Key Points
Question
Are intraoperative findings associated with the risk of postoperative complications and use of health care resources in children with complicated appendicitis?
Findings
In this multicenter cohort study of 1333 children undergoing appendectomy, intraoperative findings were found to markedly influence postoperative outcomes. Compared with patients with 1 intraoperative finding, multiple findings were associated with higher rates of complications (16.4% vs 10.6%), more revisits (22.9% vs 8.9%), longer length of stay (8.9 vs 4.0 days), and higher hospital cost ($32 282 vs $13 296).
Meaning
Adjustment for disease severity may be necessary to ensure fair reimbursement and comparative performance reporting among hospitals, particularly at hospitals treating underserved populations, where more severe presentation is common.
Abstract
Importance
The influence of disease severity on outcomes and use of health care resources in children with complicated appendicitis is poorly characterized. Adjustment for variation in disease severity may have implications for ensuring fair reimbursement and comparative performance reporting among hospitals.
Objective
To examine the association of intraoperative findings as a measure of disease severity with complication rates and resource use in children with complicated appendicitis.
Design
This retrospective cohort study used clinical data from the American College of Surgeons National Surgical Quality Improvement Program pediatric appendectomy pilot database (NSQIP-P database) and cost data from the Pediatric Health Information System database. Twenty-two children’s hospitals participated in the NSQIP Pediatric Appendectomy Collaborative Pilot Project. Patients aged 3 to 18 years with complicated appendicitis who underwent an appendectomy from January 1, 2013, through December 31, 2014, were included in the study. Appendicitis was categorized in the NSQIP-P database as complicated if any of the following 4 intraoperative findings occurred in the operative report: visible hole, fibropurulent exudate in more than 2 quadrants, abscess, or extraluminal fecalith. Data were analyzed from January 1, 2013, through December 31, 2014.
Main Outcomes and Measures
Thirty-day postoperative adverse event rate, revisit rate, hospital cost, and length of stay. Multivariable regression was used to estimate event rates and outcomes for all observed combinations of intraoperative findings, with adjusting for patient characteristics and clustering within hospitals.
Results
A total of 1333 patients (58.7% boys; median age, 10 years; interquartile range, 7-12 years) were included; multiple intraoperative findings of complicated appendicitis were reported in 589 (44.2%). Compared with single findings, the presence of multiple findings was associated with higher rates of surgical site infection (odds ratio, 1.40; 95% CI, 0.95-2.06; P = .09), higher revisit rates (odds ratio, 1.60; 95% CI, 1.15-2.21; P = .005), longer length of stay (rate ratio, 1.45; 95% CI, 1.36-1.55; P < .001), and higher hospital cost (rate ratio, 1.35; 95% CI, 1.19-1.53; P < .001). Significant differences were found among different combinations of intraoperative findings for all outcomes, including a 3.6-fold difference in rates of surgical site infection (range, 7.5% for fecalith alone to 27.2% for all 4 findings; P = .002), a 2.6-fold difference in revisit rates (range, 8.9% for exudate alone to 22.9% for all 4 findings; P = .001), a 2.2-fold difference in length of stay (range, 4.0 days for exudate alone to 8.9 days for all 4 findings; P < .001), and a 2.4-fold difference in mean cumulative cost (range, $13 296 for exudate alone to $32 282 for all 4 findings; P < .001).
Conclusions and Relevance
More severe presentations of complicated appendicitis are associated with worse outcomes and greater resource use. Severity adjustment may be needed to ensure fair reimbursement and comparative performance reporting, particularly at hospitals treating underserved populations where more severe presentations are common.
This multicenter cohort study examines the influence of intraoperative findings as a measure of disease severity on complication rates and use of health care resources in children with complicated appendicitis.
Introduction
Appendicitis is the most common abdominal surgical emergency in the pediatric population.1 Complicated appendicitis accounts for approximately 30% of cases and is associated with increased hospital cost, length of stay (LOS), and adverse outcomes.2,3,4,5,6,7,8 Although complicated appendicitis presents along a wide spectrum of disease severity in children, little is known of how different presentations affect use of health care resources and the risk of adverse outcomes. A more thorough understanding of this association may have important implications for reimbursement policy and ensuring fair comparative performance reporting among hospitals. These implications may be particularly relevant for hospitals treating underserved or rural populations, where delayed presentation is common.9,10,11
With the above considerations, the goal of this study was to examine the association of different combinations of intraoperative findings with resource use and rates of adverse events in children with complicated appendicitis. For this study, we used the American College of Surgeons National Surgical Quality Improvement Program pediatric appendectomy pilot database (hereinafter referred to as the NSQIP-P database) to leverage its multicenter platform and rigorous data collection methods. Outcomes included rates of postoperative complications, surgical site infections (SSIs), revisits, LOS, and cumulative cost from all index and revisit encounters. These outcomes were chosen to provide a comprehensive set of measures relevant to all stakeholders, including patients and their parents, hospitals, and payors.
