Abstract
Internationally, evidence-based practice (EBP) is recognised as a foundational element of healthcare professional education. Achieving competency in this area is a complex undertaking that is reflected in disparities between ‘best EBP’ and actual clinical care. The effective development and implementation of professional education to facilitate EBP remains a major and immediate challenge. To ascertain nuanced perspectives on the provision of EBP education internationally, interviews were conducted with five EBP education experts from the UK, Canada, Australia and New Zealand. Definitive advice was provided in relation to (1) EBP curriculum considerations, (2) teaching EBP and (3) stakeholder engagement in EBP education. While a considerable amount of EBP activity throughout health profession education is apparent, effectively embedding EBP throughout curricula requires further development, with a ‘real-world’ pragmatic approach that engenders dialogue and engagement with all stakeholders required.
Keywords: qualitative research
Introduction
To highlight and advance clinical effectiveness and evidence-based practice (EBP) agendas, the Institute of Medicine set a goal that by 2020, 90% of clinical decisions will be supported by accurate, timely and up-to-date clinical information and will reflect the best available evidence to achieve the best patient outcomes.1 To ensure that future healthcare users can be assured of receiving such care, healthcare professions must effectively incorporate the necessary knowledge, skills and attitudes required for EBP into education programmes.
The promotion of EBP requires a healthcare infrastructure committed to supporting organisations to deliver EBP and an education system efficient in supporting healthcare professionals in acquiring EBP competencies.2 To this end, healthcare education programmes must effectively implement curricula that target these competencies.3 To facilitate this, the Sicily consensus statement on EBP provides a description of core knowledge and skills required to practise in an evidence-based manner and a curriculum that outlines the minimum requirements for educating health professionals in EBP.2 Initiatives such as the European Union Evidence-Based Medicine project4 and EBP teaching programmes for educators facilitated by Oxford (Centre for Evidence-Based Medicine) and McMaster Universities provide support in advancing the EBP agenda within healthcare education. Over the past two decades, more than 300 articles have been published on teaching evidence-based medicine alone and in excess of 30 experiments have been conducted to measure its effects.5 Recent reviews3 6 evaluating the adoption of evidence-based recommendations for teaching EBP however point to poor uptake of existing resources available to guide EBP education.
The application of EBP continues to be observed irregularly at the point of patient contact.2 5 7 The effective development and implementation of professional education to facilitate EBP remains a major and immediate challenge.2 3 6 8 Momentum for continued improvement in EBP education in the form of investigations which can provide direction and structure to developments in this field is recommended.6
As part of a larger national project looking at current practice and provision of EBP education across healthcare professions at undergraduate, postgraduate and continuing professional development programme levels, we sought key perspectives from international EBP education experts on the provision of EBP education for healthcare professionals. The two other components of this study, namely a rapid review synthesis of EBP literature and a descriptive, cross-sectional, national, online survey relating to the current provision and practice of EBP education to healthcare professionals at third-level institutions and professional training/regulatory bodies in Ireland, will be described in later publications.
Methods
EBP expert interviews were conducted to ascertain current and nuanced information on EBP education from an international perspective. Experts from the UK, Canada, New Zealand and Australia were invited by email to participate based on their contribution to peer-reviewed literature on the subject area and recognised innovation in EBP education. Over a 2-month period, individual ‘Skype’ interviews were conducted and recorded. The interview guide (online supplementary appendix A) focused on current practice and provision of EBP education with specific attention given to EBP curricula, core EBP competencies, assessment methods, teaching initiatives and key challenges to EBP education within respective countries. Qualitative content analysis techniques as advised by Bogner et al 9 for examination of expert interviews were used. Specifically, a six-step process was applied, namely transcription, reading through/paraphrasing, coding, thematic comparison, sociological conceptualisation and theoretical generalisation. To ensure trustworthiness, a number of practices were undertaken, including explicit description of the methods undertaken, participant profile, extensive use of interview transcripts by way of representative quotations, peer review (PL-W) of the data analysis process and invited interviewees to feedback in relation to the overall findings.
bmjebm-2018-111019supp001.pdf (31.9KB, pdf)
Results
Five EBP experts participated in the interviews (table 1). All experts waived their right to anonymity.
