Key Points
Question
Is there a clinical association between exfoliation syndrome/glaucoma and inguinal hernia in the Utah Population Database?
Findings
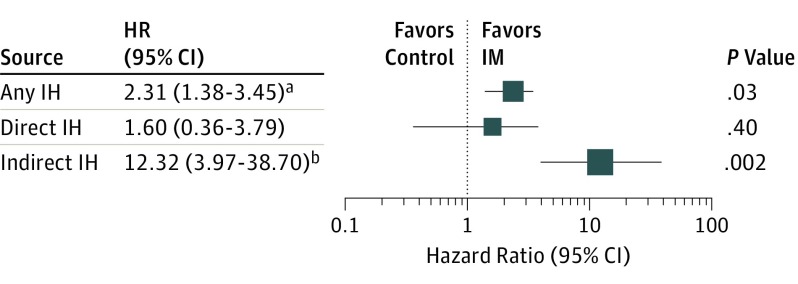
In this cross-sectional study of a Utah population from 1996 to 2015, patients with an inguinal hernia exhibited a 2.3-fold increased risk of an exfoliation syndrome diagnosis compared with control individuals; the association between the indirect hernia subtype was most notable.
Meaning
The diagnosis of exfoliation syndrome/glaucoma was more frequent in patients with inguinal hernia in the Utah Population Database, suggesting a possible shared pathogenesis.
Abstract
Importance
Exfoliation syndrome (XFS) is a systemic connective tissue disease, and abnormal connective tissue metabolism is implicated in inguinal hernias (IH). Associating XFS with comorbid conditions may illuminate their underlying pathophysiology and affect clinical screening and treatment. Exfoliation syndrome involves altered systemic extracellular matrix (ECM) homeostasis involving elastin metabolism. Hernias occur owing to abnormal ECM synthesis, metabolism, or repair. Inguinal hernias involve weakening or rupture of the abdominal/groin wall.
Objective
To determine an association between patients with XFS and patients with IH in Utah, possibly differing between direct or indirect hernia.
Design, Setting, and Participants
Cross-sectional study in a large health care system of Utah hospitals and clinics. Conditional logistic regression odds ratios were used to estimate risk of XFS in patients with IH overall and by subtype (direct or indirect) compared with control individuals. Codes specific to direct and indirect IH with additional medical records review of 186 procedures were used to classify IH subtypes that were not prespecified. Bootstrap resampling with jackknife estimation used to calculate 95% confidence intervals. The model accounted for matching on sex and age and adjusted for body mass index and tobacco use. Population-based sample using medical records from 1996 to 2015 that identified 2594 patients 40 years or older on January 1, 1996, with surgical IH repair and 12 966 random control patients with no IH history matched 5:1 on sex and birth year. Data were analyzed between September 10, 2017, and October 23, 2017.
Main Outcomes and Measures
Exfoliation syndrome outcome defined by diagnosis codes for XFS or exfoliation glaucoma from 1996 to 2015.
Results
Participants were primarily white (2532 of 2594 patients, [96.1%]; 12 454 of 12 966 control individuals [97.6%]) and non-Hispanic (2396 of 2594 patients [92.4%]); 250 participants were women (9.6%). Of study participants, 22 patients with IH and 43 control individuals were diagnosed as having XFS, respectively. Patients with IH had a 2.3-fold risk for an XFS diagnosis compared with control individuals (95% CI, 1.4-3.5; P = .03), and XFS risk with indirect IH appeared especially pronounced.
Conclusions and Relevance
Inguinal hernia was associated with an increased risk of XFS in this Utah population. Further work is needed to understand the pathophysiology, genetics, and environmental factors contributing to both diseases.
This cross-sectional study investigates the association between patients with exfoliation syndrome and risk for inguinal hernia.
Introduction
Exfoliation syndrome (XFS) is a complex, inherited systemic disorder characterized by abnormal accumulation of extracellular matrix material (ECM).1 Deposition of fibrillar ECM debris, or exfoliation material (XFM), within anterior segment structures of the eye is the disease manifestation to clinically diagnose XFS, the most common recognizable cause of open-angle glaucoma worldwide, comprising most cases in some countries.2 Patients with XFS are at high risk of developing exfoliation glaucoma (XFG), a particularly aggressive form of glaucoma.
