Abstract
Microscopic Thyroidectomy is not a new surgical technique but it is not explored much. The routine use of microscope in thyroid surgery can reduce the rate of nerve palsy and hypocalcemia. Nine cases were done exclusively with the microscope only and postoperative nerve palsy and hypocalcemia were noted. We have also discussed about optimum working distances and magnification for critical structures during thyroid surgery. No patient has any nerve palsy while one patient reported transient hypocalcemia. Recurrent laryngeal nerve could be identified at 2 × but optimal magnification for dissection of nerve should be 4 ×. We find this technique easy to adopt and critical structures can be identified and preserved easily with microscopic thyroidectomy then conventional and loupe technique. It is better to have standardized and optimum working distance and magnification during different steps of surgery. It is great teaching tool in view of its better illumination and magnification.
Keywords: Thyroid gland, Thyroidectomy
Introduction
Use of magnification in the Head and Neck surgeries is a routine practice presently. Since the description of Thyroid surgery in the “Principles of Surgery by E.T. Kocher”, numerous techniques and instruments have been used in the Thyroid surgeries. Robotic thyroidectomy is the latest addition in the management of patient with thyroid surgeries. However, from conventional to endoscopic and robotic methods, use of magnification is the cornerstone of all the modalities. Microscope is the versatile tool as far the magnification is considered for the surgery. The magnification can be changed from site to site, depending upon the surgeon requirement. The current study was conducted using microscope exclusively for thyroid surgery. We analysed our results retrospectively in terms of benefits and difficulties we faced and the patient outcomes. Microscopic technique for dealing with the thyroid tumour is not a new concept and several articles reported its usefulness in surgery but the problems faced while using microscope need further discussion.
Materials and Methods
Total of 9 patients were operated using microscope between September 2017 to March 2018. The exclusion criteria were patients with preoperative nerve palsy. For all the cases routine preoperative work up was done and all patients received single shot of preoperative antibiotics. For all the cases Leica F 20 M525 microscope was used and all cases were done by junior consultants under the supervision of senior consultant. All the surgical steps were done under microscope starting from the skin incision up to delivery of gland. Various observations were made regarding working distance, magnification, field diameter and desired magnification during different steps of surgery. All patients were postoperatively assessed for nerve injuries and for hypocalcemia.
Results
Total of 9 patients were operated out of which 6 were female and 3 were male (Table 1). The mean size of tumour in this study was 7 cm with largest being 11 cm and smallest being 4 cm in size. There were 2 patients with papillary carcinoma and one with hurthle neoplasm and all others were benign pathology. Surgeries performed were 3 total thyroidectomy, 5 hemithyroidectomy and 1 completion thyroidectomy was. The total of 13 recurrent and superior laryngeal nerves were exposed during surgeries. No patient developed postoperative nerve palsy. However, there was one patient who developed transient hypocalcaemia after surgery. Various observations were made regarding the working distance and optimum magnification at different steps of surgery (Table 2). We usually started with 1.3 × for tumours more then 8 cm and 2 × for tumours less then 8 cm. For skin, platysma and strap muscles the magnification up to 2 × has been used. In some cases, recurrent laryngeal nerve could be identified with 2 × and some cases require 4 × magnification, however once identified all dissection have done around 4 × magnification to preserve its vasa nervosum. The hilar vessels of parathyroid were of low calibre and required 4 × to 6 × magnification to identify the hilar vessels and to protect the vasculature.
Table 1.
