Abstract
Fournier's gangrene is rapidly progressive necrotizing fasciitis that mainly affects the male perineum. Despite the advancement in surgical intervention, Fournier's gangrene carries high rates of mortality. Here, we present a 51-year-old male with hypertension and history of alcohol abuse presented to the emergency department with scrotal pain and swelling for a one-week period without preceding trauma to perineal area. He underwent emergent surgical debridement for and extensive necrotizing fasciitis. Early initiation of antibiotics, surgical intervention and good wound care postoperatively were cornerstone in his recovery.
Keywords: Fournier's gangrene, Male urogenital diseases, Necrotizing fascitis
Introduction
First described by a French venereologist Jean-Alfred Fournier, Fournier's gangrene is a type of necrotizing fasciitis that involves the perineal and genital area of both sexes. Early identification of Fournier's gangrene and the decision for surgical debridement of gangrene and necrotizing fasciitis is a cornerstone of the treatment and better outcomes.1 Despite the advancement in surgical technique and evolution of medical technology and practice, Fournier's gangrene carried high mortality rate reaching 40% mortality rate.1,2 Fournier's gangrene may occur among healthy individuals with no previous medical history of chronic diseases. However, penetrating trauma, recent surgery and immunosuppression state such as diabetes mellitus and neutropenia are associated with higher risk and poorer outcomes.2
There are certain risk factors commonly present among patients who presented with Fournier's gangrene, more notably diabetes mellitus, age more than 50 years, male sex and history of alcohol misuse.1,2 The laboratory risk indicator for necrotizing fasciitis (LRINEC) and Fournier's gangrene scoring index (FGSI) are two scoring systems that predicts clinical outcomes and mortality. Both utilized different clinical parameters (i.e. temperature, heart rate), and certain laboratory investigations such as hematocrit, white blood count, serum level of sodium, potassium, bicarbonate, and creatinine to predict clinical outcomes and mortality.3 Given the complexity and severity of Fournier's gangrene, it is imperative to have an early multimodal and multidisciplinary with surgeons, nurses, physical and occupational therapists and social workers approach in the treatment course.
Case report
Here, we present a 51-year-old male with hypertension and history of alcohol abuse who presented to the emergency department with one-week history of progressive worsening of scrotal swelling and pain. These symptoms were not preceded by traumatic injury or previous surgery. Scrotal pain was also associated with penile swelling, redness around the perineal area, dysuria without relief with over the counter medication. On clinical examination, he was hypotensive to mid-80s mmHg in systolic blood pressure and tachycardic to 110 beats per minute. Physical examination of his genital area is shown in Fig. 1. Laboratory investigations were notable for leukocytosis with 33 × 103/μL white blood cells, a C-reactive protein of 150 mg/L, procalcitonin >100 ng/mL. His LRINEC and FGSI scoring were 10 and 11 points, respectively, which reflect high suspicion for necrotizing fasciitis.
Fig. 1.
Necrotic appearing perineal tissues involving scrotum, penile shaft and perianal area.
Fluid resuscitation with 30 mL/kg of normal saline bolus and broad-spectrum antibiotics with piperacillin, tazobactam, and vancomycin were initiated. Prior his surgical intervention, he underwent an evaluation with scrotal ultrasound that showed wall thickening and complex fluid collection consistent with scrotal abscess. Subsequently, he underwent emergent scrotal and penile surgical debridement. During the surgical debridement -seen in Fig. 2-, necrotic tissue was debrided from the level of the anterior abdominal wall to the ischiorectal fat on either side of the anal canal. There was no obvious perianal fistula or connection to the anal canal. The patient recovered well after the procedure and series of multidisciplinary meetings with surgeons, wound care nurses, infectious disease physicians, and the social worker were conducted to ensure a coordinated management plan.
Fig. 2.
Intraoperative picture after extensive wound detriment of Fournier's gangrene.
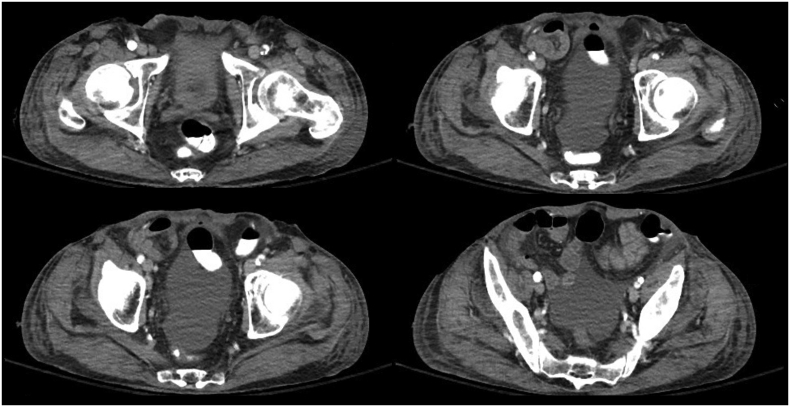
He required an aggressive wound care including negative-pressure wound therapy and subsequent daily dressing of his extensive wound (Fig. 3). Wound cultures grew numerous aerobic bacteria with methicillin-resistant Staphylococcus aureus (MRSA) and pan-sensitive Edwardsiella tarda and Klebsiella oxytoca as well as anaerobic Gram-negative bacteria, Prevotella. Post-operative care was initiated, and antibiotics were continued with intravenous ceftazidime/avibactam 2.5 g every 8 hours and metronidazole 500 mg every 8 hours for 14 days. Postoperative computed tomography scan showed no fluid collection, abscesses or signs of worsening soft tissue infection (Fig. 4).