Methods
Study Design
This retrospective cohort study used clinical data from the NSQIP-P database merged with cost data from the Pediatric Health Information System (PHIS) database. The NSQIP-P database includes a wide array of clinical and laboratory data for calculating and comparing risk-adjusted adverse event rates among 82 member hospitals.12,13 Data are procured at each hospital by dedicated, full-time medical record abstractors using standardized criteria and a rigorous medical record review process. Accuracy of data collection is facilitated through periodic auditing of participating hospitals, mandatory training for medical record abstractors, and the availability of an American College of Surgeons clinical support team to address questions surrounding data definitions and data collection protocol. This study was approved by the institutional review board of Boston Children’s Hospital, Boston, Massachusetts, which did not require informed consent.
The NSQIP Pediatric Appendectomy Collaborative Pilot Project was initiated in 2013 and includes 29 NSQIP pediatric hospitals with the goal of collecting an extended set of disease-specific variables in patients with suspected appendicitis. These variables include use of imaging, intraoperative findings, pathology findings, points of care, hospital revisits, and unique encrypted identifiers, among others, for each participating hospital. A manual of operations to ensure consistency and accuracy of data collection was distributed to all participating hospitals and reviewed via webinar before the initiation of data collection. All NSQIP data used for this analysis were obtained directly from hospitals participating in the collaborative. The American College of Surgeons was not involved in the procurement or analysis of study data.
The PHIS database contains administrative billing data from 47 children’s hospitals affiliated with the Children’s Hospital Association, Lenexa, Kansas. Patient-level data in PHIS include demographic and payor information, diagnostic codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), and International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), Current Procedural Terminology codes, and granular billing data for a wide range of clinical and hospital services. Data quality is ensured by coding consensus meetings and hospital-specific quality audits summarized in quarterly reports.
Study Cohort and Exposure Classification
The study cohort included all children aged 3 to 18 years who underwent an appendectomy for suspected appendicitis identified from the NSQIP database from January 1, 2013, through December 31, 2014. Patients were excluded if they carried a diagnosis of immunodeficiency or were missing data for intraoperative findings. Intraoperative findings considered representative of complicated appendicitis in NSQIP-P database were defined through consensus by the NSQIP Pediatric Data Definitions Committee. These definitions included any of the following 4 findings in the operative report: visible hole, diffuse fibropurulent exudate (defined as exudate in >2 quadrants of the abdomen and pelvis), intra-abdominal abscess, or an extraluminal fecalith. These findings were used for the present analysis based on data demonstrating each to be independently associated with increased complication rates, LOS, and hospital cost when present at the time of operation.8
Outcomes
Thirty-day rates of postoperative adverse events included any morbidity as defined by NSQIP-P database, overall rate of SSI as an independent outcome (organ space SSIs and incisional SSIs together), and 30-day revisit rates (emergency department or inpatient readmission). For this analysis, superficial and deep incisional SSIs were combined into a single group. Resource use outcomes included cumulative LOS and hospital cost from all index and revisit encounters occurring during the 30-day postoperative period.
Cost data were obtained from 13 of the 14 NSQIP pediatric hospitals that also participated in the PHIS database during the same study period. Children undergoing appendectomy for suspected appendicitis were identified from the PHIS database using ICD-9-CM procedure codes 47.01 and 47.09 and diagnostic codes 590.0, 590.1, and 590.9. To account for differences in unit-based cost between hospitals for individually billed items (eg, differences in the reported cost of a complete blood cell count, intravenous tubing, laparoscopic trocar, nursing shift, etc), cost data obtained for this study were standardized by applying the previously reported cost master index.14 In brief, the median cost of an item across all hospitals was used as the standardized unit cost for that item. For each patient, the standardized unit cost for each item was multiplied by the number of units billed to arrive at the standardized hospital cost for the encounter. The intent of the cost master index is to allow for a more accurate comparison of actual resource use among hospitals by adjusting for differences in reported cost for individually billed items. Standardized cost data from the PHIS were merged with clinical data from NSQIP-P using a previously validated probabilistic matching algorithm based on age at operation in days, sex, and unique hospital identifier.15
Statistical Analysis
Data were analyzed from January 1, 2013, through December 31, 2014. Multivariable, mixed-effects regression was used to measure the influence of single vs multiple findings on each outcome after adjusting for patient characteristics (age, sex, obesity, race/ethnicity, and insurance) and hospital-level random effects. A logistic link was used for the binary outcomes of adverse events and revisits, and a gamma link was used for the continuous outcomes of LOS and cost due to their skewed distributions. Measures of association were reported in terms of odds ratios (ORs) and rate ratios (RRs), accordingly. The effect of combinations of intraoperative findings on outcomes was investigated by evaluating all possible interaction terms in the mixed-effects models and retaining statistically significant terms. The final models were used to estimate hospital-level adjusted probability of adverse events, SSIs, revisits, mean LOS, and cost for each of the possible combinations of intraoperative findings (visible hole, exudate, abscess, and extraluminal fecalith). Analyses were performed with SAS statistical software (version 9.4; SAS Institute, Inc). Statistical significance was achieved with a 2-sided P < .05.