Table 1.
EBP education expert profile
| EBP expert | Title | Affiliation | Country |
| Professor Leanne Togher | Professor of Communication Disorders Following Traumatic Brain Injury | Faculty of Health Sciences, University of Sydney | Australia |
| Professor Gordon Guyatt | Distinguished Professor | Department of Health Research Methods, Evidence, and Impact, McMaster University | Canada |
| Professor Rodney Jackson | Professor of Epidemiology | School of Population Health, Faculty of Medical and Health Sciences, University of Auckland | New Zealand |
| Professor Bruce Arroll | Professor of General Practice | General Practice and Primary Healthcare, Faculty of Medical and Health Sciences, University of Auckland | New Zealand |
| Professor Carl Heneghan | Professor of Evidence-Based Medicine and Director, Centre for Evidence-Based Medicine | Department of Primary Care Health Sciences, University of Oxford | UK |
EBP, evidence-based practice.
Three main categories emerged, namely (1) ‘EBP curriculum considerations’, (2) ‘Teaching EBP’ and (3) ‘Stakeholder engagement in EBP education’. These categories informed the overarching theme of ‘Improving healthcare through enhanced teaching and application of EBP’ (figure 1).
Figure 1.
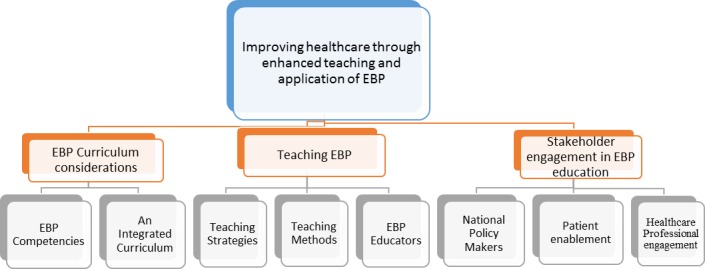
Summary of data analysis findings from evidence-based practice (EBP) expert interviews—theme, categories and subcategories.
EBP curriculum considerations
Definitive advice in relation to curriculum considerations was provided with a clear emphasis on the need for EBP principles to be integrated throughout all elements of healthcare professions curricula. Educators, regardless of teaching setting, need to be able to ‘draw out evidence-based components’ from any and all aspects of curriculum content, including its incorporation into assessments and examinations. Integration of EBP into clinical curricula in particular was considered essential to successful learning and practice outcomes. If students perceive a dichotomy between EBP and actual clinical care, then “never the twain shall meet” (GG) requiring integration in such a way that it is “seen as part of the basics of optimal clinical care” (GG). Situating EBP as a core element within the professional curriculum and linking it to professional accreditation processes places further emphasis on the necessity of teaching EBP:
…it is also core in residency programmes. So every residency programme has a curriculum on evidence-based practice where again, the residency programmes are accredited…They have to show that they’re teaching evidence-based practice. (GG)
In terms of the focus of curriculum content, all experts emphasised the oft-cited steps of asking questions, acquiring, appraising and applying evidence to patient care decisions. With regard to identifying and retrieving information, the following in particular was noted:
…the key competencies would be to identify evidence-based sources of information, and one of the key things is there should be no expectation that clinicians are going to go to primary research and evaluate primary research. That is simply not a realistic expectation. In teaching it…they have to be able to identify the pre-processed sources and they have to be able to understand the evidence and they have to be able to use it… (GG)
In addition to attaining proficiency in the fundamental EBP steps, developing competence in communicating evidence to others, including the patient, and facilitating shared decision-making were also highlighted:
…So our ability to communicate risks, benefits, understand uncertainty is so poor…that’s a key area we could improve… (CH)
…and a big emphasis [is needed] on the applicability of that information on patient care, how do you use and share the decision making, which is becoming a bigger and bigger deal. (GG)
It was suggested that these EBP ‘basics’ can be taught “from the start in very similar ways” (GG), regardless of whether the student is at an undergraduate or postgraduate level. The concept of ‘developmental milestones’ was raised by one expert. This related to different levels of expectations in learning and assessing EBP skills and knowledge throughout a programme of study with an incremental approach to teaching and learning advocated over a course of study:
…in terms of developmental milestones. So for the novice…it’s really trying to get them aware of what the structure of evidence-based practice is and knowing what the process of asking a question and the PICO process and learning about that…in their final year…they’re asked to do critically appraised topics and relate it to clinical cases…It’s a developmental process… (LT)
Teaching EBP
