Abstract
Chinese Licorice root “gan zao” (Glycyrrhiza uralensis) is an ancient, medicinal herb utilized in Traditional Chinese Medicine for its presumably antiulcer, anti-inflammatory, antiviral, antibacterial, and expectorant properties. One of the major biologically active components is glycyrrhizin, which when hydrolyzed to glycyrrhetinic acid in the human body, possesses significant hypertensive effects due to interaction with the enzyme 11-β-hydroxysteroid dehydrogenase-2.1 Glycyrrhizin and glycyrrhetinic acid also show antithrombotic properties, as orally active, direct inhibitors of blood coagulation factor Xa as well as of thrombin.2 To our knowledge, this is the first reported case of intracranial hemorrhagic stroke associated with Chinese Licorice Root, and first reported case of cerebral microbleeds (CMB) associated with it as well.
Keywords: licorice root, intracranial hemorrhage, stroke, cerebral microbleeds, hypertension
Case Report
A 68-year-old Chinese-American woman without previous medical history was presented to the hospital with acute dysarthria and right hemiparesis, and a blood pressure of 219/123. Computed tomography of the head demonstrated a 3.9 cm × 2.5 cm left basal ganglia intraparenchymal hemorrhage (IPH).
Electrocardiogram showed normal sinus rhythm without signs of left ventricle hypertrophy, and serum laboratories were grossly unremarkable. Urine toxicology was negative for drugs of abuse. Computed tomography angiography of the head and neck showed no evidence of extravasation, arteriovenous malformation, aneurysm, vasculopathy, or high-grade stenosis. Magnetic resonance imaging (MRI) of the brain confirmed stability of the IPH but also uncovered supratentorial microhemorrhages/cerebral microbleeds (CMB) in deep structures bilaterally on Susceptibility-weighted imaging (SWI) sequences (Figure 1). With low-dose intravenous nicardipine, used intermittently, over 4 days, blood pressure fell quickly to 133/86 and she was discharged home with amlodipine 5 mg only.
Figure 1.
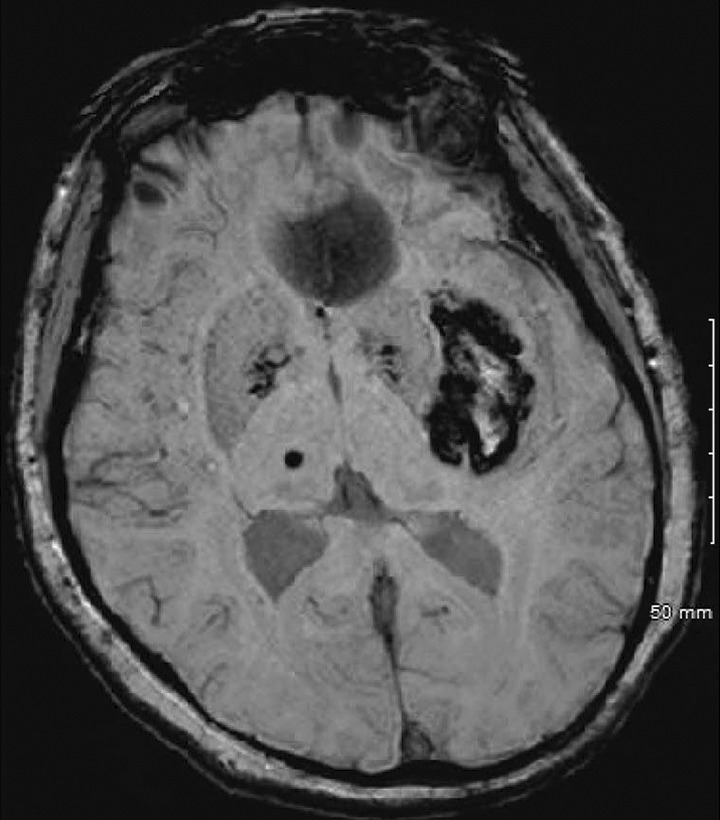
Axial SWI sequence on brain MRI demonstrates blood products in the left basal ganglia as well as cerebral microbleeds (CMB) involving the deep brain structures. MRI indicates magnetic resonance imaging.