Results
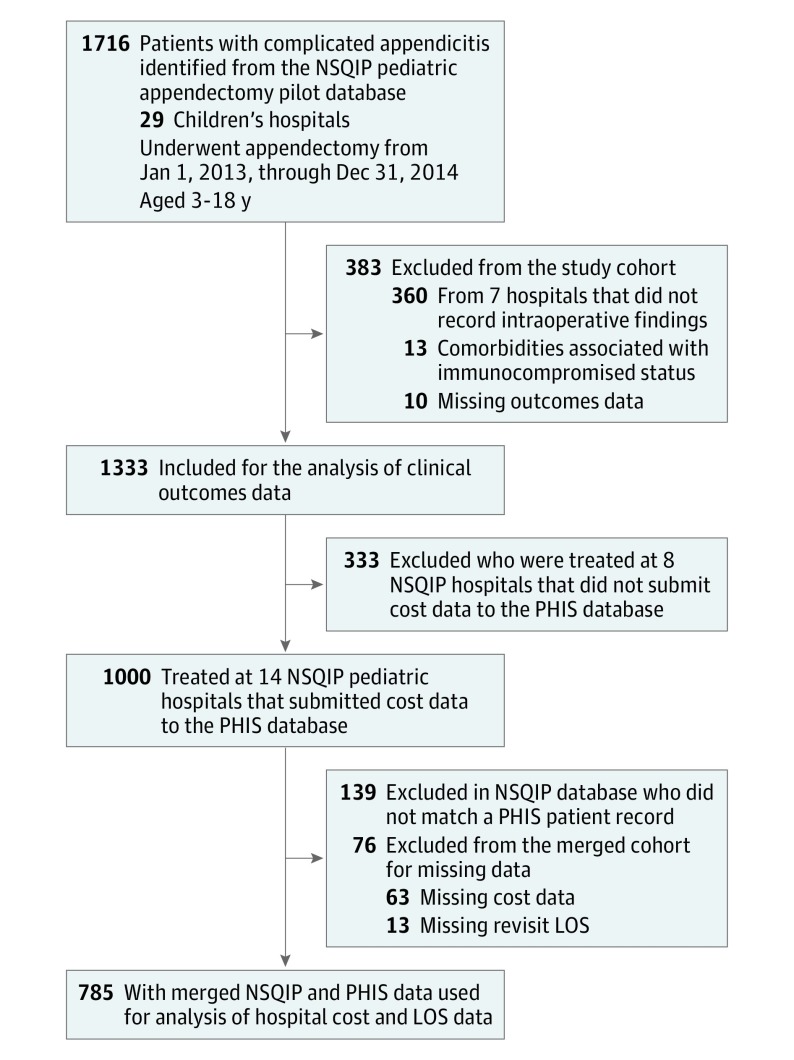
The final study cohort included 1333 patients from 22 NSQIP pediatric hospitals (Figure 1). Of these, 783 patients (58.7%) were male, 550 (41.3%) were female, 538 (40.4%) were white, 496 (37.2%) were publicly insured, and the median age was 10 years (interquartile range, 7-12 years). Multiple intraoperative findings of complicated appendicitis were reported in 589 cases (44.2%) cases, and the most frequently reported combinations of intraoperative findings included a visible hole with diffuse fibrinopurulent exudate (231 [39.2%]), visible hole with exudate and abscess (86 [14.6%]), and visible hole with abscess (80 [13.6%]). Of the 1333 patients identified from the NSQIP-P database, 1000 (75.0%) were treated at 14 hospitals that also participated in the PHIS database. Of these, 861 patients (86.1%) were successfully matched with patients in the NSQIP database. Seventy-six patients (8.8%) were excluded from the merged cohort for missing data, which resulted in a final merged cohort of 785 patients to provide hospital cost and LOS data.
Figure 1. Flow Diagram of the Study Cohort.
LOS indicates length of stay; NSQIP, National Surgical Quality Improvement Program; PHIS, Pediatric Health Information System.
