Key Points
Question
What is the association of lowering prescription defaults for postoperative opioids in an electronic medical record system with prescribing?
Finding
In a prepost intervention study of 1447 procedures before the default change and 1463 procedures after the default change, lowering the default from 30 pills to 12 pills decreased the amount of opioid prescribed by more than 15% across an entire health system.
Meaning
Lowering the default number of opioid pills prescribed in an electronic medical record system is a simple, effective, cheap, and potentially scalable intervention to decrease the amount of opioid prescribed after procedures.
Abstract
Importance
Reliance on prescription opioids for postprocedural analgesia has contributed to the opioid epidemic. With the implementation of electronic medical record (EMR) systems, there has been increasing use of computerized order entry systems for medication prescriptions, which is now more common than handwritten prescriptions. The EMR can autopopulate a default number of pills prescribed, and 1 potential method to alter prescriber behavior is to change the default number presented via the EMR system.
Objective
To investigate the association of lowering the default number of pills presented when prescribing opioids in an EMR system with the amount of opioid prescribed after procedures.
Design, Setting, and Participants
A prepost intervention study was conducted to compare postprocedural prescribing patterns during the 3 months before the default change (February 18 to May 17, 2017) with the 3 months after the default change (May 18 to August 18, 2017). The setting was a multihospital health care system that uses Epic EMR (Hyperspace 2015 IU2; Epic Systems Corporation). Participants were all patients in the study period undergoing 1 of the 10 most common operations and discharged by postoperative day 1.
Intervention
The default number of opioid pills autopopulated in the EMR when prescribing discharge analgesia was lowered from 30 to 12.
Main Outcomes and Measures
Linear regression estimating the change in the median number of opioid pills and the total dose of opioid prescribed was performed. Opioid doses were converted into morphine milligram equivalents (MME) for comparison. The frequency of patients requiring analgesic prescription refills was also evaluated.
Results
There were 1447 procedures (mean [SD] age, 54.4 [17.3] years; 66.9% female) before the default change and 1463 procedures (mean [SD] age, 54.5 [16.4] years; 67.0% female) after the default change. After the default change, the median number of opioid pills prescribed decreased from 30 (interquartile range, 15-30) to 20 (interquartile range, 12-30) per prescription (P < .001). The percentage of prescriptions written for 30 pills decreased from 39.7% (554 of 1397) before the default change to 12.9% (183 of 1420) after the default change (P < .001), and the percentage of prescriptions written for 12 pills increased from 2.1% (29 of 1397) before the default change to 24.6% (349 of 1420) after the default change (P < .001). Regression analysis demonstrated a decrease of 5.22 (95% CI, −6.12 to −4.32) opioid pills per prescription after the default change, for a total decrease of 34.41 (95% CI, −41.36 to −27.47) MME per prescription. There was no statistical difference in opioid refill rates (3.0% [4 of 135] before the default change vs 1.5% [2 of 135] after the default change, P = .41).
Conclusions and Relevance
Lowering the default number of opioid pills prescribed in an EMR system is a simple, effective, cheap, and potentially scalable intervention to change prescriber behavior and decrease the amount of opioid medication prescribed after procedures.
This prepost intervention study investigates the association of lowering the default number of pills when prescribing opioids in an electronic medical record (EMR) system with the amount of opioid prescribed after procedures among patients undergoing common outpatient procedures.
Introduction
The reliance on prescription opioids for analgesia has contributed to the rise in opioid dependency.1,2,3 Prior emphasis on pain control, such as using pain as a “fifth vital sign”4 and tying reimbursement to patient satisfaction with analgesia,5 helped to establish a medical culture that led to a high use of opioid analgesics and fueled the current epidemic. This is particularly true in procedural fields where prescribers attempt to balance control of surgical pain with the risks of overprescribing opioids. Unfortunately, physicians too often rely on opioids for postoperative analgesia; the results of a recent study6 showed that more than one-third of prescriptions written by surgeons are for opioids. Furthermore, when health care professionals prescribe opioids after procedures, they do so in quantities exceeding the needs of most patients, and 67% to 92% of surgical patients have remaining unused opioids after their recovery.7 This is a potentially dangerous scenario because access to excess opioids can lead to unintended consequences, such as chronic addiction,2 nonmedical abuse,8 and unintentional overdoses.9
There have been numerous attempts to change the culture of overprescribing opioids among prescribers. Strategies like creating guidelines and educating health care professionals on more judicious prescribing practices have demonstrated variable success.10,11,12 While the amount of opioid prescribed has been slowly decreasing nationally, it still remains alarmingly high, indicating that additional methods to decrease the overprescription of opioids are needed.13
One potential avenue to help alter prescriber behavior is through the use of computerized clinician order entry systems within electronic medical record (EMR) systems. Specifically, prescriptions for opioids written through an EMR can autopopulate with a default number of pills to prescribe. Altering the default option presented to clinicians has the potential to change prescribing behavior by resetting prescribers’ beliefs about the amount of opioid needed. It also means that health care professionals have to actively increase the amount of opioid prescribed if they believe that it is necessary; this is similar in concept to “opt out” strategies that have been used to successfully alter behaviors in a diverse set of environments, ranging from enrolling in retirement benefits14 to signing up as an organ donor.15 In this study, we evaluated the association of lowering the default number of opioid pills prescribed at discharge via an EMR system with the amount of postprocedural opioid prescribed throughout a large health system.