Patient characteristics
| S. no | Age (years) | Sex | Tumour size (cm) | Pathology | Procedure | Postoperative nerve palsy | Postoperative hypocalcemia |
|---|---|---|---|---|---|---|---|
| 1 | 27 | M | 6 | Papillary carcinoma | Total thyroidectomy | Absent | Absent |
| 2 | 21 | F | 4 | Right colloid goitre | Right hemithyroidectomy | Absent | Absent |
| 3 | 40 | F | 10 | Colloid goitre | Total thyroidectomy | Absent | Transient |
| 4 | 27 | M | 6 | Left colloid goitre | Left hemithyroidectomy | Absent | Absent |
| 5 | 55 | M | 4 | Papillary carcinoma | Completion thyroidectomy | Absent | Absent |
| 6 | 52 | F | 8 | Left colloid goitre | Left hemithyroidectomy | Absent | Absent |
| 7 | 28 | F | 11 | Left colloid goitre | Left hemithyroidectomy | Absent | Absent |
| 8 | 48 | F | 9 | Colloid goitre | Total Thyroidectomy | Absent | Absent |
| 9 | 31 | F | 5 | Left Hurthle cell neoplasm | Left hemithyroidectomy | absent | absent |
Table 2.
Working adjustments
| Magnification | Working distance (mm) | Diameter visualised (cm) | Recommended area to work on |
|---|---|---|---|
| 1.3× | 410 | 14.7 | Skin, Platysma, strap muscles |
| 2× | 410 | 8 | Skin, Platysma, strap muscles |
| 3× | 410 | 5.8 | Skin, Platysma, strap muscles, Superior pole dissection |
| 4× | 410 | 4.4 | Superior pole and recurrent laryngeal nerve dissection, Inferior thyroid artery branches identification. |
| 5× | 410 | 3.5 | Parathyroid dissection |
Discussion
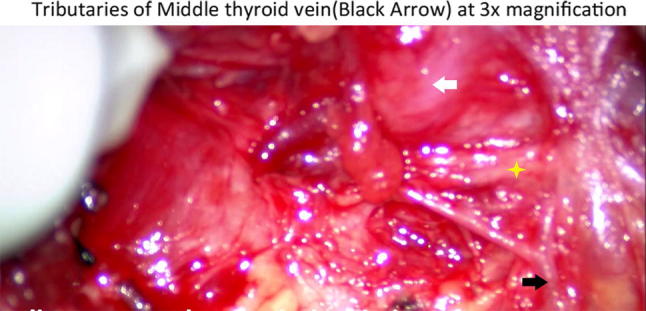
The first documented use of magnification for thyroid surgery was described in article dealing with recurrent laryngeal injuries by Lahey in 1938. He recommended use of Bereny binocular loupes and he was able to magnify the nerve by two and half times [1]. Recently in 2016, an article was published by Dorzai et al. where they have retrospectively analysed their 10 years’ experience using magnification. There were total of 738 patients included in their study and they showed remarkable result using magnification with just one patient developing transient nerve palsy after thyroid surgery [2]. The use of microscope is not new but preferring this technique over other modalities requires justification. In the era of robotic and endoscopic surgeries, where patients and surgeons both want hidden scar, use of microscope may not be so enthusiastic. Kim et al. presented their experience with 5000 gasless trans axillary thyroidectomy with the rate of Recurrent laryngeal nerve palsy was 0.4% [3]. Jinbeam Cho et al. presented their results in 105 endoscopic thyroidectomies with the rate of transient RLN palsy of 5/105 [4]. Both of the results are exciting; however, they were dealing with the mean tumour size of less than 1 cm in robotic surgeries and mean tumour size of less than 3 cm for Endoscopic surgeries. This is not the scenario in most of the developing countries, where thyroid diseases are not considered as a problems and thyroid masses are considered as the normal extension of body appendages. Our area is Sub Himalayan belt which is naturally deficient in Iodine and some of the areas are remote with no access for any healthcare facilities. The size of tumour in patients presenting to our OPD is just directly proportional to the ignorance of both people and the government. The minimum size included in our study was 4 cm, which was a young patient with papillary carcinoma and the maximum size of the tumour was 11 cm in size, with the mean size of 7 cm. The great variation in the size needs tailoring of approaches for the individual case. For small tumours robotic and endoscopies methods work fine and they provide adequate magnification for nerve identification. Robotic thyroidectomy provide 10 × magnification and it is easy to identify nerve using robotic technique [5]. RLN injury rate vary and from world centres of excellence, the reported rate is around 0.25–0.7% [6]. The large tumours pose challenge for identification of nerve and parathyroid glands and some surgeons prefer using medial to lateral approach for identification the nerve at its entry point. This technique provides