Adverse Events
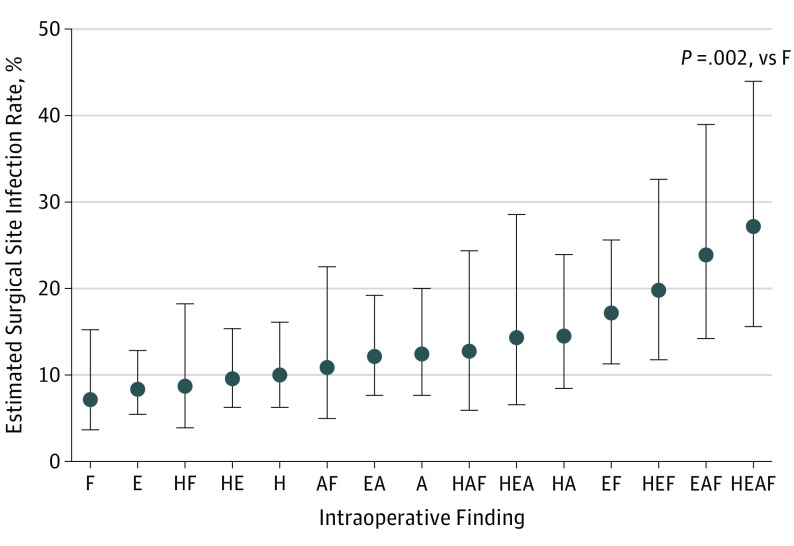
Overall, a total of 209 adverse events occurred in 181 patients (13.6%). The most common events were organ space SSIs (133 patients [73.5%]), incisional SSIs (17 [9.4%]), other occurrences (14 [7.7%]), pneumonia (8 [4.4%]), and sepsis (8 [4.4%]). Multiple intraoperative findings of complicated appendicitis were associated with higher rates of overall adverse events (OR, 1.66; 95% CI, 1.17-2.36; P = .005) and insignificantly higher SSI rates (OR, 1.40; 95% CI, 0.95-2.06; P = .09) compared with single findings. Different combinations of intraoperative findings were associated with significantly different rates of adverse outcomes, including a 4.2-fold variation in overall adverse event rates (range, 9.6% for exudate alone to 40.2% for all 4 findings; P < .001), a 3.6-fold difference in overall SSI rates (range, 7.5% for fecalith alone to 27.2% for all 4 findings; P = .002) (Figure 2), and a 3.7-fold difference in rates of organ space infection (range, 6.7% for fecalith alone to 24.8% for all 4 findings; P = .004). Incisional SSIs ranged from 0.3% for combined hole, abscess, and fecalith to 6.5% for combined exudate and fecalith, although this difference did not reach statistical significance (P = .32).
Figure 2. Association of Different Combinations of Intraoperative Findings With Estimated Overall SSI Rates in Children With Complicated Appendicitis.
Error bars indicate 95% CI. A indicates intra-abdominal abscess; E, diffuse fibropurulent exudate; F, extraluminal fecalith; H, visible hole; and SSI, surgical site infection.
Hospital Revisits
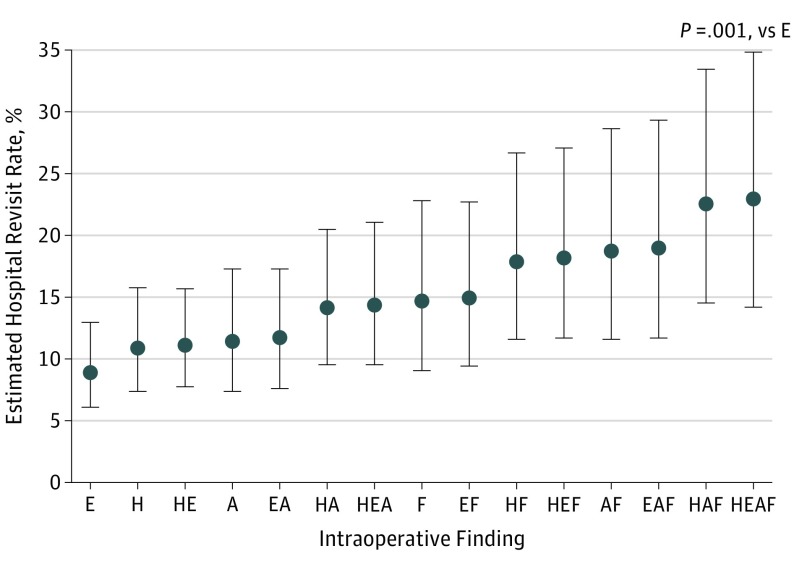
Multiple intraoperative findings of complicated appendicitis were associated with higher rates of any type of hospital revisits (OR, 1.60; 95% CI, 1.15-2.21; P = .005), higher rates of inpatient readmissions (OR, 2.04; 95% CI, 1.30-3.22; P = .002), and higher rates of ED revisits without inpatient readmission (OR, 1.52; 95% CI, 1.08-2.13; P = .02) compared with single findings. Different combinations of intraoperative findings were associated with a 2.6-fold difference in overall revisit rates (range, 8.9% for exudate alone to 22.9% for all 4 findings; P = .001) (Figure 3).
