Abstract
High throughput sequencing is discovering many likely causative genetic variants in individuals with cerebral palsy. Some investigators have suggested that this changes the clinical diagnosis of cerebral palsy and that these individuals should be removed from this diagnostic category. Cerebral palsy is a neurodevelopmental disorder diagnosed on clinical signs, not etiology. All nonprogressive permanent disorders of movement and posture attributed to disturbances that occurred in the developing fetal and infant brain can be described as “cerebral palsy.” This definition of cerebral palsy should not be changed, whatever the cause. Reasons include stability, utility and accuracy of cerebral palsy registers, direct access to services, financial and social support specifically offered to families with cerebral palsy, and community understanding of the clinical diagnosis. Other neurodevelopmental disorders, for example, epilepsy, have not changed the diagnosis when genomic causes are found. The clinical diagnosis of cerebral palsy should remain, should prompt appropriate genetic studies and can subsequently be subclassified by etiology.
Keywords: cerebral palsy, clinical definition, genomics, causation
The International Cerebral Palsy Genomics Consortium (ICPGC) recently held its 2nd Annual Meeting in Zhengzhou, China (April 13-14, 2018). Among the scientific highlights of the meeting was the growing recognition that a large number of individuals with cerebral palsy harbor potentially clinically relevant genomic findings. This insight generated robust discussion about whether a clinical diagnosis of cerebral palsy should be revised given genetic findings. The clear consensus was that the clinical diagnosis of cerebral palsy should not change despite the identification of a genetic or nongenetic cause if the person exhibits a nonprogressive permanent disorder of movement and posture. The Clinical Consensus Statement timeline is shown in Table 1. 1
Table 1.
Clinical Consensus Statement Timeline for Maintaining the Clinical Diagnosis of Cerebral Palsy Irrespective of Causation.
| Date | Activity | Description |
|---|---|---|
| April 12-15, 2018 | Planning and discussion | Discussion group chaired by Prof Alastair MacLennan at the Second International Cerebral Palsy Genomics Consortium Conference held in Zhengzhou, China |
| Agreement that the clinical diagnosis of cerebral palsy should not change irrespective of causation if the phenotype meets the clinical definition | ||
| May-June 2018 | Draft paper under development | Initial main contributors: Prof Richard Wintle, Prof Richard Leventer, Dr Sarah McIntyre, Professor Hila Ben-Pazi, Prof Jozef Gecz, Dr Michael Fahey, Prof Darcy Fehlings, Prof Luis Perez Jurado |
| May-June 2018 | Literature review | Definitions of cerebral palsy and in particular where genetic causation was debated to reclassify the clinical diagnosis |
| July 2018 | First draft circulated | Circulation of first draft of statement and request for input from multidisciplinary experts in cerebral palsy who spoke and debated at the genomic conference in Zhengzhou |
| August 2018 | Literature review | Nongenomic causes of cerebral palsy |
| September 2018 | E-mail agreement | Agreement by e-mail that progressive motor dysfunction did not meet the clinical definition of cerebral palsy |
| October 2018 | Second draft circulated | Circulation of second draft of statement, consensus reached with agreement for submission of the statement |
| November 2018 | Submission | Submission of statement to Journal of Child Neurology |
We acknowledge the difficulties in a clinical definition when there are no common signs or pathology. Cerebral palsy is conceptualized as a neurodevelopmental disorder affecting the motor domain and is a clinical diagnosis based on signs, symptoms, and medical history rather than laboratory investigations or diagnostically supportive neuroimaging. Cerebral palsy is currently defined as “a group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception, cognition, communication, and behaviour, by epilepsy, and by secondary musculoskeletal problems.”2
