Abstract
Background
The relationship of coronary artery calcium (CAC) with adverse cardiac remodeling is not well established. To study the association of CAC in middle age and change in CAC from early adulthood to middle age with left ventricular (LV) function.
Methods
CAC score was measured by computed tomography at CARDIA study year-15 (Y15) and at Y25 examinations in 3,043 and 3,189 participants, respectively. CAC score was assessed as a continuous variable and log-transformed to account for nonlinearity. Change in CAC from Y15 to Y25 was evaluated as the absolute difference of log-transformed CAC from Y15 to Y25. LV structure and function were evaluated by echocardiography at Y25.
Results
At Y25, mean age was 50.1±3.6 yr, 56.6% women, 52.4% black. In the multivariable analysis at Y25, higher CAC was related to higher LV mass (β=1.218, adjusted-p=0.007), higher LV end-diastolic volume (β=0.811, adjusted-p=0.007), higher LV end-systolic volume (β=0.350, adjusted-p=0.048), higher LA volume (β=0.214, adjusted-p=0.009), and higher E/e’ ratio (β=0.059, adjusted-p= 0.014). CAC was measured at both Y15 and Y25 in 2,449 individuals. Higher change in CAC score during follow-up was independently related to higher LV mass index in blacks (β=4.789, adjusted-p<0.001), but not in whites (β=1.051, adjusted-p=0.283).
Conclusions
Higher CAC in middle age is associated to higher LV mass and volumes, and worse LV diastolic function. Being free of CAC from young adulthood to middle age correlates to better LV function at middle age. Higher change in CAC score during follow-up is independently related to higher LV mass index in blacks.
INTRODUCTION
Coronary heart disease is a substantial public health problem and a major cause of heart failure worldwide 1. Identification of asymptomatic individuals with subclinical atherosclerosis is important to determine strategies to prevent left ventricular (LV) impairment.
Coronary artery calcium (CAC) score measured by computed tomography (CT) is an established independent biomarker of cardiovascular risk and is associated with the presence and extent of subclinical coronary artery disease and increased coronary events 2, 3. Moreover, progression in CAC score, assessed by CT performed in two different time points, is related to higher risk of future adverse cardiovascular outcomes 4, 5.
Recent studies have demonstrated the association between CAC and LV function assessed by LV myocardial strain using cardiac magnetic resonance imaging in a predominantly elderly population 6, 7. However, the relationship between CAC with LV structure and function in middle-aged individuals is not well established. This is of particular interest, since middle age is a period when subclinical LV impairment may be observed prior to an increase in heart failure incidence 1. Furthermore, the relationship between change in CAC score over time and LV remodeling are not well understood.
Therefore, we aim to evaluate the association of levels of CAC score measured by CT with LV structure and function assessed by echocardiography, and to explore the relationship of change in CAC score from early adulthood to middle age and LV remodeling in a large biracial cohort.
METHODS
Data Availability
The CARDIA Study has provided National Heart, Lung and Blood Institute (NHLBI) Data Repository Datasets for exams conducted during Years 0–25, as well as for follow-up contacts for which data collection has been completed for at least five years, and for adjudicated morbid and mortal events. The NHLBI distributes these data; additional information, including the procedures on how to request these data, can be found on the NHLBI web site: biolincc.nhlbi.nih.gov/studies/cardia/
Study Population
CARDIA is a multicenter prospective study that initially enrolled 5,115 healthy black and white adults (18–30 years) from four United States field centers (Birmingham, AL; Oakland, CA; Chicago, IL; Minneapolis, MN) in 1985–1986. In the year-15 (Y15) follow-up (2000–2001), 3,043 participants underwent CAC assessment using cardiac CT. In the year-25 (Y25) examination (2010–2011), 3,189 individuals underwent both echocardiography and cardiac CT. A total of 2,449 participants had CAC score measured at both Y15 and Y25 follow-up. The institutional review board at each site approved the study protocol and all participants gave informed consent. All participants underwent clinical assessment, as detailed in the supplementary data.