Figure 3. Association of Different Combinations of Intraoperative Findings With Estimated Revisit Rates in Children With Complicated Appendicitis.
Error bars indicate 95% CI. A indicates intra-abdominal abscess; E, diffuse fibropurulent exudate; F, extraluminal fecalith; and H, visible hole.
Resource Use
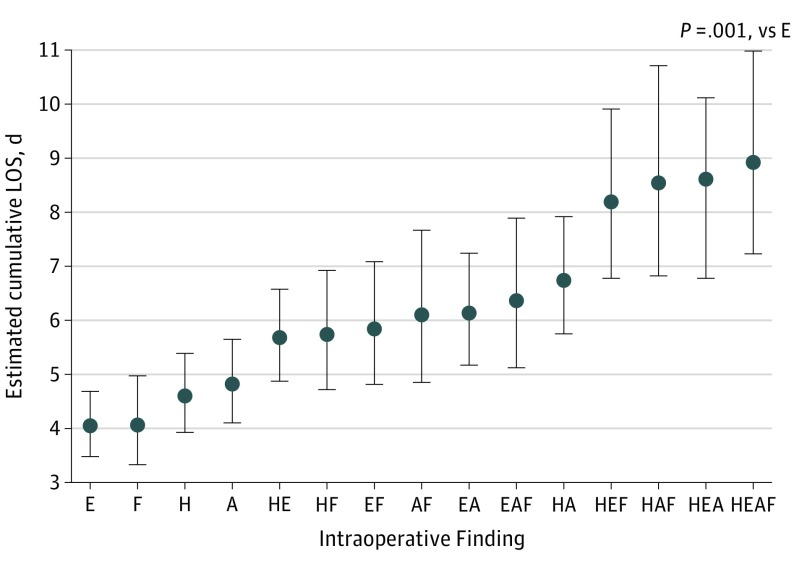
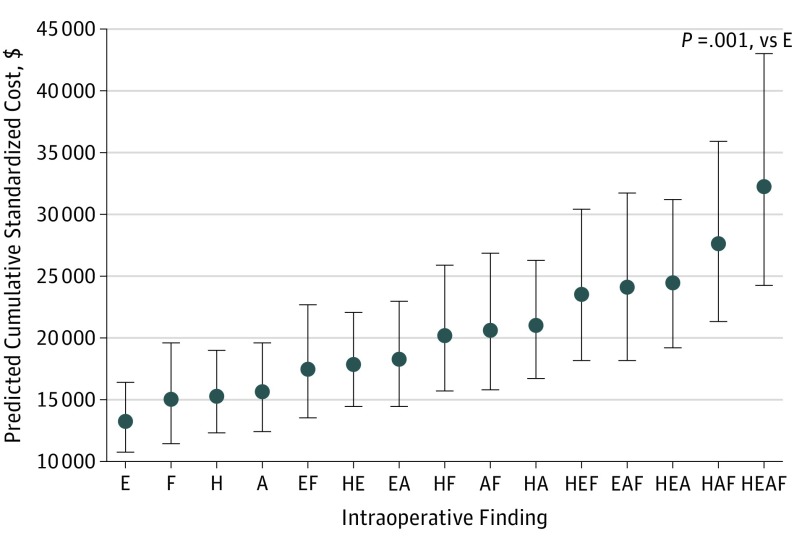
Multiple intraoperative findings of complicated appendicitis were associated with a higher cumulative LOS (RR, 1.45; 95% CI, 1.36-1.55; P < .001) and a higher cumulative cost (RR, 1.35; 95% CI, 1.19-1.53; P < .001) compared with single findings. Different combinations of intraoperative findings were associated with significantly different profiles of resource use, including a 2.2-fold difference in mean LOS (range, 4.0 days for exudate alone to 8.9 days for all 4 findings; P < .001) (Figure 4) and a 2.4-fold difference in mean cumulative cost (range, $13 296 for exudate alone to $32 282 for all 4 findings; P < .001) (Figure 5).
Figure 4. Association of Different Combinations of Intraoperative Findings With Estimated Cumulative LOS in Children With Complicated Appendicitis.
