Introduction
Intravascular lymphoma is a rare type of non-Hodgkin lymphoma and is characterized by a malignant proliferation of lymphocytes inside the lumen of blood vessels.1 Intravascular lymphoma is primarily an extranodal lymphoma, with skin and central nervous system reported as the most affected sites.2 Most cases (approximately 90%) consist of B-cell origin, but T and natural killer (NK) cell lineages have also been reported.3 Intravascular NK/T-cell lymphoma is typically related to the Epstein-Barr virus (EBV), expression of cytotoxic markers, and an aggressive course with an adverse prognosis.2 Cutaneous intravascular NK/T-cell lymphoma can be difficult to differentiate, both clinically and immunohistologically, from other cutaneous lymphomas, such as intravascular cutaneous anaplastic large cell lymphoma, extranodal NK/T-cell lymphoma (nasal type), or blastic plasmacytoid dendritic cell neoplasm.4, 5 Within the cutaneous intravascular NK/T-cell lymphomas, most reported cases are of NK cell phenotype with a constant relation to EBV, and most patients die within 6 months.2, 6 Only sporadic cases with a (NK-like) T-cell phenotype are described, with a variable immunophenotype and disease course.2, 7, 8 We describe the first case, to our knowledge, of a cutaneous EBV− intravascular cytotoxic CD4+ T-cell lymphoma, with a seemingly indolent disease course.
Case report
An 87-year-old woman presented to our dermatology clinic with progressive, partly infiltrated, asymptomatic plaques with purpuric centers and telangiectases of 2 months' duration, mainly located on the trunk (Fig 1). A biopsy from the abdomen found a dermal infiltrate of large atypical lymphocytes located in the blood vessels. The atypical cells were confined to the vessel lumen and confirmed by endothelial CD34 staining. The intravascular lymphocytes expressed CD2, CD3, CD4, TIA-1, granzyme-B, and CD56, and showed a proliferation rate of more than 90% (Fig 2). T-cell receptor (TCR) rearrangements were positive for TCR-β (TCRb), and negative for TCR-γ. The atypical lymphocytes were negative for CD5, CD7, CD8, CD123, TDT, CD30, PAX-5, and CD20. EBV-encoded RNA (EBER) in situ hybridization was negative. Staging was performed with blood examination and positron emission tomography–computed tomography and showed no signs of extracutaneous involvement or active EBV infection. A primary cutaneous EBV− intravascular cytotoxic CD4+ T-cell lymphoma was diagnosed. Considering age and condition, the patient was not eligible for intensive systemic chemotherapy and, in cooperation with the department of radiotherapy, treatment was initiated with adjusted total skin irradiation restricted to the trunk. Considering the assumed aggressive nature of the disease, a relatively high palliative dose was used of 21 Gy in 12 fractions of 1.75 Gy, 2 times per week with 4 MeV electron beam. A complete response was observed; however, the patient relapsed after 2 months. Comparable to the initial presentation, multiple characteristic plaques were located mainly on the trunk. Because of the rapid relapse after radiotherapy and the impaired physical condition of the patient, prednisone, 10 mg/d, was administered with a partial response (>50% disappearance of lesions). After 12 months of follow-up, a second positron emission tomography scan and blood examination found no signs of extracutaneous disease, and patient was still alive with stable disease. However, the patient ultimately died 2 months later of cardiac failure (unrelated to disease).
Fig 1.
Progressive, partly infiltrated, asymptomatic plaques with purpuric center and telangiectasia, mainly located on the trunk.
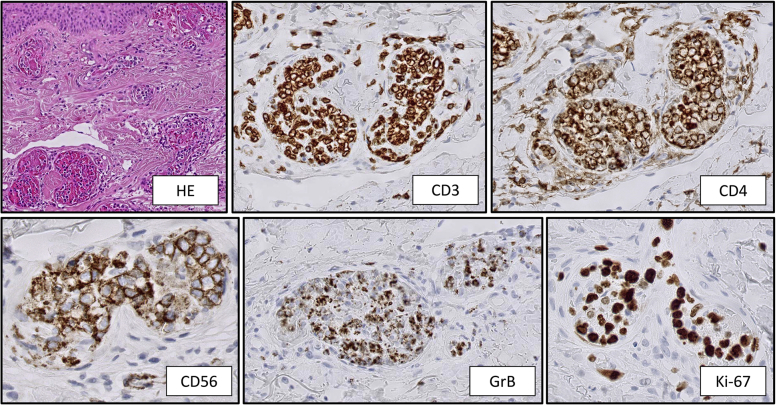
Fig 2.