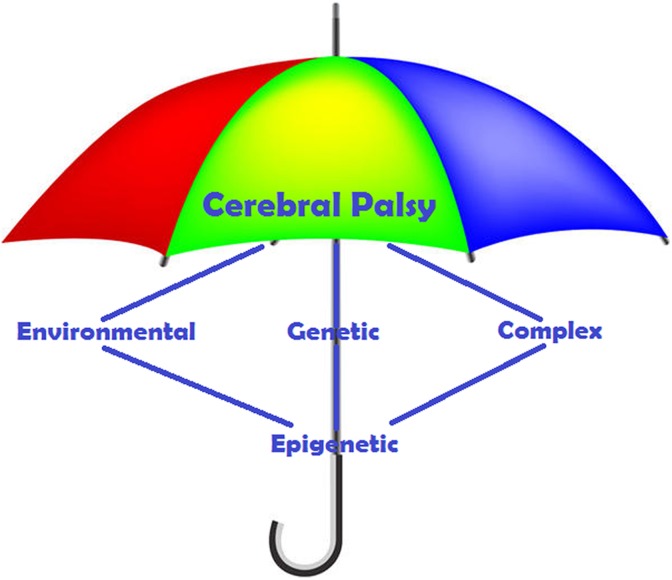
The term cerebral palsy is agnostic to underlying etiology. There are many known and most probably many unknown genetic and environmental risk factors and causal pathways.3 The numerous etiologies and heterogeneous nature of cerebral palsy were acknowledged in 1992 by Mutch et al who further described it as “an umbrella term covering a group of non-progressive, but often changing, motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of its development.”4 Given its historical underpinnings, cerebral palsy was believed to be due primarily to sentinel events around the time of delivery such as acute hypoxia at birth. However, in the modern era, current data suggest that well-defined severe acute intrapartum hypoxia using international criteria can account for only a minority of cases of cerebral palsy in high-income countries.5-8 Thus, in many individuals, the pathogenesis of cerebral palsy is unclear although prenatal risk factors are often identified.
Retaining the idea that cerebral palsy inherently implies either a recognized or occult hypoxia will only contribute to confusion around whether to continue to use the clinical diagnosis of cerebral palsy in an individual with a nonprogressive motor disorder, when a pathogenic genetic variant (or indeed any other putative “cause” for the cerebral palsy) has been identified.
Accumulating evidence shows that a potential genetic etiology can be identified in between 10% and 30% of individuals with cerebral palsy, because of both de novo and inherited genetic variants,9-14 more commonly among children without recognized environmental risk factors. Some of these identified genetic variants have been found in genes previously implicated in neurodevelopmental disorders such as TUBA1A and L1CAM.13 This has raised questions as to whether these individuals should continue to carry the clinical diagnosis of cerebral palsy after a molecular genetic diagnosis.
For the majority of these individuals, it seems most appropriate to continue to use the cerebral palsy clinical diagnosis rather than relabel such cases as cerebral palsy “masqueraders,” “mimics,” “phenocopies,” or “cerebral palsy-like.”15-17 Many rare inherited nonprogressive metabolic disorders may present with a cerebral palsy phenotype and may later be diagnosed with metabolic screening and genomic sequencing.18-20 These too should remain classified as cerebral palsy with a metabolic subtype. The importance here is that this diagnosis improves counseling, prognosis, and often specific therapy. “Reclassification” attempts may be misguided unless the newly identified etiology of the disorder is inconsistent with the clinical definition of cerebral palsy, as in the case of neurodegenerative diseases.1 And, consistent with the 2007 consensus definition,1 and reflected in the inclusion/exclusion criteria of Cerebral Palsy register programs internationally,21,22 a cerebral palsy diagnosis should be reconsidered in the case of a progressive disorder such as a mitochondrial disease.22
Individual cases of cerebral palsy may have both genetic and nongenetic etiologies and may overlap with other neurodevelopmental disorders.23 Redefining the clinical diagnosis of cerebral palsy after the identification of an underlying pathogenic genetic variant may be problematic to both cerebral palsy research and clinical care. As with other disorders characterized by symptom clusters such as autism, intellectual disability, and epilepsy, the primary unifying clinical descriptor remains unchanged after an etiology is defined.
Whether the causal pathway relates to genetics, infection, hypoxia or prematurity, if the child exhibits any early-onset nonprogressive movement disorder that has been assessed by a trained clinician and diagnosed as cerebral palsy, this clinical diagnosis should not be changed because of an identification of a putative genetic etiology. However, identifying a genetic etiology provides another layer of understanding of disease pathology, opening opportunities to refine genetic and prognostic counseling and offering the hope of precision treatments targeted to the disease mechanism.
