Key Points
Question
Is physical therapy noninferior to early surgery with arthroscopic partial meniscectomy for improving knee function among patients with nonobstructive meniscal tears?
Findings
In this noninferiority randomized clinical trial that included 321 patients, knee function that was measured by a self-administered questionnaire improved by 20.4 points in the physical therapy group vs 26.2 points in the early surgery group over a follow-up period of 24 months. The difference between the 2 treatment groups did not exceed the noninferiority margin of 8 points.
Meaning
These results demonstrate noninferiority of physical therapy compared with early surgery with arthroscopic partial meniscectomy for improving self-reported knee function in patients with nonobstructive meniscal tears.
Abstract
Importance
Despite recent studies suggesting arthroscopic partial meniscectomy (APM) is not more effective than physical therapy (PT), the procedure is still frequently performed in patients with meniscal tears.
Objective
To assess whether PT is noninferior to APM for improving patient-reported knee function in patients with meniscal tears.
Design, Setting, and Participants
Noninferiority, multicenter, randomized clinical trial conducted in 9 hospitals in the Netherlands. Participants were aged 45 to 70 years with nonobstructive meniscal tears (ie, no locking of the knee joint). Patients with knee instability, severe osteoarthritis, and body mass index greater than 35 were excluded. Recruitment took place between July 17, 2013, and November 4, 2015. Participants were followed up for 24 months (final participant follow-up, October 11, 2017).
Interventions
Three hundred twenty-one participants were randomly assigned to APM (n = 159) or a predefined PT protocol (n = 162). The PT protocol consisted of 16 sessions of exercise therapy over 8 weeks focused on coordination and closed kinetic chain strength exercises.
Main Outcomes and Measures
The primary outcome was change in patient-reported knee function on the International Knee Documentation Committee Subjective Knee Form (range, 0 to 100; from worse to best) from baseline over a 24-month follow-up period. The noninferiority margin was defined as a difference between treatment groups of 8 points and was assessed with a 1-sided α of .025. The primary analysis followed the intention-to-treat principle.
Results
Among 321 patients who were randomized (mean [SD] age, 58 [6.6] years; 161 women [50%]), 289 (90%) completed the trial (161 women and 158 men). In the PT group, 47 participants (29%) had APM during the 24-month follow-up period, and 8 participants randomized to APM (5%) did not have APM. Over a 24-month follow-up period, knee function improved in the APM group by 26.2 points (from 44.8 to 71.5) and in the PT group by 20.4 points (from 46.5 to 67.7). The overall between-group difference was 3.6 points (97.5% CI, −∞ to 6.5; P value for noninferiority = .001). Adverse events occurred in 18 participants in the APM group and 12 in the PT group. Repeat surgery (3 in the APM group and 1 in the PT group) and additional outpatient visits for knee pain (6 in the APM group and 2 in the PT group) were the most frequent adverse events.
Conclusions and Relevance
Among patients with nonobstructive meniscal tears, PT was noninferior to APM for improving patient-reported knee function over a 24-month follow-up period. Based on these results, PT may be considered an alternative to surgery for patients with nonobstructive meniscal tears.
Trial Registration
ClinicalTrials.gov Identifier: NCT01850719
This noninferiority trial compares the effects of arthroscopic partial meniscectomy vs physical therapy on patient-reported knee function in patients with meniscal tears.
Introduction
Arthroscopic partial meniscectomy (APM) is among the most frequently performed procedures in orthopedic surgery. It was estimated that in 2014, 516 800 meniscectomies were performed in the United States, and the global annual cost was estimated at $4 billion in 2006.1,2
Meniscal tears may occur as part of a degenerative process of the knee joint and occur in up to 60% of persons older than 50 years of age without knee pain.3 Because physical therapy (PT) has positive short-term effects on knee pain and function in patients with knee osteoarthritis,4 the benefit of surgical resection of the degenerative meniscal tear compared with PT is unclear.5
To date, 6 randomized clinical trials (RCTs) have assessed superiority of APM compared with either PT6,7,8,9,10 or sham surgery2 in patients with a confirmed meniscal tear. These trials reported no significant differences between treatment groups for knee function. A meta-analysis that included data from 5 RCTs found a statistically significant benefit of APM for knee function and pain at up to 6-month follow-up, but this benefit did not persist at 1- or 2-year follow-up.5,11 Evidence published to date has not led to a major decline in APM for managing meniscal tears.5,12
Therefore, the objective of this study was to determine whether PT is noninferior to APM for improving self-reported knee function over a 24-month follow-up period in patients with nonobstructive meniscal tears.
Methods
Trial Oversight and Design
This trial was a noninferiority, multicenter RCT performed in 9 hospitals in the Netherlands, comparing APM with PT in patients with meniscal tears. The study protocol has been published13 and is available with the statistical plan in Supplement 1. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Research Ethics Committees United (MEC-U; NL44188.100.13) and by the board of directors of each of the participating hospitals. All participants provided written informed consent prior to randomization. The number of patients screened for eligibility was not documented.
Patient Population
Participants aged 45 to 70 years who were referred to 1 of 9 participating hospitals with knee pain and a nonobstructive (ie, no locking of the knee joint) meniscal tear confirmed by magnetic resonance imaging (MRI) were eligible for inclusion. Exclusion criteria were locking of the knee, prior knee surgery, instability caused by an anterior or posterior cruciate ligament rupture, severe osteoarthritis (Kellgren-Lawrence score of 4, indicating large osteophytes, marked joint-space narrowing, severe sclerosis, and definite bone ends deformity),14 and a body mass index (BMI, calculated as weight in kilograms divided by height in meters squared) greater than 35. No distinction was made between traumatic and degenerative tears because in older patients, even traumatic tears may be related to degenerative changes in the knee. Recruitment was carried out between July 17, 2013, and November 4, 2015. Follow-up testing was completed on October 11, 2017.
Intervention, Randomization, and Blinding
Patients with a meniscal tear were informed about the study by their treating orthopedic surgeon at their first outpatient visit. After written informed consent was obtained, the research coordinator randomized study participants to APM or PT. Randomization was concealed and performed using a central computer-generated randomization scheme in a 1:1 ratio with variable block size (minimum block size of 2 and maximum block size of 6). Randomization was stratified by hospital and by age (45-57 and 58-70 years). Participants, physicians, and physical therapists were not blinded. Investigators who performed the statistical analysis were blinded. After the analysis was completed, data were unblinded for the final interpretation of the results.