Computed Tomography Acquisition and Analysis
Standardized protocols for data collection were used to obtain cardiac CT scans at four CARDIA study sites, as previously published.8 Briefly, CAC score was measured using either a cardiac-gated electron beam CT scanner or a multidetector CT system during the 2000–01 exam (Y15) and on 64-channel multidetector CT systems in 2010–11. The protocol for acquisition and analysis has been previously reported. Briefly, the ECG-triggering was set at 80% of the R-R interval for electron beam CT and at 50% of the R-R interval for four-detector row CT. In the Y15 follow-up, the LightSpeed QXi system used retrospective cardiac gating, and the image was selected by using an automated program designed for this reason (SmartScore; GE Medical Systems) in a post-processing step. Two sequential heart scans were acquired to obtain a mean score in Y15, while a single heart scan was performed in Y25. Technicians were trained to measure CAC using the Aquarius Workstation software (TeraRecon Inc., Foster City, CA) in Y25. A minimum pixel attenuation of 130 HU (standard threshold) was used to calculate CAC score. Observed agreement between two consecutive CT scans of the same participant for the presence of calcified coronary artery plaque was 96% and the k-statistic of 0.77 indicates strong agreement.
Echocardiography
LV structure and function were assessed at Y25 follow-up using two-dimensional echocardiography using Artida ultrasound system (Toshiba Medical Systems, Japan), and the commercially available DigiView software (Digisonics Inc., USA), following standardized protocols across the four field centers by experienced and certified sonographers and readers.
LV mass was derived from the Devereux formula. LV volumes and ejection fraction (LVEF) were estimated by bi-planar Simpson’s method. Diastolic function was evaluated by parameters derived from pulsed-Doppler: early peak diastolic mitral inflow velocity (E wave), and from tissue-Doppler: early peak diastolic mitral annular velocity (e’), measured at septal and lateral mitral annulus and presented as the average of both measurements. E/e’ ratio was calculated as an index of LV filling pressure. Left atrial (LA) volume was also assessed, using disk summation algorithm at apical four-chamber view.
LV myocardial deformation was assessed by two-dimensional speckle tracking echocardiography using the certificated Advanced Cardiology Package Wall Motion 2D Tracking (Toshiba Medical Systems Co., Japan), version 3.0, as previously described.9 More negative values of LV longitudinal strain indicate greater LV systolic shortening (better systolic function).
Reproducibility of echocardiographic variables in the CARDIA year-25 examination has been previously published elsewhere.10 Briefly, inter-reader coefficient of variation of LV ejection fraction and LV longitudinal strain were 7.7% and 10.4%, respectively.
Statistical Analysis
Continuous data are expressed as mean ± standard deviation if normally distributed, and as median and interquartile range if not normally distributed. Categorical variables are presented as counts and percentages. Data distributions were checked by histograms and Shapiro-Wilk test. Because CAC score was not normally distributed, it was log-transformed. Multivariable linear regression analysis was conducted to verify the association of CAC score at Y25 (independent variable) with continuous variables of LV structure and function (dependent variables), adjusted for Y25 covariates: age, sex, race, educational years, body mass index, systolic blood pressure, antihypertensive medication use, total cholesterol, HDL-cholesterol, lipid lowering medication use, diabetes mellitus, smoking status, alcohol consumption, and physical activity.
Currently, several algorithms to define CAC progression are available in the literature and there is no established gold standard. In this present study, we defined change in CAC score as the change in log-transformed CAC score at Y25 and log-transformed CAC score at Y15, as previously describe.11
To explore the relationship between change in CAC score (independent variable) and continuous variables of LV structure and function (dependent variables), multivariable linear regression models were adjusted for Y15 covariates and 10-year change in risk factors (body mass index, systolic blood pressure, total cholesterol, HDL-cholesterol, alcohol consumption, and physical activity), and chronic risk exposure (antihypertensive or lipid lowering medication use: consistent use at Y15 and Y25, use at Y15 but not at Y25 and vice versa compared to never use at Y15 and Y25; diabetes mellitus at Y15 and new onset of diabetes mellitus at Y25; smoking: current and former versus never).
Student’s T-test was used to compare normally distributed continuous variables of those free of CAC from Y25 to Y15 with those with any CAC at Y15 or Y25.
Interaction terms were applied to multivariable linear regression models to verify whether the associations of CAC score with echocardiographic variables are modified by sex and race.
Benjamini-Hochberg procedure was used to adjust p-values for multiple comparisons by controlling false discovery rate.
Two-sided p-values < 0.05 were considered statistically significant. All analyses were performed using Stata Statistical Software 14.2 (College Station, TX:StataCorp).