The XFS phenotype, reported in multiple populations, is highly associated with genetic variants in the lysyl oxidase like-1 (LOXL1) locus, a key enzyme in ECM deposition and repair.3,4 Extracellular matrix material synthesis and remodeling is a systemic phenomenon, and the fibrillar deposits of XFS have been observed in heterogeneous tissues.5,6 Exfoliation syndrome is a systemic disease, and investigators have proposed that abnormal ECM metabolism and repair underlies the etiology of several associated diseases; researchers have reported increased risk of cardiovascular and cerebrovascular disease, abdominal aortic aneurysm, hearing loss, and pelvic organ prolapse.7,8,9,10
Hernia is the protrusion of an organ or its part through a body structure normally containing it. Inguinal hernias (IH) are a subtype of groin hernia characterized by displacement of intra-abdominal contents through weakened abdominal wall involving the inguinal canal. Inguinal hernias are classified by anatomic location and the underlying etiology as congenital or acquired. Inguinal hernias are much more common in men vs women, with lifetime risk approximately 27% vs 3%, respectively.11 Other reported risk factors for IH include prior hernia, family history, trauma, increased age, white race/ethnicity, and smoking (hernia recurrence); increased body mass index (BMI) is inversely associated with IH risk, while chronic cough and constipation have yielded mixed reports.12,13,14,15,16 Groin hernia repairs are one of the most common surgical procedures, globally estimated at 20 million annually.17 Inguinal hernia pathogenesis, although not fully understood, is recognized as a complex, familial, and likely multifactorial heterogeneous group of alterations in ECM metabolism and repair resulting in tissue weakening.
Pathologic elastin and ECM connective tissue changes are implicated in both XFS and IH; moreover, each disease is associated with genetic predisposition, displaying familial or population aggregation.18,19,20 These observations drove our hypothesis of a clinical association between the 2 diseases. This inquiry has been supported by our 2016 work10 describing an association between XFS and pelvic organ prolapse (POP) in women, the latter a subtype of hernia resulting in protrusion of pelvic contents involving the vaginal wall, which is also genetically and environmentally influenced.10 We also hypothesized risk may differ between direct and indirect subtype given etiologic differences, a novel study aspect; to our knowledge, no studies exist that examined XFS in these subtypes. To investigate these hypotheses, we performed a population-based investigation using the Utah Population Database (UPDB), a robust research resource previously described in detail.10,21
Methods
Study Participants
Using University of Utah Healthcare (UUHC) medical records linked to Utah residents and their demographic data within the UPDB, we identified patients who underwent surgical inguinal hernia repair between 1996 and 2015 based on any occurrence of 1 or more International Classification of Diseases, Ninth Revision (ICD-9) or Current Procedural Terminology codes shown in Table 1. We examined the association of XFS (ICD-9 codes 365.52 and 366.1) in patients with IH 40 years or older on January 1, 1996, compared with random UUHC population control individuals individually sex- and age-matched to cases in a 5:1 target ratio. The UUHC system consists of 4 hospitals and 12 community health centers throughout Utah, in which more than 10 000 inpatient and more than 15 000 outpatient surgical procedures are performed annually.22 The proportion of UUHC patients 40 years and older who had a dilated eye examination at a UUHC facility was approximately 35%, and of patients having a diagnosis of IH 40 years and older in our study, 1072 of 2594 (41%) had a dilated eye examination. Institutional review board/ethics committee approval was obtained through the University of Utah institutional review board and the Resource for Genetic and Epidemiologic Research. All data were deidentified, Health Insurance Portability and Accountability Act compliant, and adhered to the tenets of the Declaration of Helsinki. Because all data were deidentified, patient consent was not obtained.
Table 1. ICD-9 and CPT Codes Used to Identify Patients With Inguinal Hernia Repair.
| Code | Definition |
|---|---|
| ICD-9 code | |
| 17.1 | Laparoscopic unilateral repair of inguinal hernia |
| 17.11 | Laparoscopic repair of direct inguinal hernia with graft or prosthesis |
| 17.12 | Laparoscopic repair of indirect inguinal hernia with graft or prosthesis |
| 17.13 | Laparoscopic repair of inguinal hernia with graft or prosthesis, NOS |
| 53 | Other unilateral repair of inguinal hernia |
| 53 | Unilateral repair of inguinal hernia, not otherwise specified |
| 53.01 | Other and open repair of direct inguinal hernia, unilateral |
| 53.02 | Other and open repair of indirect inguinal hernia, unilateral |
| 53.03 | Other and open repair of direct inguinal hernia with graft or prosthesis, unilateral |
| 53.04 | Other and open repair of indirect inguinal hernia with graft or prosthesis, unilateral |
| 53.05 | Repair of inguinal hernia with graft or prosthesis, NOS, unilateral |
| 53.1 | Other bilateral repair of inguinal hernia |
| 53.1 | Bilateral repair of inguinal hernia, not otherwise specified |
| 53.11 | Other and open bilateral repair of direct inguinal hernia |
| 53.12 | Other and open bilateral repair of indirect inguinal hernia |
| 53.13 | Other and open bilateral repair inguinal hernia, 1 direct and 1 indirect |
| 53.14 | Other and open bilateral repair of direct inguinal hernia with graft or prosthesis |
| 53.15 | Other and open bilateral repair of indirect inguinal hernia with graft or prosthesis |
| 53.16 | Other and open bilateral repair inguinal hernia, one direct and one indirect, graft or prosthesis |
| 53.17 | Bilateral inguinal hernia repair with graft or prosthesis, not otherwise specified |
| 550 | Inguinal hernia |
| 550 | Inguinal hernia with gangrene |
| 550.1 | Inguinal hernia with obstruction without mention of gangrene |
| 550.9 | Inguinal hernia without mention of obstruction or gangrene |
| CPT code | |
| 49505 | Repair initial inguinal hernia age ≥5 reducible |
| 49507 | Repair initial inguinal hernia age ≥5 incarcerated/strangulated |
| 49520 | Repair recurrent inguinal hernia, any age, reducible |
| 49521 | Repair recurrent inguinal hernia incarcerated/strangulated |
| 49525 | Repair inguinal hernia, sliding, any age |
| 49650 | Laparoscopy, surgical; repair initial inguinal hernia |
| 49651 | Laparoscopy, surgical; repair recurrent inguinal hernia |
Abbreviations: CPT, Current Procedural Terminology; ICD-9, International Classification of Diseases, Ninth Revision; NOS, not otherwise specified.