Methods
Intervention
On May 18, 2017, the Yale New Haven Health System in New Haven, Connecticut (comprising 5 hospitals with a unified EMR system) lowered the default number of pills on all electronic opioid prescriptions from 30 to 12. This new default was applied to pill formulations of all medications that contained codeine, hydrocodone, hydromorphone hydrochloride, morphine sulfate, oxycodone, or tramadol hydrochloride. The updated default of 12 pills was considered an amount that could alter prescriber behavior while remaining sufficient for most postprocedural analgesia based on clinical experience and available evidence suggesting that 10 to 15 opioid pills would be sufficient for most operations.16 Although default prescriptions were changed, health care professionals could still alter the number of pills prescribed to any amount deemed necessary. An educational session on the default change was provided to the Department of Surgery at Yale University (New Haven, Connecticut) during a grand rounds session on the opioid epidemic and on strategies for reducing opioid overprescribing. The study was approved by the Yale University Human Investigations Committee, with need for informed consent waived.
Study Design
A prepost intervention study was conducted to compare prescribing patterns during the 3 months before the EMR default opioid prescription setting change (February 18 to May 17, 2017) with the 3 months afterward (May 18 to August 18, 2017). The multihospital Yale New Haven Health System uses Epic EMR (Hyperspace 2015 IU2; Epic Systems Corporation), and electronic prescribing is conducted through the EpicCare orders module. Analysis focused on the 3 hospitals that performed most procedures, including Yale New Haven Hospital (New Haven, Connecticut), Saint Raphael Hospital (New Haven, Connecticut), and Bridgeport Hospital (Bridgeport, Connecticut).
Study Population
To reduce confounding of complex hospital stays on the amount of analgesia prescribed, only patients undergoing outpatient surgery, defined as being discharged by postoperative day 1, were included in the study. In addition, pediatric patients (<18 years) and patients with missing data, including procedure type, date, and postoperative prescription information, were excluded.
More than 1300 different coded procedures across 14 different departments were captured during the 6-month study period. To further reduce confounding of the multitude of different procedures, analysis was performed on a subset of the 10 most common procedures, which were the same in both study periods (Table 1). However, to better understand the wider association of the default change, additional analysis of all outpatient operations was also conducted; in this analysis, operations were grouped by department of the attending physician performing the procedure.
Table 1. Demographics of Patients Undergoing the 10 Most Frequent Operations.