Adoption of effective strategies and practical methods to realise successful student learning and understanding was emphasised. Of particular note was the grounding of teaching strategy and associated methods from a clinically relevant perspective with student exposure to EBP facilitated in a dynamic and interesting manner. The use of patient examples and clinical scenarios was repeatedly expressed as one of the most effective instructional practices:
…ultimately trying to get people to teach in a way where they go, “Look, this is really relevant, dynamic and interesting"…so we teach them in loads of different ways…you’re teaching and feeding the ideas as opposed to “"Here’s a definitive course in this way”. (CH)
…It’s pretty obscure stuff, but then I get them to do three examples…when they have done that they have pretty well got their heads around it…I build them lots of practical examples…clinical examples otherwise they think it’s all didactic garbage… (BA)
EBP role models were emphasised as being integral to demonstrating the application of EBP in clinical decision-making and facilitating the contextualisation of EBP within a specific setting/organisation.
…where we’ve seen success is where organisations have said, “There’s going to be two or three people who are going to be the champions and lead where we’re going”…the issue about evidence, it’s complex, it needs to be contextualised and it’s different for each setting… (CH)
It was further suggested that these healthcare professionals have the ‘X-factor’ required of EBP. The acquisition of such expertise which enables a practitioner to integrate individual EBP components culminating in evidence-based decisions was proposed as a definitive target for all healthcare professionals.
And we call it the X factor…the idea is that the clinician who has the X factor is the good clinician. It’s actually integrating the evidence, the patient values, the patient’s pathophysiology, etc. It could be behavioural issues, systems issues…Those are the four quadrants and the clinical expertise is about integrating those together…You’re not actually adding clinical expertise. It seems to me that the clinical expertise is the ability to integrate those four quadrants. (RJ)
The provision of training for educators to aid the further development of skills and use of resources necessary for effective EBP teaching was recommended:
…so we choose the option to train people as really good teachers and give them really high level skills so that they can then seed it across their organisation… (CH)
Attaining a critical mass of people who are ‘trained’ was also deemed important in making a sustained change:
…and it requires getting the teachers trained and getting enough of them. You don’t need everybody to be doing it to make an impression, but you need enough of them really doing it. (GG)
Stakeholder engagement in EBP education
Engagement of national policy makers, healthcare professionals and patients with EBP was considered to have significant potential to advance its teaching and application in clinical care. The lack of a coherent government and national policy to EBP teaching was cited as a barrier to the implementation of the EBP agenda resulting in a somewhat ‘ad-hoc’ approach, dependent on individual educational or research institutions:
…there’s no cohesive or coherent policy that exists…It’s not been a consistent approach. What we’ve tended to see is that people have started going around particular initiatives…but there’s never been any coordinated approach even from a college perspective, to say we are about improving the uptake and use of evidence in practice and/or generating evidence in practice. And so largely, it’s been left to research institutions… (CH)
To further ingrain EBP within healthcare professional practice, it was suggested that EBP processes, whether related to developing, disseminating or implementing evidence, be embedded in a more structured way into everyday clinical care to promote active and consistent engagement with EBP on a continuous basis:
…we think it should be embedded into care…we’ve got to have people being active in developing, disseminating and implementing evidence…developing can come in a number of formats. It can be an audit. It can be about a practice improvement. It can be about doing some aspect like a systematic review, but it’s very clearly close to healthcare. (CH)
Enabling patients to engage with evidence with a view to informing healthcare professional/patient interactions and care decisions was also advocated:
…I think we really need to put some energy into…this whole idea of patient-driven care, patient-led care and putting some of these tools in the hands of the consumers so that they’re enabled to be able to ask the right questions and to go into an interaction with some background knowledge about what treatments they should be expecting. (LT)
If patients are considered as recipients of EBP rather than key stakeholders, the premise of shared decision-making for care cannot be achieved.