Medical Record Review
Inguinal hernia is diagnosed clinically on physical examination; however, determination of direct vs indirect subtypes can only be definitively diagnosed during surgical repair. Because direct and indirect IH differ anatomically and epidemiologically, with biochemical evidence of partially differential pathogenesis, we analyzed the IH subtypes both independently and grouped but without prespecification.23 Initial medical record analysis revealed a large set of patients with hernia with codes specific to IH. A medical record review in a sample of 186 surgical IH repairs (165 random and 22 with an XFS history) revealed codes composed of either direct IH (n = 57), indirect IH (n = 60), or unspecified whether direct or indirect (n = 69). Goals were to (1) gauge the determinability of direct/indirect subtypes for patients unspecified for subtype and (2) assess coding accuracy of cases subtype specified. Because determination during surgical repair is considered the definitive diagnostic modality, only operative notes (ON) were considered. Previously, we assessed the coding accuracy for an XFS diagnosis in the UUHC medical record. In a random selection of 540 medical records on 1901 patients having a diagnosis of XFS, diagnostic accuracy was greater than 90%.24
Statistical Methods
Risk of XFS was estimated from a conditional logistic regression model to account for individual matching of controls to cases on sex and age (measured as birth year). Because the number of XFS outcomes in patients with IH was sparse and asymptotic estimates imprecise, we also used a bootstrap resampling method with a jackknife variance estimator to provide odds ratio (OR) and confidence intervals based on 1000 replicates.25 Nominal 2-sided P values are presented, with a significance level of .05. Additional covariates were included to adjust for BMI and tobacco use (ICD-9 codes 305.1 and V15.82), established risk factors for hernia and/or XFS.15,26 Body mass indices (calculated as weight in kilograms divided by height in meters squared) measured closest to the date of procedure were obtained from Utah driver license records linked to the UPDB. An imputed BMI based on the mean for sex and 10-year birth cohort was calculated for 2520 participants (20% of 15 560 total) where data for height and/or weight were unavailable. An indicator variable for imputation status (actual or imputed) was incorporated. Because most participants were white, adjustment for race/ethnicity did not affect estimates and therefore was not included. All analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc).
Results
Medical Record Review Results
Of 117 patients explicitly coded as either direct or indirect IH, we confirmed coding accuracy in 107 cases (91%). In 7 of 117 patients (6%), we could not confirm subtype by the ON and considered these as probable direct or indirect IH, depending on the code specified. Three cases had stated codes in obvious conflict with the ON. In the unspecified IH group (n = 69), we differentiated direct or indirect IH subtype in 57 patients (82%), either by verbatim description or by implication based on the anatomical references from the ON. We also determined that 13 patients had 1 direct and 1 indirect hernia repair performed concurrently but were coded by a single subtype, presumably arbitrarily.
Participant Characteristics
As shown in Table 2, we identified 2594 patients with IH, of whom 250 were women (9.6%), consistent with other reports in US populations.27,28 Of patients with IH, 1138 (44%) were specified by codes or determined from medical record review: 486 direct inguinal, 603 indirect inguinal, and 49 with both a direct and indirect IH (37 simultaneous and 12 sequential). We observed 22 patients with IH with an XFS diagnosis history. Of 12 966 individually sex- and birth year–matched controls (target ratio 5:1), 43 individuals had an XFS diagnosis history. Control individuals and patients with IH were predominantly white and non-Hispanic (Table 2). Patients with IH had a slightly lower imputed BMI and were more likely to have used tobacco compared with control individuals, consistent with prior reports.16,26 Both patients with IH and control individuals had a mean of more than 6 years of follow-up in Utah during a 20-year study period (1996-2015) based on UPDB demographic and medical records (Table 2).