| Variable | Before Default Change (n = 1447) | After Default Change (n = 1463) | P Value |
|---|---|---|---|
| Age, mean (SD), y | 54.4 (17.3) | 54.5 (16.4) | .88 |
| Sex, No. (%) | |||
| Male | 479 (33.1) | 483 (33.0) | .96 |
| Female | 968 (66.9) | 980 (67.0) | |
| Race/ethnicity, No. (%) | |||
| Asian | 32 (2.2) | 32 (2.2) | .36 |
| African American | 179 (12.4) | 160 (10.9) | |
| Hispanic | 191 (13.2) | 224 (15.3) | |
| White | 1019 (70.4) | 1028 (70.3) | |
| Unknown/refused | 26 (1.8) | 19 (1.3) | |
| Patient history, No. (%) | |||
| Substance abuse | 42 (2.9) | 49 (3.3) | .49 |
| Chronic pain | 90 (6.2) | 99 (6.8) | .55 |
| Substance abuse or chronic pain | 126 (8.7) | 143 (9.8) | .32 |
| Insurance status, No. (%) | |||
| Private | 739 (51.1) | 783 (53.5) | .05 |
| Medicaid | 227 (15.7) | 220 (15.0) | |
| Medicare | 423 (29.2) | 385 (26.3) | |
| Self-pay | 36 (2.5) | 59 (4.0) | |
| Other | 22 (1.5) | 16 (1.1) | |
| Prescriber level, No. (%) | |||
| Attending physician | 138 (9.5) | 155 (10.6) | .13 |
| Fellow | 34 (2.3) | 37 (2.5) | |
| Resident | 887 (61.3) | 933 (63.8) | |
| Advanced practice professional | 388 (26.8) | 338 (23.1) | |
| Procedure type, No. (%) | |||
| Laparoscopic cholecystectomy | 288 (19.9) | 312 (21.3) | .34 |
| Thyroidectomy | 201 (13.9) | 224 (15.3) | .28 |
| Cystoscopy and treatment | 161 (11.1) | 156 (10.7) | .69 |
| Cystoureterogram with lithotripsy | 140 (9.7) | 147 (10.0) | .74 |
| Laparoscopic inguinal hernia repair | 108 (7.5) | 137 (9.4) | .06 |
| Laparoscopic appendectomy | 116 (8.0) | 113 (7.7) | .77 |
| Partial mastectomy | 132 (9.1) | 88 (6.0) | <.01 |
| Total knee arthroplasty | 112 (7.7) | 93 (6.4) | .15 |
| Parathyroidectomy | 95 (6.6) | 108 (7.4) | .39 |
| Hysteroscopy and biopsy | 94 (6.5) | 85 (5.8) | .44 |
| Amount of opioid prescribed | |||
| No. of pills, mean (SD) | 26.8 (14.1) | 21.4 (14.1) | <.01 |
| No. of pills, median (IQR) | 30 (15-30) | 20 (12-30) | <.01 |
| MME, mean (SD) | 175.3 (115.6) | 137.9 (104.1) | <.01 |
| MME, median (IQR) | 150 (100-225) | 100 (75-157.5) | <.01 |
Abbreviations: IQR, interquartile range; MME, morphine milligram equivalents.
Study Variables
Patient age, sex, race/ethnicity, insurance status, and procedure type were extracted from the EMR. In addition, patient history of substance abuse (alcohol, opioid, and other illicit substances) and chronic pain was abstracted from diagnosis codes in medical records because patients with these conditions may require higher doses of analgesia.17 Prescribers were categorized as attending physicians, fellows, residents, and advanced practice professionals, which includes nurse practitioners, advanced practice registered nurses, and physician assistants.
Outcome Measures
The primary outcome measures were the change in the median number of opioid pills and the total dose of opioid prescribed per order before the default change and after the default change. To standardize different formulations and types of opioids, doses were converted into morphine milligram equivalents (MME).18 For reference, one 5-mg pill of oxycodone is the equivalent of 7.5 MME.
Prescription Refill Rates
Given concerns that reducing default opioid prescriptions may not adequately cover patient analgesic needs, we also compared the frequency of opioid prescription refills. A medical record review was conducted to determine if any additional analgesic prescriptions were written or if the patient returned to any emergency department within our hospital system for pain-related reasons within 30 days of the operation. Simple random selection of all patients in the study period undergoing 1 of the 10 most common surgical procedures was performed among the groups before the default change and after the default change. The sample size was calculated assuming a baseline refill rate of 2% based on reported rates16 and an absolute minimal detectable increase of 8% to a refill rate of 10%. The rate of 10% was selected as the most conservative level clinically acceptable based on an informal survey of attending faculty at our institution (Yale New Haven Hospital). Using a 2-sided 5% significance level and 80% power, the sample size was calculated at 135 per group (total sample size of 270).
Statistical Analysis
Comparison of continuous variables was conducted using t test and of categorical variables using χ2 test. Nonparametric analysis of continuous variables was performed using the Wilcoxon rank sum test. Linear regression was conducted to evaluate the change in the number of opioid pills and MME prescribed before the default change and after the default change. To provide insight into when prescribers changed their prescription away from the new default, multinomial logistic regression with 3 categories was performed among patients in the period after the default change; for each covariate, we compared either a dose increase (change to higher than default) or a dose decrease (change to lower than default) with the reference level of accepting the new default of 12. All regression models were adjusted for patient age, history of substance abuse, and history of chronic pain, as well as prescriber level and procedure type. Analysis was conducted using statistical software (SAS, version 9.4; SAS Institute Inc).
