Key Points
Question
Are there racial/ethnic differences in the use of oral anticoagulants, particularly direct-acting oral anticoagulants, in patients with atrial fibrillation?
Findings
In this multicenter US-based registry study of a cohort of 12 147 outpatients with atrial fibrillation, black patients were significantly less likely to receive direct-acting oral anticoagulants than white patients, even after controlling for clinical and sociodemographic features; no difference between white patients and Hispanic patients was observed.
Meaning
Reducing disparities in stroke prevention for patients with atrial fibrillation may improve overall quality of care and result in reduced complication rates.
This cohort study uses data from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II to assess racial/ethnic differences in the use of oral anticoagulants by patients with atrial fibrillation.
Abstract
Importance
Black and Hispanic patients are less likely than white patients to use oral anticoagulants for atrial fibrillation. Little is known about racial/ethnic differences in use of direct-acting oral anticoagulants (DOACs) for atrial fibrillation.
Objective
To assess racial/ethnic differences in the use of oral anticoagulants, particularly DOACs, in patients with atrial fibrillation.
Design, Setting, and Participants
This cohort study used data from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II, a prospective, US-based registry of outpatients with nontransient atrial fibrillation 21 years and older who were followed up from February 2013 to July 2016. Data were analyzed from February 2017 to February 2018.
Exposures
Self-reported race/ethnicity as white, black, or Hispanic.
Main Outcomes and Measures
The primary outcome was use of any oral anticoagulant, particularly DOACs. Secondary outcomes included the quality of anticoagulation received and oral anticoagulant discontinuation at 1 year.
Results
Of 12 417 patients, 11 100 were white individuals (88.6%), 646 were black individuals (5.2%), and 671 were Hispanic individuals (5.4%) with atrial fibrillation. After adjusting for clinical features, black individuals were less likely to receive any oral anticoagulant than white individuals (adjusted odds ratio [aOR], 0.75 [95% CI, 0.56, 0.99]) and less likely to receive DOACs if an anticoagulant was prescribed (aOR, 0.63 [95% CI, 0.49-0.83]). After further controlling for socioeconomic factors, oral anticoagulant use was no longer significantly different in black individuals (aOR, 0.78 [95% CI, 0.59-1.04]); among patients using oral anticoagulants, DOAC use remained significantly lower in black individuals (aOR, 0.73 [95% CI, 0.55-0.95]). There was no significant difference between white and Hispanic groups in use of oral anticoagulants. Among patients receiving warfarin, the median time in therapeutic range was lower in black individuals (57.1% [IQR, 39.9%-72.5%]) and Hispanic individuals (51.7% [interquartile range {IQR}, 39.1%-66.7%]) than white individuals (67.1% [IQR, 51.8%-80.6%]; P < .001). Black and Hispanic individuals treated with DOACs were more likely to receive inappropriate dosing than white individuals (black patients, 61 of 394 [15.5%]; Hispanic patients, 74 of 409 [18.1%]; white patients, 1003 of 7988 [12.6%]; P = .01). One-year persistence on oral anticoagulants was the same across groups.
Conclusions and Relevance
After controlling for clinical and socioeconomic factors, black individuals were less likely than white individuals to receive DOACs for atrial fibrillation, with no difference between white and Hispanic groups. When atrial fibrillation was treated, the quality of anticoagulant use was lower in black and Hispanic individuals. Identifying modifiable causes of these disparities could improve the quality of care in atrial fibrillation.
Introduction
Atrial fibrillation (AF) is the most common heart rhythm disorder in the United States and a significant risk factor for ischemic stroke.1,2,3,4 Long-term oral anticoagulant therapy (OAC) can reduce the stroke risk attributable to AF.5,6 While the prevalence of AF is lower in black individuals, they face a higher risk of stroke.7,8,9 Similarly, the prevalence of AF is lower in Hispanic patients but with poorer outcomes observed compared with white patients with AF.10,11,12
Prior studies have shown that anticoagulation use in underrepresented ethnic groups with AF is lower than in white individuals, with some of this disparity explained by socioeconomic status.13,14 Time in the therapeutic range (TTR) of international normalized ratio (INR) of 2.0 to 3.0 on warfarin, a measure of anticoagulation quality, has also been shown to be lower in black patients compared with white patients, as well as in patients with limited English proficiency, increasing the stroke risk in these populations.15,16 However, these studies did not examine whether these differences in AF care extended to the use of direct-acting oral anticoagulants (DOACs).17,18,19,20
We assessed contemporary racial/ethnic disparities in the use of warfarin and DOACs for patients with AF in the US-based Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II (ORBIT-AF II). The objectives of our analysis were to determine the rates of warfarin and DOAC use in patients with AF by race/ethnicity, assess the appropriateness of anticoagulant use by race/ethnicity per standard guidelines based on patients’ CHA2DS2-VASc scores,21 and examine anticoagulant quality and persistence by race/ethnicity.