Table 2. Characteristics of the Inguinal Hernia Study Participants.
| Characteristic | No. (%) | |
|---|---|---|
| Control Individuals (Matched 5:1) | Patients With Inguinal Hernia | |
| Total | 12 966 (100.0) | 2594 (100.0) |
| Men | 11 717 (90.4) | 2344 (90.4) |
| Women | 1249 (9.6) | 250 (9.6) |
| Race/ethnicity | ||
| White | 12 454 (96.1) | 2532 (97.6) |
| Nonwhite | 512 (3.9) | 62 (2.4) |
| Ethnicity | ||
| Non-Hispanic | 11 987 (92.4) | 2396 (92.4) |
| Hispanic | 979 (7.6) | 198 (7.6) |
| Tobacco use diagnosis | ||
| No | 10 403 (80.2) | 1986 (76.6) |
| Yes | 2563 (19.8) | 608 (23.4) |
| BMI, mean (SD) | 27.6 (4.85) | 26.1 (3.60) |
| BMI imputed | 1905 (14.7) | 615 (23.7) |
| Vital status | ||
| Alive at last follow-up | 10 872 (83.9) | 2183 (84.2) |
| Died prior to study end | 2094 (16.1) | 411 (15.8) |
| Follow-up, mean (SD), y | 6.8 (4.98) | 6.1 (5.10) |
| XFS diagnosis history | ||
| Unaffected | 12 923 (99.7) | 2572 (99.2) |
| Affected | 43 (0.3) | 22 (0.8) |
| XFS age, mean (SD), y | 70.7 (17.34) | 75.3 (8.49) |
| Inguinal hernia subtypea | ||
| Direct hernia | 2429 (18.7) | 486 (18.7) |
| Indirect hernia | 3014 (23.2) | 603 (23.2) |
| Both direct and indirect | 245 (1.9) | 49 (1.9) |
| Unspecified | 7278 (56.1) | 1456 (56.1) |
| Age at hernia diagnosis, mean (SD), y | 59.6 (12.2) | 59.6 (12.15) |
| 40 to 59 | 6715 (51.8) | 1343 (51.8) |
| 60 to 69 | 3273 (25.2) | 662 (25.5) |
| ≥70 | 2978 (23.0) | 589 (22.7) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); XFS, exfoliation syndrome.
Specified direct or indirect inguinal hernia from Current Procedural Terminology code or medical record review.
Association With Exfoliation Syndrome
Overall, patients with IH had a 2.3-fold increased risk of an XFS diagnosis compared with control individuals (95% CI, 1.4-3.5; P = .03; Figure). Of patients with a direct IH, increased risk of XFS was not observed (OR, 1.6; 95% CI, 0.4-3.7; P = .40). In contrast, patients with an indirect IH repair exhibited a 12-fold increased risk of an XFS diagnosis compared with matched control individuals, although the estimate was imprecise (95% CI, 4.0-38.7; P = .002). These findings, based on a bootstrap resampling approach to provide more reliable estimates given relatively few XFS diagnoses, were consistent with point estimates using an asymptotic (classic) conditional logistic regression model either adjusted for covariates or unadjusted (eTable in the Supplement). In the few patients with IH who had both a direct and indirect IH repair, risk of XFS was similar to patients with an indirect repair only (eTable in the Supplement). In the subset of 250 women with an IH repair, a similar increased risk of XFS compared with female control individuals was observed, although few outcomes (3 patients with IH and 3 control individuals had XFS) did not allow us to distinguish between risk of IH subtypes in women.
Figure. Risk of Exfoliation Syndrome (XFS) in 2594 Patients With Inguinal Hernia (IH) Compared With 12 966 Control Individuals.
Model accounting for matching on sex and birth year and adjusted for tobacco use, body mass index (BMI), and imputed BMI indicator. Number of patients with IH with an XFS history: 22 any IH, 4 direct IH, and 12 indirect IH. Number of control individuals with an XFS history: 43 matched to any IH, 15 matched to direct IH, and 5 matched to indirect patient with IH.
aP = .03
bP = .002
Discussion
Lysyl oxidase like-1 belongs to the family of lysyl monoamine oxidases, a group of 5 copper-dependent enzymes (LOX and LOXL1-4). This enzyme family is heavily involved in collagen and elastin metabolism; specifically, LOXL1 covalently cross-links collagen and elastin fibers.29 Dysregulation of LOXL1 is suspected to play a role in XFM formation, with XFM deposits likely resulting from increased synthesis or impaired degradation of elastin and ECM elements. Given the ubiquity of elastin and LOXL1 in ECM components, systemic disease associations with XFS beyond classical ocular manifestations have garnered interest; increased risk of cardiovascular disease, cerebrovascular disease, and sensorineural hearing loss have been reported.7,9,24,30 In 2016, we reported the association of XFS with increased risk of pelvic organ prolapse (POP) in women, where LOXL1 has been hypothesized to play a role.10 Research also supports a role for LOXL1 in the pathogenesis of IH.31,32 The tendency for XFS to aggregate within specific populations along with secondary environmental insults, such as trauma and/or ultraviolet exposure, has been described. This suggests an underlying genetic predisposition to develop XFS/XFG and possibly other ECM pathologies including POP and hernias.33,34,35
Inguinal hernias are classified into direct and indirect subtypes and distinguished structurally by anatomic location and etiologically as congenital or acquired. Hernia manifestation occurs with pathological alteration of normal body wall fibromuscular tissues and/or ECM within the complex milieu of repeated mechanical insults, intrinsic connective tissue disorders, and modifiable or nonmodifiable risk factors.36,37,38 Direct IH results when intra-abdominal contents press into the transversalis fascia in the region of Hesselbach triangle, notably medial to the inferior epigastric vessels. The hernia sac may or may not rupture into the inguinal canal and protrude through the external (superficial) inguinal ring. Direct IHs are thought to occur owing to acquired weaknesses of abdominal wall tissues.39