Performing a meticulous rereview of her social history revealed that she had been dabbling in TCM over the last 40 years and occasionally consuming a Chinese herbal supplement containing Licorice Root for a panoply of sporadic gastrointestinal complaints.
However, because of a recent 2-week bout of dyspepsia and indigestion, she increased her consumption to every single day for 2 weeks straight. The ingredients are listed in Figure 2 and include “Chinese Licorice (gan zao) Root 800 mg.”
Figure 2.
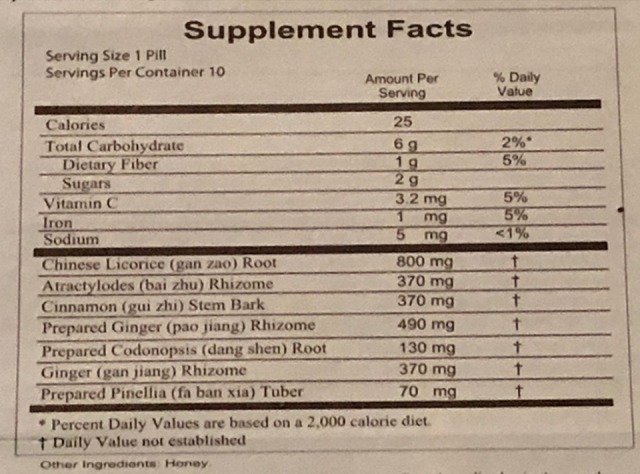
Ingredient list of Chinese herbal medicine used by patient.
Discussion
Typically, deep IPH, particularly in the basal ganglia, results from poorly controlled, long-standing hypertension—which our patient had never been diagnosed with prior to admission. We hypothesize that her sporadic use of Licorice Root, as-needed, only rarely provoked elevated blood pressures, which never came to anyone’s attention because after licorice discontinuation, such a pseudo-hypertension would normalize again. For the past 2 weeks however, our patient was consuming approximately 800 mg per day of glycyrrhetinic acid as seen in Figure 2. The maximum dose of glycyrrhizin recommended by the European Commission Scientific Committee on Food is 100 mg per day, though the committee acknowledged the limited amount of research on human toxicity of this compound.3 We suspect that inadvertently, our patient’s recently increased dosing regimen for 2 weeks straight 18 likely provoked an accelerated hypertension that finally reached a critical threshold that led to hypertensive emergency with cerebral end-organ damage in the form of IPH.
When the licorice ingredient glycyrrhizin inhibits the enzyme corticosteroid 11-beta-dehydrogenase isozyme 2, cortisol outcompetes aldosterone and activates mineralocorticoid receptors in renal collecting ducts, leading to pseudo-hyperaldosteronism and hypertension.1,4,5 Although rare, Licorice Root-associated hypertension is documented in the literature and should be considered on an extended differential diagnosis list during “physiologic tailoring” of treatment-resistant hypertension.6 There has been documentation of posterior reversible encephalopathy syndrome after licorice consumption,7 and a few reported cases of licorice-associated bleeding, such as melena for example,8 but to our knowledge, this is the first reported case of licorice-associated intracranial hemorrhagic stroke.
Besides its hypertensive effect, glycyrrhizin has been shown to have evidence of a significant anticoagulant effect—which we suspect further increased our patient’s risk of intracerebral hemorrhage.2,9 Mendes-Silva et al showed a thrombin-reducing effect of glycyrrhizin in rats and Jiang et al identified that glycyrrhetinic acid acts as an inhibitor of Factor Xa in a dose-dependent fashion, and increased in vivo rat tail-bleeding.2,9 Theoretically, by consuming Licorice Root in such quantity, it was as if our patient was taking oral anticoagulant medications—both a thrombin-inhibitor (such as dabigatran) and a Xa-inhibitor (such as apixaban or rivaroxaban) in the setting of dangerously uncontrolled hypertension for 2 weeks. We cannot exclude the possibility of coexisting undiagnosed hypertension, especially given that the patient was discharged on a daily antihypertensive (albeit low dose).