Methods
Study Design
The rationale, design, and methods of the ORBIT-AF II registry have been published previously.22 Briefly, ORBIT-AF II is a prospective, multicenter, US-based registry of outpatients with AF. Patients were enrolled at 244 sites by various health care professionals, including primary care physicians, general cardiologists, and electrophysiologists. The ORBIT-AF II study only enrolled patients who either had a new diagnosis of AF within the prior 6 months or started receiving a DOAC for AF within the prior 3 months. The ORBIT-AF I cohort was not used in the current analysis since it preceded widespread use of DOAC medications.23 Eligible patients were those 21 years or older with electrocardiographically documented AF. Patients with transient AF owing to a reversible cause (eg, postoperative status), solitary atrial flutter without AF, or an estimated life expectancy of less than 6 months were excluded. A web-based case report form was used to collect patient demographics, medical history, medications, vital signs, laboratory data (including INR tests), imaging, and electrocardiographic parameters. Changes in pharmacotherapy, cardiac rhythm, and subsequent cardiovascular events and procedures were documented in follow-up.
Participants in the ORBIT-AF II study provided written informed consent, and sites received regulatory board approval for this study pursuant to local regulations. The study was coordinated by the Duke Clinical Research Institute and approved by the Duke University Institutional Review Board.
Study Population
Between February 2013 and July 2016, the registry enrolled 13 404 patients. Follow-up occurred at 6-month intervals and lasted 12 to 24 months, depending on enrollment date. At baseline, patients were asked to identify their race and ethnicity. Racial/ethnic groups were treated as mutually exclusive. For the present analysis, patients who selected identifiers other than “White,” “Black/African American,” or “Hispanic/Latino” at intake were excluded. We also excluded patients without any available follow-up information.
Statistical Analysis
Use of anticoagulants at the index ORBIT-II enrollment visit and other baseline characteristics were compared across race/ethnicity. Categorical variables are presented as frequencies and percentages, with differences between groups assessed by the χ2 test. Continuous variables are presented as median (interquartile range [IQR]) with differences between groups assessed by the Kruskal-Wallis test.
Racial/ethnic comparisons of percentages of any anticoagulant use, warfarin use, and DOAC use overall and in groups stratified by CHA2DS2-VASc scores (an index composed of points for congestive heart failure; hypertension; age ≥75 years; diabetes mellitus; prior stroke, transient ischemic attack, or thromboembolism; vascular disease; age 65-74 years; and sex category [female]) less than 2 or 2 or greater were assessed by the χ2 test. A multivariable logistic regression model with site as a random effect was used to evaluate the association between race/ethnicity and overall OAC use at baseline. The same model strategy was repeated for the association between race/ethnicity and DOAC use at baseline among patients on any OAC. The white racial group served as the reference group. Continuous variables, nonlinear with respect to the outcome, were fit with linear splines. The model was adjusted for patient characteristics that might explain the association between race/ethnicity and outcomes, including clinical characteristics (eg, medical history, laboratory data, medications, and AF type), clinician type, and sociodemographic characteristics (eg, education, insurance type, and median household income). Median household income was obtained from the American Community Survey (5-year estimate for the 2010-2014 data set) and linked using patient zip code.
Missing data (nonresponses) on the covariates used in the modeling was handled with multiple imputation, and imputed values were obtained by Markov chain Monte Carlo or regression methods. All variables included for adjustment had less than 5% missing, except for left ventricular ejection fraction (1339 of 12417 [10.8%]), estimated glomerular filtration rate (885 of 12417 [7.1%]), hematocrit (1435 of 12417 [11.6%]), and hemoglobin levels (1368 of 12417 [11.0%]). Associations are presented with odds ratios (ORs), 95% CIs, and P values.