By contrast, indirect IHs enter a weakened internal (deep) inguinal ring via a patent processus vaginalis (PV) lateral to the inferior epigastric vessels, course the inguinal canal, and possibly exit the external (superficial) ring. During normal male embryologic development, the PV lumen obliterates postnatally; failure results in a patent PV, a physiological defect of the abdominal wall providing a herniation pathway.40,41 Although considered congenital, indirect IH displays a bimodal distribution with risk increasing through adulthood. This suggests additional genetic and/or environmental factors are superimposed on the developmental defect to manifest disease.42
Direct and indirect IHs share abnormalities in connective tissue metabolism and genetic risk factors, but subtle variations in tissue histology, biomarkers, and demographics suggest overlapping yet distinct pathogenic mechanisms.23 Unique risk factors specific for indirect IH include a patent PV (notably with histological evidence of abnormal smooth muscle cells thickening the internal inguinal ring) and occupational exposures involving increased abdominal pressure (standing, lifting).42,43,44 Biomarkers suggestive of a chronic, low-grade, profibrotic inflammatory state have been reported in XFS, some that parallel with IH.1 Additionally, XFS investigators have described impaired pupillary dilation and altered intraocular muscle function, as well as histopathologic evidence of degenerative/atrophic changes in the iris, suggesting smooth muscle dysfunction may play a role in XFS.45,46,47 The causes underlying the differential risk for direct and indirect IH with XFS observed in this study are unclear. However, the presence of abnormal smooth muscle cells observed in the patent PV of patients with indirect IH, coupled with the smooth muscle dysfunction and proinflammatory state in XFS, could hypothetically promote fibrosis and weakening of internal inguinal ring tissues, ultimately leading to herniation.
There is substantial support for genetic risk as a component of multiple hernia types.19 Epidemiology studies in diverse geographic populations that include both men and women have found an increased risk specifically for primary IH by family history.12,19,48,49 A large Swedish registry identified an increased familial risk in all hernia forms; notably, IH (and femoral hernia) carried the highest risks among all hernia types when a sibling had the concordant hernia type.19 Interestingly, the Scandinavian population was where XFS was originally identified and genotyped.3
Study Strengths
To our knowledge, this is the first health care system population investigation of an association between XFS and IH. The UPDB is a unique resource compiling comprehensive medical information electronically available since 1996, state vital records, and census data from more than 9 million individuals residing in Utah since the late 1800s. Additionally, it houses Utah genealogic records, allowing construction of large family pedigrees linked to medical and vital records. A unique resource of its kind, it enables high-quality epidemiology research to identify cosegregating diseases, familial disease clustering, and environmental exposures. Our results are generalizable to similar white populations of primarily northern European descent with access to a large health care system.
Study Limitations
Although a medical record review indicated that administrative codes were accurate to identify IH and its subtypes in our sample, we acknowledge potential bias from misclassification. Although most UPDB individuals have long follow-up times in Utah based on vital records and medical data, we cannot rule out that unaffected individuals with no hernia diagnosis or procedure in our data may have been treated outside of Utah, although we believe any misclassification from this source would be minimal. We acknowledge that patients having a clinical diagnosis of IH but who have not undergone surgical repair are not included in this analysis, and the association with XFS in this group is indeterminate. However, because IH subtype determination during surgical repair is considered the criterion standard, we elected to analyze only surgically confirmed IH to remove misdiagnosis confounders. While there is sparse literature on the proportion of patients with IH who undergo surgical repair, 1 randomized clinical trial comparing watchful waiting with operative repair in asymptomatic men with IH reported 79% of men older than 65 years in the watchful waiting group eventually underwent surgical repair at 10 years’ follow-up.50 Additionally, for patients 40 years or older in the UUHC database with an ICD-9 diagnosis code for IH, 97% also had an accompanying IH repair/procedure code. Thus, we believe our approach captured most IH diagnoses for UUHC patients in the database.50 We acknowledge that XFS was relatively uncommon among patients with IH 40 years and older, given that XFS is generally diagnosed at older than 60 years during a routine vision examination. Beginning in 1996, when electronic medical records became available, more than half of our study participants with an IH diagnosis were younger than the mean age at which XFS is clinically recognized. We also note that patients with XFS were overrepresented in our medical record review; thus, estimates of risk within hernia subtype may be inflated. However, across all patients with IH, including those with subtype unspecified by code who were not selected for medical record review, we observed a more than doubling of XFS risk using both bootstrap and classical techniques; thus, we believe the association is not a spurious one. We did not control for multiple comparisons because the study was restricted to a limited number of planned comparisons and nominal P values are presented. Thus, we cannot rule out a chance observation.
