Introduction
Oral isotretinoin, an isomer of retinoic acid, has been used for more than 35 years for the treatment of severe nodular acne. It is also indicated for the treatment of moderate acne that is treatment resistant or for the management of acne that is producing physical scarring or psychological distress.1 Adverse events are well known and frequently dermatologic in nature, including exfoliative cheilitis, diffuse xerosis, delayed wound healing, acne fulminans, or paronychia. Adverse events are mostly of mild intensity and do not generally require dose adjustment. The other main toxicities include depression/mood changes, bone demineralization, transaminitis, dyslipidemia and teratogenic effects.1
Here we report a young female patient who progressively had diffuse painful oral aphthous-like lesions secondary to a severe vitamin B12 deficiency induced by long-term isotretinoin therapy that required discontinuation of the treatment.
Case report
A 17-year-old female patient with no medical history except acne was referred to the dermatologic department for severe recurrent oral ulcers that had progressed for 4 months associated with physical deterioration and fatigue. She had been treated with oral isotretinoin for 7 months (3.6 g cumulative dose of isotretinoin for 50 kg). Two years before, she received a first course of isotretinoin for 11 months (6 g cumulative dose). Oral examination found multiple small well-defined ulcers mimicking aphthous stomatitis of the herpetiform type, involving both keratinized and nonkeratinized mucosae (Fig 1, A-C). A smooth red plaque of the border and the dorsum of the tongue was also present, suggestive of Hunter glossitis. Bacterial/fungal swab cultures and in situ polymerase chain reaction screening for herpes simplex virus 1-2, varicella zoster virus, cytomegalovirus, and coxsackievirus were all negative. Biological assessment, which was rapidly required, found a macrocytic anemia (7 g/dL hemoglobin; mean cell volume of 115μ3) associated with transaminitis (3-5 times the upper limit of normal), high lactate dehydrogenase level (>4000 IU/L), thrombocytopenia (65 g/L), very low vitamin B12 level (not measurable), and vitamin B9 deficiency (3 ng/mL; normal range, 5-15 ng/mL). Immunologic tests with specific autoantibodies (anti-intrinsic factor, antiendomysium, antiparietal cell, antitransglutaminase antibodies) were normal, and digestive endoscopic screening (esophagogastroduodenoscopy) with biopsy did not find any antral atrophic gastritis or atrophy of duodenal villosity. The Schilling test and a barium small bowel meal did not reveal any vitamin B12 malabsorption. Withdrawal of oral isotretinoin combined with oral vitamin B12 (1 ampulla [1 mg/2 mL]/d, twice a day) and vitamin B9 (5 mg/d, 3 times per day) supplementation led to complete healing of the oral ulcers in 2 weeks (Fig 2, A and B). Hemoglobin and vitamin B12 levels were normal 1 month later. At her 8-month follow-up, neither the oral lesions (Fig 2, C) nor the macrocytic anemia or vitamin deficiency had recurred, despite discontinuation of vitamin B12 supplementation after 2 months of treatment.
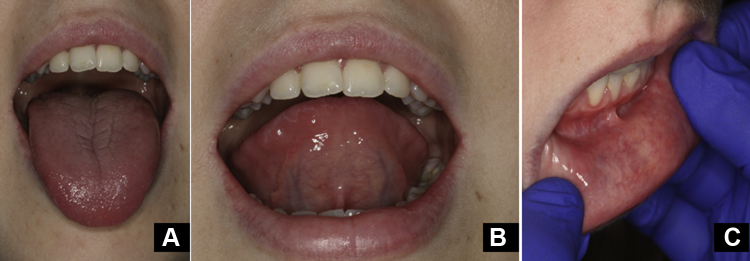
Fig 1.
Multiple small well-limited ulcers mimicking aphthous stomatitis of the herpetiform type on the dorsum of the tongue (A) with erythematous aspect of the border, the ventral side of the tongue (B), and the labial mucosa (C) at baseline.
Fig 2.
Oral ulcers on the dorsum (A) and the ventral aspect (B) of the tongue have disappeared 2 weeks after vitamin B12 supplementation and discontinuation of systemic isotretinoin. Labial mucosa (C) 8 months later, without any recurrence.