Error bars indicate 95% CI. A indicates intra-abdominal abscess; E, diffuse fibropurulent exudate; F, extraluminal fecalith; H, visible hole; and LOS, length of stay.
Figure 5. Association of Different Combinations of Intraoperative Findings With Estimated Cumulative Standardized Cost in Children With Complicated Appendicitis.
Error bars indicate 95% CI. A indicates intra-abdominal abscess; E, diffuse fibropurulent exudate; F, extraluminal fecalith; H, visible hole; and LOS, length of stay.
Discussion
In this multicenter analysis of 1333 patients from 22 children’s hospitals, different combinations of intraoperative findings were found to markedly influence the risk of adverse outcomes and resource use in children with complicated appendicitis. Children presenting with multiple findings of complicated disease had a nearly 50% higher complication rate and 30% higher cumulative cost compared with children with isolated findings. An even greater magnitude of variation in outcomes was observed across the spectrum of intraoperative findings, including a nearly 4-fold variation in complication rates and a 2-fold variation in hospital cost.
The results of this study add to the growing body of evidence that not all cases of complicated appendicitis are created equally with respect to clinical course and resource use. In a single-center study of 918 patients,16 perforated disease with diffuse peritonitis was associated with higher rates of SSIs (41.9% vs 32.0%) and intra-abdominal abscesses (35.7% vs 12.2%) and a longer median LOS (9 days vs 4 days) compared with perforated disease with localized free fluid. In a single-center study of 88 children with complicated appendicitis,17 extensive peritoneal contamination (defined as fibropurulent exudate extending to the liver) was associated with a 2.5-fold higher odds of a postoperative drainage procedure, 50% longer median LOS, and a 30% higher cumulative median hospital cost compared with localized contamination confined to the right lower quadrant or pelvis. Another single-center study of 122 patients with perforated appendicitis18 graded disease severity on a scale of 1 to 4 based on the extent of peritonitis and number of intra-abdominal abscesses found at operation. Higher rates of postoperative abscesses, longer length of stay, and longer duration of antibiotics were all associated with higher grades of disease severity. Although these data support the premise that disease severity can influence outcomes in complicated appendicitis, the generalizability of these studies may be limited by their single-center analyses and the use of relatively subjective criteria for defining complicated disease. To our knowledge, the present study is the first to characterize the association between disease severity and outcomes in a multicenter format using standardized definitions for exposures and outcomes.
The increased risk of complications with multiple intraoperative findings may be explained by different mechanisms of treatment failure associated with different findings. Diffuse fibropurulent exudate may represent more extensive peritoneal surface contamination (ie, a greater burden of residual biofilm after an appendectomy), whereas the presence of an intra-abdominal abscess may represent longer disease chronicity and a more established biofilm.19,20 The presence of an extraluminal fecalith may be a marker of gross and microscopic fecal contamination, and this finding has been associated with particularly high rates of postoperative abscesses and failure of nonoperative management.21,22,23 Given that each finding may be associated with a different mechanism for treatment failure, different combinations of findings may be cumulative in their risk for postoperative complications and increased resource use. Increasing severity was notable with each intraoperative finding and with the addition of each additional finding; however, the study was not powered to reach significance among each combination and to establish a gradient of severity.
The findings of this study may have important implications for ensuring fair and equitable reimbursement across hospitals, particularly for those that treat rural or socioeconomically disadvantaged populations. Higher rates of complicated appendicitis have been reported in these populations,9,10,11 and these children may also have more severe (and resource-intensive) presentations of complicated appendicitis. Diagnosis related group–based reimbursement is currently used by many public insurers (Centers for Medicaid & Medicare Services) and an increasing number of private insurers to set case-based hospital reimbursement fees for surgical procedures. In the management of acute appendicitis, diagnosis related group–based reimbursement for appendectomy currently recognizes 2 levels of disease severity based on ICD codes (complicated and uncomplicated) and is intended to differentiate perforated from nonperforated appendicitis.24 Based on the results of this study, diagnosis related group–based stratification (eg, ICD classification) of disease severity would appear inadequate for children with complicated appendicitis. Hospitals that treat populations at high risk for delayed presentation may therefore be at risk for underpayment. Modification of future ICD-based classification to include specific operative findings within the category of complicated appendicitis may more effectively match reimbursement with the resources required to treat individual patients. This modification may be particularly important with the increasing trend toward global payment reimbursement models.