good exposure to nerve without too much dissection and the landmark does not seem to change with large tumour. However, the extra laryngeal branching of the recurrent laryngeal nerve can pose the nerve at risk while using this approach. In all of our cases we have used lateral to medial dissection and we faced no problem in identifying the nerve or parathyroid even in tumours size of 10 cm. Right RLN nerve has been reported to be more difficult to identify then left side, but in our study we have exposed 5 nerves on right side and we have faced no difficulty using microscope to identify it [6]. The magnification provided by the microscope was so good that in some cases we were even able to identify the parasympathetic fibres which are carried by recurrent laryngeal nerve to trachea and oesophagus (Fig. 1). In one of our cases there was dilatation of vasa nervosum and it was causing pulsation of RLN (Fig. 2). For beginners we recommend using the microscope starting from the Skin incision as used by Davidson et al. in their experience [7]. Working under microscope and getting accustomed to it requires time. It takes a lot of exercise and simulation training for developing proper hand–eye–coordination for using microscopes efficiently. Working distance is also important so that extra strain in not put on surgeon during surgery. We have done all of our cases around 410 mm distance in standing position. D’orazi et al. has used 17 inches (431 mm) working distance in their cases [2]. Finding optimal distance for oneself is surgeon specific, we were comfortable using 410 mm focal distance since it was comfortable for our neck and hands. Surgeons are more prone to musculoskeletal problems and study by Davidson et al. has shown that using microscope put less stress on neck and can reduce neck complaints [7]. We have found that for 410 mm working distance 1.3 × magnification can be used for dealing with skin, platysma and strap muscles. Since lower magnification gives large field to work and one need to practice and get used to work under microscope before beginning microscopic dissection in the critical areas. Compared to surgical loupes this unique advantage of “dynamic magnification” is present with microscope only and this can be adjusted according to the surgeon comfort level and surgical requirement. Initial 2 × magnification should be used to identify the nerve in lower cervical course as one can get working field diameter of around 8 cm. If one is not able to identify the nerve using lower magnification, magnification should be increased to 4 ×. The general principle of nerve identification should always be kept in mind, do not cut anything before identifying the nerve. Working under high magnification can be problem when one is trying to identify the nerve. Working at wrong place under high magnification can cause even ansa and cervical plexus nerves to look like recurrent laryngeal nerve. Higher magnification appears tempting to use, but then it takes extra time and need much more meticulous dissection to identify the nerve. Even under high magnification small vessels and tributaries give wrong impression of inferior thyroid artery and tributaries of middle thyroid vein (Fig. 3). Surgeon requires much more patience and there is undue increase in the surgical time which can again increase the stress level of surgeon. There are more than 20 variations between RLN and inferior thyroid artery and it requires very meticulous dissection to preserve all the critical structures [8]. The ansa cervicalis can be easily preserved by using microscope and if surgical requirement demand Ansa-RLN anastomosis, same can be done without using any extra equipment.
Fig. 1.

Right recurrent laryngeal nerve at 4 × magnification with parasympathetic branch (black arrow)
Fig. 2.
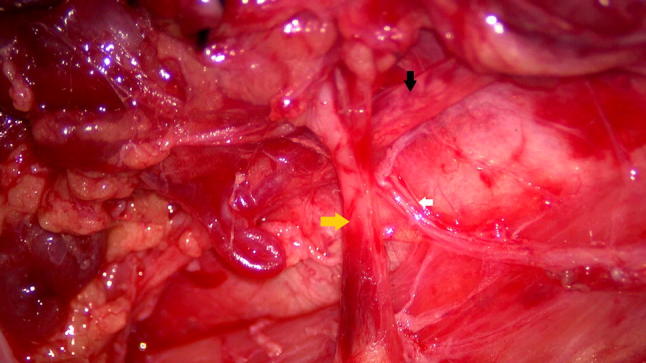
Left recurrent laryngeal at 4.5 × magnification with parasympathetic supply to esophagus. (Yellow arrow—inferior thyroid artery, black arrow—recurrent laryngeal nerve with dilated vessel inside the sheath, white arrow—Parasympathetic branch)
Fig. 3.