Fig. 3.
Post-operative day 3 picture showing the early stage of granulation tissue formation in anterior lower abdomen, penile shaft and around scrotum.
Fig. 4.
Computed tomography of the abdomen and pelvis that showed no signs of fluid collections, or abscess.
Discussion
Fournier's gangrene is a life-threatening condition caused by mixed aerobic and anaerobic infection, leading to extensive skin and subcutaneous tissue necrosis that urge surgical debridement.1, 2, 3 Diabetes mellitus, age more than 50 years, male sex and history of alcohol misuse are known to be risk factors with strong association with Fournier's gangrene.2 Despite surgical advances in urology to rescue Fournier's gangrene patients, the mortality is still high.1,2 Main principles in managing patients with Fournier's gangrene include urgent resuscitation with fluids and broad-spectrum antibiotics, urgent surgical debridement. Early multimodal and multidisciplinary are cornerstones in managing patient with Fournier's gangrene.
Several scoring systems were used to predict disease severity and clinical outcomes. Two scoring methods are commonly used to ascertain the severity of Fournier's gangrene and predict outcome 3. Scoring of 9 or more in both scoring systems were associated with high-value predictors of worse clinical outcomes and death.3 Our patient has LRINEC score of 10 points and FGSI of 11 points which both reflected as high suspicion for necrotizing fasciitis associated with worsen clinical outcomes.
Urinary or fecal diversion procedures are needed in selected cases. Colostomy creation is not necessary for the optimization of outcomes in patients with severe Fournier's gangrene. Management of the wound bed without endorectal tube diversion-if no plan for skin graft or flap reconstruction - after the initial debridement. Creations of urinary or fecal diversion are associated with higher rates of failure (local leaks and urinary retention) with no significant mortality benefits.4
Aggressive skin and necrotic tissue debridement in Fournier's gangrene often leaves substantial loss of skin and subcutaneous tissue in the perineal area.3,5 Post-operative skin graft and wound care of the damaged skin and subcutaneous tissue are the cornerstones in good recovery. An approach adopted by El-Sabbagh is when the exposure of the one testis is complete; the use of scrotal advancement flap. However, when the other testis is partially or completely exposed; a coverage with pudendal thigh flap is recommended with fewer complication than other surgical approaches (i.e., burying the testis in the subcutaneous pouches).3,5 Our patient - with his bilateral testes involvement and extensive skin and subcutaneous exposure - underwent bilateral pudendal thigh flap (not shown).
Conclusions
In conclusions, Fournier's gangrene is a diagnosis that requires emergent surgical intervention to prevent morbidity and mortality. A multimodal and multidisciplinary approach with surgeons, wound care nurse, infectious disease specialists and physical and occupational therapists are recommended.
Acknowledgement
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100943.
Contributor Information
Abdulaziz Joury, Email: abdulaziz.joury@ochsner.org.
Arjun Mahendra, Email: arjun.mahendra@ochsner.org.
Mona Alshehri, Email: v-malshehri@ochsner.org.
Asia Downing, Email: asia.downing@ochsner.org.
Funding
None.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Fournier's gangrene Eke N. A review of 1726 cases. Br J Surg. 2000;87(6):718–728. doi: 10.1046/j.1365-2168.2000.01497.x. [DOI] [PubMed] [Google Scholar]
- 2.Wong C.H., Chang H.C., Pasupathy S., Khin L.W., Tan J.L., Low C.O. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 2003;85-A(8):1454–1460. [PubMed] [Google Scholar]
- 3.Kincius M., Telksnys T., Trumbeckas D., Jievaltas M., Milonas D. Evaluation of LRINEC scale feasibility for predicting outcomes of fournier gangrene. Surg Infect. 2016 Aug;17(4):448–453. doi: 10.1089/sur.2015.076. [DOI] [PubMed] [Google Scholar]
- 4.Rosen D.R., Brown M.E., Cologne K.G., Ault G.T., Strumwasser A.M. Long-term follow-up of Fournier's Gangrene in a tertiary care center. J Surg Res. 2016 Nov;206(1):175–181. doi: 10.1016/j.jss.2016.06.091. [DOI] [PubMed] [Google Scholar]
- 5.El-Sabbagh A.H. Coverage of the scrotum after Fournier's gangrene. GMS Interdiscip Plast Reconstr Surg DGPW. 2018 Jan 15;7:Doc01. doi: 10.3205/iprs000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.