RESULTS
Participant Characteristics
Baseline characteristics of individuals with CAC score measured at Y25 (n=3,189) are shown in table 1. Mean age of those with CAC score measured at Y25 was 50.1±3.6 years, 57% were women, and 52% were whites. Use of antihypertensive medication was reported by 27% of the participants, while 16% of the participants reported use of lipid lowering medication. Diabetes mellitus was found in 13% individuals. Current, former and never smokers were 17%, 23%, and 60%, respectively. A total of 2,449 participants had CAC score measured at both Y15 and Y25.
Table 1.
Characteristics of individuals with CAC score measured at year-25 examination
| Year-25 examination | |
|---|---|
| Individuals with CAC score measured | 3,189 |
| Age (years) | 50.1± 3.6 |
| Female | 1805 (57%) |
| White | 1672 (52%) |
| Education (years) | 15 ± 3 |
| Body mass index (Kg/m2) | 30.3 ± 7.1 |
| Systolic blood pressure (mmHg) | 119 ± 15 |
| Diastolic blood pressure (mmHg) | 74 ± 11 |
| On use of antihypertensive medication (%) | 873 (27%) |
| Heart rate (bpm) | 67 ± 11 |
| Total cholesterol (mg/dL) | 193 ± 37 |
| HDL-cholesterol (mg/dL) | 58 ± 18 |
| On use of lipid lowering medication (%) | 503 (16%) |
| Diabetes mellitus | 423 (13%) |
| Smoking status | |
| Never | 1908 (60%) |
| Former | 691 (23%) |
| Current | 541 (17%) |
| Alcohol consumption (mL/day) | 2.4 [IQR: 0-15] |
| Physical activity (exercise units) | 335 ± 275 |
Variables normally distributed are reported as mean ± standard deviation; variables not normally distributed are expressed as median [interquartile range]; categorical variables are reported as n (%).
CAC = coronary artery calcium; IQR = interquartile range
CAC score and LV structure and function
At Y25, CAC score equals zero was found in 2,282 (72%) participants.
In the univariate linear regression analysis, higher CAC score was significantly related to higher LV mass index, higher LV end-diastolic and systolic volumes, higher LV longitudinal strain (worse systolic function), higher LA volume index, and higher E/e’ ratio, adjusted-p < 0.001 for all. LV ejection fraction was not significantly related to CAC score (adjusted-p=0.071).
In the multivariable model, after adding demographics and traditional cardiovascular risk factors to the model, higher CAC score remained significantly associated with higher LV mass (β = 1.218, adjusted-p = 0.007), higher LV end-diastolic volume (β =0.811, adjusted-p = 0.007), higher LV end-systolic volume (β = 0.350, adjusted-p = 0.048), higher LA volume index (β =0.214, adjusted-p= 0.009), and higher E/e’ ratio (β = 0.059, adjusted-p = 0.014), table 2.
Table 2.
Multivariable linear regression models for the association of log-transformed CAC score and LV structure and function at Y25
| Univariate Analysis | Multivariable Analysis* | |||||
|---|---|---|---|---|---|---|
| Coefficient | SE | Adjusted p- values† |
Coefficient | SE | Adjusted p-values† |
|
| LV Mass Index (g/m2) | 2.408 | 0.206 | <0.001 | 1.218 | 0.213 | 0.007 |
| LV End-Diastolic Volume (mL) | 2.784 | 0.282 | <0.001 | 0.811 | 0.265 | 0.007 |
| LV End-Systolic Volume (mL) | 1.302 | 0.169 | <0.001 | 0.350 | 0.165 | 0.048 |
| LV Ejection Fraction (%) | −0.126 | 0.070 | 0.071 | −0.029 | 0.078 | 0.834 |
| LV Longitudinal Strain (%) | 0.111 | 0.024 | <0.001 | 0.005 | 0.025 | 0.836 |
| LA Volume Index (mLm2) | 0.089 | 0.021 | <0.001 | 0.214 | 0.074 | 0.009 |
| E/e' Ratio | 0.193 | 0.047 | <0.001 | 0.059 | 0.022 | 0.014 |
Adjusted for year-25 covariates: age, sex, race, educational years, body mass index, systolic blood pressure, use of anti-hypertensive medication, total cholesterol, HDL-cholesterol, use of lipid-lowering medication, diabetes mellitus, smoking status, alcohol consumption, and physical activity.