The discontinuation of OAC medications was defined as a report of discontinuation of OAC with a discontinuation date and a patient’s receiving no OAC at the following visit. This definition minimizes discontinuations that are temporary. Time to discontinuation is displayed via a Kaplan-Meier plot. A Cox frailty model, with a random effect for site, was used to evaluate the association between race/ethnicity and OAC discontinuation before and after adjustment for potential confounders. Associations are presented as hazard ratios, 95% CIs, and P values.
We assessed quality of warfarin anticoagulation by TTR as calculated from the first INR to the last INR available, using the Rosendaal method.24 Any inter-INR test gaps greater than 8 weeks (ie, 56 days) were excluded. The median TTR length during follow-up was compared across groups with the Kruskal-Wallis test. For patients receiving DOACs at baseline, quality was assessed by whether the dose prescribed matched the US Food and Drug Administration label for each patient, given the patient’s age, weight, renal function, and concomitant medications, as previously described.22 The percentage of patients classified as appropriately dosed was compared across race/ethnicity by the χ2 test.
Statistical analyses were performed using SAS version 9.4 (SAS Institute), and 2-tailed P values <.05 were considered significant for all statistical tests. Data analysis occurred from February 2017 to February 2018.
Results
The baseline ORBIT-AF II population included 13 404 patients enrolled at 244 sites from February 2013 to July 2016. For this analysis, we excluded 546 patients who identified as races/ethnicities other than white, black, or Hispanic. We also excluded 1 patient who was taking more than 1 anticoagulant and 440 patients without any follow-up information. This yielded a study cohort of 12 417 patients, including 9166 patients with newly diagnosed AF (within 6 months of study entry). A total of 8572 of 12 417 patients (69.0%) were enrolled by general cardiologists, 2806 of 12 417 (22.6%) by electrophysiologists, and 942 of 12 417 (7.6%) by internists or primary care clinicians. Within this cohort, 11 100 patients (89.4%) were white, 646 (5.2%) were black, and 671 (5.4%) were Hispanic (Table 1).
Table 1. Patient Characteristics at Baseline by Race and Ethnicity.
| Demographic | Patients, No. (%) | P Value | ||
|---|---|---|---|---|
| White (n = 11 100) | Black (n = 646) | Hispanic (n = 671) | ||
| Age, median (IQR) | 71.0 (64.0-78.0) | 67.0 (60.0-76.0) | 72.0 (64.0-80.0) | <.001 |
| Female | 4544 (40.9) | 300 (46.4) | 315 (46.9) | <.001 |
| Insurance | ||||
| Private | 5947 (53.6) | 242 (37.5) | 297 (44.3) | <.001 |
| Medicaid | 318 (2.9) | 75 (11.6) | 104 (15.5) | |
| Medicare | 4326 (39.0) | 252 (39.0) | 198 (29.5) | |
| Other | 372 (3.4) | 63 (9.8) | 58 (8.6) | |
| None | 137 (1.2) | 14 (2.2) | 14 (2.1) | |
| Education level | ||||
| Some school | 853 (7.7) | 123 (19.0) | 228 (34.0) | <.001 |
| High school graduate | 5392 (48.6) | 361 (55.9) | 281 (41.9) | |
| College graduate | 3291 (29.6) | 111 (17.2) | 124 (18.5) | |
| Postgraduate | 1078 (9.7) | 22 (3.4) | 25 (3.7) | |
| Household income, median (IQR), $ | 56 354 (45 056-75 180) |
42 580 (33 557-52 572) |
51 010 (40 180-64 089) |
<.001 |
| CHA2DS2-VASc scorea | ||||
| Low (0) | 447 (4.0) | 23 (3.6) | 23 (3.4) | .06 |
| Medium (1) | 1228 (11.1) | 60 (9.3) | 60 (8.9) | |
| High (≥2) | 9425 (84.9) | 563 (87.2) | 588 (87.6) | |
| ORBIT bleeding scoreb | ||||
