Abstract
Recurrent painful ophthalmoplegic neuropathy is a form of cranial neuralgia and rare source of pediatric headache. We present 2 children who presented with headaches accompanied by visual symptoms including eye pain, blurry vision, and diplopia. MRI in both patients demonstrated enhancement of the cisternal segment of the oculomotor nerve in the affected side, correlating with the observed symptoms.
Keywords: Oculomotor nerve enhancement, Recurrent painful opthalmoplegic neuropathy
Introduction
Ophthalmoplegic neuropathy is a rare condition that is characterized by recurrent episodes of headaches and paresis of 1 or more ocular cranial nerves. There is an estimated annual incidence of 0.7 per million, but the exact etiology is unknown [1], [2], [3], [4]. Mydriasis and ptosis are common symptoms, as the oculomotor nerve is the most commonly affected. Symptoms typically begin in childhood with an average age of onset younger than 10 years, but symptoms can persist throughout adulthood. The symptoms often resolve completely within days to a few weeks following onset of an acute attack, but a small percentage of patients have permanent neurologic deficits [5], [6], [7]. Ophthalmoplegic migraine is commonly confused with migraine with visual aura, in which a patient has a migraine headache with associated transient visual phenomena [8]. Ophthalmoplegic migraine has been reclassified under cranial neuralgia in the International Classification of Headache Disorders. The diagnostic criteria described for this condition in the International Classification of Headache Disorders include unilateral headache and ipsilateral paresis of the third, fourth, or sixth cranial nerve. Orbital, parasellar, and posterior fossa lesions must be excluded as potential causes to qualify. Contrast-enhanced MRI can be utilized to identify oculomotor nerve palsies during the symptomatic period and upon resolution of symptoms [[9], [10]]. Presented here are 2 pediatric cases of pediatric ophthalmoplegic migraine with distinctive MRI findings.
Case report 1
The patient was a 15-year-old male with past medical history of seasonal allergies who initially presented to the emergency department complaining of 5 days of right eye redness, burning, and diplopia as well as right eye ptosis for 2 days. The patient also complained of continuous right sided periorbital headache and 1 episode of 102°F fever. A diagnosis of sinus infection was assigned, and the eye pain was attributed to this diagnosis. The patient was prescribed azithromycin as well as an oral antihistamine. A steroid injection was also administered. The patient was sent home from school 2 days later due to new onset ptosis of the right eye. He was then referred to an ophthalmologist who noted right eyelid ptosis, slightly diminished supraduction of the right eye, normal optic nerves bilaterally, and normal ocular pressure. The ophthalmologist diagnosed the patient with right orbital cellulitis and referred him to the emergency department for urgent IV antibiotics and further imaging.
The patient was afebrile upon presentation to the ED. He was administered empiric ceftriaxone and clindamycin for 2 days. On physical exam, the patient described blurry vision and vertical diplopia. His right eye pain exacerbated with upward eye movements. He also complained of ear fullness, a 1-week history of sinus congestion, and sudden onset of dizziness when he would sit up rapidly. The patient denied any weakness in the upper or lower extremities, paresthesia, difficulty walking, nausea, photophobia, or loss of vision. Additional laboratory testing including thyroid function tests, angiotensin converting enzyme levels, antinuclear antibody, C3/C4 levels, erythrocyte sedimentation rate, C-reactive protein levels, and ganglioside antibody panel were unremarkable. Regarding the infectious etiology assessment, the patient was only positive for Epstein-Barr virus nuclear antigen antibody indicative of a prior Epstein-Barr virus infection.
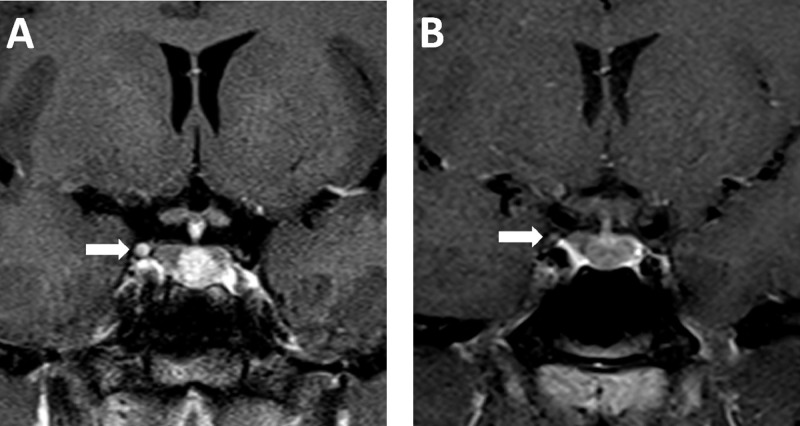
An initial head CT without contrast did not reveal any acute intracranial abnormalities. MRI of the brain and orbits with and without contrast demonstrated diffuse enlargement and enhancement of the third cranial nerve on the right (Fig. 1A). Cerebrospinal fluid analysis revealed a mildly elevated protein with normal cytology. As this raised concern for a Guillain-Barre variant affecting cranial nerves, intravenous immunoglobin therapy was initiated; however, the patient's extraocular movements continued to worsen, so high dose IV solumedrol was administered for 3 days which resulted in some clinical improvement. Electromyography was unremarkable. A Guillain-Barre etiology was then felt to be unlikely, and intravenous immunoglobin was stopped after 4 days. The patient was transitioned to oral prednisone.