P-values adjusted for multiple comparisons using the Benjamini-Hochberg procedure.
CAC = coronary artery calcium; LA = left atrial LV = left ventricular; SE = standard error; Y25 = year-25 examination.
Exploratory Analysis of Change in CAC score and LV structure and function
From Y15 to Y25 examinations, 1,721 participants had no CAC in both assessments. Of those in the CAC change category, 488 (77%) had CAC score equals zero 10 years before. In a multivariable linear regression analysis, CAC score progression was independently related to increasing age, male sex, black race, higher systolic blood pressure, use of antihypertensive medication, higher total cholesterol, use of lipid lowering medication, diabetes mellitus, and current smoking, supplemental table 1.
Compared to individuals with any CAC at Y15 or Y25, those free of CAC from Y15 to Y25 demonstrated at Y25 lower LV mass index (93 ± 24 vs. 83 ± 20 g/m2, p < 0.001), lower LV end-diastolic volume (118 + 30 vs. 108 ± 28 mL p < 0,001), lower LV end-systolic volume (42 ± 16 vs. 46 ± 18 mL, p < 0.001), lower LV longitudinal strain reflecting better systolic function (−14.8 ± 2.4 vs. −15.2 ± 2.4%, p = 0.001), lower LA volume index (25.7 ± 7.6 vs. 24.8 ± 7.0 mL/m2, p = 003), and lower E/e’ ratio (8.0 ± 2.4 vs. 7.8 ± 2.2, p = 0.016), whereas no difference was found for LV ejection fraction, table 3.
Table 3.
Association of change in CAC score with LV structure and function at Y25
| 10-Years Free of CAC | Presence of CAC at Y15 or Y25 | p-value | |
|---|---|---|---|
| LV Mass index (g/m2) | 83 ± 20 | 93 ± 24 | <0.001 |
| LV End-Diastolic Volume (mL) | 108 ± 28 | 118 ± 30 | <0.001 |
| LV End-Systolic Volume (mL) | 42 ± 16 | 46 ± 18 | <0.001 |
| LV Ejection Fraction (%) | 62 ± 7 | 61 ± 8 | 0.350 |
| LV Longitudinal Strain (%) | −15.2 ± 2.4 | −14.8 ± 2.4 | 0.001 |
| LA Volume Index (mL/m2) | 24.8 ± 7.0 | 25.7 ± 7.6 | 0.003 |
| E/e' Ratio | 7.8 ± 2.2 | 8.0 ± 2.4 | 0.016 |
CAC = coronary artery calcium; LA = left atrial; LV = left ventricular; Y15 = year-15 examination; Y25 = year-25 examination
In the univariate linear regression analysis, higher change in CAC score was significantly associated with higher LV mass index (adjusted-p = 0.002), higher LV end-diastolic and systolic volumes (adjusted-p=0.002 for both), higher LV longitudinal strain reflecting worse systolic function (adjusted-p=0.002), higher LA volume index (adjusted-p=0.007), and higher E/e’ ratio (adjusted-p=0.004). LV ejection fraction was not significantly related to CAC score (adjusted-p = 0.119).
After adjusting for Y15 demographics and cardiovascular risk factors, 10-year change in risk factors, and chronic risk exposure to the model, only the association of higher change in CAC score with higher LV mass index remained statistically significant (β=2.508, adjusted-p= .007), table 4.
Table 4.
Multivariable linear regression models for the association of change in log-transformed CAC score and LV structure and function
| Univariate Analysis | Multivariable Analysis* | |||||
|---|---|---|---|---|---|---|
| Coefficient | SE | Adjusted p- values† |
Coefficient | SE | Adjusted p-values† |
|
| LV Mass Index (g/m2) | 6.919 | 0.742 | 0.002 | 2.508 | 0.771 | 0.007 |
| LV End-Diastolic Volume (mL) | 6.879 | 0.987 | 0.002 | 2.118 | 0.938 | 0.082 |
| LV End-Systolic Volume (mL) | 3.174 | 0.574 | 0.002 | 1.220 | 0.577 | 0.082 |
| LV Ejection Fraction (%) | −0.387 | 0.249 | 0.119 | −0.416 | 0.279 | 0.238 |
| LV Longitudinal Strain (%) | 0.333 | 0.085 | 0.002 | 0.091 | 0.091 | 0.317 |
| LA Volume Index (mLm2) | 0.655 | 0.239 | 0.007 | 0.299 | 0.269 | 0.310 |
| E/e' Ratio | 0.227 | 0.076 | 0.004 | 0.095 | 0.079 | 0.310 |
Adjusted for year-15 covariates (age, sex, race, educational years, body mass index, systolic blood pressure, use of anti-hypertensive medication, total cholesterol, HDL-cholesterol, use of lipid-lowering medication, diabetes mellitus, smoking status, alcohol consumption, physical activity) and for chronic risk exposure and 10-year change in risk factors.