The implementation of a successful EBP education is necessary so that learners not only understand the importance of EBP and be competent in the fundamental steps, but it ultimately serves to influence behaviour in terms of decision-making, through application of EBP in their professional practice. In essence, it serves the function of developing practitioners who value EBP and have the knowledge and skills to implement such practice. The ultimate goal of this agenda is to enhance the delivery of healthcare for improved patient outcomes. The overarching theme of ‘Improving healthcare through enhanced teaching and application of EBP’ represents the focus and purpose of the effort required to optimally structure healthcare professional (HCP) curricula, promote effective EBP teaching and learning strategies, and engage with key stakeholders for the overall advancement of EBP education as noted:
…we think that everyone in training should be in the game of improving healthcare…It’s not just saying I want to do some evidence-based practice…it’s ultimately about…improving healthcare. (CH)
Discussion and recommendations
Education programmes and associated curricula act as a key medium for shaping healthcare professional knowledge, skills and attitudes, and therefore play an essential role in determining the quality of care provided.10 Unequivocal recommendations were made in relation to the pervasive integration of EBP throughout the academic and clinical curricula. Such integration is facilitated by the explicit inclusion of EBP as a core competency within professional standards and requirements in addition to accreditation processes.11
Further emphasis on communication skills was also noted as being key to enhancing EBP competency, particularly in relation to realising shared decision-making between patients and healthcare practitioners in making evidence-based decisions. A systematic review by Galbraith et al,12 which examined a ‘real-world’ approach to evidence-based medicine in general practice, corroborates this recommendation by calling for further attention to be given to communication skills of healthcare practitioners within the context of being an evidence-based practitioner. This resonates with recommendations by Gorgon et al 13 for the need to expose students to the intricacies of ‘real world’ contexts in which EBP is applied.
Experts in EBP, together with trends throughout empirical research and recognised educational theory repeatedly, make a number of recommendations for enhancing EBP teaching and learning strategies. These include (1) clinical integration of EBP teaching and learning, (2) a conscious effort on behalf of educators to embed EBP throughout all elements of healthcare professional programmes, (3) the use of multifaceted, dynamic teaching and assessment strategies which are context-specific and relevant to the individual learner/professional cohort, and (4) ‘scaffolding’ of learning.
At a practical level this requires a more concerted effort to move away from a predominant reliance on stand-alone didactic teaching towards clinically integrative and interactive teaching.10 14–17 An example provided by one of the EBP experts represents such integrated teaching and experiential learning through the performance of GATE/CATs (Graphic Appraisal Tool for Epidemiological studies/Critically Appraised Topics) while on clinical rotation, with assessment conducted by a clinician in practice. Such an activity fulfils the criteria of being reflective of practice, facilitating the identification of gaps between current and desired levels of competence, identifying solutions for clinical issues and allowing re-evaluation and opportunity for reflection of decisions made with a practitioner. This level of interactivity facilitates ‘deeper’ learning, which is essential for knowledge transfer.8 Such practices are also essential to bridge the gap between academic and clinical worlds, enabling students to experience ‘real’ translation of EBP in the clinical context.6 ‘Scaffolding’ of learning, whereby EBP concepts and their application increase in complexity and are reinforced throughout a programme, was also highlighted as an essential instructional approach which is in keeping with recent literature specific both to EBP education and from a broader curriculum development perspective.3 6 18 19
In addition to addressing challenges such as curriculum organisation and programme content/structure, identifying salient barriers to implementing optimal EBP education is recommended as an expedient approach to effecting positive change.20 Highlighted strategies to overcome such barriers included (1) ‘Training the trainers’, (2) development of and investment in a national coherent approach to EBP education, and (3) structural incorporation of EBP learning into workplace settings.