The atypical cells are confined to the vessel lumen. The intravascular lymphocytes express CD3, CD4, CD56, granzyme-B and Ki-67 greater than 90%.
Discussion
Intravascular lymphoma, especially of NK/T-cell origin, is an extremely rare disease. Intravascular NK/T-cell lymphoma is usually primarily located in the skin, associated with EBV infection, a cytotoxic profile, and an aggressive disease course. Cutaneous intravascular NK/T-cell lymphoma can further be differentiated in intravascular NK-cell lymphoma and intravascular (NK-like) T-cell lymphoma. Most (cutaneous) intravascular NK/T-cell lymphomas reported in literature are CD3+, CD4−, CD56+, TIA-1+ and EBER+ and suggest a NK-cell origin. T-cell receptor genes are not rearranged in true NK cells. Our current case showed expression of T-cell markers (CD2, CD3, CD4) and demonstrated TCRb rearrangements, which favors a T-cell origin. Besides the extremely rare intravascular T-cell phenotype, other peculiar findings are negativity for EBER/EBV and positivity for CD4 combined with a cytotoxic profile (CD56, TIA-1, granzyme-B).7, 9 This combination of an intravascular T-cell lymphoma with NK-cell characteristics can imply an NK/T-cell origin.10 NK/T cells express or lack CD4 and CD8 and share features with NK cells such as CD56 expression and granzyme production and are important regulators of the immune response. We excluded blastic plasmacytoid dendritic cell neoplasm (intravascular distribution, CD123−, TCRb+), cutaneous anaplastic large T-cell lymphoma (CD30−, no blasts), and extranodal NK/T-cell lymphoma (nasal type) (EBER−, CD4+, TCRb+). In literature, only sporadic cases of cutaneous intravascular (cytotoxic) T-cell lymphomas have been described (Table I). Most patients were of older age (median age, 75; range, 23-87) and presented with purpuric plaques on the trunk. Of the patients with available data, 4 of 7 were EBER+, 6 of 7 expressed cytotoxic markers, 4 of 5 were treated with systemic chemotherapy, and 5 of 8 died of disease.2, 6, 8, 9, 11, 12, 13 Intravascular NK/T-cell lymphoma is extremely rare and usually associated with a poor prognosis. We report a new case of a cutaneous EBV− intravascular cytotoxic CD4+ (NK-like) T-cell lymphoma with an unusual phenotype and an indolent disease course.
Table I.
Characteristics of cutaneous (cytotoxic) intravascular T-cell lymphomas reported in the literature∗
| Case no. | Age | Gender | Type skin lesions | Immunophenotype/molecular analysis | Treatment | Status last follow up (mo)† |
|---|---|---|---|---|---|---|
| 1. Cerroni et al2 | 87 | M | Reddish-brownish lesions on the trunk | CD3+, CD4−, CD8−, TIA−, GrB− CD30−, CD56−, EBER+, PCR TCR+ | Died before treatment | D+ (0) |
| 2. Alegria et al6 | 81 | M | Purpuric plaques trunk | CD3+, CD4−, CD8−, GrB+, CD30+, CD56−, EBER+, PCR TCR+ | Died before treatment | D+ (0) |
| 3. Gleason et al8 | 62 | M | Plaques on medial calves | CD3+, CD4−, CD8−, TIA+, GrB+, CD30−, CD56+, EBER−, PCR TCR+, | Chemotherapy | A+ (8) |
| 4. Martinez-Escala et al9 | 67 | M | Purpuric patches on chest and abdomen | CD3+, CD4−, CD8−, TIA+, GrB+, CD56−, EBER−, PCR TCR+, | Chemotherapy and stem cell transplantation | Ao (6) |
| 5. Okonkwo and Jaffe11 | 51 | F | Plaques legs | CD3+, CD8+, GrB+, TIA+, CD56−, EBER+, TCR PCR+ | — | — |
| 6. Sepp et al12 | 81 | F | Hemorrhagic nodules trunk, face and extremities | CD3+, CD4+, CD8+ | Died before treatment | D+ (6) |
| 7. Sepp et al12 | 75 | F | Nodules upper legs | CD4+, CD8−/+, CD30−/+, Southern blot TCR+ | Chemotherapy | D+ (18) |
| 8. Jang et al13 | 23 | F | Erythematous patches with fine red telangiectasias on trunk and extremities | CD3+, CD4−, CD8+, TIA+, GrB+, CD30−, CD56−, EBER+, PCR TCR− | Chemotherapy | D+ (15) |
| 9. Current case | 87 | F | Plaques trunk | CD3+, CD4+, CD8−, TIA+, GrB+, CD30−, CD56+, EBER−, PCR TCR+ | RT, prednisone | Do (14) |
PCR, Polymerase chain reaction.