This case reminds us of the importance of performing a quality, thorough history that includes cultural sensitivities such as Asian heritage and eastern medicinal product use. Interestingly, licorice sweets and Glycyrrhiza glabra are also used as a sweetener in confectionaries.4,7,8 Identifying licorice use in any form may have diagnostic and therapeutic implications, given its triple-hit of hypertensive and anticoagulant properties, and also its interaction with the P450 system which affects absorption of concomitant medications.10 Neurologists in particular must be vigilant of supplement intake in patients who have deep brain IPH without previously diagnosed hypertension and who require little (if any) antihypertensive therapy to adequately control blood pressure while hospitalized or upon discharge. Although deep CMB on SWI sequence (Figure 1) is typically associated with hypertension (rather than amyloid angiopathy, for example), their presence plus the larger macro-bleed IPH simultaneously on MRI points to a plausible association with CMB lesions and Licorice Root as well.
Acknowledgments
All authors are in agreement with the content of the manuscript.
Authors’ Note: Informed consent has been granted from patient to publish the case report.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Ms. Shin and Dr. Chung declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Dr. Rose has participated in clinical trials with and received honoraria for advisory board/speaker bureau from Boehringer Ingelheim, Boston Scientific, Medtronic, Chiesi and CSL-Behring.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Rossi GP, Nussdorfer GG. The role of the 11β-hydroxysteroid dehydrogenase type 2 in human hypertension. J Hypertens. 2000;18(7):971. [DOI] [PubMed] [Google Scholar]
- 2. Mendes-Silva W, Assafim M, Ruta B, Monteiro RQ, Guimarães JA, Zingali RB. Antithrombotic effect of Glycyrrhizin, a plant-derived thrombin inhibitor. Thromb Res. 2003;112(1-2):93–98. [DOI] [PubMed] [Google Scholar]
- 3. Scientific Committee on Food. Opinion of the Scientific Committee on Food on Glycyrrhizinic Acid and Its Ammonium Salt. Brussels: European Commission Heath and Consumer Protection Directorate General; https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scf_out186_en.pdf (Accessed April 2017). Opinion expressed on 4 April 2003 [Google Scholar]
- 4. Murphy SC, Agger S, Rainey PM. Too much of a good thing: a woman with hypertension and hypokalemia. Clin Chem. 2009;55(12):2093–2096. [DOI] [PubMed] [Google Scholar]
- 5. Penninkilampi R, Eslick EM, Eslick GD. The association between consistent licorice ingestion, hypertension and hypokalaemia: a systematic review and meta-analysis. J Hum Hypertens. 2017;31(11):699–707. [DOI] [PubMed] [Google Scholar]
- 6. Spence JD. Physiologic tailoring of treatment in resistant hypertension. Curr Cardiol Rev. 2010;6(2):119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tassinari D, Bergamaschi R, Corsini I, et al. Posterior reversible encephalopathy syndrome associated with licorice consumption: a case report in a 10-year-old boy. Pediatr Neurol. 2015;52(4):457–459. [DOI] [PubMed] [Google Scholar]
- 8. Liu JF, Srivatsa A, Kaul V. Black licorice ingestion: yet another confounding agent in patients with melena. World J Gastrointest Surg. 2010;2(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jiang L, Wang Q, Shen S, Xiao T, Li Y. Discovery of glycyrrhetinic acid as an orally active, direct inhibitor of blood coagulation factor Xa. Thromb Res. 2014;133(3):501–506. [DOI] [PubMed] [Google Scholar]
- 10. Kent UM. The licorice root derived isoflavan glabridin inhibits the activities of human cytochrome P450S 3A4, 2B6, and 2C9. Drug Metab Dispos. 2002;30(6):709–715. [DOI] [PubMed] [Google Scholar]