National surveys of EBP education delivery21 22 found that a lack of academic and clinical staff knowledgeable in teaching EBP was a barrier to effective and efficient student learning. This was echoed by findings from EBP expert interviews, which correspond with assertions by Hitch and Nicola-Richmond6 that while recommended educational practices and resources are available, their uptake is somewhat limited. Effective teacher/leader education is required to improve EBP teaching quality.10 16 23 24 Such formal training should extend to academic and clinical educators. Supporting staff to have confidence and competence in teaching EBP and providing opportunities for learning throughout education programmes is necessary to facilitate tangible change in this area.
A national and coherent plan with associated investment in healthcare education specific to the integration of EBP was highlighted as having an important impact on educational outcomes. The lack of a coordinated and cohesive approach and perceived value of EBP in the midst of competing interests, particularly within the context of the healthcare agenda, was suggested to lead to an ‘ad-hoc’ approach to the implementation of and investment in EBP education and related core EBP resources. Findings from a systematic scoping review of recommendations for the implementation of EBP16 draw attention to a number of interventions at a national level that have potential to further promote and facilitate EBP education. Such interventions include government-level policy direction in relation to EBP education requirements across health profession programmes and the instalment and financing of a national institute for the development of evidence-based guidelines.
Incorporating EBP activities into routine clinical practice has potential to promote the consistent participation and implementation of EBP. Such incorporation can be facilitated at various different levels and settings. At a health service level, the provision of computer and internet facilities at the point of care with associated content management/decision support systems allowing access to guidelines, protocols, critically appraised topics and condensed recommendations was endorsed. At a local workplace level, access to EBP mentors, implementation of consistent and regular journal clubs, grand rounds, audit and regular research meetings are important to embed EBP within the healthcare and education environments. This in turn can nurture a culture which practically supports the observation and actualisation of EBP in day-to-day practice16 and could in theory allow the coherent development of cohorts of EBP leaders.
There are study limitations which must be acknowledged. Four of the five interviewees were medical professionals. Further inclusion of allied healthcare professionals may have increased the representativeness of the findings. However, the primary selection criteria for participants were extensive and recognised expertise in relation to EBP education, the fundamental premises of which traverse specific professional boundaries.
Conclusion
Despite positive attitudes towards EBP and a predominant recognition of its necessity for the delivery of quality and safe healthcare, its consistent translation at the point of care remains elusive. To this end, continued investigations which seek to provide further direction and structure to developments in EBP education are recommended.6 Although the quality of evidence has remained variable regarding the efficacy of individual EBP teaching interventions, consistent trends in relation to valuable andragogically sound educational approaches, fundamental curricular content and preferential instructional practices are evident within the literature in the past decade. The adoption of such trends is far from prevalent, which brings into question the extent of awareness that exists in relation to such recommendations and accompanying resources. There is a need to translate EBP into an active clinical resolution, which will have a positive impact on the delivery of patient care. In particular, an examination of current discourse between academic and clinical educators across healthcare professions is required to progress a ‘real world’ pragmatic approach to the integration of EBP education which has meaningful relevance to students and engenders active engagement from educators, clinicians and policy makers alike. Further attention is needed on strategies that not only focus on issues such as curricula structure, content and programme delivery but which support educators, education institutions, health services and clinicians to have the capacity and competence to meet the challenge of providing such EBP education.
Summary Box.
What is already known?
Evidence-based practice (EBP) is established as a fundamental element and key indicator of high-quality patient care.
Both achieving competency and delivering instruction in EBP are complex processes requiring a multimodal approach.
Currently there exists only a modest utilisation of existing resources available to further develop EBP education.
What are the new findings?