Future Investigation
Given our intriguing population-based association between IH and XFS, we plan to expand our study to other types of hernia (eg, femoral, ventral, and gastric) and interrogate a larger IH data set. We will determine the feasibility of extracting accurate data for other documented or suspected risk factors for IH, including trauma, chronic cough, and constipation, as potential covariates. Because we previously found an increased risk of XFS in women with POP, our study data indicate that women with IH are more likely to have had a POP diagnosis than women with no IH history (OR, 1.7; 95% CI, 1.5-2.0; P < .001; data not shown). We will pursue obtaining medical records of other health care systems in Utah linked to the UPDB, including those of Medicare beneficiaries, as well as patient biospecimens to further explore a potential association between hernia, POP, and XFS. Studied independently, the pathogenesis of both XFS and IH are complex, familial, and multifactorial and appear to be associated comorbidities based on this UPEXS study. Both diseases independently illustrate epidemiologic evidence of population aggregation and familial predisposition, suggesting an underlying genetic component in pathogenesis.3
Conclusions
Exfoliation syndrome has historically been viewed primarily as an ophthalmic disorder. This investigation provides additional evidence to support a broad change in perception. The exploration of the role of XFS with disorders of elastin and ECM metabolism has just begun. Determining molecular pathways and the definitive DNA sequence markers for this inherited disorder may catalyze these investigations. It may become increasingly important for the medical field to broaden appreciation of XFS as a systemic condition. Exfoliation syndrome may serve as an example of a group of inherited systemic conditions that exist just at or below the level of detection that influence human health, positively and negatively, throughout one’s lifetime.
eTable. Association of Inguinal Hernia (IH) Diagnosis in University of Utah Healthcare (UUHC) Patients (1996-2015)
References
- 1.Zenkel M, Schlötzer-Schrehardt U. The composition of exfoliation material and the cells involved in its production. J Glaucoma. 2014;23(8)(suppl 1):S12-S14. doi: 10.1097/IJG.0000000000000123 [DOI] [PubMed] [Google Scholar]
- 2.Ritch R. Exfoliation syndrome-the most common identifiable cause of open-angle glaucoma. J Glaucoma. 1994;3(2):176-177. [PubMed] [Google Scholar]
- 3.Thorleifsson G, Magnusson KP, Sulem P, et al. Common sequence variants in the LOXL1 gene confer susceptibility to exfoliation glaucoma. Science. 2007;317(5843):1397-1400. doi: 10.1126/science.1146554 [DOI] [PubMed] [Google Scholar]
- 4.Founti P, Haidich A-B, Chatzikyriakidou A, et al. Ethnicity-based differences in the association of LOXL1 polymorphisms with pseudoexfoliation/pseudoexfoliative glaucoma: a meta-analysis. Ann Hum Genet. 2015;79(6):431-450. doi: 10.1111/ahg.12128 [DOI] [PubMed] [Google Scholar]
- 5.Streeten BW, Li Z-Y, Wallace RN, Eagle RC Jr, Keshgegian AA. Pseudoexfoliative fibrillopathy in visceral organs of a patient with pseudoexfoliation syndrome. Arch Ophthalmol. 1992;110(12):1757-1762. doi: 10.1001/archopht.1992.01080240097039 [DOI] [PubMed] [Google Scholar]
- 6.Schlötzer-Schrehardt UM, Koca MR, Naumann GOH, Volkholz H. Pseudoexfoliation syndrome: ocular manifestation of a systemic disorder? Arch Ophthalmol. 1992;110(12):1752-1756. doi: 10.1001/archopht.1992.01080240092038 [DOI] [PubMed] [Google Scholar]
- 7.Wang W, He M, Zhou M, Zhang X. Ocular pseudoexfoliation syndrome and vascular disease: a systematic review and meta-analysis. PLoS One. 2014;9(3):e92767. doi: 10.1371/journal.pone.0092767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yüksel N, Anik Y, Altintaş O, Onur I, Cağlar Y, Demirci A. Magnetic resonance imaging of the brain in patients with pseudoexfoliation syndrome and glaucoma. Ophthalmologica. 2006;220(2):125-130. doi: 10.1159/000090578 [DOI] [PubMed] [Google Scholar]
- 9.Djordjevic-Jocic J, Jovanovic P, Bozic M, Tasic A, Rancic Z. Prevalence and early detection of abdominal aortic aneurysm in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Curr Eye Res. 2012;37(7):617-623. doi: 10.3109/02713683.2012.665120 [DOI] [PubMed] [Google Scholar]