Fig. 1.
15-year-old male with recurrent painful ophthalmolplegic neuropathy. Coronal T1-weighted image of the sella turcica with contrast at original presentation (A) and 2 months following steroid therapy (B).
The patient's symptoms continued to improve during the admission and resolved completely within a week after being discharged from the hospital. He did not have any residual vision problems including photosensitivity, changes in color vision, or diplopia. His follow-up ophthalmology evaluation was normal. MRI of brain and orbits with contrast 2 months after onset of symptoms revealed minimal residual enhancement of the proximal right oculomotor nerve (Fig 1B) with very mild relative enlargement of the right oculomotor nerve compared to the left.
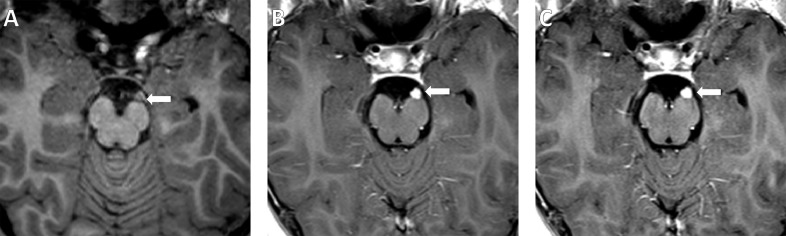
Fig. 2.
11-year-old male with recurrent painful ophthalmolplegic neuropathy. Axial T1-weighted image of the brain at the level of the proximal oculomotor nerve without contrast (A). Follow-up T1-weighted image with contrast (B) shows avid enhancement of the cisternal segment of the left oculomotor nerve (arrow). Recurrence was observed 1 year later with similar imaging findings (C).
Case report 2
The patient was an 11-year-old male who presented to the emergency department with a 3-day history of left eyelid swelling, nausea, vomiting, confusion, and headaches. He also had 1 episode of 103°F fever. The patient had experienced sharp stabbing left eye pain multiple times a day and monocular left blurry vision for several days. The physical exam was remarkable for left eye ptosis, diplopia, and eye pain with movements. His complete blood count, comprehensive metabolic panel, cerebrospinal fluid analysis, cryptococcal antigen, oligoclonal bands, IgG, and angiotensin converting enzyme levels were all unremarkable.
His family had also noticed that the patient would walk with his head flexed to better perceive the ground, as his left eye was nearly closed. His home medications included bismuth subsalicylate, acetaminophen, and pseudoephedrine which did not appear to alleviate his symptoms. According to a caregiver, he had experienced episodes of left eyelid swelling, headaches, nausea, vomiting, and vertiginous sensations intermittently in recent years. During these episodes, the patient seemed more somnolent and had decreased appetite. The patient would also experience light and noise sensitivity, nausea, vomiting, blurry vision, dizziness, occasional loss of memory, tearing of the eye or nose, left eye redness, ptosis, and irritation. These episodes usually lasted about a week at a time, were similar in presentation and course, and the symptoms would gradually go away with supportive treatment. A brain MRI without contrast showed vague enlargement of the left oculomotor nerve (Fig. 2A).
A follow-up MRI with contrast revealed isolated enhancement and enlargement of the cisternal segment of the left oculomotor nerve (Fig. 2B). He was administered topiramate with significant improvement in the severity of his headaches and oculomotor symptoms.
One year later, the patient presented to the ED due to 2 weeks of worsening nausea, vomiting, left temporal headache, and left ptosis as well as decreased appetite and 1 episode of 104°F fever. Since the prior admission, the patient had continued to experience daily left temporal headaches that were shorter in duration and less severe in intensity. Brain MRI with contrast revealed a similar appearance of the brain compared to the MRI obtained 1 year prior and was significant for enhancement along the proximal third cranial nerve on the left (Fig 2C). The patient's symptoms improved during the admission on topiramate therapy, and the headache had resolved on discharge.
Discussion
Ophthalmoplegic migraine in the pediatric population is a cranial neuralgia that is frequently associated with enhancement of the affected cranial nerve on contrast-enhanced MRI, most commonly the oculomotor nerve. The primary differential considerations for these MRI findings are oculomotor nerve schwannoma, carcinomatosis, granulomatosis, and inflammatory or infectious neuritis. The diagnosis is generally made clinically with the MRI serving as an important adjunct, as headache is not typically the primary symptom in these other disorders. It should be noted that this entity is distinct from migraine with aura, another disorder involving cephalgia with visual disturbances. In migraine with visual aura, there are transient visual disturbances including blind spots, flashes of light, and light sensitivity. Enhancement of the oculomotor nerve has not been reported in migraine with visual aura.