In addition to developing competence in the fundamental EBP steps of ‘Ask’, ‘Acquire’, ‘Appraise’, ‘Apply’ and ‘Assess’, developing competence in effectively communicating evidence to others, in particular patients/service users, is an area newly emphasised as requiring additional attention by healthcare educators.
The successful expansion of the assessment and evaluation of EBP requires a pragmatic amplification of the discourse between academic and clinical educators.
How might it impact on clinical practice in the foreseeable future?
Quality of care is improved through the integration of the best available evidence into decision-making as routine practice and not in the extemporised manner often currently practised.
Acknowledgments
Special thanks to Professor Leanne Togher, Professor Carl Heneghan, Professor Bruce Arroll, Professor Rodney Jackson and Professor Gordon Guyatt, who provided key insights on EBP education from an international perspective. Thank you to Dr Niamh O’Rourke, Dr Eve O’Toole, Dr Sarah Condell and Professor Dermot Malone for their helpful direction throughout the project.
Footnotes
Contributors: This project formed part of a national project on EBP education in Ireland of which all named authors are members. The authors named on this paper made substantial contributions to both the acquisition and analysis of data, in addition to reviewing the report and paper for submission.
Funding: This research was funded by the Clinical Effectiveness Unit of the National Patient Safety Office (NPSO), Department of Health, Ireland.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethical committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval was granted by the Social Research Ethics Committee, University College Cork (Log 2016–140).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The full report entitled ’Research on Teaching EBP in Ireland to healthcare professionals and healthcare students' is available on the National Clinical Effectiveness, Department of Health website.
References
- 1. Institute of Medicine (IOM) (US) Roundtable on Evidence-Based Medicine. Leadership Commitments to Improve Value in Healthcare: Finding Common Ground: Workshop Summary. Washington (DC: National Academies Press (US), 2009. [PubMed] [Google Scholar]
- 2. Dawes M, Summerskill W, Glasziou P, et al. . Sicily statement on evidence-based practice. BMC Med Educ 2005;5:1–5. 10.1186/1472-6920-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomas A, Saroyan A, Dauphinee WD. Evidence-based practice: a review of theoretical assumptions and effectiveness of teaching and assessment interventions in health professions. Adv Health Sci Educ Theory Pract 2011;16:253–76. 10.1007/s10459-010-9251-6 [DOI] [PubMed] [Google Scholar]
- 4. Thangaratinam S, Barnfield G, Weinbrenner S, et al. . Teaching trainers to incorporate evidence-based medicine (EBM) teaching in clinical practice: the EU-EBM project. BMC Med Educ 2009;9:1–8. 10.1186/1472-6920-9-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barends E, Briner R. Teaching evidence-based practice: lessons from the pioneers: an interview with amanda burls and gordon guyatt. Academy of Management Learning and Education 2014;13:476–83. 10.5465/amle.2014.0136 [DOI] [Google Scholar]
- 6. Hitch D, Nicola-Richmond K. Instructional practices for evidence-based practice with pre-registration allied health students: a review of recent research and developments. Adv Health Sci Educ Theory Pract 2017;22:1031–45. 10.1007/s10459-016-9702-9 [DOI] [PubMed] [Google Scholar]
- 7. Zeleníková R, Beach M, Ren D, et al. . Faculty perception of the effectiveness of EBP courses for graduate nursing students. Worldviews Evid Based Nurs 2014;11:401–13. 10.1111/wvn.12068 [DOI] [PubMed] [Google Scholar]
- 8. Aglen B. Pedagogical strategies to teach bachelor students evidence-based practice: A systematic review. Nurse Educ Today 2016;36:255–63. 10.1016/j.nedt.2015.08.025 [DOI] [PubMed] [Google Scholar]
- 9. Bogner A, Littig B, Menz W, et al. . Interviewing Experts. UK: Palgrave MacMillian, 2009. [Google Scholar]