Participants randomized to APM were scheduled for surgery within 4 weeks of randomization. Surgery was performed in an outpatient clinic under general or spinal anesthesia. During surgery, standard anteromedial and anterolateral portals were introduced for inspection of the knee joint. The affected meniscus was partially removed until a stable and solid meniscus remained. All participants received perioperative instructions and a home exercise program. Participants were only referred to PT after APM if they did not recover as anticipated (ie, they did not adequately improve or experienced a decrease in knee function, ability to participate in daily activities, and/or had an increase in knee pain), as defined by the Dutch Orthopedic Association guideline.15
Participants randomized to PT were referred to PT clinics directly after randomization and their initial PT session was scheduled within 2 weeks after randomization. Participating PT clinics were instructed about the exercise protocol by a knee-specialized physical therapist or the primary investigator, prior to the first participant’s referral. The PT exercise protocol was developed by a knee-specialized physical therapist and consisted of 16 sessions of 30 minutes each conducted over 8 weeks (eFigure 1 in Supplement 2). The PT protocol included cardiovascular, coordination/balance, and closed kinetic chain strength exercises (in which the distal part of the extremity is fixed to an object that is stationary). If PT failed (eg, knee pain or limitations in daily activities persisted or locking occurred), the participant could attend additional PT sessions or have APM, depending on their preference.
Outcomes
The primary outcome was the change in patient-reported knee function on the Subjective Knee Form of the International Knee Documentation Committee (IKDC) from baseline over 24 months. The IKDC is a validated and self-administered questionnaire designed for patients with a variety of knee disorders that assesses knee function, symptoms, and ability to engage in sports activities.16,17,18 IKDC scores range from 0 to 100, in which 100 indicates no knee symptoms or limitations in daily or sporting activities. Normative values for the IKDC in the United States are 88 (SD, 14) for men aged 51 to 65 years and 85 (SD, 16) for women aged 51 to 65 years in a population without current knee problems or a history of knee surgery. In a population of people with and without current knee problems, the normative scores are 77 (SD, 23) for men aged 51 to 65 years and 71 (SD, 26) for women aged 51 to 65 years.19
Because a minimal clinically important difference (MCID) for the IKDC has not been defined in a population consisting only of patients with meniscal tears, the noninferiority margin was defined as the smallest detectable change of 8.8 points,17 rounded down to a margin of 8 points.
Secondary outcomes included knee pain during weight-bearing, general health, the progression of osteoarthritis, and activity level. Knee pain during weight-bearing was measured on a visual analog scale (VAS20; range, 0-100, with 0 anchored as “no pain” and 100 as “worst pain imaginable”). General health was measured with the RAND-36 Physical Component Score, derived from the RAND-36 questionnaire21 (range, 0-100, with higher scores indicating better health). The mean (SD) score in the general population is 50 (10).21 Progression of osteoarthritis was measured using the Kellgren-Lawrence classification (range, 0-4, in which grade 0 [no osteophytes or joint-space narrowing] indicates no osteoarthritis and grade 4 [>50% joint-space narrowing] indicates severe osteoarthritis).14 Activity level was measured with the Tegner Activity Scale, which measures the level of working activities and sport activities on a scale from 0 to 10, with higher scores indicating a higher level of activity.22 Although these outcomes were originally intended to test for noninferiority, no noninferiority margins were defined in advance. Therefore, the secondary outcomes were tested for superiority. After data analyses, MCIDs were identified in the literature to guide interpretation of observed differences between treatment groups. Adverse events were categorized as serious and nonserious.
Other prespecified outcomes included resource utilization, health-related quality of life, patient-specific complaints, participant expectations, and participant satisfaction. These outcomes will be analyzed and reported separately.
Participants completed study questionnaires at baseline, and at 3, 6, 12, and 24 months after randomization. If participants did not respond, up to 3 reminders were sent and, if needed, the participant was contacted by telephone.
MRIs and x-rays were taken at the time of enrollment and x-rays were performed 24 months after randomization. One radiologist reviewed all x-rays to grade osteoarthritis severity on the Kellgren-Lawrence classification,14 while another radiologist reviewed all MRIs for classification of the meniscal tears according to the Modified International Cartilage Repair Society classification.23 Both radiologists were unable to assess whether a participant had surgery and were blinded to treatment allocation.
Sample Size Calculation and Statistical Analysis
The sample size was based on an SD of 18 points on the IKDC, a power of 90%, a 2-sided α of .05, and a noninferiority margin of 8 points on the IKDC. With an anticipated 20% loss to follow-up and a 25% delayed APM rate after 24 months, 160 participants per treatment group were needed.
Mixed models were used for longitudinal data analyses, with a 3-level structure, ie, repeated measurements were clustered within participants and participants were clustered within the participating centers, to calculate the overall between-group differences. Unadjusted between-group differences were calculated based on a model with the baseline score and treatment group as independent variables. To define the between-group differences per follow-up period, time was added to the model as a categorical variable, as well as a time-by-treatment interaction. Adjusted between-group differences were calculated based on similar models including potential confounders as independent variables. These confounders were sex, age, BMI, education level,24 Kellgren-Lawrence classification,14 location of tear (medial, lateral, both), mechanical complaints, and baseline knee pain during weight-bearing.
Progression of osteoarthritis was analyzed using a mixed model with Kellgren-Lawrence score at 24 months as the dependent variable and intervention group and baseline Kellgren-Lawrence score as independent variables. Analyses followed the intention-to-treat principle, in which patients were analyzed according to their randomized treatment allocation, regardless of any deviations from the protocol.
To test the robustness of the results, analyses that followed the as-treated principle were performed for the unadjusted and adjusted between-group differences for the outcomes of knee function and pain. In these analyses, participants were analyzed based on their adherence to randomized treatment allocation in 3 groups: (1) participants randomized to the APM group who received APM, (2) participants randomized to the PT group who completed the PT protocol without having APM during the follow-up period, and (3) participants randomized to the PT group who had APM during follow-up (delayed APM group). Patients who were randomized to the APM treatment group but did not have surgery and patients who were randomized to PT but did not complete the PT protocol and did not have delayed APM were not included in the as-treated analysis.
Adverse events were reported descriptively. Post hoc exploratory analyses were performed to assess effect modification on the primary outcome, by evaluating the interaction term between each of the potential confounders listed above.
A 97.5% CI (ie, a 1-sided α of .025) was used for the knee function outcome, whereas a 95% CI (ie, a 2-sided α of .05) was used for the other outcomes. Because the analyses for the secondary outcomes were not corrected for type 1 error, they should be considered exploratory.
Noninferiority was demonstrated when the 97.5% CI did not include the noninferiority margin. Missing data were handled using full maximum likelihood estimation. If participants withdrew from the trial, the data collected prior to withdrawal were used in the analyses, with the participant’s approval. All analyses were conducted using IBM SPSS version 22 (IBM).