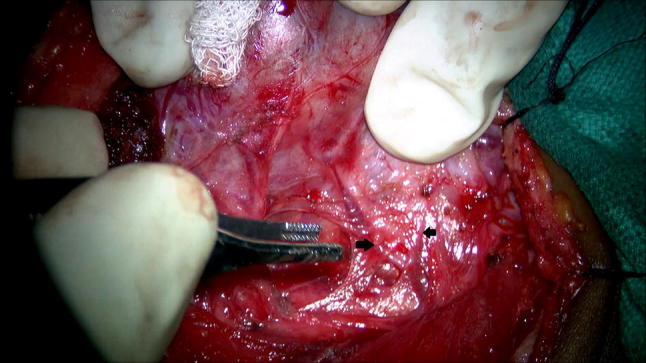
Tributaries of middle thyroid vein (black arrow) at 3 × magnification
Superior laryngeal nerve divisions lie in close association with superior pole of thyroid. We were able to differentiate between the external and internal branch using microscope (Fig. 4). The internal branch can be confirmed as it traverses courses through thyrohyoid membrane along with superior laryngeal vessels. In some of our cases we were able to identify superior laryngeal vessels with ease and we were even able to identify and preserve even the internal branch of superior laryngeal nerve (Fig. 4). Although internal branch can be identified but it is not of much concern during thyroid surgery. The idea of presenting this finding is to highlight the details which one is able to get using microscope.
Fig. 4.
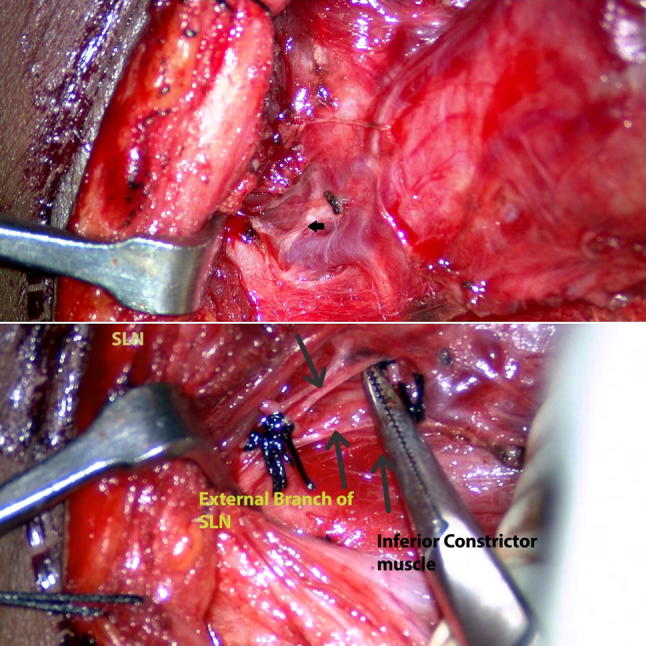
a Internal branch of superior laryngeal nerve (black arrow) at 3 × magnification. b External branch and internal branch of Superior laryngeal nerve visible after ligating superior pole
Hypocalcemia is another dreaded complication which increases morbidity and hospital cost [9]. Parathyroid anatomy is not consistent and they can lie anywhere in the neck and mediastinum. In study of D’orzai et al., only three patients out of 738 develop permanent hypocalcemia. In our cases we were able to identify all the parathyroid in all the cases, however one patient develops postoperative transient hypocalcemia. Parathyroid especially superior parathyroid which lie in superior fat pad are not easy to identify even with using microscope. We identify the parathyroid using their hilar vessels and for inferior parathyroid we were able to identify the dedicated branch of inferior thyroid artery in all of the cases (Fig. 5). For superior parathyroid we were able to identify clearly superior parathyroid vessels in 4 cases but for other cases there was superior fat pad and vessels seems to ramify in that superior pad and we had to separate whole of superior pad from the gland. In big tumor, especially in colloid goitre we have noticed that the superior thyroid fat no longer exists and superior parathyroid is easy to identify (Fig. 5). Inspite of identifying the arterial supply of parathyroid, damage to venous supply can cause edema and can compromise parathyroid function [9]. There are reporting of cases of delayed hypocalcemia many years after thyroid surgery with the hypothesis of compromise of blood supply during surgery [10]. More work need to be done regarding the vascular anatomy of parathyroid gland and with the advent of Supermicrosurgery which was pionerred by Koshima, it can be applied to thyroid surgery also [11]. Vascularised Lymph node transfer is already being done for the Lymphedema patient, on similar principles the parathyroid can be transplanted with their vascular pedicle. This could only be possible with using microscope during thyroid surgery. Tubercle of zuckerkandl has been advocated in literature as a nerve marker. But we usually do not recommend its routine use because sometimes the embryological variation of the nerve can cover the nerve and put nerve at risk during dissection. We don’t use tubercle of Zuckerkandl to identify nerve at our centre because of close approximation of thyroid to nerve (Fig. 6).
