Key Points
Question
What are the cultural and structural factors of surgical training associated with residency and career dissatisfaction in residents who become pregnant and have children during training?
Findings
In this nationwide survey of childbearing general surgery residents, 3 risk factors were associated with professional dissatisfaction: altering fellowship training plans owing to difficulty balancing childbearing with the original choice of subspecialty; lack of formal maternity leave policies; and perception of stigma associated with pregnancy.
Meaning
To improve professional fulfillment and reduce risk of attrition in residents who undergo childbearing during residency, training programs must implement formal maternity leave policies, reduce pregnancy-related stigma, and foster mentor-mentee relationships supporting work-life integration and fellowship selection.
Abstract
Importance
Previous work shows women who have children during surgical residency face difficulty balancing childbearing with training, which negatively affects residency and career satisfaction. Little is known about the factors that drive professional discontent.
Objective
To determine factors associated with professional dissatisfaction for childbearing residents.
Design, Setting, and Participants
Self-administered survey questionnaire electronically distributed through the Association of Program Directors in Surgery, the Association of Women Surgeons, and targeted Twitter and Facebook platforms. The survey was distributed in January 2017 to surgeons who delivered at least 1 child during a US general surgery residency and was available online for 4 weeks.
Main Outcomes and Measures
Respondents were reported to be dissatisfied with their residency if they indicated agreement that they considered leaving residency owing to challenges surrounding childbearing (considered leaving). Respondents were reported to be unhappy with their career if they indicated agreement with statements that (1) given an opportunity to revisit their job choice, they would choose a nonsurgical career more accommodating of motherhood (revisit career choice) or (2) they would advise a female medical student against a surgical career owing to difficulties balancing motherhood with the profession (advise against surgery). Logistic regression was used to determine predictors of agreement with each of the 3 statements of professional dissatisfaction.
Results
In total, 347 women responded to the survey and reported 452 pregnancies, and the mean (SD) age was 30.5 (2.7) years. One hundred seventy-nine respondents (51.6%) agreed with at least 1 statement of residency or career dissatisfaction. Lack of a formal maternity leave policy was associated with “considered leaving” (odds ratio [OR], 1.83; 95% CI, 1.07-3.10). Perception of stigma during pregnancy was associated with “revisit career choice” (OR, 1.79; 95% CI, 1.01-3.19). Changing fellowship plans owing to perceived difficulty balancing motherhood with the originally chosen subspecialty was associated with all 3 markers of residency and career dissatisfaction (“considered leaving” OR, 2.68; 95% CI, 1.30-5.56; “revisit career choice” OR, 2.23; 95% CI, 1.13-4.43; and “advise against surgery” OR, 2.44; 95% CI, 1.23-4.84).
Conclusions and Relevance
Surgery residents who perceived stigma during pregnancy, did not have a formal institutional maternity leave policy, or altered their fellowship training plans because of challenges of childbearing expressed greater professional dissatisfaction. Mentorship in subspecialty selection and work-life integration, interventions to reduce workplace bias, and identification of obstacles to establishment of maternity leave policies are needed to enhance professional fulfillment for childbearing residents.
This survey study identifies factors associated with professional dissatisfaction among childbearing residents in surgery.
Introduction
The number of women in medical school is increasing, now composing half of US graduates in 2018.1 Despite reduction in sex disparity among trained physicians, women represent just one-third of applicants to general surgery residencies.2 Perception of a stressful career causing conflict between professional and family responsibilities has been cited as a factor dissuading students from pursuing training in surgery.3,4,5 After entering surgical residencies, women have higher rates of attrition than men (25% vs 15%),6,7,8 with uncontrollable lifestyle being a commonly reported reason for leaving the profession.6 Studies investigating the effect of occupational demands on a female surgeon’s ability to bear children describe reproductive challenges such as infertility, need for assisted reproductive technology, and increased rates of perinatal complications.9,10 However, studies capturing the views of women surgeons who begin families during training have been limited.
We previously published results of a national survey of women surgeons who had at least 1 child during residency, describing their perspectives and the potential effect on training. This study reported responses on 5 broad themes pertaining to workplace culture during pregnancy, maternity leave policies, lactation support, childcare assistance, and career and residency satisfaction following childbirth.11 More than one-third of respondents reported seriously considering leaving residency owing to the challenges of balancing residency with pregnancy and motherhood.
This study builds on the results of the prior publication by exploring important remaining questions with regards to the cultural and structural factors within residency that influence professional satisfaction. Discontent among childbearing residents reflects a conundrum in the current training paradigm that may contribute to the surgical sex gap and workforce shortage. To better answer these highly complex issues and inform future policy changes to support childbearing residents, we a priori planned an in-depth analysis of factors associated with residency and career dissatisfaction. We present the findings of this analysis to help surgical leaders identify effective policy improvements to mitigate risk of professional dissatisfaction in our future surgical workforce.