Deviations From the Original Trial Protocol
Four inconsistencies with the original protocol need to be addressed (Supplement 1). First, the power calculation was adjusted after an interim analysis of the first 100 participants’ IKDC scores at 1-year follow-up, which demonstrated that the SD was 18 points compared with the anticipated 20 points derived from Crawford and colleagues17 used in the sample size calculation. This allowed for a reduction of the sample size from 402 to 320.
Second, the description of the primary outcome in the original protocol was the change from baseline to 24-month follow-up. However, the trial was designed to include all follow-up time points in the primary outcome measure and, therefore, the originally intended primary outcome measure was the change from baseline over 24-month follow-up. This was not explicitly specified in the protocol.
Third, the original protocol described generalized estimating equations for longitudinal analyses. During the study, and more than a year prior to data analysis, statistical consultation indicated that a mixed-model approach was more suitable for our data set. The advantages of a mixed-model analysis over generalized estimating equations are the ability to correct for recruitment center without significant loss of power and the ability to handle missing data using maximum likelihood estimation without the need for imputation.
Fourth, an error was made in the protocol as it mentions a loss to follow-up of 10%, while the anticipated percentage was 20%.
Results
Participants
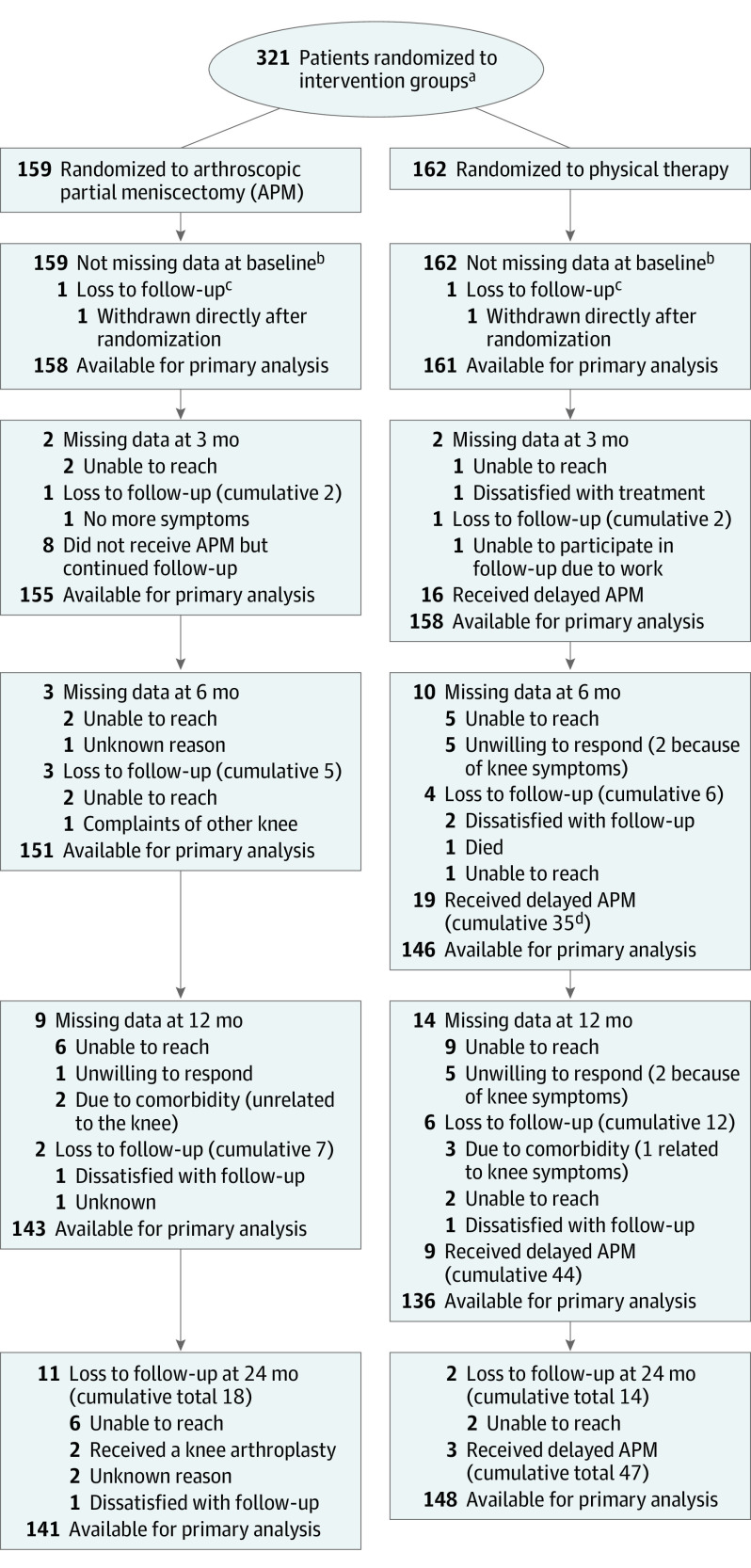
Between July 17, 2013, and November 4, 2015, 321 participants were enrolled and randomly assigned to APM (n = 159) or PT (n = 162; Figure 1). Two participants (1 in each group) withdrew consent immediately after randomization without providing a reason. After 24 months, 289 participants (90%) completed follow-up, with the final participant’s follow-up visit occurring on October 11, 2017. The baseline characteristics in the 2 treatment groups were comparable (mean [SD] age, 58 [6.6] years; 161 women (50%); Table 1). The distributions of baseline knee function and knee pain during weight-bearing are presented in eFigures 2 and 3 in Supplement 2.
Figure 1. Flow of Patients Through the ESCAPE Trial.
aThe number of patients screened for eligibility was not available.
bMissing data refer to data that were missing at a specific time point, while patients remained available for the remaining follow-up times.
cLoss to follow-up refers to actual dropout from the study; eg, patients who did not participate at any of the remaining time points (cumulative numbers are total number of dropouts).
dCumulative number of delayed APM refers to total number of participants from the physical therapy group who received delayed APM from baseline until that follow-up.