| Low (0-2 points) | 7336 (66.1) | 366 (56.7) | 363 (54.1) | <.001 |
| Medium (3 points) | 1496 (13.5) | 117 (18.1) | 88 (13.1) | |
| High (≥4 points) | 1536 (13.8) | 117 (18.1) | 113 (16.8) | |
| Smoking history | ||||
| Never | 5639 (50.8) | 334 (51.7) | 463 (69.0) | <.001 |
| Current | 792 (7.1) | 62 (9.6) | 28 (4.2) | |
| Former | 4669 (42.0) | 250 (38.7) | 180 (26.8) | |
| Hypertension | 8770 (79.0) | 572 (88.5) | 567 (84.5) | <.001 |
| Hyperlipidemia | 7214 (65.0) | 397 (61.5) | 410 (61.1) | .03 |
| Diabetes | 2759 (24.9) | 238 (36.8) | 264 (39.3) | <.001 |
| Congestive heart failure | 2333 (21.0) | 214 (33.1) | 141 (21.0) | <.001 |
| History of coronary artery disease | 2986 (26.9) | 162 (25.1) | 150 (22.4) | .02 |
| Prior cerebrovascular accident | 1212 (10.9) | 90 (13.9) | 80 (11.9) | .049 |
| BMI, median (IQR)c | 29.8 (26.0-34.9) | 31.2 (26.9-37.9) | 29.9 (26.2-34.4) | <.001 |
| Systolic blood pressure, median (IQR), mm Hgc | 126.0 (116.0-138.0) | 130.0 (120.0-142.0) | 128.0 (118.0-140.0) | <.001 |
| Clinician specialty | ||||
| Primary care | 736 (6.6) | 64 (9.9) | 142 (21.2) | <.001 |
| Cardiology | 7682 (69.2) | 419 (64.9) | 471 (70.2) | |
| Electrophysiology | 2585 (23.3) | 163 (25.2) | 58 (8.6) | |
| Neurology | 96 (0.9) | 0 (0.0) | 0 (0.0) | |
| Site region | ||||
| West | 1979 (17.8) | 80 (12.4) | 321 (47.8) | <.001 |
| Northeast | 2186 (19.7) | 70 (10.8) | 68 (10.1) | |
| Midwest | 2527 (22.8) | 83 (12.8) | 26 (3.9) | |
| South | 4408 (39.7) | 413 (63.9) | 256 (38.2) | |
| Contraindication to anticoagulationd | 675 (6.1) | 37 (5.7) | 32 (4.8) | .36 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
CHA2DS2-VASc stands for congestive heart failure; hypertension; age 75 years or older; diabetes mellitus; prior stroke, transient ischemic attack, or thromboembolism; vascular disease; age 65 to 74 years; and sex category (female).
ORBIT stands for older age (≥75 years); reduced hemoglobin, hematocrit, or history of anemia; bleeding history; insufficient kidney function; and treatment with an antiplatelet agent.
Values are median (IQR).
Included in contraindication to anticoagulation are a need for dual antiplatelet therapy, high bleeding risk, change in renal function, prior intracranial hemorrhage, and frequent falls or frailty.
Relative to white patients and Hispanic patients, black patients were significantly younger (median [IQR] age, white patients, 71.0 [64.0-78.0] years; black patients, 67.0 [60.0-76.0] years; Hispanic patients, 72.0 [64.0-80.0] years; P < .001; Table 1). Relative to white patients, black patients and Hispanic patients were more likely to be women (white patients, 4544 of 11100 [40.9%]; black patients, 300 of 646 [46.4%]; Hispanic patients, 315 of 671 [46.9%]; P < .001), more likely to have Medicaid health insurance (white patients, 318 [2.9%]; black patients, 75 [11.6%]; Hispanic patients, 104 [15.5%]; P < .001), and less likely to be college graduates (white patients, 3291 [29.6%]; black patients, 111 [17.2%]; Hispanic patients, 124 [18.5%]; P < .001) than white patients.
Black patients and Hispanic patients were more likely to have a high ORBIT bleeding risk score (white patients, 1536 [13.8%]; black patients, 117 [18.1%]; Hispanic patients, 113 [16.8%]; P < .001). (The ORBIT score assigns points for older age [≥75 years]; reduced hemoglobin, hematocrit, or history of anemia; bleeding history; insufficient kidney function; and treatment with an antiplatelet agent. In this study, a score of 4 or more points on a scale of 0 to 7 points was considered high.)