Fig. 5.
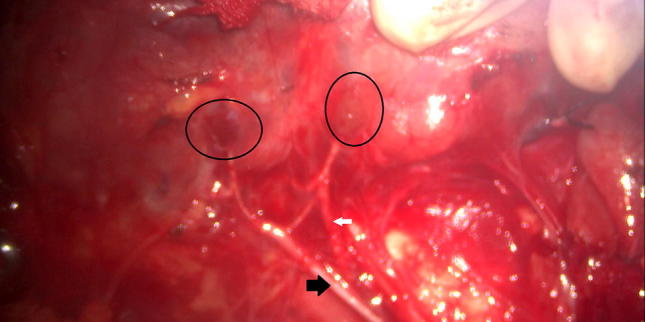
Parathyroid blood supply. superior and inferior parathyroid (black circles) supplied by branches of inferior thyroid artery (white arrow) and one of the branch of inferior thyroid artery looping around recurrent laryngeal nerve (3 × magnification). Note the absence of fat pad along the superior parathyroid gland
Fig. 6.
Relation of recurrent laryngeal nerve with tubercle of Zuckerkandl (white arrow—tubercle of Zuckerkandl, black arrow—inferior thyroid artery, yellow star—recurrent laryngeal nerve)
Apart from good dissection tool, microscope is also a great teaching tool and we were able to inspire our trainee about thyroid surgery and were able to teach them more about the thyroid surgery. At the early stage they can grasp the important steps and tissue handling of the critical structures appropriately with the help of microscope. All of the high-quality data were recorded and it could be used again as a teaching tool.
There is learning curve for this technique but surgeons with background of doing microscopic surgeries can learn this technique quite fast. In our department surgeons use microscope routinely for parotid and ear surgeries, it is not difficult for transition from conventional method to microscopic method. But surgeons who are not in routine use of microscope, may find it difficult to adapt to this technique and may take longer to operate initially. The same has been concurred by the Nielsen study in which otologists who are already accustomed with use of microscope find this technique easy to adopt [12].
One should be thorough about the microscope like optics of the microscope and what is the magnification provided by it. We have used Leica F 20 M525 in our cases, which provides magnification of 12 × and provide working diameter of 183 mm with 10 × eye piece, however the microscope is not motorized and we have to put great effort in shifting it from one operative field to other. Since one cannot cover whole of the operative field with microscope, in our opinion motorized microscope will be better to use or maybe one can use light weight microscope with good optics.
To add, we feel that the high-quality data can be recorded and can safeguard surgeons against the medico legal litigations. The use of microscope adds no extra cost to the surgery and provides excellent magnification to the details that vasa nervosa of the nerve can be identified and preserved without any extra effort. In addition to the great learning tool, the microscope aid can provide excellent patient outcomes.