Methods
We analyzed data from a 2017 national survey of women who were pregnant and delivered at least 1 child during surgical training. Questions were structured as statements to which respondents indicated their agreement on a 4-point Likert scale, from strongly agree, agree, disagree, to strongly disagree. Responses were dichotomized, with those categorized as “agree” representing the sum of agree and strongly agree and “disagree” representing the sum of disagree and strongly disagree. Demographic and program information, number of pregnancies and stage of training during pregnancy, and past or anticipated graduation date were collected. Development and findings of this survey were previously reported, and the survey is available online.11 A link to the survey was electronically distributed to active members of the Association of Women Surgeons, to members of the Association of Program Directors in Surgery listserv, and through Twitter and Facebook. Program directors were asked to forward the survey to current and past women trainees. Two large private Facebook groups were used, including the Physician Moms Group (67 156 participants) and the Surgeon Moms Group (960 participants), both of whose membership is by invitation of another physician or surgeon. The survey was distributed in January 2017 and was available online for 4 weeks. Responses were anonymous, and participants were not remunerated. Completion of the survey inferred consent. This study was approved by the Association of Program Directors in Surgery Committee on Research, and the Partners Human Research Committee institutional review board granted exemption.
Study Participants
Responses from women who were pregnant and delivered 1 or more children during an Accreditation Council for Graduate Medical Education–accredited US general surgery training program, and who completed residency in 2007 or later, were examined. Responses of those who had a child during training but did not complete surgical residency were included if the respondent’s year of graduation was expected to be 2007 or later.
Independent Variables and Outcomes
Respondents were queried about cultural and structural characteristics of their training program including perceptions on working while pregnant, maternity leave policies, breastfeeding and lactation, childcare and motherhood, the presence of stigma, and satisfaction with residency program and colleague support. Data were collected on postgraduate subspecialty training plans before and after pregnancy. Respondents who altered their fellowship training plans after pregnancy and agreed with the statement, “I changed my surgical subspecialty due to difficulty balancing pregnancy/motherhood with the demands of my original choice of subspecialty,” were included in further analysis.
Outcome variables included 3 statements that were developed to assess professional satisfaction. These were modified from similar measures used to evaluate job satisfaction in comprehensive national surveys of practicing surgeons, physicians, and surgical residents.8,12,13,14,15 Simple or general questions about professional fulfillment have been found to be insufficient to assess the multiple variables contributing to physicians’ occupational happiness,14 suggesting a multimodal approach improves understanding. Because residency takes place during a finite period, professional satisfaction was differentiated into categories of residency satisfaction and overall contentment with the surgical career. Participants were reported to be unhappy with their residency if they indicated agreement with the statement, “my experience of pregnancy/motherhood during residency made me strongly reconsider whether I wanted to stay in surgery” (“considered leaving”). Respondents were reported to be unhappy with their career if they indicated agreement with the statements: (1) “if I could choose again, I would choose a career more accommodating of parenthood than surgery” (“revisit career choice”); or (2) “if a female medical student came to me for advice, I would caution her against choosing surgery because of the difficulty of balancing a surgical career with motherhood” (“advise against surgery”).
Statistical Analysis
Multivariate logistic regression was used to determine independent factors associated with agreement with each of the 3 statements on professional dissatisfaction. Covariates with a P value of .20 or less on univariate analysis were included in the multivariate models. Multicollinearity was assessed using the variance inflation factor. A P value of .05 or less was accepted as statistically significant, and P values were 2-sided. Data were analyzed using Stata, version 14.0 (StataCorp).
Results
A total of 347 women responded to the survey and met inclusion criteria. They reported a total of 452 pregnancies during residency. Given the methods of survey distribution, the response rate could not be determined. Eighty-three percent of respondents (273 of 327) had at least 1 pregnancy during clinical (nonresearch) training, with more than 25% (n = 100 of 346) reporting more than 1 pregnancy during residency. Most pregnancies took place during or after the third postgraduate year. Most respondents were residents of an academic training program with at least 4 chief residents per class, with equal geographical representation from the 4 regions of the country (West, Midwest, South, and Northeast) (Table 1).
Table 1. Participant Demographics.