With exclusion of intravascular cutaneous anaplastic large cell lymphoma.
A+, alive with disease; Do, died of unrelated disease; D+, died of lymphoma.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Pfleger L., Tappeiner J. [On the recognition of systematized endotheliomatosis of the cutaneous blood vessels (reticuloendotheliosis?] Hautarzt. 1959;10:359–363. [PubMed] [Google Scholar]; Pfleger L, Tappeiner J. [On the recognition of systematized endotheliomatosis of the cutaneous blood vessels (reticuloendotheliosis?]. Hautarzt. 1959;10:359-363. [PubMed]
- 2.Cerroni L., Massone C., Kutzner H., Mentzel T., Umbert P., Kerl H. Intravascular large T-cell or NK-cell lymphoma: a rare variant of intravascular large cell lymphoma with frequent cytotoxic phenotype and association with Epstein-Barr virus infection. Am J Surg Pathol. 2008;32(6):891–898. doi: 10.1097/PAS.0b013e31815d29c9. [DOI] [PubMed] [Google Scholar]; Cerroni L, Massone C, Kutzner H, Mentzel T, Umbert P, Kerl H. Intravascular large T-cell or NK-cell lymphoma: a rare variant of intravascular large cell lymphoma with frequent cytotoxic phenotype and association with Epstein-Barr virus infection. The Am J Surg Pathol. 2008;32(6):891-898. [DOI] [PubMed]
- 3.Wu H., Said J.W., Ames E.D. First reported cases of intravascular large cell lymphoma of the NK cell type: clinical, histologic, immunophenotypic, and molecular features. Am J Clin Pathol. 2005;123(4):603–611. doi: 10.1309/X597-G3QM-XAFB-CM5V. [DOI] [PubMed] [Google Scholar]; Wu H, Said JW, Ames ED, Chen C, McWhorter V, Chen P, et al. First reported cases of intravascular large cell lymphoma of the NK cell type: clinical, histologic, immunophenotypic, and molecular features. Am J Clin Pathol. 2005;123(4):603-611. [DOI] [PubMed]
- 4.Santucci M., Pimpinelli N., Massi D. Cytotoxic/natural killer cell cutaneous lymphomas. Report of EORTC Cutaneous Lymphoma Task Force Workshop. Cancer. 2003;97(3):610–627. doi: 10.1002/cncr.11107. [DOI] [PubMed] [Google Scholar]; Santucci M, Pimpinelli N, Massi D, Kadin ME, Meijer CJ, Muller-Hermelink HK, et al. Cytotoxic/natural killer cell cutaneous lymphomas. Report of EORTC Cutaneous Lymphoma Task Force Workshop. Cancer. 2003;97(3):610-627. [DOI] [PubMed]
- 5.Assaf C., Gellrich S., Whittaker S. CD56-positive haematological neoplasms of the skin: a multicentre study of the Cutaneous Lymphoma Project Group of the European Organisation for Research and Treatment of Cancer. J Clin Pathol. 2007;60(9):981–989. doi: 10.1136/jcp.2006.042135. [DOI] [PMC free article] [PubMed] [Google Scholar]; Assaf C, Gellrich S, Whittaker S, Robson A, Cerroni L, Massone C, et al. CD56-positive haematological neoplasms of the skin: a multicentre study of the Cutaneous Lymphoma Project Group of the European Organisation for Research and Treatment of Cancer. J Clin Pathol. 2007;60(9):981-989. [DOI] [PMC free article] [PubMed]
- 6.Alegria-Landa V., Manzarbeitia F., Salvatierra Calderon M.G., Requena L., Rodriguez-Pinilla S.M. Cutaneous intravascular natural killer/T cell lymphoma with peculiar immunophenotype. Histopathology. 2017;71(6):994–1002. doi: 10.1111/his.13332. [DOI] [PubMed] [Google Scholar]; Alegria-Landa V, Manzarbeitia F, Salvatierra Calderon MG, Requena L, Rodriguez-Pinilla SM. Cutaneous intravascular natural killer/T cell lymphoma with peculiar immunophenotype. Histopathology. 2017;71(6):994-1002. [DOI] [PubMed]