Discussion
Oral mucosal changes including glossitis and aphthous-like lesions represent a cardinal symptom of vitamin B12 deficiency and may represent the earliest clinical sign of B12 deficiency, as in our patient. To date, the occurrence of mucosal lesions in the context of vitamin B12 and folate deficiencies has been reported during treatment by isotretinoin in only 1 patient with a perianal mucosal involvement together with nonulcerative erythema of the oral mucosa.2 The literature includes few studies that evaluated the effect of isotretinoin therapy on blood levels of vitamin B12, vitamin B9, holotranscobalamin, hemoglobin, and homocysteine.2, 3, 4, 5, 6, 7, 8, 9 Despite conflicting results, we speculate that long-term or high-dose isotretinoin therapy tends to decrease folic acid and vitamin B12 levels.3, 5 Indeed, 2 studies in particular reported a decrease in vitamin B12 and folate levels in 2 large cohorts of patients treated by isotretinoin for 6 and 4 months, respectively.3, 4 Karadag et al4 also noted an associated hyperhomocysteinemia. However, the mechanisms of B12 and folate deficiency during isotretinoin treatment remain unclear.2, 3, 4, 5, 6, 7, 8, 9 Isotretinoin could interact with the transport system for vitamin B12 absorption via enterocytes and interaction with the metabolism of holotranscobalamin.4 Moreover, the decrease in the levels of vitamin B12 and folate alters the methylation pathway and induces high blood homocysteine levels.4 Finally, hyperhomocysteinemia may result in an elevated frequency of thrombosis in the feeding arterioles that supply the oral epithelial cells and may lead to the formation of oral ulcers.10
The progressive development of glossitis and oral ulcers during the second cycle of isotretinoin therapy, together with the absence of evidence suggestive of pernicious anemia or inflammatory bowel disease and the lack of recurrence after treatment discontinuation, strongly suggest that the development of vitamin B12/folate deficiency in our patient was strictly related to isotretinoin therapy. Cumulative doses of isotretinoin may play a role in the occurrence of mucosal lesions, especially because a short course of isotretinoin may not be associated with vitamin B12 or folate deficiency.6, 8, 9 To our knowledge, this case represents the first clinical characterization of severe oral lesions related to vitamin B12 deficiency induced by systemic isotretinoin therapy. Clinicians should be aware that isotretinoin therapy can induce vitamin B12 and folic acid deficiencies and that secondary oral mucosal changes can occur in this context.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Zaenglein A.L., Pathy A.L., Schlosser B.J. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–973. doi: 10.1016/j.jaad.2015.12.037. [DOI] [PubMed] [Google Scholar]; Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016; 74:945-973. [DOI] [PubMed]
- 2.Jasim Z.F., McKenna K.E. Vitamin B12 and folate deficiency anaemia associated with isotretinoin treatment for acne. Clin Exp Dermatol. 2006;31:599. doi: 10.1111/j.1365-2230.2006.02144.x. [DOI] [PubMed] [Google Scholar]; Jasim ZF, McKenna KE. Vitamin B12 and folate deficiency anaemia associated with isotretinoin treatment for acne. Clin Exp Dermatol. 2006; 31:599. [DOI] [PubMed]
- 3.Gökalp H., Bulur I., Gürer M. Decreased vitamin B12 and folic acid concentrations in acne patients after isotretinoin therapy: a controlled study. Indian J Dermatol. 2014;59:630. doi: 10.4103/0019-5154.143533. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gokalp H, Bulur I, Gurer M. Decreased vitamin B12 and folic acid concentrations in acne patients after isotretinoin therapy: a controlled study. Indian J Dermatol. 2014; 59:630. [DOI] [PMC free article] [PubMed]