| Participant Characteristics (N = 347a) | No. (%) |
|---|---|
| Current role | |
| Practicing surgeon | 159 (45.8) |
| Fellow | 53 (15.3) |
| Resident | 135 (38.9) |
| Past or anticipated residency completion, y | |
| 2007-2009 | 24 (6.9) |
| 2010-2012 | 53 (15.3) |
| 2013-2015 | 79 (22.8) |
| 2016-2018 | 136 (39.2) |
| 2019-2022 | 55 (15.9) |
| Pregnancies during residency, No. (n = 346) | |
| 1 | 246 (71.1) |
| 2 | 94 (27.2) |
| 3 | 6 (1.7) |
| Level of training during pregnancyb (n = 327) | |
| PGY 1 | 16 (4.9) |
| PGY 2 | 41 (12.5) |
| PGY 3 | 72 (22.0) |
| PGY 4 | 55 (16.8) |
| PGY 5 | 89 (27.2) |
| Research yc | 54 (16.5) |
| Survey access (n = 346) | |
| Physician moms group | 56 (16.2) |
| Surgeon moms group | 96 (27.7) |
| Link emailed from program director | 79 (22.8) |
| Link emailed from other | 99 (28.6) |
| 16 (4.6) | |
| Program characteristics | |
| Type of program (n = 342) | |
| Academic | 297 (86.8) |
| Independent | 45 (13.2) |
| Program size | |
| 1-3 Chief residents | 48 (13.8) |
| 4-6 Chief residents | 173 (49.9) |
| ≥7 Chief residents | 126 (36.3) |
| Geographic locationd (n = 346) | |
| Northeast | 104 (30.1) |
| Midwest | 82 (23.7) |
| West | 75 (21.7) |
| South | 85 (24.6) |
| Program had formal maternity leave policy | |
| Yes | 121 (34.9) |
| No | 168 (48.4) |
| Unknown | 58 (16.7) |
| Hospital had lactation facility other than bathroom | |
| Yes | 220 (63.4) |
| No | 96 (27.7) |
| Unknown | 31 (8.9) |
| Hospital/program offered childcare supporte | |
| Yes | 64 (18.4) |
| No | 262 (75.5) |
| Unknown | 21 (6.1) |
Abbreviation: PGY, postgraduate year.
Each question was answered by more than 90% of participants except where otherwise noted.
Women who had more than 1 child and had at least 1 during clinical residency were listed under the earliest postgraduate year they were pregnant.
Women were listed under research years only if they had all their children during nonclinical time
Northeast: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania; Midwest: Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; West: Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon, and Washington; South: Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, Washington, DC, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, and Texas.
Childcare support included any of the following: monetary support, backup childcare, and/or preferential childcare enrollment.
Fifty-two percent of respondents (n = 180 of 346) agreed with at least 1 statement of professional dissatisfaction. Thirty-nine percent of respondents (n = 135 of 346) agreed with “considered leaving,” 27% of respondents (n = 94 of 346) agreed with “revisit career choice,” and 30% (n = 102 of 346) agreed with “advise against surgery.”
On univariate analysis, professional dissatisfaction was associated with perceptions of negative stigma during pregnancy, lack of formal program maternity leave policies, dissatisfaction with mentorship on integrating career with motherhood, and changing subspecialty owing to perceived difficulties balancing childbearing with the originally selected subspecialty (Table 2).
Table 2. Univariate Analysis.
| Participants’ Reported Training Experience | Surrogate Markers of Career Dissatisfaction in Residency | |||||
|---|---|---|---|---|---|---|
| “My Experience of Pregnancy/Motherhood During Residency Made Me Strongly Reconsider Whether I Wanted to Stay in Surgery” (Considered Leaving)a | “If I Could Choose Again, I Would Choose a Career More Accommodating of Parenthood Than Surgery” (Revisit Career Choice)b | “If a Female Medical Student Came to Me for Advice, I Would Caution Her Against Choosing Surgery Because of the Difficulty of Balancing a Surgical Career With Motherhood” (Advise Against Surgery)c | ||||
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Had lighter work schedule during pregnancy | 0.8 (0.4-1.5) | .50 | 1.0 (0.5-2.0) | .90 | 1.1 (0.6-2.1) | .80 |
| Felt negative stigma associated with pregnancy | 1.9 (1.2-3.0)d | .006d | 1.7 (1.0-2.8)d | .03d | 1.2 (0.7-1.9) | .50 |
| Maternity leave >6 wk | 1.2 (0.7-2.1) | .50 | 0.8 (0.5-1.5) | .50 | 1.1 (0.6-2.0) | .80 |
| Program not reported to have a formal maternity leave policy | 1.9 (1.2-3.1)d | .01d | 1.6 (0.9-2.7) | .09 | 1.8 (1.0-3.1)d | .04d |
| Program provided childcare support | 1.2 (0.7-2.0) | .60 | 0.8 (0.4-1.4) | .40 | 1.0 (0.6-1.9) | .90 |
| Had access to adequate lactation facilities | 0.6 (0.4-1.0) | .05 | 0.9 (0.6-1.5) | .80 | 0.8 (0.5-1.4) | .50 |
| Felt comfortable to scrub out of case to pump | 0.5 (0.3-1.1) | .08 | 0.9 (0.4-1.8) | .70 | 0.8 (0.4-1.7) | .60 |
| Satisfied with mentorship regarding difficulties of motherhood | 0.6 (0.4-1.0)d | .04d | 0.6 (0.4-1.0) | .05 | 0.6 (0.3-1.0)d | .04d |
| Changed fellowship plans because of difficulty balancing pregnancy/motherhood and original choice of subspecialty | 2.7 (1.5-5.0)d | .001d | 2.1 (1.1-3.9)d | .02d | 2.2 (1.2-4.1)d | .01d |
| Had female leadership in program | 0.9 (0.5-1.5) | .60 | 1.2 (0.7-1.9) | .6 | 0.8 (0.5-1.4) | .40 |
Of all participants, 39% agreed.