P-values adjusted for multiple comparisons using the Benjamini-Hochberg procedure.
CAC = coronary artery calcium; LA = left atrial LV = left ventricular; SE = standard error; Y25 = year-25 examination.
Race and Sex Differences
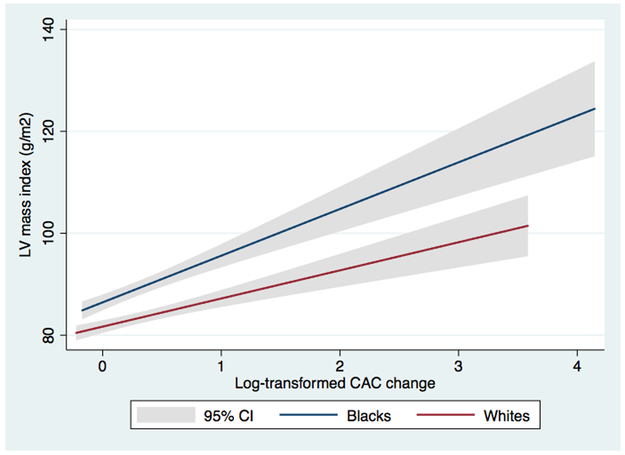
A significant interaction between race and both CAC score and change in CAC score in the multivariable linear regression models for LV mass index was found. In a stratified analysis by race, blacks showed a synergistic interaction with CAC score at Y25, with higher β-coefficients in the association of log-transformed CAC score with LV mass (β = 2.071, SE = 0.339, p < 0.001) compared to whites (β = 0.539, SE = 0.271, p = 0.047) at Y25. While the relationship of change in CAC score with LV mass index was significant in blacks (β = 4.789, SE = 1.263, p < 0.001), but not in whites (β = 1.051, SE = 0.979, p = 0.283), figure 1.
Figure 1.
Linear regression analysis of the relationship between change in coronary artery calcium score and left ventricular mass index stratified by race. CAC = coronary artery calcim; CI = confidence interval; LV = left ventricular.
Race difference was also found in the multivariable linear regression model for the association of CAC score at Y25 and E/e’ ratio, which was significant in blacks (β = 0.108, SE = 0.037, p = 0.004), but not in whites (β = 0.027, SE = 0.027, p = 0.398).
Interaction terms of sex and CAC were not statistically significant.
DISCUSSION
This study reports the relationship between both CAC score and change in CAC from young adulthood to middle age with LV structure and function assessed by two-dimensional echocardiography in an asymptomatic large biracial cohort. Independent associations of higher CAC score with higher LV mass index, higher LV volumes, higher LV filling pressures, and higher LA volume index were found in individuals at middle age. Moreover, in an exploratory analysis, individuals free of CAC over 10 years of follow-up demonstrated lower LV mass and volumes, as well as better echocardiographic indices of LV systolic and diastolic function. After adjusting for baseline (Y15) demographics and cardiovascular risk factors, 10-year change in risk factors, and chronic risk exposure, higher CAC score remained independently related to higher LV mass index. Furthermore, we found race differences in the relationship between CAC and adverse cardiac remodeling. A synergistic interaction was found between black race and CAC score at Y25 on both LV mass index and LV filling pressures. Of note, in a stratified analysis, change in CAC was related to higher LV mass in blacks, but not in whites.
The association of higher levels of CAC with LV mass was a prominent finding in our study. Previously, Tong et al. reported a significant correlation between higher CAC with an increase in LV mass index in an investigation including 159 African-American individuals 12. Also, Madaj et al. showed a significant relationship between CAC and LV mass both assessed by CT in 230 healthy subjects 13. In the CARDIA study, Gardin et al. exhibited an independent association of LV mass at year-5 and positive CAC at Y15 14. Our findings are consistent with these results, and importantly extend them by demonstrating independent association of change in CAC score with higher LV mass index in African Americans over 10 years of follow-up.