Improvement in enhancement of the affected cranial nerve can occur with concurrent resolution of the symptoms. Ophthalmoplegic migraine is likely underdiagnosed in the pediatric population without appropriate imaging since it shares common clinical features with other neurological diseases. This diagnosis should be considered among patients who present with recurrent ocular focal neurological deficits and/or severe headaches.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Doran M., Larner A.J. MRI findings in ophthalmoplegic migraine: nosological implications. J Neurol. 2004;251:100–101. doi: 10.1007/s00415-004-0219-4. [DOI] [PubMed] [Google Scholar]; Doran M., Larner A.J.MRI findings in ophthalmoplegic migraine: nosological implications. J Neurol2004;251:100–101. [DOI] [PubMed]
- 2.O'Hara M.A., Anderson R.T., Brown D. Magnetic resonance imaging in ophthalmoplegic migraine of children. J AAPOS. 2001;5:307–310. doi: 10.1067/mpa.2001.118670. [DOI] [PubMed] [Google Scholar]; O'Hara M.A., Anderson R.T., Brown D.Magnetic resonance imaging in ophthalmoplegic migraine of children. J AAPOS2001;5: 307–310. [DOI] [PubMed]
- 3.Bharucha D.X., Campbell T.B., Valenia I., Hardison H.H., Kothare S.V. MRI findings in pediatric ophthalmoplegic migraine: a case report and literature review. Pediatr Neurol. 2007;37(1):59–63. doi: 10.1016/j.pediatrneurol.2007.03.008. [DOI] [PubMed] [Google Scholar]; Bharucha D.X., Campbell T.B., Valenia I., Hardison H.H., Kothare S.V.MRI findings in pediatric ophthalmoplegic migraine: a case report and literature review. Pediatr Neurol. 2007;37(1):59–63. [DOI] [PubMed]
- 4.Gelfand A.A., Gelfand J.M., Prabakhar P., Goadsby P.J. Ophthalmoplegic ‘‘migraine’’ or recurrent ophthalmoplegic cranial neuropathy: new cases and a systematic review. J Child Neurol. 2012;27(6):759–766. doi: 10.1177/0883073811426502. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gelfand A.A., Gelfand J.M., Prabakhar P., Goadsby P.J.Ophthalmoplegic ‘‘migraine’’ or recurrent ophthalmoplegic cranial neuropathy: new cases and a systematic review. J Child Neurol. 2012;27(6):759–766. [DOI] [PMC free article] [PubMed]
- 5.McMillan H.J., Keene D.L., Jacob P., Humphreys P. Ophthalmoplegic migraine: inflammatory neuropathy with secondary migraine? Can J Neurol Sci. 2007;34(3):349–355. doi: 10.1017/s0317167100006818. [DOI] [PubMed] [Google Scholar]; McMillan H.J., Keene D.L., Jacob P., Humphreys P.Ophthalmoplegic migraine: inflammatory neuropathy with secondary migraine?Can J Neurol Sci. 2007;34(3):349–355. [DOI] [PubMed]
- 6.Ramelli G.P., Vella S., Lovblad K., Remonda L., Vassella F. Swelling of the third nerve in a child with transient oculomotor paresis: a possible ause of ophthalmoplegic migraine. Neuropediatrics. 2000;31:145–147. doi: 10.1055/s-2000-7532. [DOI] [PubMed] [Google Scholar]; Ramelli G.P., Vella S., Lovblad K., Remonda L., Vassella F.Swelling of the third nerve in a child with transient oculomotor paresis: a possible ause of ophthalmoplegic migraine. Neuropediatrics2000;31:145–147. [DOI] [PubMed]
- 7.Carlow T.J. Oculomotor ophthalmoplegic migraine: is it really migraine? J Neuroophthalmol. 2002;22(3):215–221. doi: 10.1097/00041327-200209000-00006. [DOI] [PubMed] [Google Scholar]; Carlow T.J.Oculomotor ophthalmoplegic migraine: is it really migraine?J Neuroophthalmol. 2002;22(3):215–221 [DOI] [PubMed]
- 8.Hansen S.L., Borelli-Moller L., Strange P., Nielsen B.M., Olesen J. Ophthalmoplegic migraine: diagnostic criteria, incidence of hospitalization and possible etiology. Acta Neurol Scand. 1990;81(1):54–60. doi: 10.1111/j.1600-0404.1990.tb00931.x. [DOI] [PubMed] [Google Scholar]; Hansen S.L., Borelli-Moller L., Strange P., Nielsen B.M., Olesen J.Ophthalmoplegic migraine: diagnostic criteria, incidence of hospitalization and possible etiology. Acta Neurol Scand. 1990; 81(1):54–60 [DOI] [PubMed]
- 9.Headache Classification Subcommittee of the International Headache Society The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl. 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]; Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl. 1): 9–160. [DOI] [PubMed]
- 10.Lane R., Davies P. Ophthalmoplegic migraine: the case for reclassification. Cephalalgia. 2010;30(6):655–661. doi: 10.1111/j.1468-2982.2009.01977.x. [DOI] [PubMed] [Google Scholar]; Lane R., Davies P.Ophthalmoplegic migraine: the case for reclassification. Cephalalgia. 2010;30(6):655–661. [DOI] [PubMed]