- 4.Karadag A.S., Tutal E., Ertugrul D.T., Akin K.O. Effect of isotretinoin treatment on plasma holotranscobalamin, vitamin B12, folic acid, and homocysteine levels: non-controlled study. Int J Dermatol. 2011;50:1564–1569. doi: 10.1111/j.1365-4632.2011.05027.x. [DOI] [PubMed] [Google Scholar]; Karadag AS, Tutal E, Ertugrul DT, Akin KO. Effect of isotretinoin treatment on plasma holotranscobalamin, vitamin B12, folic acid, and homocysteine levels: non-controlled study. Int J Dermatol. 2011; 50:1564-1569. [DOI] [PubMed]
- 5.Ghiasi M., Mortazavi H., Jafari M. Efficacy of folic acid and vitamin B12 replacement therapies in the reduction of adverse effects of isotretinoin: a randomized controlled trial. Skinmed. 2018;16:239–245. [PubMed] [Google Scholar]; Ghiasi M, Mortazavi H, Jafari M. Efficacy of folic acid and vitamin B12 replacement therapies in the reduction of adverse effects of isotretinoin: a randomized controlled trial. Skinmed. 2018; 16:239-245. [PubMed]
- 6.Polat M., Lenk N., Bingöl S. Plasma homocysteine level is elevated in patients on isotretinoin therapy for cystic acne: a prospective controlled study. J Dermatolog Treat. 2008;19:229–232. doi: 10.1080/09546630701846079. [DOI] [PubMed] [Google Scholar]; Polat M, Lenk N, Bingol S, Oztaş P, Ilhan MN, Artuz F, et al. Plasma homocysteine level is elevated in patients on isotretinoin therapy for cystic acne: a prospective controlled study. J Dermatolog Treat. 2008; 19:229-232. [DOI] [PubMed]
- 7.Chanson A., Cardinault N., Rock E. Decreased plasma folate concentration in young and elderly healthy subjects after a short-term supplementation with isotretinoin. J Eur Acad Dermatol Venereol. 2008;22:94–100. doi: 10.1111/j.1468-3083.2007.02386.x. [DOI] [PubMed] [Google Scholar]; Chanson A, Cardinault N, Rock E, Martin JF, Souteyrand P, D'Incan M, et al. Decreased plasma folate concentration in young and elderly healthy subjects after a short-term supplementation with isotretinoin. J Eur Acad Dermatol Venereol. 2008; 22:94-100. [DOI] [PubMed]
- 8.Kamal M., Polat M. Effect of different doses of isotretinoin treatment on the levels of serum homocysteine, vitamin B 12 and folic acid in patients with acne vulgaris: a prospective controlled study. J Pak Med Assoc. 2015;65:950–953. [PubMed] [Google Scholar]; Kamal M, Polat M. Effect of different doses of isotretinoin treatment on the levels of serum homocysteine, vitamin B 12 and folic acid in patients with acne vulgaris: a prospective controlled study. J Pak Med Assoc. 2015; 65:950-953. [PubMed]
- 9.Roodsari M.R., Akbari M.R., Sarrafi-rad N., Saeedi M., Gheisari M., Kavand S. The effect of isotretinoin treatment on plasma homocysteine levels in acne vulgaris. Clin Exp Dermatol. 2010;35:624–626. doi: 10.1111/j.1365-2230.2010.03778.x. [DOI] [PubMed] [Google Scholar]; Roodsari MR, Akbari MR, Sarrafi-rad N, Saeedi M, Gheisari M, Kavand S. The effect of isotretinoin treatment on plasma homocysteine levels in acne vulgaris. Clin Exp Dermatol. 2010; 35:624-626. [DOI] [PubMed]
- 10.Chiang C.P., Yu-Fong Chang J., Wang Y.P., Wu Y.H., Wu Y.C., Sun A. Recurrent aphthous stomatitis - etiology, serum autoantibodies, anemia, hematinic deficiencies, and management. J Formos Med Assoc. 2018 doi: 10.1016/j.jfma.2018.10.023. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]; Chiang CP, Yu-Fong Chang J, Wang YP, Wu YH, Wu YC, Sun A. Recurrent aphthous stomatitis - etiology, serum autoantibodies, anemia, hematinic deficiencies, and management. J Formos Med Assoc. 2018 Nov 14. [DOI] [PubMed]