Of all participants, 27% agreed.
Of all participants, 30% agreed.
Statistically significant.
Independent risk factors contributing to each of the 3 measures of professional dissatisfaction are listed in Table 3. Changing subspecialty owing to the perceived challenges of balancing motherhood with the surgeon’s original preference was independently associated with agreement with all 3 statements of professional discontent. Lack of formal institutional maternity leave policy was associated with “considered leaving.” Perceptions of negative stigma associated with pregnancy was associated with “revisit career choice.”
Table 3. Factors Independently Associated With Career Dissatisfaction Among Pregnant Surgical Residents.
| Factor | OR (95% CI) | ||
|---|---|---|---|
| Lack of Institutional Maternity Leave Policy at Respondent’s Residency Program | Perception of Negative Stigma Associated With Being a Pregnant Resident | Changed Fellowship Plans Because of Difficulty Balancing Childbearing With Original Choice of Subspecialty | |
| “My experience of pregnancy/motherhood during residency made me strongly reconsider whether I wanted to stay in surgery” (considered leaving)a |
1.83 (1.07-3.10) | Not significant | 2.68 (1.30-5.56) |
| “If I could choose again, I would choose a career more accommodating of parenthood than surgery” (revisit career choice)b |
Not significant | 1.79 (1.01-3.19) | 2.23 (1.13-4.43) |
| “If a female medical student came to me for advice, I would caution her against choosing surgery because of the difficulty of balancing a surgical career with motherhood” (advise against surgery)c |
Not significant | Not significant | 2.44 (1.23-4.84) |
Abbreviation: OR, odds ratio.
Of all participants, 39% responded yes.
Of all participants, 27% responded yes.
Of all participants, 30% responded yes.
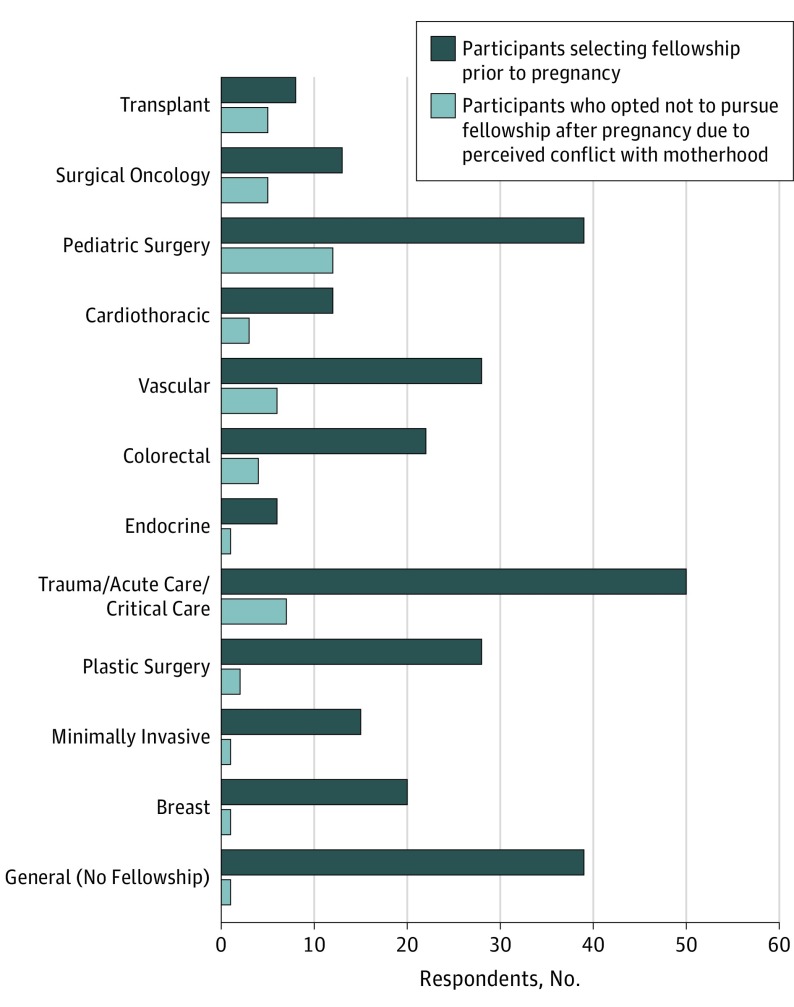
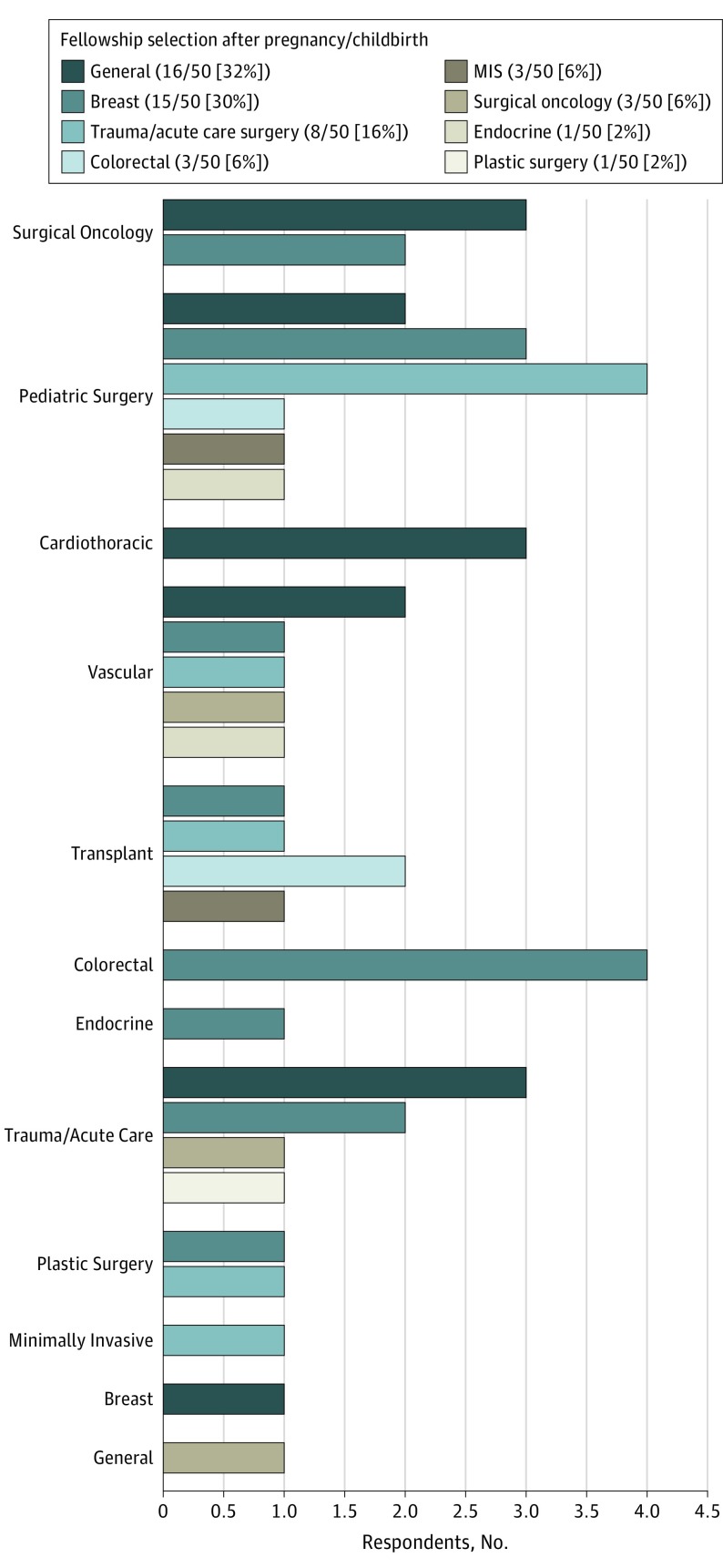