- 10. Young T, Rohwer A, Volmink J, et al. . What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One 2014;9:86706:e86706 10.1371/journal.pone.0086706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Frenk J, Chen L, Bhutta ZA, et al. . Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923–58. 10.1016/S0140-6736(10)61854-5 [DOI] [PubMed] [Google Scholar]
- 12. Galbraith K, Ward A, Heneghan C. A real-world approach to Evidence-Based Medicine in general practice: a competency framework derived from a systematic review and Delphi process. BMC Med Educ 2017;17:1–15. 10.1186/s12909-017-0916-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gorgon EJ, Basco MD, Manuel AT. Teaching evidence based practice in physical therapy in a developing country: a national survey of Philippine schools. BMC Med Educ 2013;13:154 10.1186/1472-6920-13-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ilic D, Hart W, Fiddes P, et al. . Adopting a blended learning approach to teaching evidence based medicine: a mixed methods study. BMC Med Educ 2013;13:1–11. 10.1186/1472-6920-13-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Coomarasamy A, Khan KS. What is the evidence that postgraduate teaching in evidence based medicine changes anything? A systematic review. BMJ 2004;329:1–5. 10.1136/bmj.329.7473.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scoping review. BMJ Open 2013;3:e001881 10.1136/bmjopen-2012-001881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kortekaas MF, Bartelink ML, van der Heijden GJ, et al. . Development and validation of a new instrument measuring guideline adherence in clinical practice. Fam Pract 2016;33:562–8. 10.1093/fampra/cmw063 [DOI] [PubMed] [Google Scholar]
- 18. Elçin M, Turan S, Odabaşı O, et al. . Development and evaluation of the evidence-based medicine program in surgery: a spiral approach. Med Educ Online 2014;19:24269–6. 10.3402/meo.v19.24269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ilic D, Maloney S. Methods of teaching medical trainees evidence-based medicine: a systematic review. Med Educ 2014;48:124–35. 10.1111/medu.12288 [DOI] [PubMed] [Google Scholar]
- 20. Baker R, Camosso-Stefinovic J, Gillies C, et al. . Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2010;3:CD005470 10.1002/14651858.CD005470.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blanco MA, Capello CF, Dorsch JL, et al. . A survey study of evidence-based medicine training in US and Canadian medical schools. J Med Libr Assoc 2014;102:160–8. 10.3163/1536-5050.102.3.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Meats E, Heneghan C, Crilly M, et al. . Evidence-based medicine teaching in UK medical schools. Med Teach 2009;31:332–7. 10.1080/01421590802572791 [DOI] [PubMed] [Google Scholar]
- 23. Ingvarson L, Rowe K. Conceptualising and evaluating teacher quality: substantive and methodological issues. The Economics of Teacher Quality Conference 2007:1–28. 10.1177/000494410805200102 [DOI] [Google Scholar]
- 24. Walczak J, Kaleta A, Gabryś E, et al. . How are "teaching the teachers" courses in evidence based medicine evaluated? A systematic review. BMC Med Educ 2010;10:64 10.1186/1472-6920-10-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ahmadi SF, Baradaran HR, Ahmadi E. Effectiveness of teaching evidence-based medicine to undergraduate medical students: a BEME systematic review. Med Teach 2015;37:21–30. 10.3109/0142159X.2014.971724 [DOI] [PubMed] [Google Scholar]
- 26. Cook DA, West CP. Perspective: Reconsidering the focus on "outcomes research" in medical education: a cautionary note. Acad Med 2013;88:162–7. 10.1097/ACM.0b013e31827c3d78 [DOI] [PubMed] [Google Scholar]
- 27. Ilic D. Teaching evidence-based practice: perspectives from the undergraduate and post-graduate viewpoint. Ann Acad Med Singapore 2009;38:559–63. [PubMed] [Google Scholar]
- 28. Tilson JK, Kaplan SL, Harris JL, et al. . Sicily statement on classification and development of evidence-based practice learning assessment tools. BMC Med Educ 2011;11:78 10.1186/1472-6920-11-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjebm-2018-111019supp001.pdf (31.9KB, pdf)