Table 1. Baseline Characteristics of the Intention-to-Treat Population.
| No. (%) | ||
|---|---|---|
| APM Group (n = 158) |
PT Group (n = 161) |
|
| Demographics | ||
| Age, mean (SD), y | 57.6 (6.5) | 57.3 (6.8) |
| Women | 80 (50.6) | 81 (50.3) |
| Right knee | 88 (55.7) | 81 (50.3) |
| Education level, beyond high schoola | 67 (42.4) | 86 (53.4) |
| BMI, mean (SD) | 26.7 (3.8) | 27.2 (4.0) |
| 18.5<BMI<25 | 56 (35.4) | 53 (32.9) |
| 25≤BMI<30 | 72 (45.6) | 67 (41.6) |
| 30≤BMI<35 | 30 (19.0) | 41 (25.5) |
| Mechanical complaintsb | 56 (35.4) | 67 (41.6) |
| Imagingc | ||
| Affected meniscus | ||
| Medial | 126 (79.7) | 136 (84.5) |
| Lateral | 30 (19.0) | 25 (15.5) |
| Both | 2 (1.3) | 0 (0) |
| Type of tear on MRI (ISAKOS23) | n = 151 | n = 152 |
| Longitudinal-vertical | 5 (3.3) | 5 (3.3) |
| Horizontal | 80 (53.0) | 69 (45.4) |
| Complex degenerative | 47 (31.1) | 58 (38.1) |
| Radial | 13 (8.6) | 10 (6.6) |
| Vertical flap | 2 (1.3) | 5 (3.3) |
| Unclassifiable | 1 (0.7) | 5 (3.3) |
| Horizontal flap | 3 (2.0) | 0 (0) |
| Osteoarthritis score on radiographs (KL classification14)d | n = 150 | n = 149 |
| 0: None | 18 (12.0) | 15 (10.1) |
| 1: Doubtful | 81 (54.0) | 74 (49.7) |
| 2: Minimal | 45 (30.0) | 55 (36.9) |
| 3: Moderate | 6 (4.0) | 5 (3.3) |
| Knee Function and Pain | ||
| Knee function | ||
| IKDC score (0 [most limitations] to 100 [no limitations]), mean (SD)e | 44.8 (16.6) | 46.5 (14.6) |
| Knee pain | n = 145 | n = 151 |
| VAS during weight-bearing (0 [no pain] to 100 [worst pain imaginable]), median (IQR)f | 61.1 (44.9-83.4) | 59.3 (44.9-77.4) |
Abbreviations: APM, arthroscopic partial meniscectomy; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IKDC, International Knee Documentation Committee; IQR, interquartile range; ISAKOS, International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine; KL, Kellgren-Lawrence; MRI, magnetic resonance imaging; PT, physical therapy; VAS, visual analog scale.
Education level was measured according to the International Standard Classification of Education (ISCED) and dichotomized to low (ISCED level 0-3; eg, early childhood education, primary education, or high school) or high (ISCED level 4-8; eg, any education beyond high school, including bachelor’s, master’s, or doctoral degree).24
In contrast to locking of the knee joint, which was an exclusion criterion, mechanical complaints, such as clicking or catching, were allowed for inclusion.
All participants underwent MRI prior to inclusion, and information on the affected meniscus was based on clinical readings by different radiologists and orthopedic surgeons in participating centers. The type of tear was based on post-hoc readings of the MRIs by one radiologist, and osteoarthritis scores were based on study readings of the MRIs by one other radiologist. Some radiographs and MRIs were unavailable (8 and 7 for APM and 12 and 9 for PT, respectively) for study readings.
KL grade 0 (no osteophytes or joint-space narrowing) indicates no osteoarthritis, grade 1 (questionable osteophytes) indicates early-onset osteoarthritis, grade 2 (definite osteophytes, possible joint-space narrowing) indicates mild osteoarthritis, grade 3 (moderate osteophytes, definite joint-space narrowing, some sclerosis, possible bone-end deformity) indicates moderate osteoarthritis, and grade 4 (large osteophytes, marked joint-space narrowing, severe sclerosis, definite bone ends deformity) indicates severe osteoarthritis.14 KL grade 4 was an exclusion criterion.
IKDC scores range from 0 to 100, in which 0 indicates the highest level of knee symptoms and lowest level of function in daily or sporting activities, and 100 indicates the lowest knee symptoms and highest level of function in daily or sporting activities. Normative mean (SD) values for the IKDC in the United States are 88 (14) for men aged 51 to 65 years and 85 (16) for women aged 51 to 65 years in a population without current knee problems or a history of knee surgery. In a mixed population of people with and without current knee problems, the normative mean (SD) scores are 77 (23) for men aged 51 to 65 years and 71 (26) for women aged 51 to 65 years.19 For example, a patient scores 50.6 on the IKDC if the highest level of activities and the effect of the knee on activities are graded as “moderate” for all asked activities, the level of knee pain is “moderate” (5 of 11), mechanical complaints are absent, and the current knee function is graded as “moderate” (5 of 11).
VAS score ranged from 0 to 100, and was anchored as 0 indicating no pain and 100 indicating maximum pain.
Eight participants (5%) of the APM group chose not to have surgery because they determined their symptoms were not severe enough for surgical management. Four of these participants attended a mean of 14.5 PT sessions (range, 6-23), while the other 4 did not receive PT. Two participants in the APM group had a total knee arthroplasty within 2 years of their APM.
Participants in the PT group attended a mean of 17 PT sessions (range, 0-40). In the PT group, 47 participants (29%) had APM due to the persistence of symptoms, and 35 (75%) had APM within 6 months of randomization. Three participants in the PT group had a total knee arthroplasty within the 24-month follow-up period. Seventeen participants did not complete the PT protocol (<16 sessions).