We offer the following reasons for diagnostic consistency and continuity:
Globally, cerebral palsy registries exist that monitor the jurisdictional birth prevalence and provide critical epidemiologic information of broad public health importance.24 These registries link to research projects, including clinical trials. Removing large numbers of cases with genetic variants would artificially lower the prevalence of cerebral palsy and may encourage false claims that different interventions contributed to this reduction.
Many cerebral palsy clinics explicitly follow children with cerebral palsy for the early detection, monitoring, and management of hip subluxation, contractures, scoliosis, pain, or other comorbidities.25 Removing the clinical diagnosis of cerebral palsy may inadvertently cause these children to miss out on these vital prevention and surveillance programs.
In many countries, families with a child diagnosed with cerebral palsy are eligible for diagnosis-based governmental financial support. Although all types of disability, regardless of cause, should receive support, removing the cerebral palsy diagnosis could disenfranchise these individuals and their families from this support. Designated cerebral palsy advocacy groups also support these families. Removing the designation of “cerebral palsy” could potentially make the child ineligible for such assistance. Withdrawing the cerebral palsy clinical diagnosis may also contribute to distrust and medicolegal issues, implying “my child was misdiagnosed as having cerebral palsy.”
The existing clinical diagnosis of cerebral palsy aligns with modern definitions of other neurodevelopmental disorders where etiology is distinguished from clinical diagnosis, for example, epilepsy.26,27 Using cerebral palsy as a clinical diagnosis that is independent of etiology urges clinicians to seek an underlying cause, which may have important implications for treatment and family planning.
Lastly, when children with cerebral palsy are described to others by their parents, it may be more meaningful to say “my child has cerebral palsy (due to a genetic cause)” than “my child has TUBA1A syndrome” or any of a large number of variants/causal pathways currently being found in cerebral palsy. Individuals with cerebral palsy due to genetic mutations and their families may connect with both the cerebral palsy and rare disease communities, but these associations are both likely to be of benefit and not mutually exclusive.
As we learn more about the various pathways to cerebral palsy through modern neuroimaging, genomics, and mechanism-based studies, individuals with cerebral palsy may be more accurately classified and understood by adding “due to” and “caused by” to the description—for example, cerebral palsy due to lissencephaly caused by a TUBA1A mutation. As the majority of identified cerebral palsy genetic etiologies are rare monogenetic diseases, cerebral palsy nosologies and classifications will need to increasingly align to rare diseases coding and ontologies, such as Orphanet Classifications and the Orphanet Rare Diseases Ontology (http://www.orphadata.org/cgi-bin/inc/about.inc.php.). For example, recent progress in understanding the penetrance in disease-causing mutations will enhance our understanding of the genetic architecture and the association between genotype and disease phenotype.28 This research affirms that complex causal pathways are at play and this in turn reinforces the need for phenotypically driven clinical descriptions, as well as more accurately identified etiologies, to facilitate precision medicine. This “layering” of clinical, etiologic, and mechanism-based descriptions reflects the continuing progress of clinical medicine and its ever-evolving understanding of the biological processes that underlie disease/disorders.
In epilepsy, a disorder that is frequently comorbid with cerebral palsy, genetic diagnoses have extended the etiologic understanding. Since the identification of the first idiopathic epilepsy gene in 1995, more than 260 other genes now28 contribute to the knowledge of this condition.29,30 Before then, many doubted the relevance of epileptic genetic factors. The identification of genetic etiologies for epilepsy did not alter the primary clinical diagnosis; instead, it refined it, and has led to improvements in epilepsy phenotyping, improved epilepsy classification, and fostered progress toward precision medicine.26,27 Maintaining the clinical diagnosis of cerebral palsy will encourage the development of improved nomenclature and classification for these disorders, ultimately enhancing further genetic and other etiologic discoveries and informing clinical care.