The criticism of our study is small sample size, our sample size is inadequate to compare this technique to the established technique. The sample size is too low to comment on patient’s complication rates and patient outcomes. The present study demonstrates the applicability of microscopic techniques in preserving the critical structures in thyroid surgery due to its better illumination and magnification and it is not difficult to adopt this technique for ENT surgeons.
Conclusion
In conclusion we recommend the routine use of microscope instead of loupes whenever open thyroid procedures are done. The dynamic magnification and high definition output of microscope is blessing for both surgeon and trainees and it could be used as a great teaching tool.
Funding
This research received no specific Grant from any funding agency, commercial or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
Authors declares that they have no conflict of interest.
Ethical Approval
It is approved by Institutional Ethics Committee of AIIMS Rishikesh. (AIIMS/IEC/18/344).
References
- 1.Lahey FH, Hoover WB. Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg. 1938;108(4):545–562. doi: 10.1097/00000658-193810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D’Orazi V (2016) Use of loupes magnification and microsurgical technique in thyroid surgery: ten years experience in a single center. Giornale di Chirurgia J Surg. http://www.giornalechirurgia.it/common/php/portiere.php?ID=b07bf1aa3480b98c0f66d65cfa419399 [DOI] [PMC free article] [PubMed]
- 3.Kim MJ, Nam K-H, Lee SG, Choi JB, Kim TH, Lee CR, et al. Yonsei experience of 5000 gasless transaxillary robotic thyroidectomies. World J Surg. 2018;42(2):393–401. doi: 10.1007/s00268-017-4209-y. [DOI] [PubMed] [Google Scholar]
- 4.Cho J, Lee D, Baek J, Lee J, Park Y, Sung K. Single-incision endoscopic thyroidectomy by the axillary approach with gas inflation for the benign thyroid tumor: retrospective analysis for a single surgeon’s experience. Surg Endosc. 2017;31(1):437–444. doi: 10.1007/s00464-016-5093-5. [DOI] [PubMed] [Google Scholar]
- 5.Gupta AK, Kumar A, Singh A, Subash A (2018) Robot assisted trans axillary thyroidectomy: a subcontinent experience. Indian J Otolaryngol Head Neck Surg. http://link.springer.com/10.1007/s12070-018-1357-9 [DOI] [PMC free article] [PubMed]
- 6.Beneragama T, Serpell JW. Extralaryngeal bifurcation of the recurrent laryngeal nerve: a common variation. ANZ J Surg. 2006;76(10):928–931. doi: 10.1111/j.1445-2197.2006.03899.x. [DOI] [PubMed] [Google Scholar]
- 7.Davidson BJ, Guardiani E, Wang A. Adopting the operating microscope in thyroid surgery: safety, efficiency, and ergonomics. Head Neck. 2009;32(2):154–159. doi: 10.1002/hed.21157. [DOI] [PubMed] [Google Scholar]
- 8.Yalcxin B. Anatomic configurations of the recurrent laryngeal nerve and inferior thyroid artery. Surgery. 2006;139(2):181–187. doi: 10.1016/j.surg.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 9.Abboud B, Sargi Z, Akkam M, Sleilaty F. Risk factors for postthyroidectomy hypocalcemia. J Am Coll Surg. 2002;195(4):456–461. doi: 10.1016/S1072-7515(02)01310-8. [DOI] [PubMed] [Google Scholar]
- 10.Halperin I, Nubiola A, Vendrell J, Vilardell E. Late-onset hypocalcemia appearing years after thyroid surgery. J Endocrinol Investig. 1989;12(6):419–420. doi: 10.1007/BF03350718. [DOI] [PubMed] [Google Scholar]
- 11.Badash I, Gould DJ, Patel KM (2018) Supermicrosurgery: history, applications, training and the future. Front Surg. http://journal.frontiersin.org/article/10.3389/fsurg.2018.00023/full [DOI] [PMC free article] [PubMed]
- 12.Nielsen TR, Andreassen UK, Brown CL, Balle VH, Thomsen J (2018) Microsurgical technique in thyroid surgery—a 10-year experience. J Laryngol Otol. http://www.journals.cambridge.org/abstract_S0022215100141076 [DOI] [PubMed]