Results
Cohort of Patients Undergoing the 10 Most Frequent Procedures
Over the 6-month study period, there were 2910 operations among the 10 most frequent procedures. This represented 22.3% of the total 13 027 procedures performed in this period. Of the most frequent operations, 1447 (49.7%) occurred before the default change and 1463 (50.3%) occurred after the default change. The patient population was similar in age, race/ethnicity, and insurance status during both periods, and there were no statistical differences in the percentage of patients with a history of substance abuse or chronic pain (Table 1).
Change in Prescribing Patterns
Overall, the median number of opioid pills prescribed per operation decreased from 30 (interquartile range, 15-30) before the change in the prescription default to 20 (interquartile range, 12-30) after the change in the prescription default (P < .001) (Figure 1). The percentage of prescriptions written for 30 pills decreased from 39.7% (554 of 1397) before the default change to 12.9% (183 of 1420) after the default change (P < .001), and the percentage of prescriptions written for 12 pills increased from 2.1% (29 of 1397) before the default change to 24.6% (349 of 1420) after the default change (P < .001). There was also a significant increase in the number of prescriptions written for 20 pills from 12.2% (171 of 1397) before the default change to 19.6% (278 of 1420) after the default change (P < .001).
Figure 1. Number of Opioid Pills Prescribed Before the Default Change and After the Default Change.
The prechange distribution of pills per prescription (A) is compared with the postchange distribution (B).
The results from adjusted linear regression analysis showed that the number of opioid pills decreased by 5.22 (95% CI, −6.12 to −4.32) per prescription after the default change when controlling for all other factors (Table 2). The change in total opioid prescribed decreased by 34.41 (95% CI, −41.36 to −27.47) MME after the default change.
Table 2. Adjusted Linear Regression Estimating the Number of Opioid Pills Prescribed and Total Morphine Milligram Equivalents (MME) Prescribed.
| Variable | Estimate (95% CI) | |
|---|---|---|
| No. of Pills | MME | |
| Intercept | 30.17 (27.31 to 33.02) | 227.33 (205.27 to 249.39) |
| Study period | ||
| Before default change | 1 [Reference] | 1 [Reference] |
| After default change | −5.22 (−6.12 to −4.32) | −34.41 (−41.36 to −27.47) |
| Age, y | −0.01 (−0.04 to 0.04) | −0.21 (−0.52 to 0.09) |
| Sex | ||
| Male | 1 [Reference] | 1 [Reference] |
| Female | −0.50 (−1.63 to 0.63) | −14.35 (−23.08 to −5.63) |
| Race/ethnicity | ||
| Asian | 2.43 (−0.71 to 5.57) | 17.17 (−7.10 to 41.44) |
| African American | −0.04 (−1.51 to 1.43) | −0.25 (−11.61 to 11.12) |
| Hispanic | −1.47 (−2.90 to −0.03) | −12.41 (−23.52 to −1.30) |
| White | 1 [Reference] | 1 [Reference] |
| Unknown/refused | −1.28 (−5.09 to 2.53) | −18.21 (−47.65 to 11.22) |
| Patient history | ||
| Substance abuse | 1.56 (−1.02 to 4.13) | 11.86 (−8.05 to 31.77) |
| Chronic pain | 1.60 (−0.26 to 3.46) | 21.49 (7.11 to 35.87) |
| Insurance status | ||
| Private | 1 [Reference] | 1 [Reference] |
| Medicaid | 0.99 (−0.42 to 2.40) | 10.81 (−0.10 to 21.7) |
| Medicare | −2.06 (−3.41 to −0.70) | −16.59 (−27.04 to −6.14) |
| Self-pay | −0.94 (−3.58 to 1.71) | −8.50 (−28.91 to 11.91) |
| Other | −1.05 (−5.03 to 2.92) | 10.63 (−20.05 to 41.32) |
| Prescriber level | ||
| Attending physician | 1 [Reference] | 1 [Reference] |
| Fellow | −4.18 (−7.59 to −0.76) | −23.52 (−49.93 to 2.88) |
| Resident | −0.65 (−2.25 to 0.94) | 8.55 (−6.14 to 23.2) |
| Advanced practice professional | −0.10 (−2.00 to 1.80) | −3.37 (−15.70 to 8.95) |
| Procedure type | ||
| Laparoscopic cholecystectomy | 1 [Reference] | 1 [Reference] |
| Thyroidectomy | −3.77 (−5.74 to −1.80) | −72.20 (−87.41 to −57.00) |
| Cystoscopy and treatment | −9.59 (−11.34 to −7.80) | −72.87 (−86.67 to −59.08) |
| Cystoureterogram with lithotripsy | −4.52 (−6.28 to −2.75) | −40.36 (−53.98 to 26.74) |
| Laparoscopic inguinal hernia repair | 0.79 (−1.30 to 2.88) | 6.63 (−9.54 to 22.80) |