Black patients and Hispanic patients were also more likely to have a diagnosis of hypertension (white patients, 8770 [79.0%]; black patients, 572 [88.5%]; Hispanic patients, 567 [84.5%]; P < .001) and diabetes (white patients, 2759 [24.9%]; black patients; 238 [36.8%]; Hispanic patients, 264 [39.3%]; P < .001), and a history of stroke (white patients, 1212 [10.9%]; black patients, 90 [13.9%]; Hispanic patients, 80 [11.9%]; P = .049). In addition, they had higher median (IQR) systolic blood pressure levels (white patients, 126.0 [116.0-138.0] mm Hg; black patients, 130.0 [120.0-142.0] mm Hg; Hispanic patients: 128.0 [118.0-140.0] mm Hg; P < .001). Black patients had higher median body mass index values (calculated as weight in kilograms divided by height in meters squared) than the other groups did (white patients, 29.8 [26.0-34.9]; black patients, 31.2 [26.9-37.9]; Hispanic patients, 29.9 [26.2-34.4]; P < .001). Hispanic patients and black patients were more likely than white patients to be enrolled in the study by a primary care clinician (white patients, 736 [6.6%]; black patients, 64 [9.9%]; Hispanic patients, 142 [21.2%]; P < .001). Most black patients were from the South (n = 413 [63.9%]), nearly half of Hispanic patients were from the West (n = 321 [47.8%]), and white patients were more evenly distributed over US geographic regions, although the largest proportion came from the South (n = 4408 [39.7%]).
Physicians reported contraindications to oral anticoagulant therapy (including high bleeding risk, frequent falls, and frailty). The proportion with contraindications did not differ by race/ethnicity (Table 1).
Overall OAC use, either with warfarin or DOACs, was high, with 9865 of 11 100 white patients (88.9%), 544 of 646 black patients (84.2%), and 586 of 671 Hispanic patients (87.3%) reporting taking any OAC (Table 2). The unadjusted OR for any anticoagulant use among black patients compared with white patients was 0.71 (95% CI, 0.56-0.90). After adjusting for baseline clinical features, the OR increased modestly to 0.75 (95% CI, 0.56-0.99) (Table 2). There was no significant difference observed in OAC use between Hispanic patients and white patients (adjusted OR [aOR], 0.90 [95% CI, 0.66-1.23]).
Table 2. Association Between Race/Ethnicity and Use of Any Oral Anticoagulant.
| Racial/Ethnic Group | Patients Using OACs, No. (%) | Unadjusted | Adjusted for Baseline Clinical Featuresa | Adjusted for Additional Baseline Socioeconomic Markersb | |||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95%CI) | P Value | Odds Ratio (95%CI) | P Value | Odds Ratio (95%CI) | P Value | ||
| White (n = 11 000) | 9865 (88.9) | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Black (n = 646) | 544 (84.2) | 0.71 (0.56-0.90) | .005 | 0.75 (0.56-0.99) | 0.04 | 0.78 (0.59-1.04) | .09 |
| Hispanic (n = 671) | 586 (87.3) | 0.85 (0.65-1.12) | .25 | 0.90 (0.66-1.23) | 0.50 | 0.98 (0.71-1.36) | .92 |
Abbreviations: NA, not applicable; OAC, oral anticoagulant.
Baseline clinical features include demographics, medical history, medications, laboratory data, atrial fibrillation status, and enrolling physician specialty.
Baseline socioeconomic markers include median household income by zip code, level education, and insurance type. US geographic region is also included in this regression model.
Among patients receiving any OAC, DOACs were used more frequently than warfarin and differences between black patients and white patients were more clearly evident; the unadjusted OR was 0.60 (95% CI, 0.46-0.77). After adjustment for clinical features, the aOR was 0.63 (95% CI, 0.49-0.83) (Table 3). There was no significant difference observed in DOAC use between Hispanic individuals and white individuals (aOR, 0.92 [95% CI, 0.69-1.22]).