- 7.Deetz C.O., Gilbertson K.G., 2nd, Anadkat M.J., Dehner L.P., Lu D. A rare case of intravascular large T-cell lymphoma with an unusual T helper phenotype. Am J Dermatopathol. 2011;33(8):e99–e102. doi: 10.1097/DAD.0b013e318221bc25. [DOI] [PubMed] [Google Scholar]; Deetz CO, Gilbertson KG, 2nd, Anadkat MJ, Dehner LP, Lu D. A rare case of intravascular large T-cell lymphoma with an unusual T helper phenotype. Am J Dermatopathol. 2011;33(8):e99-102. [DOI] [PubMed]
- 8.Gleason B.C., Brinster N.K., Granter S.R., Pinkus G.S., Lindeman N.I., Miller D.M. Intravascular cytotoxic T-cell lymphoma: a case report and review of the literature. J Am Acad Dermatol. 2008;58(2):290–294. doi: 10.1016/j.jaad.2006.12.022. [DOI] [PubMed] [Google Scholar]; Gleason BC, Brinster NK, Granter SR, Pinkus GS, Lindeman NI, Miller DM. Intravascular cytotoxic T-cell lymphoma: a case report and review of the literature. J Am Acad Dermatol. 2008;58(2):290-294. [DOI] [PubMed]
- 9.Martinez-Escala M.E., Guggina L.M., Cotliar J., Winter J.N., Guitart J. Cutaneous involvement in a case of intravascular T-cell lymphoma with a gammadelta phenotype. Am J Dermatopathol. 2016;38(2):e27–e29. doi: 10.1097/DAD.0000000000000383. [DOI] [PubMed] [Google Scholar]; Martinez-Escala ME, Guggina LM, Cotliar J, Winter JN, Guitart J. Cutaneous involvement in a case of intravascular T-cell lymphoma with a gammadelta phenotype. Am J Dermatopathol. 2016;38(2):e27-e29. [DOI] [PubMed]
- 10.Godfrey D.I., MacDonald H.R., Kronenberg M., Smyth M.J., Van Kaer L. NKT cells: what's in a name? Nat Rev Immunol. 2004;4(3):231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]; Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. NKT cells: what's in a name? Nat Rev Immunol. 2004;4(3):231-237. [DOI] [PubMed]
- 11.Okonkwo L., Jaffe E.S. Intravascular large cell lymphoma of NK/T-cell type, EBV positive. Blood. 2017;130(6):837. doi: 10.1182/blood-2017-05-785857. [DOI] [PMC free article] [PubMed] [Google Scholar]; Okonkwo L, Jaffe ES. Intravascular large cell lymphoma of NK/T-cell type, EBV positive. Blood. 2017;130(6):837. [DOI] [PMC free article] [PubMed]
- 12.Sepp N., Schuler G., Romani N. “Intravascular lymphomatosis” (angioendotheliomatosis): evidence for a T-cell origin in two cases. Hum Pathol. 1990;21(10):1051–1058. doi: 10.1016/0046-8177(90)90255-4. [DOI] [PubMed] [Google Scholar]; Sepp N, Schuler G, Romani N, Geissler D, Gattringer C, Burg G, et al. "Intravascular lymphomatosis" (angioendotheliomatosis): evidence for a T-cell origin in two cases. Human pathology. 1990;21(10):1051-1058. [DOI] [PubMed]
- 13.Jang Y.H., Lee S.J., Choi Y.H. Intravascular cytotoxic T-cell lymphoma in a young immunocompetent woman. Ann Dermatol. 2014;26(4):496–500. doi: 10.5021/ad.2014.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jang YH, Lee SJ, Choi YH, Lee WJ, Kim DW, Kim J, et al. Intravascular cytotoxic T-cell lymphoma in a young immunocompetent woman. Ann Dermatol. 2014;26(4):496-500. [DOI] [PMC free article] [PubMed]