Cerebral palsy is, and should remain, an umbrella concept and clinical diagnosis that encompasses the diverse motor phenotypes/topographies and etiologies of this disorder (Figure 1). There is room under this umbrella for classification by known and unknown causal pathways and in the future by other mechanisms, including epigenetic, multigenic, and environmental triggers in those with genetic susceptibility. Given the recent exciting progress in identifying a genetic etiology in a significant proportion of cerebral palsy, it is appropriate now to consider genomic testing in the etiologic workup of cerebral palsy.8-14 There are increasing numbers of initiatives addressing this, which strengthens the relevance and timeliness of an approach that embraces genomic medicine while retaining fundamental clinical principles based on a unifying framework.31 Individuals with cerebral palsy are best served by a dynamic phenotypic framework, informed through an increasingly precise (molecular) understanding of causation. To this end, the creation of an international database of genetic variants involved in cerebral palsy causation is in progress and will be made available by the International Cerebral Palsy Genomic Consortium (www.icpgc.org.32
Figure 1.
The clinical diagnosis of cerebral palsy covers all causes.
In sum, identifying genetic etiologies or any other specific etiology should not change the clinical diagnosis of cerebral palsy, and individuals with this diagnosis should continue to be included in cerebral palsy registries and receive the rehabilitation, health care, financial, and social support that they and their families deserve.
Footnotes
Author Contributions: AHM wrote the first draft of this manuscript. All the authors contributed equally to this final consensus.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hilla Ben-Pazi, MD  https://orcid.org/0000-0002-8039-4761
https://orcid.org/0000-0002-8039-4761
References
- 1. Rosenfeld RM, Nnacheta C, Corrigan MD. Clinical consensus statement developmental manual. Otolaryngol Head Neck Surg. 2015;153:S1–S14. [DOI] [PubMed] [Google Scholar]
- 2. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2007;109:8–14. [PubMed] [Google Scholar]
- 3. Stanley F, Blair E, Alberman E. Cerebral palsies: epidemiology & causal pathways In: Clinics in Developmental Medicine. Cambridge, UK: Cambridge University Press; 2000:151. [Google Scholar]
- 4. Mutch LW, Alberman E, Hagberg B, Kodama K, Perat MV. Cerebral palsy epidemiology: where are we now and where are we going? Dev Med Child Neurol. 1992;34:547–555. [DOI] [PubMed] [Google Scholar]
- 5. Strijbis EMM, Oudman I, van Essen P, MacLennan AH. Cerebral palsy and the application of the international criteria for acute intrapartum hypoxia. Obstet Gynecol. 2006;107:1357–1365. [DOI] [PubMed] [Google Scholar]
- 6. MacLennan AH, et al. A template for defining a causal relation between acute events and cerebral palsy: international consensus statement. BMJ. 1999;319(7216):1054–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hankins GDV, Speer M. Defining the pathogenesis and pathophysiology of neonatal encephalopathy and cerebral palsy. Obstet Gynecol. 2003;102:628–636. [DOI] [PubMed] [Google Scholar]
- 8. Himmelmann K, Uvebrant P. The panorama of cerebral palsy in Sweden part XII shows that patterns changed in the birth years 2007-2010. Acta Paediatr. 2018;107:462–468. [DOI] [PubMed] [Google Scholar]
- 9. Moreno-De-Luca A, Ledbetter DH, Martin CL. Genetic insights into the causes and classification of the cerebral palsies. Lancet Neurol. 2012;11:283–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fahey MC, MacLennan AH, Kretzschmar D, Gecz J, Kruer MC. The genetic basis of cerebral palsy. Dev Med Child Neurol. 2017;59:462–469. [DOI] [PubMed] [Google Scholar]
- 11. Zarrei M, Fehlings D, Mawjee K, et al. De novo and rare inherited copy number variations in the hemiplegic form of cerebral palsy. Genet Med. 2018;20:172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Oskoui M, Gazzellone M, Thiruvahindrapuram B, et al. Clinically relevant copy number variations detected in cerebral palsy. Nat Commun. 2015;6:7949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McMichael G, Bainbridge MN, Haan E, et al. Whole-exome sequencing points to considerable genetic heterogeneity of cerebral palsy. Mol Psychiatry. 2015;20:176–182. [DOI] [PubMed] [Google Scholar]