- 10.Wirostko BM, Curtin K, Ritch R, et al. Risk for exfoliation syndrome in women with pelvic organ prolapse: a Utah Project on Exfoliation Syndrome (UPEXS) study. JAMA Ophthalmol. 2016;134(11):1255-1262. doi: 10.1001/jamaophthalmol.2016.3411 [DOI] [PubMed] [Google Scholar]
- 11.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996;25(4):835-839. [DOI] [PubMed] [Google Scholar]
- 12.Lau H, Fang C, Yuen WK, Patil NG. Risk factors for inguinal hernia in adult males: a case-control study. Surgery. 2007;141(2):262-266. doi: 10.1016/j.surg.2006.04.014 [DOI] [PubMed] [Google Scholar]
- 13.Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol. 2007;165(10):1154-1161. doi: 10.1093/aje/kwm011 [DOI] [PubMed] [Google Scholar]
- 14.Burcharth J, Pommergaard H-C, Bisgaard T, Rosenberg J. Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov. 2015;22(3):303-317. doi: 10.1177/1553350614552731 [DOI] [PubMed] [Google Scholar]
- 15.Zendejas B, Hernandez-Irizarry R, Ramirez T, Lohse CM, Grossardt BR, Farley DR. Relationship between body mass index and the incidence of inguinal hernia repairs: a population-based study in Olmsted County, MN. Hernia. 2014;18(2):283-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ravanbakhsh S, Batech M, Tejirian T. Increasing body mass index is inversely related to groin hernias. Am Surg. 2015;81(10):1043-1046. [PubMed] [Google Scholar]
- 17.Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet. 2003;362(9395):1561-1571. [DOI] [PubMed] [Google Scholar]
- 18.Wang L, Yu Y, Fu S, Zhao W, Liu P. LOXL1 gene polymorphism with exfoliation syndrome/exfoliation glaucoma: a meta-analysis. J Glaucoma. 2016;25(1):62-94. doi: 10.1097/IJG.0000000000000128 [DOI] [PubMed] [Google Scholar]
- 19.Zöller B, Ji J, Sundquist J, Sundquist K. Shared and nonshared familial susceptibility to surgically treated inguinal hernia, femoral hernia, incisional hernia, epigastric hernia, and umbilical hernia. J Am Coll Surg. 2013;217(2):289-99.e1. doi: 10.1016/j.jamcollsurg.2013.04.020 [DOI] [PubMed] [Google Scholar]
- 20.Gong Y, Shao C, Sun Q, et al. Genetic study of indirect inguinal hernia. J Med Genet. 1994;31(3):187-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Utah Population Database: Overview. http://healthcare.utah.edu/huntsmancancerinstitute/research/updb/. Accessed August 15, 2018.
- 22.Villasenor M. University of Utah named number one health care system in Utah. https://healthcare.utah.edu/publicaffairs/news/2015/07/07-21-15_US_News_rankings.php. Accessed August 15, 2018.
- 23.Öberg S, Andresen K, Rosenberg J. Etiology of inguinal hernias: a comprehensive review. Front Surg. 2017;4:52. doi: 10.3389/fsurg.2017.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bettis DI, Allingham RR, Wirostko BM. Systemic diseases associated with exfoliation syndrome. Int Ophthalmol Clin. 2014;54(4):15-28. doi: 10.1097/IIO.0000000000000044 [DOI] [PubMed] [Google Scholar]
- 25.Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1(1):54-75. doi: 10.1214/ss/1177013815 [DOI] [Google Scholar]
- 26.Hemberg A, Holmberg H, Norberg M, Nordin P. Tobacco use is not associated with groin hernia repair, a population-based study. Hernia. 2017;21(4):517-523. doi: 10.1007/s10029-017-1617-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landin M, Kubasiak JC, Schimpke S, et al. The effect of tobacco use on outcomes of laparoscopic and open inguinal hernia repairs: a review of the NSQIP dataset. Surg Endosc. 2017;31(2):917-921. doi: 10.1007/s00464-016-5055-y [DOI] [PubMed] [Google Scholar]
- 28.Aquina CT, Fleming FJ, Becerra AZ, et al. Explaining variation in ventral and inguinal hernia repair outcomes: a population-based analysis. Surgery. 2017;162(3):628-639. doi: 10.1016/j.surg.2017.03.013 [DOI] [PubMed] [Google Scholar]
- 29.Liu X, Zhao Y, Gao J, et al. Elastic fiber homeostasis requires lysyl oxidase-like 1 protein. Nat Genet. 2004;36(2):178-182. doi: 10.1038/ng1297 [DOI] [PubMed] [Google Scholar]
- 30.Ritch R. Systemic associations of exfoliation syndrome. Asia Pac J Ophthalmol (Phila). 2016;5(1):45-50. doi: 10.1097/APO.0000000000000187 [DOI] [PubMed] [Google Scholar]
- 31.Pascual G, Rodríguez M, Mecham RP, Sommer P, Buján J, Bellón JM. Lysyl oxidase like-1 dysregulation and its contribution to direct inguinal hernia. Eur J Clin Invest. 2009;39(4):328-337. doi: 10.1111/j.1365-2362.2009.02099.x [DOI] [PubMed] [Google Scholar]