| Laparoscopic appendectomy | −3.77 (−5.64 to −1.91) | −32.57 (−46.98 to −18.16) |
| Partial mastectomy | −3.83 (−5.43 to −2.24) | −44.30 (−56.62 to −31.98) |
| Total knee arthroplasty | 13.42 (11.24 to 15.61) | 126.60 (109.74 to 143.46) |
| Parathyroidectomy | 0.64 (−1.51 to 2.78) | −55.04 (−71.59 to −38.48) |
| Hysteroscopy and biopsy | −14.2 (−16.50 to −11.93) | −102.95 (−120.57 to −85.32) |
Factors Associated With Deviation From the New Default
Prescribers changed to a higher opioid pill count 63.5% (95% CI, 61.0%-66.0%) of the time, and the most significant factor associated with doing so was performance of total knee arthroplasty (odds ratio [OR], 4.68; 95% CI, 2.04-11.54 compared with laparoscopic cholecystectomy) (eTable 1 in the Supplement). Compared with residents, fellows were less likely to increase above the default (OR, 0.26; 95% CI, 0.11-0.57), and attending physicians had an increased odds of prescribing higher than the default, although this was not statistically significant.
Opioid pill counts were changed to an amount lower than the new default 12.7% (95% CI, 10.9%-14.4%) of the time. Patients undergoing less invasive procedures, such as cystoscopy and treatment (OR, 4.58; 95% CI, 2.31-9.06) and hysteroscopy and biopsy (OR, 3.53; 95% CI, 1.62-7.68), were more likely to receive fewer than 12 pills compared with those undergoing laparoscopic cholecystectomy. Total knee arthroplasty, which had higher odds of increasing pill counts, also had increased odds of lowering pill counts to less than the default (OR, 3.78; 95% CI, 1.07-13.38), showing that for this procedure prescribers were likely to change from the default in both directions. In addition, attending physicians were most likely to change prescriptions below the default compared with residents (OR, 2.54; 95% CI, 1.38-4.68), and advanced practice professionals were less likely to prescribe lower than the new default compared with residents (OR, 0.49; 95% CI, 0.27-0.89). There was no significant association of patient age, race/ethnicity, substance abuse history, chronic pain history, or insurance status with deviating from the default in either direction.
Change in Refill Frequency
There were no significant demographic differences between the sample before the default change and the sample after the default change (n = 270) selected to evaluate opioid prescription refill rates or in the distribution of surgical procedures performed (eTable 2 in the Supplement). The total amount of opioid prescribed among this random sample was similar to that in the overall sample in both the period before the default change and the period after the default change (Table 2). Evaluation of prescription refill rates showed that there was no statistical difference in opioid refill rates before and after the intervention (3.0% [4 of 135] before the default change vs 1.5% [2 of 135] after the default change; P = .41) (eTable 2 in the Supplement).
Association of Lowering Pill Count Defaults With All Outpatient Procedures
Overall, there were 6461 operations before the default change and 6566 operations after the default change. The patient demographics and the proportion of operations performed by department between the period before the default change and the period after the default change were generally similar (eTable 3 in the Supplement). Outpatient procedures were performed by 14 different departments, mostly with the same proportions before and after the default change, with notable exceptions of an increase in medicine and plastic surgery procedures and a decrease in orthopedic procedures.
For all patients undergoing outpatient surgery, the percentage of prescriptions written for 12 opioid pills increased from 1.8% (111 of 6088) before the default change to 17.9% (1106 of 6188) after the default change (P < .001) (eFigure 1 in the Supplement). The percentage of prescriptions written for 30 pills decreased from 35.6% (2170 of 6088) before the default change to 17.0% (1051 of 6188) after the default change (P < .001).