Primary Outcome
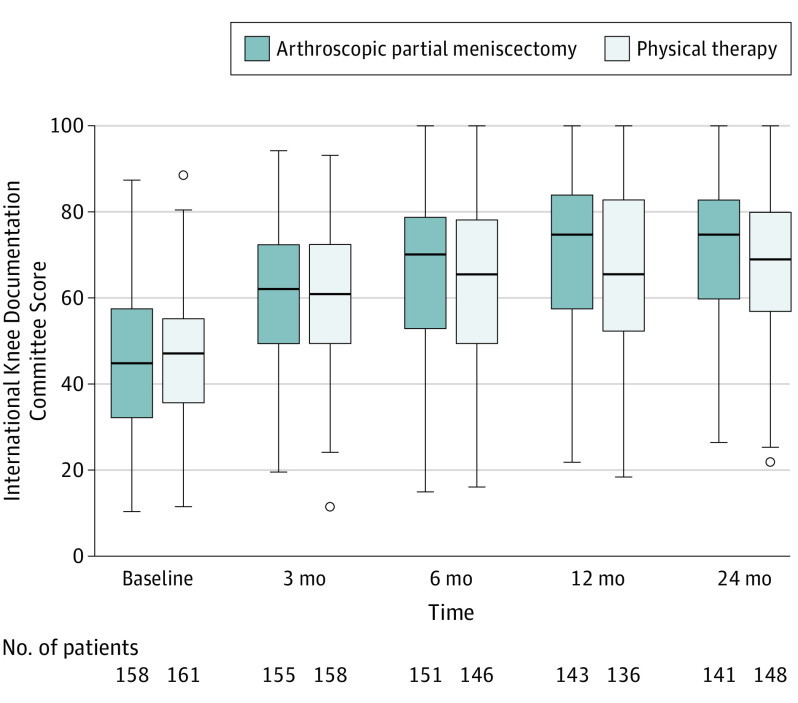
Figure 2 shows the improvement in knee function from baseline over the 24-month follow-up period for the APM and PT groups. In the APM group, knee function improved from 44.8 points at baseline to 71.5 points at 24 months (mean difference [MD], 26.2 points [95% CI, 23.2 to 29.3]). In the PT group, knee function improved from 46.5 points at baseline to 67.7 points at 24 months (MD, 20.4 points [95% CI, 17.5 to 23.2]). The primary mixed model analysis of the overall effects found a between-group difference of 3.6 points (97.5% CI, −∞ to 6.5; P value for noninferiority = .001) in favor of the APM group, indicating noninferiority of PT compared with APM (Table 2). The between-group differences at 3 (0.78 points [97.5% CI, –∞ to 4.3]) and 6 (3.4 points [97.5% CI, –∞ to 7.0]) months after randomization also demonstrated noninferiority of PT; however, the effects at 12 (5.7 points [97.5% CI, –∞ to 9.4]) and 24 (4.8 points [97.5% CI, –∞ to 8.5]) months after randomization did not demonstrate noninferiority. The adjusted between-group differences as well as the individual change scores from baseline to 24 months are presented in eTable 1 and eFigure 4, respectively, in Supplement 2.
Figure 2. Distribution of International Knee Documentation Committee (IKDC) Score of Knee Function.
The figure represents the results of the primary outcome knee function on the IKDC (range, 0 to 100; from worse to best) for intention-to-treat analysis. The data represent actual patient data at each time. In each comparison, the box indicates the range between the 25th and 75th percentile, with the median indicated as a horizontal line within the box. The whiskers extend to the upper and lower adjacent values, the most extreme values that are within 1.5 × interquartile range (IQR) beyond the 26th and 75th percentiles. Circles indicate points beyond these values. The median IKDC data are in eTable 5 in Supplement 2.
Table 2. Unadjusted Intervention Effects for the IKDC Score of Knee Function.
| Outcome | Mean IKDC Score | APM vs PT | Delayed APM vs PT | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| APM | PT | Delayed APM | Between-Group Difference (97.5% CI)a | P Value for Noninferiorityb | Between-Group Difference (97.5% CI)a | P Value for Noninferiorityb | ||||
| Points | No. of Patients (%) | Points | No. of Patients (%) | Points | No. of Patients (%) | |||||
| Primary Outcome (Intention-to-Treat) | ||||||||||
| Baseline | 44.8 | 158 (99) | 46.5 | 161 (99) | ||||||
| Overallc | 66.5 | 590 | 64.2 | 588 | 3.6 (−∞ to 6.5) | .001 | ||||
| 3 mo | 59.9 | 155 (97) | 60.0 | 158 (98) | 0.78 (−∞ to 4.3) | <.001 | ||||
| 6 mo | 64.7 | 151 (95) | 63.2 | 146 (90) | 3.4 (−∞ to 7.0) | .006 | ||||
| 12 mo | 70.7 | 143 (90) | 66.4 | 136 (84) | 5.7 (−∞ to 9.4) | .11 | ||||
| 24 mo | 71.5 | 141 (89) | 67.7 | 148 (91) | 4.8 (−∞ to 8.5) | .04 | ||||
| Secondary Outcome (as Treatedd) | ||||||||||
| Baseline | 43.9 | 150 (99) | 48.6 | 97 (100) | 40.8 | 47 (100) | - | |||
| Overallc | 66.2 | 561 | 66.6 | 372 | 57.6 | 163 | 1.7 (−∞ to 5.1) | <.001 | −5.8 (−∞ to −1.2) | <.001 |
| 3 mo | 59.3 | 147 (97) | 64.3 | 97 (100) | 49.8 | 47 (100) | −2.9 (−∞ to 1.3) | <.001 | −10.8 (−∞ to −5.2) | <.001 |
| 6 mo | 64.5 | 144 (95) | 65.3 | 93 (96) | 55.7 | 40 (85) | 1.6 (−∞ to 5.7) | .001 | −6.9 (−∞ to −1.0) | <.001 |
| 12 mo | 70.5 | 137 (91) | 67.5 | 90 (93) | 63.8 | 35 (74) | 4.9 (−∞ to 9.1) | .07 | −0.78 (−∞ to 5.3) | .002 |
| 24 mo | 71.1 | 133 (88) | 69.2 | 92 (95) | 63.0 | 41 (87) | 4.1 (−∞ to 8.3) | .04 | −2.1 (−∞ to 3.8) | <.001 |
Abbreviations: APM, arthroscopic partial meniscectomy; IKDC, International Knee Documentation Committee (range, 0 [most limitations] to 100 [no limitations]); PT, physical therapy.
The between-group difference for different follow-up points and as overall effect corrected only for IKDC score at baseline. Positive values signify that patients did better with (delayed) APM.
P values for noninferiority based on a 1-sample Z test with respect to the noninferiority margin. One-sided α of .025.
Overall estimate over 24 months refers to the overall IKDC score within each group and between groups including all time points. The overall effect is based on a model including intervention group and baseline IKDC score. The No. represents the number of observations entered into the model.
In the as-treated model, participants were analyzed who adhered to their randomized treatment in 3 groups: (1) participants allocated to the APM group who received APM, (2) participants allocated to the PT group who completed the PT protocol without having APM during the follow-up period (eg, ≥16 PT sessions; <16 sessions was considered a protocol violation), and (3) participants randomized to the PT group who had APM during follow-up (delayed APM group). Patients who were randomized to APM but did not have surgery and patients who were randomized to PT but did not complete the PT protocol and did not have delayed APM were removed from the as-treated analysis.
Exploratory Outcomes
Knee pain during weight-bearing improved in the APM group from 61.1 mm at baseline to 19.6 mm at 24 months (MD, 39.2 mm [95% CI, 33.8 to 44.6]) and in the PT group, knee pain during weight-bearing improved from 59.3 mm at baseline to 25.5 mm at 24 months (MD, 32.5 mm [95% CI, 26.7 to 38.3]) (Table 3 and eFigure 5 in Supplement 2). The mixed-model analysis of the overall effects found a between-group difference of 5.9 mm (95% CI, 1.4 to 10.3; P = .01) in favor of APM (Table 3). The adjusted between-group differences are presented in eTable 2 in Supplement 2.