The observed relationship between CAC with LV mass, at least in part, may result from a potential increase of LV filling pressures due to silent ischemia in individuals with higher burden of coronary atherosclerosis, marked by higher and progressive levels of CAC. Supporting this hypothesis, our results also show association of CAC score and CAC progression with higher LV filling pressures and higher LA volume index, a marker of chronic elevation in LV diastolic pressures.
Of note, LVEF was not associated with CAC score or change in CAC score. However, individuals with higher CAC score had worse LV myocardial strain, suggesting subclinical LV systolic impairment. The relationship of subclinical atherosclerosis and LV strain was shown in prior studies using cardiovascular magnetic resonance imaging. In the MESA study cohort, Fernandes et al. demonstrated a relationship between higher carotid intima-medial thickness with worse segmental myocardial strain in asymptomatic individuals 7. Also in the MESA study cohort, Edvardsen et al. found a reduction in segmental myocardial strain assessed by MRI associated with higher CAC score in individuals with no history of heart disease. Similar to our study, LVEF was not correlated with CAC score 6. Using SPECT imaging, Anand et al. showed association of higher CAC score and more incidence of myocardial perfusion abnormalities reflecting silent myocardial ischemia in those with CAC score ≥ 400 15. Another potential pathway to explain the relationship of CAC with LV impairment, even in the absence of obstructive coronary artery disease, might be increased peripheral resistance, endothelial dysfunction, and microembolization secondary to plaque rupture.16
Progression of CAC score is associated with traditional cardiovascular risk factors and increased risk for future cardiovascular events.4, 5, 17 In a prior study of this CARDIA cohort, Gidding et al. reported that increase in CAC appears to be driven by baseline and change in cardiovascular risk over time.18 Therapeutic interventions for cardiovascular risk control, including statin therapy, have not been shown to slow progression of CAC, despite lowering overall risk, which may reflect a plaque healing response to plaque stabilizing therapies 4, 19 In a recent study, CAC progression was not associated with cardiovascular disease after adjustment for the follow-up CAC, suggesting that if a serial CAC score is performed, the latest examination should be used for risk assessment.20 Our findings showed that, after adjusting for 10-year change in risk factors and chronic risk exposure, change in CAC score remained related to higher LV mass index, although such association might be explained, at least in part, by the relationship between positive CAC at Y15 and higher LV mass index at Y25.
Importantly, the relationship between change in CAC score and LV mass index was significant only in blacks. Moreover, black race had a synergistic interaction with CAC score at Y25 in the model for LV mass index, while higher LV filling pressures was significantly related to higher CAC at Y25 only in blacks. Race-differences in cardiac structure and function, as well as in cardiovascular mortality have been reported.21, 22 The reason for the greater propensity for adverse cardiac remodeling and cardiovascular events among blacks is not fully understood. Genetic factors and environmental exposures might be implicated in different cardiac remodeling pathways.
Finally, participants who remained free of CAC in this period of time exhibited at middle age lower LV volumes, lower LV mass, and better systolic and diastolic functions compared to those with CAC identified 10 years earlier. In prior study, a CAC score of zero was associated with a low risk of mortality, which persists for more than 15 years, especially for individuals younger than 60 years.23
LIMITATIONS
M-mode-derived LV mass was calculated using Devereux formula, which can be less accurate in the setting of greater heterogeneity of segmental wall thickness or abnormal LV shape. Nevertheless, M-mode-derived LV mass is a simple and quick measure, and subject to less measurement variability, which are important advantages to study large populations, such as CARDIA. Furthermore, most studies that associate LV mass to adverse cardiovascular events are based on this method. The lack of echocardiographic assessment at Y15 is a caveat regarding the interpretation of the results from the exploratory analysis of the relationship between change in CAC score and echocardiographic parameters at Y25. Cross-sectional associations between CAC and cardiac parameters at Y25 might have existed at Y15, hence impacting on the subsequent changes and the associations detected at Y25.