Fifty of 328 respondents (15.3%) altered their plans for fellowship training owing to perceived challenges integrating motherhood with their originally selected subspecialty. Those who originally intended to pursue transplant (n = 5 of 8 [62.5%]), surgical oncology (n = 5 of 13 [38.46%]), and pediatric surgery (n = 12 of 39 [30.77%]) fellowships were most likely to change their postgraduate plans (Figure 1). These women most commonly did not pursue fellowship (n = 16 of 50 [32.0%]), switched to breast surgery (n = 15 50 [30.0%]), or switched to trauma and acute care surgery (n = 8 of 50 [16.0%]). Figure 2 demonstrates subsequent postgraduate or fellowship plans of the 50 respondents who altered their fellowship choices after their pregnancies.
Figure 1. Changes in Fellowship Selection Before and After Pregnancy/Childbirth.
Figure 2. Fellowship Selection in Respondents Who Changed Fellowship Training Plans After Pregnancy/Childbirth.
MIS indicates minimally invasive surgery.
Discussion
The results of this national survey characterized several sources of professional dissatisfaction in participants who were pregnant and delivered a child during surgical training: (1) altering career trajectory owing to difficulty balancing childbearing with the original choice of subspecialty, (2) lack of formal institutional maternity leave policies, and (3) perception of a negative stigma associated with pregnancy. This builds on previous work describing the experience of pregnancy during residency11 by identifying the sources of greatest strain that may benefit from increased support and intervention.
A 2018 report published by the American Medical Association projecting physician workforce volume predicted a shortage of 29 000 surgeons by 2030.16 As demand for surgeons outpaces supply, resident attrition is of significant concern.17,18 A 2017 meta-analysis6 showed that women leave surgical training programs more often than their male counterparts, commonly citing uncontrollable lifestyle as the cause. Thirty-nine percent of participants in our survey indicated they had seriously considered leaving their residency, significantly higher than the 15% reported among all general surgery trainees in the 2008 National Study of Expectations and Attitudes of Residents in Surgery survey.19 This suggests women who become pregnant during training may be at particularly high risk for attrition.