Table 3. Unadjusted Intervention Effects for the VAS for Weight-Bearing Pain.
| Secondary Outcome | Mean VAS Weight-Bearing | APM vs PT | Delayed APM vs PT | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| APM | PT | Delayed APM | Between-Group Difference (95% CI)a |
P Valueb | Between-Group Difference (95% CI)a |
P Valueb | ||||
| Points | No. of Patients (%) | Points | No. of Patients (%) | Points | No. of Patients (%) | |||||
| Intention-to-Treat | ||||||||||
| Baseline | 61.1 | 145 (91) | 59.3 | 150 (93) | ||||||
| Overallc | 24.5 | 559 | 28.8 | 555 | −5.9 (−10.3 to −1.4) | .01 | ||||
| 3 mo | 30.4 | 154 (97) | 33.4 | 151 (93) | −3.1 (−8.8 to 2.7) | .30 | ||||
| 6 mo | 25.4 | 151 (95) | 31.0 | 145 (90) | −8.2 (−14.1 to −2.3) | .007 | ||||
| 12 mo | 21.0 | 139 (87) | 24.4 | 134 (83) | −5.3 (−11.4 to 0.73) | .08 | ||||
| 24 mo | 19.6 | 115 (72) | 25.5 | 125 (77) | −7.7 (−14.0 to −1.3) | .02 | ||||
| As-Treatedd | ||||||||||
| Baseline | 62.5 | 137 (91) | 56.0 | 91 (94) | 66.4 | 43 (91) | ||||
| Overallc | 24.9 | 531 | 24.7 | 349 | 39.8 | 154 | −1.7 (−6.8 to 3.3) | .50 | 13.8 (6.8 to 20.8) | <.001 |
| 3 mo | 30.8 | 146 (97) | 27.5 | 91 (94) | 48.0 | 46 (98) | 2.4 (−4.3 to 9.1) | .49 | 18.8 (9.7 to 27.9) | <.001 |
| 6 mo | 26.0 | 144 (95) | 28.0 | 92 (95) | 40.8 | 40 (85) | −4.5 (−11.2 to 2.3) | .20 | 12.7 (3.2 to 22.2) | .009 |
| 12 mo | 21.0 | 133 (88) | 21.0 | 89 (92) | 31.4 | 34 (72) | −2.4 (−9.3 to 4.5) | .49 | 6.8 (−3.2 to 16.8) | .18 |
| 24 mo | 20.5 | 108 (72) | 21.6 | 77 (79) | 36.0 | 34 (72) | −3.6 (−10.9 to 3.7) | .33 | 13.4 (3.2 to 23.5) | .01 |
Abbreviations: APM, arthroscopic partial meniscectomy; PT, physical therapy; VAS, visual analog scale (range, 0 [no pain] to 100 [worst pain imaginable]).
The between-group difference for different follow-up points and as overall effect corrected only for VAS score at baseline. Negative values signify that patients did better with (delayed) APM.
P values with respect to zero (superiority testing). Standard P values resulting from the mixed-model analysis in SPSS. One-sided α of .05.
Overall estimate over 24 months refers to the overall VAS score within each group and between groups including all time points. The overall effect is based on a model including intervention group and baseline VAS score. The No. represents the number of observations entered into the model.
In the as-treated model, participants were analyzed who adhered to their randomized treatment in 3 groups: (1) participants randomized to the APM group who received APM, (2) participants randomized to the PT group who completed the PT protocol without having APM during the follow-up period (eg, ≥16 PT sessions; <16 sessions was considered a protocol violation), and (3) participants randomized to the PT group who had APM during follow-up (delayed APM group). Patients who were randomized for APM but did not have surgery and patients who were randomized to PT but did not complete the PT protocol and did not have delayed APM were removed from the as-treated analysis.
General health in the APM group improved from 37.6 points at baseline to 51.1 points at 24 months (MD, 13.1 points [95% CI, 11.6 to 14.6]) and in the PT group, general health improved from 37.9 points at baseline to 48.7 points at 24 months (MD, 10.5 points [95% CI, 8.9 to 12.1]) (eFigure 6 in Supplement 2). The mixed-model analysis of the overall effects found an overall between-group difference of 1.3 points (95% CI, −0.2 to 2.7; P = .08) in favor of APM.
The activity level in the APM group improved from 2.6 points at baseline to 2.9 points at 24 months (MD, 0.34 points [95% CI, −0.00 to 0.69]) and in the PT group, the activity level improved from 2.5 points at baseline to 3.0 points at 24 months (MD, 0.38 points [95% CI, 0.08 to 0.68]) (eFigure 7 in Supplement 2). The mixed-model analysis of the overall effects found no significant between-group difference (0.04 points [95% CI, −0.3 to 0.2; P = .73]).
Osteoarthritis severity in the APM group progressed from 1.3 points at baseline to 1.6 points at 24 months (MD, 0.37 points [95% CI, 0.25 to 0.49]) and in the PT group, osteoarthritis severity progressed from 1.3 points at baseline to 1.5 points at 24 months (MD, 0.18 points [95% CI, 0.04 to 0.31]). The mixed-model analysis found no significant between-group difference (0.10 points more progression in the APM group [95% CI, −0.05 to 0.26; P = .18]).
As-Treated Analysis
In the as-treated analysis, 150 participants were analyzed in the APM group, 97 participants in the PT group, and 47 in the delayed APM group. All differences in knee function and pain during weight-bearing between the APM and PT groups were smaller in the as-treated analysis compared with the intention-to-treat analysis (Table 2 and Table 3).
Knee function improved in all 3 treatment groups (in the APM group from 43.9 points at baseline to 71.1 points at 24 months [MD, 26.8 points {95% CI, 23.6 to 29.9}]; in the PT group, from 48.6 points at baseline to 69.2 points at 24 months [MD, 20.2 points {95% CI, 16.5 to 23.8}]; and in the delayed APM group, from 40.8 points at baseline to 63.0 points at 24 months [MD, 21.5 points {95% CI, 15.8 to 27.3}]) (Table 2). The mixed-model analysis of the overall effects found a between-group difference of 1.7 points in favor of APM compared with PT (97.5% CI, −∞ to 5.1; P value for noninferiority < .001), indicating noninferiority of PT compared with APM (Table 2). The between-group differences at 3 (−2.9 points [97.5% CI, –∞ to 1.3]) and 6 (1.6 points [97.5% CI, –∞ to 5.7]) months after randomization also demonstrated noninferiority; however, the effects at 12 (4.9 points [97.5% CI, –∞ to 9.1]) and 24 (4.1 points [97.5% CI, –∞ to 8.3]) months after randomization did not demonstrate noninferiority .