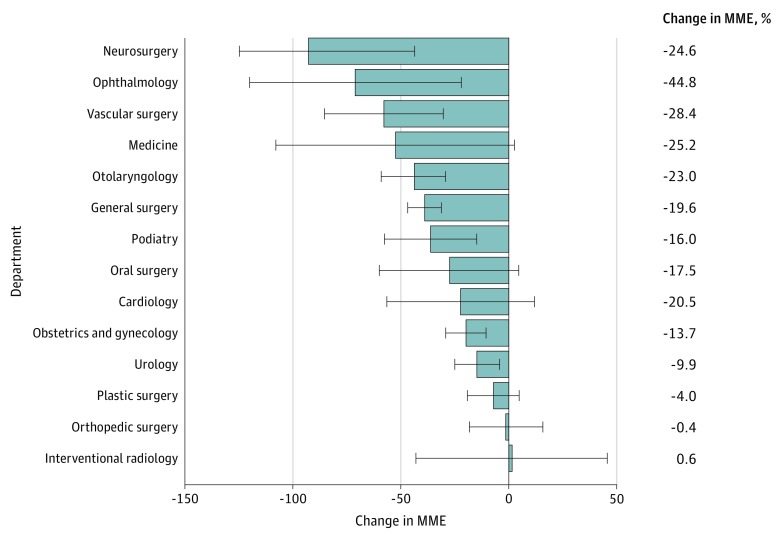
Adjusted linear regression models estimating the number of opioid pills prescribed demonstrated decreases of 4.23 (95% CI, −4.81 to −3.66) pills and 26.82 (95% CI, −22.34 to −31.31) MME across all outpatient procedures after the default change (eTable 4 in the Supplement). Significant decreases in the mean amount of postoperative opioid prescribed were observed in 8 of 14 departments in the hospital system, ranging from a decrease of 14.7 MME in urology to 92.6 MME in neurosurgery (Figure 2 and eTable 5 in the Supplement).
Figure 2. Mean Change in the Amount of Opioid Prescribed by Department.
The departments are arranged in descending order by the mean decrease in morphine milligram equivalents (MME), and the 95% CIs are shown. The percentage change in MME prescribed is shown at the right. Specific prescription amounts by department are available in eTable 5 in the Supplement.
Discussion
Lowering the default number of opioid pills prescribed in an EMR system is a simple, effective, essentially cost-free, and potentially wide-reaching intervention to change prescriber behaviors. Changing electronic prescribing defaults helped decrease the mean amount of opioid analgesia prescribed to patients undergoing outpatient procedures by more than 15%. When evaluating the association over our entire hospital system, the decrease in the amount of opioid prescribed during 3 months was the equivalent of almost 25 000 fewer pills of 5 mg of oxycodone distributed. In addition, lowering the prescription defaults required only a change in computer programming that was completed within days. The costs of this intervention included only the nominal technical support needed to activate the change in Epic EMR, making this a cost-effective way to influence prescribing habits of health care professionals.
The EMR change also immediately altered prescribing patterns throughout a wide range of departments across our health system with multiple hospitals. Most procedural departments had a significant reduction in the amount of opioid prescribed. Given the fact that electronic prescribing now represents the vast majority of prescriptions written nationwide, altering electronic prescribing defaults is an opportunity to not only influence multiple departments in a hospital system but also change practice patterns in health systems across the country.19
While the most common number of opioid pills prescribed changed from 30 to 12 after the intervention, there was also a significant increase in the number of prescriptions written for 20 pills. This likely represents prescribers who were influenced by the new default of 12 but believed that this was too low and increased their prescription to 20 pills, an amount still lower than the previous default. This can be attributed to “anchoring” produced by the new default. Well described in the behavioral economic literature,20 anchoring reflects the idea that human adjustments of estimates are based on a given starting value. In this case, estimates of the number of opioid pills needed for analgesia were anchored around the default number of pills presented, and a new, lower anchor helped decrease overall prescribing.
Residents are the least likely prescriber level to deviate from the defaults, and attending physicians are the most likely. This may point to the fact that residents are less frequently involved in the long-term outpatient postoperative care of patients and have decreased experience to drawn on in terms of postoperative analgesic management, causing them to more often use the defaults. In line with this trend is the fact that more experienced fellows are more likely than residents to deviate from defaults. In addition, prescribers may deviate based on the type of operation (especially for knee arthroplasty, with a particularly wide practice pattern for this operation), which suggests that procedure-specific defaults could be even more effective in altering prescriber behavior.