Table 3. Association Between Race/Ethnicity and Direct-Acting Oral Anticoagulant Use Among Patients Taking Oral Anticoagulants.
| Racial/Ethnic Group | Patients Using DOACs, No. (%) | Unadjusted | Adjusted for Baseline Clinical Featuresa | Adjusted for Additional Baseline Socioeconomic Markersb | |||
|---|---|---|---|---|---|---|---|
| Odds Ratio (95%CI) | P Value | Odds Ratio (95%CI) | P Value | Odds Ratio (95%CI) | P Value | ||
| White (n = 9865) | 8403 (85.2) | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Black (n = 544) | 423 (77.8) | 0.60 (0.46-0.77) | <.001 | 0.63 (0.49-0.83) | <.001 | 0.73 (0.55-0.95) | .02 |
| Hispanic (n = 586) | 465 (79.4) | 0.83 (0.64-1.09) | .19 | 0.92 (0.69-1.22) | .56 | 1.10 (0.81-1.49) | .54 |
Abbreviations: DOAC, direct-acting oral anticoagulant, NA, not applicable.
Baseline clinical features include demographics, medical history, medications, laboratory data, atrial fibrillation status, and enrolling physician specialty.
Baseline socioeconomic markers include median household income, level education, and insurance type. Geographic region is also included in this regression model.
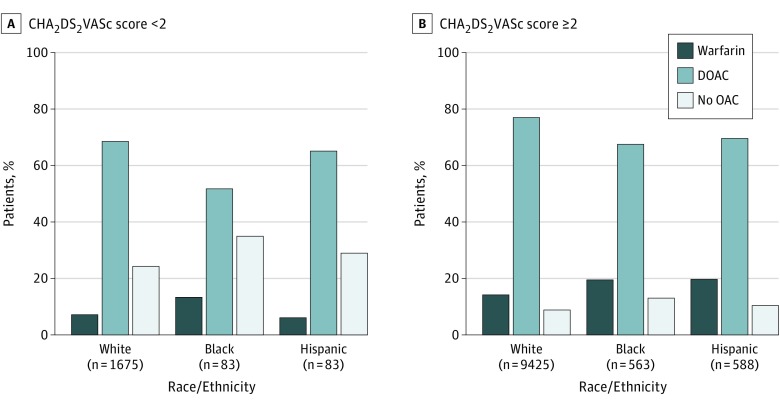
Across race/ethnicity, overall anticoagulant use was greater for those with CHA2DS2-VASc scores of 2 or more (9614 of 10 576 [90.9%]) than with those with CHA2DS2-VASc scores less than 2 (1381 of 1841 [75.0%]; P < .001) (Figure). Both black patients and Hispanic patients with CHA2DS2-VASc scores of 2 or more were less likely to receive DOACs than white patients (black patients, 67.5% [95% CI, 63.6%-71.4%]; Hispanic patients, 69.9% [95% CI, 66.2%-73.6%]; white patients, 77.0% [95% CI, 76.1%-77.8%]). Notably, differences between black and white patients persisted among patients with a CHA2DS2-VASc score less than 2 (black patients, 51.8% [95% CI, 41.1%-62.6%] vs white patients, 68.6% [95% CI, 66.4%-70.8%]), with no significant difference observed between white patients and Hispanic patients (65.1% [95% CI, 54.8%-75.3%]).
Figure. Association Between Race/Ethnicity and Use of Anticoagulants by Patients With Atrial Fibrillation by CHA2DS2-VASc Stroke Scores of Less Than 2 or 2 or Greater.
CHA2DS2-VASc indicates a score composed of points for congestive heart failure; hypertension; age ≥75 years; diabetes mellitus; prior stroke, transient ischemic attack, or thromboembolism; vascular disease; age 65-74 years; and sex category (female).
Adjusting for Socioeconomic Status
Additional adjusting for level of education, median household income by zip code, and insurance type, the markers of socioeconomic status, as well as region, produced a small change in the OR of use of any anticoagulant by black patients or white patients, but the value was no longer significant (aOR, 0.78 [95% CI, 0.59-1.04]; Table 2). (Complete results of the full model are provided in eTable 1 in the Supplement.) Addition of socioeconomic status markers reduced the difference between black patients and white patients with respect to DOAC use, but the independent effect of race remained significant (aOR, 0.73 [95% CI, 0.55-0.95]) (Table 3; eTable 2 in the Supplement). After adjustment for socioeconomic status, there remained no significant difference between Hispanic patients and white patients in any anticoagulant use (aOR, 0.98 [95% CI, 0.71-1.36]) or in DOAC use (aOR, 1.10 [95% CI, 0.81-1.49]). When the analyses were restricted to the 9166 patients with newly diagnosed AF, the results were highly similar (eTables 3 and 4 in the Supplement).