When comparing PT with delayed APM, all between-group differences in knee function favored PT, demonstrating noninferiority of PT compared with delayed APM overall and at all time points (P < .002). The adjusted between-group differences are presented in eTable 1 in Supplement 2.
Knee pain during weight-bearing improved in all 3 groups (in the APM group, from 62.5 mm at baseline to 20.5 mm at 24 months [MD, 39.8 mm {95% CI, 34.1 to 45.5}]; in the PT group, from 56.0 mm at baseline to 21.6 mm at 24 months [MD, 33.6 mm {95% CI, 26.0 to 41.2}]; and in the delayed APM group, from 66.4 mm at baseline to 36.0 mm at 24 months [MD, 27.5 mm {95% CI, 16.0 to 39.1}]) (Table 3). The mixed-model analysis of the overall effects found no statistically significant between-group differences when comparing APM with PT (all P ≥ .20), and an overall between-group difference of 13.8 mm (95% CI, 6.8 to 20.8; P < .001) in favor of the PT group when comparing delayed APM with PT (Table 3). The adjusted between-group differences are presented in eTable 2 in Supplement 2.
Adverse Events
Serious adverse events (eg, cardiovascular, neurological or internal medicine conditions, venous thromboembolism, or repeat knee surgery) occurred in 9 participants in the APM group and 8 in the PT group. Nonserious adverse events (eg, reactive arthritis, joint paint resulting in extra consultation or surgical site infection) occurred in 9 participants in the APM group and 4 in the PT group. All adverse events are reported in eTable 3 in Supplement 2.
Post Hoc Exploratory Analysis
Post hoc exploratory analyses evaluated effect modification by the predefined potential confounders on the primary outcome, the IKDC score for knee function, and identified 2 statistically significant effect modifiers. First, there was interaction between baseline pain during weight-bearing and the treatment effect (regression coefficient, 0.14 [95% CI, 0.01 to 0.27; P value for interaction = .03]), indicating that the effect of APM was 0.14 points larger compared with PT on the IKDC score for each millimeter increase in baseline pain. Second, the effect of the intervention differed between BMI categories (P for interaction = .02 for obesity vs normal; P for interaction = .01 for obesity vs overweight). Specifically, obese participants in the APM group scored on average 10.7 IKDC points (95% CI, 4.7 to 16.8; P = .001) higher than obese participants in the PT group, while the difference between treatments was not statistically significant in the other groups (normal: 1.4 [95% CI, −3.4 to 6.2; P = .57] and overweight: 1.2 [95% CI, −3.1 to 5.4; P = .60]). There were no statistically significant interaction effects observed for location of the tear (P = .12), education level (P = .15), osteoarthritis severity (P = .74), mechanical complaints (P = .81), sex (P = .60), age (P = .53), and baseline IKDC score (P = .21) (eTable 4 in Supplement 2).
Discussion
This multicenter RCT showed that, in patients older than 45 years old with knee pain and nonobstructive meniscal tears, PT was noninferior to APM for knee function over a 24-month follow-up period. The results of this trial support the recommendations from the current guidelines that PT may be considered an appropriate alternative to APM as first-line therapy for patients with meniscal tears.25,26
Although noninferiority was demonstrated for the overall between-group difference in patient-reported knee function, and for the 3- and 6-month follow-up time points, results did not demonstrate noninferiority at the 12- and 24-month time points. Longer follow-up will provide more details on the effect of time on the between-group differences. To date, only 1 trial has reported 5-year outcomes in a similar population with meniscal tears, and reported no statistically significant differences in knee function between APM combined with PT (n = 45) and PT alone (n = 47).10
The previously reported clinical trials included a combined 838 patients and each trial reported no statistically significant differences between groups for knee function. These trials, however, were designed to assess superiority and had smaller sample sizes or shorter follow-up. Pooling these trials resulted in small statistically significant benefits of APM at up to 6-month follow-up.5,11 The current trial had a larger sample size and longer follow-up and demonstrated a small benefit of APM, consistent with the pooled results from earlier trials.5,11 Because this benefit from APM as compared with PT was smaller than the predefined noninferiority margin, and within the previously reported MCID in patients with different knee pathologies,27 the results of this trial demonstrated noninferiority of PT as compared with APM, and are consistent with current consensus that APM should not be the first treatment in middle-aged and older patients with meniscal tears.25,26
In this trial, 29% of participants from the PT group received delayed APM, demonstrating that not all patients initially treated with PT were satisfied with their results. The post-hoc exploratory findings on effect modification could guide future research on the characteristics of individuals who may be less likely to respond to PT to improve their treatment options and functional outcome.
Limitations
This study has several limitations. First, participants were not blinded to group assignment. Second, a screening log was not kept of patients who were eligible but not randomized, which limits the ability to assess the generalizability of the results. Third, the predefined noninferiority margin was a conservative estimate of potentially relevant differences, based on the smallest detectable change of 8.8 points.17 The smallest detectable change quantifies the amount of change that can be reliably detected by a measurement instrument, while noninferiority margins should be based on the maximum clinically acceptable difference that a patient is willing to give up in exchange for the secondary benefits of the alternative therapy. While the exact threshold of clinical relevance is unknown in a population with meniscal tears, Irrgang and colleagues27 reported an MCID for the IKDC of 11.5 points in patients with different types of knee disorders. If an MCID of 11.5 points was applied, PT would have been noninferior to APM both overall and at all individual time points. Fourth, noninferiority testing was intended for the secondary analyses, but no noninferiority margins were specified in the protocol. Therefore, the comparisons between the groups for the secondary outcomes were treated as standard 2-sided superiority hypotheses. Fifth, MCIDs for the secondary outcomes were not defined until after data analyses (identified in different populations; 13.7 mm for pain on the VAS28 and 2.0 points for RAND-36 PCS29). None of the observed between-group differences in these secondary outcomes exceeded MCID values, indicating that the clinical relevance of these findings is likely limited. Sixth, x-rays were interpreted by a single radiologist. Having 2 or more radiologists interpret x-rays may have resulted in more valid interpretations of osteoarthritis progression. Seventh, the combination of APM and PT may be more effective than APM alone. However, the authors followed the national guideline for generalizability of the study results and therefore APM was not always followed by PT.15
Conclusions
Among patients with nonobstructive meniscal tears, PT was noninferior to APM for improving patient-reported knee function over a 24-month follow-up period. Based on these results, PT may be considered as an alternative to surgery for patients with nonobstructive meniscal tears.