Concerns that lowering the default number of opioid pills prescribed would leave patients with insufficient analgesia were unsubstantiated. Our results demonstrated that the number of additional opioid prescriptions required by patients remained unchanged before and after the intervention and was consistent with the analgesia refill rates reported elsewhere.16 This may not be surprising given evidence showing that even 12 opioid pills exceeds the needs of most patients after outpatient procedures.16 This result, combined with the aforementioned anchoring association, suggests that an even lower default may be able to simultaneously provide sufficient analgesia while further reducing the amount of opioid prescribed. Future study is warranted to identify an optimal default setting that minimizes opioid prescriptions while providing sufficient analgesia.
The implementation of low prescribing defaults can be successful in areas where prior programs directed at the opioid crisis have found shortcomings. For example, there have been increasing regulations placed on prescribers to attempt to change prescribing patterns. Notably, legislative initiatives have limited the maximal number of days for which opioid prescriptions can be written.21 However, proposed limits are commonly 7 days for acute pain, far longer than most patients will need.16 Furthermore, a study22 of physicians in Wisconsin demonstrated that a significant number are unaware of such laws, and analysis of prior legal restrictions of opioid prescribing have found that these result in minimal influence.23 In contrast, lowering EMR prescribing defaults encourages the use of opioid amounts far less than 7 days’ worth and required minimal additional dissemination of program information, which is particularly helpful in academic medical systems where new trainees are arriving every year and are not always prepared with proper opioid prescribing education.24 However, health care professional education is still essential and can act synergistically with a default change because a low default can serve as a constant reinforcement of lessons taught.
Limitations
Our study has several limitations. First, this work reflects the experience of a single health system that benefits from a uniform EMR, and it remains unclear if these results can be reproduced at institutions where the EMR is not uniform or that use a different system. Second, while the findings demonstrate that this intervention has near-immediate results in decreasing opioid prescriptions, the study period was brief, and long-term follow-up is needed to determine if the changes observed are lasting. Third, this was not a controlled trial, and there are other unaccounted factors that could have influenced a change in prescribing patterns. In particular, there has been ever-increasing awareness and media attention paid to the opioid epidemic, and 1 potential explanation for our findings herein is the continuation of a general trend in decreased opioid prescribing. However, analysis of 3 to 6 months before the intervention showed that opioid prescribing was essentially the same as the 3 months immediately before the intervention, which suggests that the decrease in prescribing was likely attributable to our intervention (eFigure 2 in the Supplement). In addition, opioid prescribing education was provided during general surgery grand rounds when the new default was introduced, which could have influenced prescribing rates; however, substantial decreases in prescription amounts observed in departments that did not receive formal education suggest that the default change had an independent association. Fourth, analysis of opioid refill rates was limited to those within our health system, and we cannot know for sure whether patients may have gone to other locations for additional pain medication, including other hospitals or primary care physicians not in our hospital system. Moreover, using opioid refill rates as a surrogate for sufficient analgesia may be an inadequate measure because some patients may not request opioid refills even if they continue to have pain.
Conclusions
Curtailing the opioid epidemic is a national priority and requires a multifaceted approach. Lowering the default quantity of opioid pills prescribed after procedures via an EMR system is a simple, effective, cheap, and potentially wide-reaching intervention that can be harnessed to help change the culture of opioid overprescribing among health care professionals.