Participants in this study who changed their fellowship training plans owing to difficulty balancing pregnancy and childcare with their original fellowship choice were at greatest risk for professional discontent. Studies of the factors driving surgical career selection show both sexes place equal value on interest in the field, intellectual challenge, technical aspects, and clinical opportunities, but women may be more likely to be influenced by lifestyle when choosing their specialty.20 Female surgeons spend more time fulfilling parenting obligations,21 are more likely to report that child-rearing has slowed their career,22 and experience more work-home conflicts than their male colleagues.21 These conflicts are linked to higher levels of burnout and unhappiness with the profession.13,22 The results of this survey show that women residents who alter their subspecialty plans after pregnancy most commonly forgo fellowship training altogether. Discontent with this decision appears to affect both residency and overall career satisfaction and may stem from a commonly held belief among surgical residents that subspecialty training is important to improve future lifestyle, compensation, and marketability for jobs.19 Sacrificing career prospects and the intellectual rewards of a preferred subspecialty to reconcile domestic duties may reduce enthusiasm to complete training. Role models of the same sex and subspecialty are essential to challenge negative stereotypes23,24 and demonstrate that the rewards of the desired subspecialty are commensurate with the commitment required to complete training. Women mentors may be better aligned to provide experience-based advice on balancing childbearing and career, but the scarcity of women in senior faculty positions requires novel approaches to ensure trainees have access to such role models. Residents should be reminded that multiple mentors of both sexes may be necessary to address different facets of their career.20,25 Structured mentoring programs and planned faculty-resident social interactions have been shown to be effective in reducing burnout,26 in encouraging pursuit of a particular fellowship,27,28 and in increasing faculty approachability when trainees face personal strain.29
Nearly half the respondents of this study reported their training program lacked a formal maternity leave policy, which was associated with the desire to withdraw from residency. Other authors have suggested that pregnant residents in programs without detailed maternity policies experience negative influences from their colleagues who are asked to unexpectedly cover their workload.30 Structured service coverage plans that provide equal distribution of responsibilities, with the pregnant resident completing more difficult rotations earlier in pregnancy, may reduce resentment from peers and increase predictability in subsequent maternity leave. Support for pregnancy in graduate medical education is widely variable, with programs only required to comply with US government laws. Although the American Board of Surgery reformatted their website to clarify availability of flexible training tracks,11,31,32 residency programs are not required by the Accreditation Council for Graduate Medical Education to offer these alternate pathways to accommodate parental leave.33 The increased risk of residency dissatisfaction in participants from programs without leave policies demonstrates the need for collaboration between surgical training program directors, Accreditation Council for Graduate Medical Education leaders, and the American Board of Surgery to form a unified stance on parental leave policies including implementation of alternate training tracks.
Sixty percent of respondents to this survey indicated that pregnancy during residency was correlated with stigma, similar to results of a 2008 survey of members of the American College of Surgeons that reported 67% of women surgeons had perceived negative opinions of pregnancy during training.34 Qualitative interviews with pregnant residents describe unease about diminished reputation, including being viewed as “a burden on colleagues,” “lazy,” or “not carrying my weight.”35 These concerns may be driven by faculty who subtly discourage pregnancy during training, with 61% of general surgery program directors indicating that a female trainee’s performance is negatively influenced by becoming a mother35 and 50% of postmatch fourth-year medical students reporting questions regarding plans for pregnancy during their surgical residency interviews.36 This study suggests perception of stigma related to pregnancy is associated with dissatisfaction with the surgical career. Such maternal discrimination, which is a distinct phenomenon from sex discrimination, has been shown to be associated with higher levels of self-reported burnout among female physicians.37 Workplace interventions that increase duration of maternity leave, improve childcare, and provide lactation support may mitigate perceived stigma,37 decrease apprehension associated with requesting accommodations, provide predictability for peers when planning for a pregnant resident’s leave, and increase program appeal when recruiting future trainees.36 Practical and successful solutions for childcare include access to onsite daycare,38 backup child care,39 and financial childcare support.40 Breastfeeding residents should be supported in their need to pump milk during long cases by permitting periods of cross-coverage by fellow residents and by providing appropriate lactation facilities near the operating room.41
Limitations
Limitations of this study include the method of survey distribution, which did not allow calculation of a response rate. However, given that the number of women who have been pregnant during training is unknown, social media platforms were used to disseminate the survey to as many surgeon mothers as possible. Selection bias may have affected the results if those who had greater residency or career dissatisfaction were more likely to participate in these interest groups or to reply to electronic requests for participation from the Association of Women Surgeons and program directors. Despite this, the study cohort exhibits a balance of program sizes and types and wide geographic distribution. Additionally, response and social desirability bias may be a factor in any self-reported data, with a tendency for participants to answer questions in a way that will be viewed favorably. The factors driving subspecialty selection are complex, and it is possible that issues other than pregnancy and parenthood drove career changes. Future studies with parallel data on training and career satisfaction of male residents and female residents without children may provide useful comparison with this cohort. Data about social and financial supports, such as marital status, family assistance, and annual income, which may have influenced career decisions and the level of work-life conflicts, were not collected. Although an effort was made to report the most contemporary experience by including only responses from those who completed or were expected to complete residency 2007 or later, responses are subject to recall bias. Lastly, the cross-sectional design does not allow causal associations to be drawn.