Anticoagulation Quality and Persistence
The study cohort included 1704 patients with AF who were treated with warfarin. The median number of INR tests during the follow-up period for patients taking warfarin for whom a TTR could be calculated (ie, those having at least 2 INR tests) was 18 (IQR, 8-26). The median number of INR tests by race/ethnicity was 17 (IQR, 8-26) for white patients, 18 (IQR, 8-26) for black patients, and 23 (IQR, 9-31) for Hispanic patients. Of patients taking warfarin, 799 of 1704 (46.9%) had their INRs managed by an anticoagulation clinic, with 72 of 121 Hispanic patients (59.5%) compared with 60 of 121 black patients (49.6%) and 667 of 1462 white patients (45.6%) followed up at such clinics. Relative to white patients, the median TTR was markedly lower in black patients and Hispanic patients (white patients, 67.1% [IQR, 51.8%-80.6%]; black patients, 57.1% [IQR, 39.9%-72.5%]; Hispanic patients, 51.7% [IQR, 39.1%-66.7%]; Table 4). Specifically, black patients (20.0% [IQR, 8.7%-41.2%]) and Hispanic patients (27.4% [IQR, 15.5%-41.0%]) had a significantly higher percentage of time spent with INR less than 2 than white patients did (16.0% [5.0%-29.4%]), with no significant difference observed in percent time with INR greater than 3.
Table 4. Quality of Anticoagulant Use by Race/Ethnicity.
| Characteristic | Patients Overall | White Patients | Black Patients | Hispanic Patients | P Value |
|---|---|---|---|---|---|
| Warfarin | |||||
| No. | 1704 | 1462 | 121 | 121 | |
| Time in therapeutic range during follow-up, median (IQR), %a | 66.0 (50.0-79.3) | 67.1 (51.8-80.6) | 57.1 (39.9-72.5) | 51.7 (39.1-66.7) | <.001 |
| Time spent with international normalized ratio, %, median (IQR) | |||||
| <2 | 17.0 (5.7-31.6) | 16.0 (5.0-29.4) | 20.0 (8.7-41.2) | 27.4 (15.5-41.0) | <.001 |
| >3 | 10.8 (1.4-21.2) | 10.4 (0.8-20.4) | 11.5 (2.5-22.4) | 13.5 (2.2-23.6) | .23 |
| Dose of direct-acting oral anticoagulant, No. (%) | |||||
| No. | 8791 | 7988 | 394 | 409 | |
| Underdose | 824 (9.4) | 726 (9.1) | 44 (11.2) | 54 (13.2) | .01 |
| Appropriate | 7653 (87.1) | 6985 (87.4) | 333 (84.5) | 335 (81.9) | |
| Excessive | 314 (3.6) | 277 (3.5) | 17 (4.3) | 20 (4.9) |
Abbrevation: IQR, interquartile range.
Missing 26.1% of data in the time in therapeutic range in follow-up overall, including 26.1% of white patients, 28.1% of black patients, and 24.8% of Hispanic patients.
Overall, DOAC dosing differed from that specified on the Food and Drug Administration label in 13.0% of cases. Such inappropriate DOAC dosing was seen in 15.5% of black patients (underdosing, 44 of 394 patients [11.2%]; excessive dosing, 17 patients [4.3%]) and 18.1% of Hispanic patients (underdosing, 54 of 409 patients [13.2%]; excessive dosing, 20 patients [4.9%]) compared with 12.6% of white patients (underdosing, 726 of 7988 patients [9.1%]; excessive dosing, 277 patients [3.5%]; P = .01 for differences across the 3 groups) (Table 4). Most inappropriate dosing of DOACs was underdosing.
The time to discontinuation of anticoagulation was similar across racial/ethnic groups (eFigure in the Supplement). After adjusting for patient sociodemographic and clinical factors, the adjusted hazard ratio for discontinuing anticoagulant therapy was 0.88 (95% CI, 0.70-1.12) for black patients and 0.99 (95% CI, 0.79-1.25) for Hispanic patients compared with white patients.