- 32.Siegel RC. Lysyl oxidase. Int Rev Connect Tissue Res. 1979;8:73-118. [DOI] [PubMed] [Google Scholar]
- 33.Aboobakar IF, Allingham RR. Genetics of exfoliation syndrome and glaucoma. Int Ophthalmol Clin. 2014;54(4):43-56. doi: 10.1097/IIO.0000000000000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiwani AZ, Pasquale LR. Exfoliation syndrome and solar exposure: new epidemiological insights into the pathophysiology of the disease. Int Ophthalmol Clin. 2015;55(4):13-22. doi: 10.1097/IIO.0000000000000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pasquale LR, Kang JH, Wiggs JL. Consideration for gene-environment interactions as novel determinants of exfoliation syndrome. Int Ophthalmol Clin. 2014;54(4):29-41. doi: 10.1097/IIO.0000000000000040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellón JM, Bajo A, Ga-Honduvilla N, et al. Fibroblasts from the transversalis fascia of young patients with direct inguinal hernias show constitutive MMP-2 overexpression. Ann Surg. 2001;233(2):287-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henriksen NA, Yadete DH, Sorensen LT, Agren MS, Jorgensen LN. Connective tissue alteration in abdominal wall hernia. Br J Surg. 2011;98(2):210-219. doi: 10.1002/bjs.7339 [DOI] [PubMed] [Google Scholar]
- 38.Casanova AB, Trindade EN, Trindade MRM. Collagen in the transversalis fascia of patients with indirect inguinal hernia: a case-control study. Am J Surg. 2009;198(1):1-5. doi: 10.1016/j.amjsurg.2008.07.021 [DOI] [PubMed] [Google Scholar]
- 39.Rodrigues Junior AJ, Rodrigues CJ, da Cunha AC, Jin Y, Jin Y. Quantitative analysis of collagen and elastic fibers in the transversalis fascia in direct and indirect inguinal hernia. Rev Hosp Clin Fac Med Sao Paulo. 2002;57(6):265-270. doi: 10.1590/S0041-87812002000600004 [DOI] [PubMed] [Google Scholar]
- 40.Abrahamson J. Etiology and pathophysiology of primary and recurrent groin hernia formation. Surg Clin North Am. 1998;78(6):953-972, vi. doi: 10.1016/S0039-6109(05)70364-9 [DOI] [PubMed] [Google Scholar]
- 41.van Veen RN, van Wessem KJP, Halm JA, et al. Patent processus vaginalis in the adult as a risk factor for the occurrence of indirect inguinal hernia. Surg Endosc. 2007;21(2):202-205. [DOI] [PubMed] [Google Scholar]
- 42.van Wessem KJP, Simons MP, Plaisier PW, Lange JF. The etiology of indirect inguinal hernias: congenital and/or acquired? Hernia. 2003;7(2):76-79. doi: 10.1007/s10029-002-0108-7 [DOI] [PubMed] [Google Scholar]
- 43.Jiang ZP, Yang B, Wen LQ, et al. The etiology of indirect inguinal hernia in adults: congenital or acquired? Hernia. 2015;19(5):697-701. doi: 10.1007/s10029-014-1326-5 [DOI] [PubMed] [Google Scholar]
- 44.Vad MV, Frost P, Bay-Nielsen M, Svendsen SW. Impact of occupational mechanical exposures on risk of lateral and medial inguinal hernia requiring surgical repair. Occup Environ Med. 2012;69(11):802-809. doi: 10.1136/oemed-2012-100787 [DOI] [PubMed] [Google Scholar]
- 45.Carpel EF. Pupillary dilation in eyes with pseudoexfoliation syndrome. Am J Ophthalmol. 1988;105(6):692-694. [DOI] [PubMed] [Google Scholar]
- 46.Suzuki R, Kurimoto S. Intraocular muscle function in pseudoexfoliation syndrome. Ophthalmologica. 1992;204(4):192-198. doi: 10.1159/000310293 [DOI] [PubMed] [Google Scholar]
- 47.Asano N, Schlötzer-Schrehardt U, Naumann GO. A histopathologic study of iris changes in pseudoexfoliation syndrome. Ophthalmology. 1995;102(9):1279-1290. [PubMed] [Google Scholar]
- 48.Liem MSL, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven TJ; The Coala Trial Group . Risk factors for inguinal hernia in women: a case-control study. Am J Epidemiol. 1997;146(9):721-726. doi: 10.1093/oxfordjournals.aje.a009347 [DOI] [PubMed] [Google Scholar]
- 49.Ashindoitiang JA, Ibrahim NA, Akinlolu OO. Risk factors for inguinal hernia in adult male Nigerians: a case control study. Int J Surg. 2012;10(7):364-367. doi: 10.1016/j.ijsu.2012.05.016 [DOI] [PubMed] [Google Scholar]
- 50.Fitzgibbons RJ Jr, Ramanan B, Arya S, et al. ; Investigators of the Original Trial . Long-term results of a randomized controlled trial of a nonoperative strategy (watchful waiting) for men with minimally symptomatic inguinal hernias. Ann Surg. 2013;258(3):508-515. doi: 10.1097/SLA.0b013e3182a19725 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Association of Inguinal Hernia (IH) Diagnosis in University of Utah Healthcare (UUHC) Patients (1996-2015)