eTable 1. Multinomial Regression of Changing Prescriptions to Lower (<12) or Higher (>12) Than New Defaults Compared to Accepting New Default
eTable 2. Demographics and Number of Analgesic Refills Needed Among Random Sample
eTable 3. Characteristics of All Operative Patients Pre- and Post-Default Change
eTable 4. Linear Regression Analysis of Change in Number of Pills of Opioid and Morphine Milligram Equivalent Prescribed
eTable 5. Amount of Opioid Prescribed (in Morphine Milligram Equivalents) Pre- and Post-Default Change, by Department
eFigure 1. Number of Pills of Narcotic Prescribed Among All Operations A. Pre- and B. Post-Default Change
eFigure 2. Trend in Mean Prescribing Patterns Before and After Default Change
References
- 1.McLellan AT, Turner B. Prescription opioids, overdose deaths, and physician responsibility. JAMA. 2008;300(22):2672-2673. doi: 10.1001/jama.2008.793 [DOI] [PubMed] [Google Scholar]
- 2.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. doi: 10.1136/bmj.g1251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morone NE, Weiner DK. Pain as the fifth vital sign: exposing the vital need for pain education. Clin Ther. 2013;35(11):1728-1732. doi: 10.1016/j.clinthera.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tefera L, Lehrman WG, Conway P. Measurement of the patient experience: clarifying facts, myths, and approaches. JAMA. 2016;315(20):2167-2168. doi: 10.1001/jama.2016.1652 [DOI] [PubMed] [Google Scholar]
- 6.Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic–prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med. 2015;49(3):409-413. doi: 10.1016/j.amepre.2015.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066-1071. doi: 10.1001/jamasurg.2017.0831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154-163. doi: 10.1056/NEJMra1508490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voepel-Lewis T, Wagner D, Tait AR. Leftover prescription opioids after minor procedures: an unwitting source for accidental overdose in children. JAMA Pediatr. 2015;169(5):497-498. doi: 10.1001/jamapediatrics.2014.3583 [DOI] [PubMed] [Google Scholar]
- 10.Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018;267(3):468-472. [DOI] [PubMed] [Google Scholar]
- 11.Franklin GM, Mai J, Turner J, Sullivan M, Wickizer T, Fulton-Kehoe D. Bending the prescription opioid dosing and mortality curves: impact of the Washington State opioid dosing guideline. Am J Ind Med. 2012;55(4):325-331. doi: 10.1002/ajim.21998 [DOI] [PubMed] [Google Scholar]
- 12.Cochella S, Bateman K. Provider detailing: an intervention to decrease prescription opioid deaths in Utah. Pain Med. 2011;12(suppl 2):S73-S76. doi: 10.1111/j.1526-4637.2011.01125.x [DOI] [PubMed] [Google Scholar]
- 13.Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704. doi: 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thaler RH, Benartzi S. Save More Tomorrow: using behavioral economics to increase employee saving. J Polit Econ. 2004;112(S1):S164-S187. doi: 10.1086/380085 [DOI] [Google Scholar]
- 15.Johnson EJ, Goldstein DG. Defaults and donation decisions. Transplantation. 2004;78(12):1713-1716. doi: 10.1097/01.TP.0000149788.10382.B2 [DOI] [PubMed] [Google Scholar]
- 16.Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265(4):709-714. doi: 10.1097/SLA.0000000000001993 [DOI] [PubMed] [Google Scholar]
- 17.Volkow ND, McLellan AT. Opioid abuse in chronic pain: misconceptions and mitigation strategies. N Engl J Med. 2016;374(13):1253-1263. doi: 10.1056/NEJMra1507771 [DOI] [PubMed] [Google Scholar]
- 18.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain: United States, 2016. JAMA. 2016;315(15):1624-1645. doi: 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gabriel MH, Swain M. E-Prescribing Trends in the United States. Washington, DC: Office of the National Coordinator for Health Information Technology; July 2014. ONC Data Brief 18. [Google Scholar]
- 20.Tversky A, Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124-1131. doi: 10.1126/science.185.4157.1124 [DOI] [PubMed] [Google Scholar]
- 21.Huff C. States aim to limit opioid prescriptions. https://acpinternist.org/archives/2016/10/laws.htm. Published October 2016. Accessed January 2018.
- 22.Wolfert MZ, Gilson AM, Dahl JL, Cleary JF. Opioid analgesics for pain control: Wisconsin physicians’ knowledge, beliefs, attitudes, and prescribing practices. Pain Med. 2010;11(3):425-434. doi: 10.1111/j.1526-4637.2009.00761.x [DOI] [PubMed] [Google Scholar]
- 23.Meara E, Horwitz JR, Powell W, et al. State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med. 2016;375(1):44-53. doi: 10.1056/NEJMsa1514387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chiu AS, Healy JM, DeWane MP, Longo WE, Yoo PS. Trainees as agents of change in the opioid epidemic: optimizing the opioid prescription practices of surgical residents. J Surg Educ. 2017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Multinomial Regression of Changing Prescriptions to Lower (<12) or Higher (>12) Than New Defaults Compared to Accepting New Default
eTable 2. Demographics and Number of Analgesic Refills Needed Among Random Sample
eTable 3. Characteristics of All Operative Patients Pre- and Post-Default Change
eTable 4. Linear Regression Analysis of Change in Number of Pills of Opioid and Morphine Milligram Equivalent Prescribed
eTable 5. Amount of Opioid Prescribed (in Morphine Milligram Equivalents) Pre- and Post-Default Change, by Department
eFigure 1. Number of Pills of Narcotic Prescribed Among All Operations A. Pre- and B. Post-Default Change
eFigure 2. Trend in Mean Prescribing Patterns Before and After Default Change