More granular adjustment for disease severity may also improve the accuracy and utility of performance benchmarking data for appendicitis such as that provided by the NSQIP-P database. The NSQIP Pediatric Appendectomy Procedure Targeted Semi-Annual report currently provides a broad array of comparative performance data to more than 100 hospitals, including rates of SSIs, deep organ space infections, percutaneous drainage procedures, postoperative imaging, and hospital revisits, among other measures.25 Similar to current reimbursement policy, the NSQIP-P database stratifies its hospital-level performance reporting along 2 levels of severity, which may bias results against hospitals that treat the highest-risk populations. More granular adjustment for disease severity may result in a more accurate estimate of hospital performance and provide hospitals with more meaningful comparative data to prioritize their quality improvement efforts. Finally, the results of this study may have implications for study design and methods used to report clinical research focusing on complicated appendicitis. These implications may be particularly relevant for comparative effectiveness studies, where the matching and reporting of treatment groups on intraoperative findings (ie, disease severity) could improve the validity of study results.
Limitations
Several limitations of this study should be acknowledged. Although the NSQIP-P and PHIS databases are subject to extensive and rigorous quality assurance audits, medical record extraction and coding errors are possible. Data collected in the PHIS and NSQIP-P databases are obtained from large academic teaching hospitals and may not be generalizable to community hospitals and other health care settings. The definition of complicated appendicitis used in this analysis was based on 4 intraoperative criteria, and findings other than those examined in this study may also be associated with poor outcomes and increased resource use. These criteria were chosen specifically based on previous data demonstrating each to be independently associated with postoperative complications and increased resource use,8 therefore providing the most rigorous evidence-based definition of complicated disease available.
Conclusions
Despite these limitations, the results of this study strongly support the notion that not all cases of complicated appendicitis are created equally with respect to clinical course and resource use. Further efforts are needed to explore and characterize the degree of overpayment and underpayment across hospitals associated with the current 2-tiered reimbursement system. The imperative for this will become increasingly relevant with the expansion of accountable care organizations, where standardized bundled payments for surgical procedures are earmarked to cover professional fees and cost of the hospitalization.26,27
References
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910-925. doi: 10.1093/oxfordjournals.aje.a115734 [DOI] [PubMed] [Google Scholar]
- 2.Kelly KN, Fleming FJ, Aquina CT, et al. Disease severity, not operative approach, drives organ space infection after pediatric appendectomy. Ann Surg. 2014;260(3):466-471. doi: 10.1097/SLA.0000000000000874 [DOI] [PubMed] [Google Scholar]
- 3.Schlottmann F, Sadava EE, Peña ME, Rotholtz NA. Laparoscopic appendectomy: risk factors for postoperative intraabdominal abscess. World J Surg. 2017;41(5):1254-1258. doi: 10.1007/s00268-017-3869-y [DOI] [PubMed] [Google Scholar]
- 4.Farach SM, Danielson PD, Walford NE, Harmel RP Jr, Chandler NM. Operative findings are a better predictor of resource utilization in pediatric appendicitis. J Pediatr Surg. 2015;50(9):1574-1578. doi: 10.1016/j.jpedsurg.2015.02.064 [DOI] [PubMed] [Google Scholar]
- 5.Cameron DB, Graham DA, Milliren CE, et al. Quantifying the burden of interhospital cost variation in pediatric surgery: implications for the prioritization of comparative effectiveness research. JAMA Pediatr. 2017;171(2):e163926. doi: 10.1001/jamapediatrics.2016.3926 [DOI] [PubMed] [Google Scholar]
- 6.Rice-Townsend S, Barnes JN, Hall M, Baxter JL, Rangel SJ. Variation in practice and resource utilization associated with the diagnosis and management of appendicitis at freestanding children’s hospitals: implications for value-based comparative analysis. Ann Surg. 2014;259(6):1228-1234. doi: 10.1097/SLA.0000000000000246 [DOI] [PubMed] [Google Scholar]
- 7.Rice-Townsend S, Hall M, Barnes JN, Baxter JK, Rangel SJ. Hospital readmission after management of appendicitis at freestanding children’s hospitals: contemporary trends and financial implications. J Pediatr Surg. 2012;47(6):1170-1176. doi: 10.1016/j.jpedsurg.2012.03.025 [DOI] [PubMed] [Google Scholar]