Trial Protocol
eTable 1. Adjusted Intervention Effects for the IKDC Score of Knee Function
eTable 2. Adjusted Intervention Effects for the VAS for Weight-Bearing Pain
eTable 3. Adverse events
eTable 4. Results of Interaction Effects of Post-Hoc Exploratory Analyses
eTable 5. Median IKDC points by treatment group
eFigure 1. Physical Therapy Protocol
eFigure 2. Histogram of Baseline IKDC Score of Knee Function per Treatment Group
eFigure 3. Histogram of baseline VAS for Knee Pain per Treatment Group
eFigure 4. Parallel Line Plot of Individual Change Scores in IKDC Score of Knee Function From Baseline to 24 Months
eFigure 5. Distribution of VAS for Knee Pain During Weight-Bearing
eFigure 6. Distribution of RAND-36 PCS Score for General Health
eFigure 7. Distribution of TAS for Activity Level
Data Sharing Statement
References
- 1.Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.pdf. Accessed August 15, 2018. [PubMed]
- 2.Sihvonen R, Paavola M, Malmivaara A, et al. ; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group . Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515-2524. doi: 10.1056/NEJMoa1305189 [DOI] [PubMed] [Google Scholar]
- 3.Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359(11):1108-1115. doi: 10.1056/NEJMoa0800777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015;1(1):CD004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. doi: 10.1136/bmj.j1982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675-1684. doi: 10.1056/NEJMoa1301408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740. doi: 10.1136/bmj.i3740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yim JH, Seon JK, Song EK, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41(7):1565-1570. doi: 10.1177/0363546513488518 [DOI] [PubMed] [Google Scholar]
- 9.Østerås H, Østerås B, Torstensen TA. Medical exercise therapy, and not arthroscopic surgery, resulted in decreased depression and anxiety in patients with degenerative meniscus injury. J Bodyw Mov Ther. 2012;16(4):456-463. doi: 10.1016/j.jbmt.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 10.Herrlin SV, Wange PO, Lapidus G, Hållander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? a five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):358-364. doi: 10.1007/s00167-012-1960-3 [DOI] [PubMed] [Google Scholar]
- 11.van de Graaf VA, Wolterbeek N, Mutsaerts EL, et al. Arthroscopic partial meniscectomy or conservative treatment for nonobstructive meniscal tears: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2016;32(9):1855-1865.e4. doi: 10.1016/j.arthro.2016.05.036 [DOI] [PubMed] [Google Scholar]
- 12.Stahel PF, Wang P, Hutfless S, et al. Surgeon practice patterns of arthroscopic partial meniscectomy for degenerative disease in the United States: a measure of low-value care. JAMA Surg. 2018;153(5):494-496. doi: 10.1001/jamasurg.2017.6235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van de Graaf VA, Scholtes VA, Wolterbeek N, et al. ; Escape Research Group . Cost-effectiveness of Early Surgery versus Conservative Treatment with Optional Delayed Meniscectomy for Patients over 45 years with non-obstructive meniscal tears (ESCAPE study): protocol of a randomised controlled trial. BMJ Open. 2016;6(12):e014381. doi: 10.1136/bmjopen-2016-014381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. doi: 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Arkel ERA, van Essen A, Koëter S, et al. Artroscopie van de knie: indicatie en behandeling. Dutch Orthopedic Association guideline. http://www.rep-online.nl/homepage/richtlijnen. Accessed January 1, 2018.
- 16.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600-613. doi: 10.1177/03635465010290051301 [DOI] [PubMed] [Google Scholar]
- 17.Crawford K, Briggs KK, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the IKDC score for meniscus injuries of the knee. Arthroscopy. 2007;23(8):839-844. doi: 10.1016/j.arthro.2007.02.005 [DOI] [PubMed] [Google Scholar]
- 18.van de Graaf VA, Wolterbeek N, Scholtes VA, Mutsaerts EL, Poolman RW. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med. 2014;42(6):1408-1416. doi: 10.1177/0363546514524698 [DOI] [PubMed] [Google Scholar]
- 19.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee . The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128-135. doi: 10.1177/0363546505280214 [DOI] [PubMed] [Google Scholar]
- 20.Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127-1131. doi: 10.1016/S0140-6736(74)90884-8 [DOI] [PubMed] [Google Scholar]
- 21.VanderZee KI, Sanderman R, Heyink JW, de Haes H. Psychometric qualities of the RAND 36-Item Health Survey 1.0: a multidimensional measure of general health status. Int J Behav Med. 1996;3(2):104-122. doi: 10.1207/s15327558ijbm0302_2 [DOI] [PubMed] [Google Scholar]
- 22.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43-49. [PubMed] [Google Scholar]
- 23.Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(suppl 2):58-69. doi: 10.2106/00004623-200300002-00008 [DOI] [PubMed] [Google Scholar]
- 24.United Nations Educational, Scientific and Cultural Organization (UNESCO) Institute for Statistics . ISCED mappings. http://uis.unesco.org/en/isced-mappings. Accessed January 1, 2018.
- 25.Beaufils P, Becker R, Kopf S, et al. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):335-346. doi: 10.1007/s00167-016-4407-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stone JA, Salzler MJ, Parker DA, Becker R, Harner CD. Degenerative meniscus tears: assimilation of evidence and consensus statements across three continents: state of the art. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine. 2017;2(2):108-119. doi: 10.1136/jisakos-2015-000003 [DOI] [Google Scholar]
- 27.Irrgang JJ, Anderson AF, Boland AL, et al. ; International Knee Documentation Committee . Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567-1573. doi: 10.1177/0363546506288855 [DOI] [PubMed] [Google Scholar]
- 28.Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(6):927-932. doi: 10.1016/j.jse.2009.03.021 [DOI] [PubMed] [Google Scholar]
- 29.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384-391. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Adjusted Intervention Effects for the IKDC Score of Knee Function
eTable 2. Adjusted Intervention Effects for the VAS for Weight-Bearing Pain
eTable 3. Adverse events
eTable 4. Results of Interaction Effects of Post-Hoc Exploratory Analyses
eTable 5. Median IKDC points by treatment group
eFigure 1. Physical Therapy Protocol
eFigure 2. Histogram of Baseline IKDC Score of Knee Function per Treatment Group
eFigure 3. Histogram of baseline VAS for Knee Pain per Treatment Group
eFigure 4. Parallel Line Plot of Individual Change Scores in IKDC Score of Knee Function From Baseline to 24 Months
eFigure 5. Distribution of VAS for Knee Pain During Weight-Bearing
eFigure 6. Distribution of RAND-36 PCS Score for General Health
eFigure 7. Distribution of TAS for Activity Level
Data Sharing Statement