CONCLUSIONS
In middle age, higher CAC score were associated with cardiac adverse remodeling, independent of demographics and traditional cardiovascular risk factors. In comparison with individuals who remained free of CAC from young adulthood to middle age, those with change in CAC score demonstrated higher LV mass and volumes, and worse LV myocardial deformation and diastolic function at middle age. After adjusting for 10-year change in risk factors and chronic risk exposure, change in CAC score remained independently related to higher LV mass index in blacks, but not in whites.
Supplementary Material
CLINICAL PERSPECTIVE.
Coronary artery calcium (CAC) score is related to the presence and extent of coronary artery disease and is a risk marker of cardiovascular events. Middle age is a period when subclinical left ventricular (LV) impairment may be observed prior to an increase in cardiovascular events. Our study showed that, in individuals at middle age, CAC score is independent related to echocardiographic markers of adverse cardiac remodeling. Furthermore, individuals free of CAC over 10 years of follow-up, from young adulthood to middle age, had better echocardiographic indices of cardiac structure and diastolic function at middle age. Of note, higher increase in CAC score over the follow-up period was independently related to higher LV mass index. Importantly, black race showed a significant interaction on the relationship between higher CAC at middle age and higher LV mass index, while CAC score progression was independently related to higher LV mass in blacks, but not in whites. Taken together, these findings suggest that a strict cardiovascular risk factors control, starting during young adulthood, may result in better cardiovascular function at middle age, especially in black individuals.
Acknowledgments
SOURCES OF FUNDING
The CARDIA study is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging (NIA), and an intra-agency agreement between NIA and NHLBI (AG0005).
Footnotes
DISCLAIMER
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the NHLBI; the NIH; or the U.S. Department of Health and Human Services.
DISCLOSURES
None.
REFERENCES
- 1.Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–1402. [DOI] [PubMed] [Google Scholar]
- 2.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr., Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. [DOI] [PubMed] [Google Scholar]
- 3.Carr JJ, Jacobs DR Jr., Terry JG, Shay CM, Sidney S, Liu K, Schreiner PJ, Lewis CE, Shikany JM, Reis JP, Goff DC Jr. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years With Incident Coronary Heart Disease and Death. JAMA Cardiol. 2017;2:391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McEvoy JW, Blaha MJ, Defilippis AP, Budoff MJ, Nasir K, Blumenthal RS, Jones SR. Coronary artery calcium progression: an important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56:1613–1622. [DOI] [PubMed] [Google Scholar]
- 5.Budoff MJ, Young R, Lopez VA, Kronmal RA, Nasir K, Blumenthal RS, Detrano RC, Bild DE, Guerci AD, Liu K, Shea S, Szklo M, Post W, Lima J, Bertoni A, Wong ND. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2013;61:1231–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edvardsen T, Detrano R, Rosen BD, Carr JJ, Liu K, Lai S, Shea S, Pan L, Bluemke DA, Lima JA. Coronary artery atherosclerosis is related to reduced regional left ventricular function in individuals without history of clinical cardiovascular disease: the Multiethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2006;26:206–211. [DOI] [PubMed] [Google Scholar]
- 7.Fernandes VR, Polak JF, Edvardsen T, Carvalho B, Gomes A, Bluemke DA, Nasir K, O’Leary DH, Lima JA. Subclinical atherosclerosis and incipient regional myocardial dysfunction in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis (MESA). J Am Coll Cardiol. 2006;47:2420–2428. [DOI] [PubMed] [Google Scholar]
- 8.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR Jr., Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. [DOI] [PubMed] [Google Scholar]
