analysis of loneliness among older people in Great Britain. J Psychol, 146, 313–331. [DOI] [PubMed] [Google Scholar]
- Victor CR and Yang K (2012). The prevalence of loneliness among adults: a case study of the United Kingdom. J Psychol, 146, 85–104. [DOI] [PubMed] [Google Scholar]
- Wang H, et al. (2017). Inconsistency Between Univariate and Multiple Logistic Regressions. Shanghai Arch Psychiatry, 29, 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE Jr. and Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care, 30, 473–483. [PubMed] [Google Scholar]
- Wilson C and Moulton B (2010). Loneliness among Older Adults: A National Survey of Adults 45+. Washington, D.C.: AARP. [Google Scholar]
- Yan Z, Yang X, Wang L, Zhao Y and Yu L (2014). Social change and birth cohort increase in loneliness among Chinese older adults: a cross-temporal meta-analysis, 1995–2011. Int Psychogeriatr, 26, 1773–1781. [DOI] [PubMed] [Google Scholar]
- Yu J, Lam CL and Lee TM (2016). Perceived loneliness among older adults with mild cognitive impairment. Int Psychogeriatr, 28, 1681–1685. [DOI] [PubMed] [Google Scholar]
- Zebhauser A, et al. (2014). How much does it hurt to be lonely? Mental and physical differences between older men and women in the KORA-Age Study. Int J Geriatr Psychiatry, 29, 245–252. [DOI] [PubMed] [Google Scholar]