- 8.Cameron DB, Melvin P, Graham DA, et al. Influence of intraoperative findings on outcomes and resource utilization in children with appendicitis: indications for an evidence-based and public health relevant definition for complicated disease. Paper presented at: 98th Annual Meeting of the New England Surgical Society; September 9, 2017; Brent Woods, NH. [Google Scholar]
- 9.O’Toole SJ, Karamanoukian HL, Allen JE, et al. Insurance-related differences in the presentation of pediatric appendicitis. J Pediatr Surg. 1996;31(8):1032-1034. doi: 10.1016/S0022-3468(96)90079-2 [DOI] [PubMed] [Google Scholar]
- 10.O’Toole SJ, Karamanoukian HL, Glick PL. Insurance and the risk of ruptured appendix. N Engl J Med. 1995;332(6):396. [PubMed] [Google Scholar]
- 11.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331(7):444-449. doi: 10.1056/NEJM199408183310706 [DOI] [PubMed] [Google Scholar]
- 12.Bruny JL, Hall BL, Barnhart DC, et al. American College of Surgeons National Surgical Quality Improvement Program Pediatric: a beta phase report. J Pediatr Surg. 2013;48(1):74-80. doi: 10.1016/j.jpedsurg.2012.10.019 [DOI] [PubMed] [Google Scholar]
- 13.Rowell KS, Turrentine FE, Hutter MM, Khuri SF, Henderson WG. Use of National Surgical Quality Improvement Program data as a catalyst for quality improvement. J Am Coll Surg. 2007;204(6):1293-1300. doi: 10.1016/j.jamcollsurg.2007.03.024 [DOI] [PubMed] [Google Scholar]
- 14.Keren R, Luan X, Localio R, et al. ; Pediatric Research in Inpatient Settings (PRIS) Network . Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155-1164. doi: 10.1001/archpediatrics.2012.1266 [DOI] [PubMed] [Google Scholar]
- 15.Cameron DB, Melvin P, Graham DA, et al. Extended versus narrow-spectrum antibiotics in the management of uncomplicated appendicitis in children: a propensity-matched comparative effectiveness study [published online June 26, 2017]. Ann Surg.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28654543&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 16.Garst GC, Moore EE, Banerjee MN, et al. Acute appendicitis: a disease severity score for the acute care surgeon. J Trauma Acute Care Surg. 2013;74(1):32-36. doi: 10.1097/TA.0b013e318278934a [DOI] [PubMed] [Google Scholar]
- 17.Feng C, Anandalwar S, Sidhwa F, et al. Beyond perforation: influence of peritoneal contamination on clinical severity and resource utilization in children with perforated appendicitis. J Pediatr Surg. 2016;51(11):1896-1899. doi: 10.1016/j.jpedsurg.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 18.Yousef Y, Youssef F, Dinh T, et al. Risk stratification in pediatric perforated appendicitis: prospective correlation with outcomes and resource utilization. J Pediatr Surg. 2018;53(2):250-255. doi: 10.1016/j.jpedsurg.2017.11.023 [DOI] [PubMed] [Google Scholar]
- 19.Reijnen MM, Bleichrodt RP, van Goor H. Pathophysiology of intra-abdominal adhesion and abscess formation, and the effect of hyaluronan. Br J Surg. 2003;90(5):533-541. doi: 10.1002/bjs.4141 [DOI] [PubMed] [Google Scholar]
- 20.Marshall JC. Intra-abdominal infections. Microbes Infect. 2004;6(11):1015-1025. doi: 10.1016/j.micinf.2004.05.017 [DOI] [PubMed] [Google Scholar]
- 21.Shindoh J, Niwa H, Kawai K, et al. Predictive factors for negative outcomes in initial non-operative management of suspected appendicitis. J Gastrointest Surg. 2010;14(2):309-314. doi: 10.1007/s11605-009-1094-1 [DOI] [PubMed] [Google Scholar]
- 22.Henry MC, Walker A, Silverman BL, et al. Risk factors for the development of abdominal abscess following operation for perforated appendicitis in children: a multicenter case-control study. Arch Surg. 2007;142(3):236-241. doi: 10.1001/archsurg.142.3.236 [DOI] [PubMed] [Google Scholar]
- 23.Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM. Failure in the nonoperative management of pediatric ruptured appendicitis: predictors and consequences. J Pediatr Surg. 2007;42(6):934-938. doi: 10.1016/j.jpedsurg.2007.01.024 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare & Medicaid Services. Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual. https://www.cms.gov/icd10manual/fullcode_cms/P0153.html. Accessed January 18, 2018.
- 25.Ranagel SJ. NSQIP-P Appendectomy Pilot Project: final data report and next steps. http://www.acsnsqip.org/nsqippublicdocs/service?pubid1/42014confpres&docid1/449178. July 26, 2-14. Accessed January 20, 2018.
- 26.Iorio R. Strategies and tactics for successful implementation of bundled payments: bundled payment for care improvement at a large, urban, academic medical center. J Arthroplasty. 2015;30(3):349-350. doi: 10.1016/j.arth.2014.12.031 [DOI] [PubMed] [Google Scholar]
- 27.Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information. https://innovation.cms.gov/initiatives/bundled-payments/index.html. Updated May 7, 2018. Accessed January 17, 2018.