Conclusions
This is a pivotal time for sex equity in the workforce. Surgical training is at a crossroads, with lifestyle issues affecting recruitment and retention. The rising number of women beginning families during residency34 requires surgical leaders and program directors to address the challenges faced by childbearing trainees. This study shows that expectant residents who feel compelled to alter their fellowship plans owing to family priorities, who lack maternity leave policies at their training programs, and who perceive negative stigma around pregnancy are at increased risk of experiencing career dissatisfaction. Surgical training programs must refine mentor-mentee relationships, targeting support in work-life integration and fellowship selection. Interventions at the program and national levels should focus on identifying obstacles to maternity leave policies, designing a collaborative approach to implementation of flexible training tracks, and examining methods to reduce maternal discrimination. This may improve professional fulfillment, reduce attrition, and improve the residency experience for childbearing residents.
References
- 1.AAMC.org Facts: applicants, matriculants, enrollment, graduates, MD-PhD, and residency applicants’ data. https://www.aamc.org/download/321442/data/factstablea1.pdf. Accessed January 22, 2018.
- 2.AAMC.org Facts: residency applicants from US MD-granting schools to ACFME-accredited programs by specialty and sex, 2017-2018. https://www.aamc.org/download/321560/data/factstablec2.pdf. Accessed January 22, 2018.
- 3.Park J, Minor S, Taylor RA, Vikis E, Poenaru D. Why are women deterred from general surgery training? Am J Surg. 2005;190(1):141-146. [DOI] [PubMed] [Google Scholar]
- 4.Cochran A, Melby S, Neumayer LA. An internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg. 2005;189(6):742-746. [DOI] [PubMed] [Google Scholar]
- 5.Wendel TM, Godellas CV, Prinz RA. Are there gender differences in choosing a surgical career? Surgery. 2003;134(4):591-596. [DOI] [PubMed] [Google Scholar]
- 6.Khoushhal Z, Hussain MA, Greco E, et al. Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg. 2017;152(3):265-272. [DOI] [PubMed] [Google Scholar]
- 7.Naylor RA, Reisch JS, Valentine RJ. Factors related to attrition in surgery residency based on application data. Arch Surg. 2008;143(7):647-651. [DOI] [PubMed] [Google Scholar]
- 8.Gifford E, Galante J, Kaji AH, et al. Factors associated with general surgery residents’ desire to leave residency programs: a multi-institutional study. JAMA Surg. 2014;149(9):948-953. [DOI] [PubMed] [Google Scholar]
- 9.Phillips EA, Nimeh T, Braga J, Lerner LB. Does a surgical career affect a woman’s childbearing and fertility? a report on pregnancy and fertility trends among female surgeons. J Am Coll Surg. 2014;219(5):944-950. [DOI] [PubMed] [Google Scholar]
- 10.Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. J Am Coll Surg. 2009;208(2):293-297. [DOI] [PubMed] [Google Scholar]
- 11.Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training: results of a nationwide survey of general surgery residents [published online March 21, 2018]. JAMA Surg. doi: 10.1001/jamasurg.2018.0153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463-471. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Freischlag J, Kaups KL, et al. Work-home conflicts have a substantial impact on career decisions that affect the adequacy of the surgical workforce. Arch Surg. 2012;147(10):933-939. [DOI] [PubMed] [Google Scholar]
- 14.Frank E, McMurray JE, Linzer M, Elon L; Society of General Internal Medicine Career Satisfaction Study Group . Career satisfaction of US women physicians: results from the Women Physicians’ Health Study. Arch Intern Med. 1999;159(13):1417-1426. [DOI] [PubMed] [Google Scholar]
- 15.Levinson W, Tolle SW, Lewis C. Women in academic medicine: combining career and family. N Engl J Med. 1989;321(22):1511-1517. [DOI] [PubMed] [Google Scholar]
- 16.HIS Markit Inc The complexities of physician supply and demand: projections from 2015-2030. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf. Accessed January 2, 2018.