- 9.Moreira HT, Nwabuo CC, Armstrong AC, Kishi S, Gjesdal O, Reis JP, Schreiner PJ, Liu K, Lewis CE, Sidney S, Gidding SS, Lima JAC, Ambale-Venkatesh B. Reference Ranges and Regional Patterns of Left Ventricular Strain and Strain Rate Using Two-Dimensional Speckle-Tracking Echocardiography in a Healthy Middle-Aged Black and White Population: The CARDIA Study. J Am Soc Echocardiogr. 2017;30:647–658 e642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong AC, Ricketts EP, Cox C, Adler P, Arynchyn A, Liu K, Stengel E, Sidney S, Lewis CE, Schreiner PJ, Shikany JM, Keck K, Merlo J, Gidding SS, Lima JA. Quality Control and Reproducibility in M-Mode, Two-Dimensional, and Speckle Tracking Echocardiography Acquisition and Analysis: The CARDIA Study, Year 25 Examination Experience. Echocardiography. 2015;32:1233–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronmal RA, McClelland RL, Detrano R, Shea S, Lima JA, Cushman M, Bild DE, Burke GL. Risk factors for the progression of coronary artery calcification in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2007;115:2722–2730. [DOI] [PubMed] [Google Scholar]
- 12.Tong W, Lima JA, Lai H, Celentano DD, Dai S, Lai S. Relation of coronary artery calcium to left ventricular mass in African-Americans. Am J Cardiol. 2004;93:490–492. [DOI] [PubMed] [Google Scholar]
- 13.Madaj PM, Pagali SR, Hamirani YS, Raina S, Nair S, Zeb I, Mao S, Budoff MJ. Coronary artery calcium and plaque association with left ventricular mass, assessed by multi-row detector computed tomography. Coron Artery Dis. 2010;21:428–434. [DOI] [PubMed] [Google Scholar]
- 14.Gardin JM, Iribarren C, Detrano RC, Liu K, Schreiner PJ, Loria CM, Wong ND. Relation of echocardiographic left ventricular mass, geometry and wall stress, and left atrial dimension to coronary calcium in young adults (the CARDIA study). Am J Cardiol. 2005;95:626–629. [DOI] [PubMed] [Google Scholar]
- 15.Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, Lipkin D, Lahiri A. Risk stratification in uncomplicated type 2 diabetes: prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713–721. [DOI] [PubMed] [Google Scholar]
- 16.Wang L, Jerosch-Herold M, Jacobs DR Jr., Shahar E, Detrano R, Folsom AR. Coronary artery calcification and myocardial perfusion in asymptomatic adults: the MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2006;48:1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raggi P, Callister TQ, Shaw LJ. Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapy. Arterioscler Thromb Vasc Biol. 2004;24:1272–1277. [DOI] [PubMed] [Google Scholar]
- 18.Gidding SS, Rana JS, Prendergast C, McGill H, Carr JJ, Liu K, Colangelo LA, Loria CM, Lima J, Terry JG, Reis JP, McMahan CA. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Risk Score in Young Adults Predicts Coronary Artery and Abdominal Aorta Calcium in Middle Age: The CARDIA Study. Circulation. 2016;133:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah PK. Temporal Change in CAC Score and Prognosis: Follow-Up Score Is Simpler and as Good as a Change in Score. JACC Cardiovasc Imaging. 2016;9:1430–1431. [DOI] [PubMed] [Google Scholar]
- 20.Radford NB, DeFina LF, Barlow CE, Lakoski SG, Leonard D, Paixao AR, Khera A, Levine BD. Progression of CAC Score and Risk of Incident CVD. JACC Cardiovasc Imaging. 2016;9:1420–1429. [DOI] [PubMed] [Google Scholar]
- 21.Pool LR, Ning H, Lloyd-Jones DM, Allen NB. Trends in Racial/Ethnic Disparities in Cardiovascular Health Among US Adults From 1999–2012. J Am Heart Assoc. 2017;6:e006027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kishi S, Reis JP, Venkatesh BA, Gidding SS, Armstrong AC, Jacobs DR Jr., Sidney S, Wu CO, Cook NL, Lewis CE, Schreiner PJ, Isogawa A, Liu K, Lima JA. Race-ethnic and sex differences in left ventricular structure and function: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Am Heart Assoc. 2015;4:e001264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Valenti V, B OH, Heo R, Cho I, Schulman-Marcus J, Gransar H, Truong QA, Shaw LJ, Knapper J, Kelkar AA, Sandesara P, Lin FY, Sciarretta S, Chang HJ, Callister TQ, Min JK. A 15-Year Warranty Period for Asymptomatic Individuals Without Coronary Artery Calcium: A Prospective Follow-Up of 9,715 Individuals. JACC Cardiovasc Imaging. 2015;8:900–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The CARDIA Study has provided National Heart, Lung and Blood Institute (NHLBI) Data Repository Datasets for exams conducted during Years 0–25, as well as for follow-up contacts for which data collection has been completed for at least five years, and for adjudicated morbid and mortal events. The NHLBI distributes these data; additional information, including the procedures on how to request these data, can be found on the NHLBI web site: biolincc.nhlbi.nih.gov/studies/cardia/