- 14. Segel R, Ben-Pazi H, Zeligson S, et al. Copy number variations in cryptogenic cerebral palsy. Neurology. 2015;84(16):1660–1668. [DOI] [PubMed] [Google Scholar]
- 15. Takezawa Y, Kikuchi A, Haginoya K, et al. Genomic analysis identifies masqueraders of full-term cerebral palsy. Ann Clin Trans Neurol. 2018;5(5):538–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pacheva IH, Todorov T, Ivanov I, et al. TSEN54 gene-related pontocerebellar hypoplasia type 2 could mimic dyskinetic cerebral palsy with severe psychomotor retardation. Front Pediatr. 2018;6:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee RW, Poretti A, Cohen JS, et al. A diagnostic approach for cerebral palsy in the genomic era. Neuromolecular Med. 2014;16(4):821–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sharawat IK, Dawman L. Glutaric aciduria type 1 with microcephaly: masquerading as spastic cerebral palsy. J Pediatr Neurosci. 2018;13(3):349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Friedman J, Roze E, Abdenur JE, et al. Sepiapterin reductase deficiency: a treatable mimic of cerebral palsy. Ann Neurol. 2012;71(4):520–530. [DOI] [PubMed] [Google Scholar]
- 20. Leach EL, Shevell M, Bowden K, et al. Treatable inborn errors of metabolism presenting as cerebral palsy mimics: systematic literature review. Orphanet J Rare Dis. 2014;9:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fryer A, Appleton R, Sweeney MG, Rosenbloom L, Harding AE. Mitochondrial DNA 8993 (NARP) mutation presenting with a heterogeneous phenotype including “cerebral palsy.” Arch Dis Child. 1994;71:419–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Badawi N, Watson L, Petterson B, et al. What constitutes cerebral palsy? Dev Med Child Neurol. 1998;40:520–527. [DOI] [PubMed] [Google Scholar]
- 23. Smithers-Sheedy H, Badawi N, Blair E, et al. What constitutes cerebral palsy in the twenty-first century? Dev Med Child Neurol. 2014;56(4):323–328. [DOI] [PubMed] [Google Scholar]
- 24. Goldsmith S, McIntyre S, Smithers-Sheedy H, et al. An international survey of cerebral palsy registers and surveillance systems. Dev Med Child Neurol. 2016;58(suppl 2):11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wynter M, Gibson N, Kentish M, Love S, Thomason P, Graham HK. The consensus statement on hip surveillance for children with cerebral palsy: Australian standards of care. J Pediatr Rehabil Med. 2011;4:183–195. [DOI] [PubMed] [Google Scholar]
- 26. Scheffer IE, Berkovic S, Capovilla G, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58:512–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brodie MJ, Zuberi SM, Scheffer IE, Fisher RS. The 2017 ILAE classification of seizure types and the epilepsies: what do people with epilepsy and their caregivers need to know? Epileptic Disord. 2018;20:77–87. [DOI] [PubMed] [Google Scholar]
- 28. Castel SE, Cervera A, Mohammadi P, et al. Modified penetrance of coding variants by cis-regulatory variation contributes to disease risk. Nat Genet. 2018;50:1327–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Steinlein OK, Mulley JC, Propping P, et al. A missense mutation in the neuronal nicotinic acetylcholine receptor alpha 4 subunit is associated with autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet. 1995;11:201–203. [DOI] [PubMed] [Google Scholar]
- 30. Epi4 K Consortium, Epilepsy Phenome/Genome Project; Allen AS, Berkovic SF, Cossette P, et al. De novo mutations in epileptic encephalopathies. Nature. 2013;501(7466):217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Koy A, Timmermann L. Deep brain stimulation in cerebral palsy: challenges and opportunities. Eur J Paediatr Neurol. 2017;21:118e21. [DOI] [PubMed] [Google Scholar]
- 32. MacLennan AH, Kruer MC, Baynam G, et al. Cerebral palsy and genomics; an international consortium. Dev Med Child Neurol. 2018;60:209–210. [DOI] [PubMed] [Google Scholar]