- 17.Dodson TF, Webb AL. Why do residents leave general surgery? the hidden problem in today’s programs. Curr Surg. 2005;62(1):128-131. [DOI] [PubMed] [Google Scholar]
- 18.Longo WE, Seashore J, Duffy A, Udelsman R. Attrition of categoric general surgery residents: results of a 20-year audit. Am J Surg. 2009;197(6):774-778. [DOI] [PubMed] [Google Scholar]
- 19.Yeo H, Viola K, Berg D, et al. Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. JAMA. 2009;302(12):1301-1308. [DOI] [PubMed] [Google Scholar]
- 20.Dageforde LA, Kibbe M, Jackson GP. Recruiting women to vascular surgery and other surgical specialties. J Vasc Surg. 2013;57(1):262-267. [DOI] [PubMed] [Google Scholar]
- 21.Colletti LM, Mulholland MW, Sonnad SS. Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135(8):972-977. [DOI] [PubMed] [Google Scholar]
- 22.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211-217. [DOI] [PubMed] [Google Scholar]
- 23.Burack JH, Irby DM, Carline JD, Ambrozy DM, Ellsbury KE, Stritter FT. A study of medical students’ specialty-choice pathways: trying on possible selves. Acad Med. 1997;72(6):534-541. [DOI] [PubMed] [Google Scholar]
- 24.Gordinier ME, Ramondetta LM, Parker LP, et al. Survey of female gynecologic oncologists and fellows: balancing professional and personal life. Gynecol Oncol. 2000;79(2):309-314. [DOI] [PubMed] [Google Scholar]
- 25.Freischlag JA, Silva MM. Preventing general surgery residency attrition: it is all about the mentoring. JAMA Surg. 2017;152(3):272-273. [DOI] [PubMed] [Google Scholar]
- 26.Elmore LC, Jeffe DB, Jin L, Awad MM, Turnbull IR. National survey of burnout among US general surgery residents. J Am Coll Surg. 2016;223(3):440-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCord JH, McDonald R, Sippel RS, Leverson G, Mahvi DM, Weber SM. Surgical career choices: the vital impact of mentoring. J Surg Res. 2009;155(1):136-141. [DOI] [PubMed] [Google Scholar]
- 28.McCord JH, McDonald R, Leverson G, et al. Motivation to pursue surgical subspecialty training: is there a gender difference? J Am Coll Surg. 2007;205(5):698-703. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan MC, Bucholz EM, Yeo H, Roman SA, Bell RH, Sosa JA. “Join the club”: effect of resident and attending social interactions on overall satisfaction among 4390 general surgery residents. Arch Surg. 2012;147(5):408-414. [DOI] [PubMed] [Google Scholar]
- 30.Garza RM, Weston JS, Furnas HJ. Pregnancy and the plastic surgery resident. Plast Reconstr Surg. 2017;139(1):245-252. [DOI] [PubMed] [Google Scholar]
- 31.The American Board of Surgery Leave Policy http://www.absurgery.org/default.jsp?policygsleave. Accessed October 21, 2017.
- 32.Abbett SK, Hevelone ND, Breen EM, et al. Interest in and perceived barriers to flexible-track residencies in general surgery: a national survey of residents and program directors. J Surg Educ. 2011;68(5):365-371. [DOI] [PubMed] [Google Scholar]
- 33.Humphries LS, Lyon S, Garza R, Butz DR, Lemelman B, Park JE. Parental leave policies in graduate medical education: a systematic review. Am J Surg. 2017;214(4):634-639. [DOI] [PubMed] [Google Scholar]
- 34.Turner PL, Lumpkins K, Gabre J, Lin MJ, Liu X, Terrin M. Pregnancy among women surgeons: trends over time. Arch Surg. 2012;147(5):474-479. [DOI] [PubMed] [Google Scholar]
- 35.Sandler BJ, Tackett JJ, Longo WE, Yoo PS. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program directors. J Am Coll Surg. 2016;222(6):1090-1096. [DOI] [PubMed] [Google Scholar]
- 36.Santen SA, Davis KR, Brady DW, Hemphill RR. Potentially discriminatory questions during residency interviews: frequency and effects on residents’ ranking of programs in the national resident matching program. J Grad Med Educ. 2010;2(3):336-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adesoye T, Mangurian C, Choo EK, Girgis C, Sabry-Elnaggar H, Linos E; Physician Moms Group Study Group . Perceived discrimination experience by physician mothers and desired workplace changes: a cross-sectional survey. JAMA Intern Med. 2017;177(7):1033-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McGuire LK, Bergen MR, Polan ML. Career advancement for women faculty in a U.S. school of medicine: perceived needs. Acad Med. 2004;79(4):319-325. [DOI] [PubMed] [Google Scholar]
- 39.Herman RE, Koppa D, Sullivan P. Sick-child daycare promotes healing and staffing. Nurs Manage. 1999;30(4):46-47. [PubMed] [Google Scholar]
- 40.Key LL., Jr Child care supplementation: aid for residents and advantages for residency programs. J Pediatr. 2008;153(4):449-450. [DOI] [PubMed] [Google Scholar]
- 41.Merchant SJ, Hameed SM, Melck AL. Pregnancy among residents enrolled in general surgery: a nationwide survey of attitudes and experiences. Am J Surg. 2013;206(4):605-610. [DOI] [PubMed] [Google Scholar]