Discussion
Anticoagulation is standard therapy for patients with AF who are at increased stroke risk. Racial and ethnic disparities in anticoagulant use have been described previously.25,26 However, few studies have explored racial/ethnic disparities in the use of DOACs by patients with AF. We examined the association between race/ethnicity and the use of any OAC, and specifically DOACs, in patients with AF in the ORBIT-AF II registry. There are several notable findings from this analysis. First, although OAC use was high in the ORBIT-AF II registry, black patients were less likely to use any OAC than white patients and were particularly less likely to use DOACs. Hispanic patients, however, had similar treatment rates with any OAC and DOACs as white patients. Second, while we expected to see the difference in race mediated by socioeconomic status, differences between black and white patients largely persisted despite inclusion of socioeconomic markers in our statistical models. Third, anticoagulation quality was poorer in black patients and Hispanic patients, with lower overall TTR and lower rates of appropriate DOAC dosing. Lastly, rates of discontinuation of OAC were similar across races/ethnicities.
Prior studies have addressed racial/ethnic disparities in the use of anticoagulants in AF. Using the American College of Cardiology National Cardiovascular Data Registry’s outpatient registry, Katz et al27 found that black patients with AF had a lower odds of receiving any OAC (OR, 0.85 [95% CI, 0.81-0.90]) and specifically DOAC prescriptions (OR, 0.66 [95% CI, 0.60-0.73]) compared with white patients. A limitation of this study was its high rate of missing data (29.7%-33.0%) for race/ethnicity. Using Get with the Guidelines–Stroke data, Patel et al28 found the aOR of receiving DOAC therapy was 1.2 times greater for white patients than for nonwhite patients with AF (95% CI, 1.09-1.32), but this study only included patients who were hospitalized with stroke.
Using a random sample of Medicare beneficiaries newly diagnosed with AF, researchers found that black race was significantly associated with a lower odds of receiving DOACs (ie, dabigatran and rivaroxaban) compared with receiving warfarin.29 The study period for this report from Medicare concluded on December 31, 2012, and was thus unlikely to represent current DOAC usage patterns. The earlier ORBIT-AF I registry also observed differences in anticoagulant use and treatment quality by race/ethnicity.30 However, the ORBIT-AF I study was unable to assess contemporary use of DOAC medications. Additionally, none of these studies included detailed data on INR measures and DOAC dosing, as the present analysis does.
There have been several possible reasons proposed to explain racial/ethnic disparities in AF management. First, limited access to specialists in minority populations has been described and remains an important target of interventions to reduce disparities.31 In our study, a higher percentage of black patients and Hispanic patients than white patients were enrolled by primary care physicians. While we observed that internal medicine and primary care clinicians were less likely to prescribe DOACs than cardiologists and electrophysiologists, our results were adjusted for clinician type (eTables 1 and 2 in the Supplement). Second, out-of-pocket costs for DOACs may be a greater barrier to their use among patients in lower socioeconomic brackets. Adjustment for socioeconomic status did not substantially reduce the racial differences in our results, but our control for economic determinants is incomplete. Others have also highlighted the roles of health literacy, patient perceptions, patient adherence, implicit bias, and trust in medical care as additional explanations of racial/ethnic disparities in care.16,32,33,34,35 This study cannot address these latter features. Detailed assessment of the respective roles and preferences of patients and physicians in the anticoagulation decision is merited.
Notably, we found that increased rates of OAC use among white patients extended to patients with CHA2DS2-VASc scores less than 2, a group at low risk of stroke in which there may be little net benefit of OACs. Such possible overuse is consistent with other observations of potentially harmful medical overuse among individuals of higher socioeconomic status in the United States.36 While racial/ethnic disparities are usually marked by underuse, overuse in racial/ethnic majority populations is another reasonable target for quality improvement initiatives.
As we and others have shown, the quality of warfarin treatment is lower in racial/ethnic minority patients than white patients, and poor TTR is associated with increased stroke risk.37,38 Further, black patients with AF were less likely to receive DOACs, which are easier to use than warfarin and likely safer.39,40 Recent evidence has shown that medication adherence is higher for DOACs than for warfarin.41 This increase in adherence to DOACs over warfarin may serve as a way to improve anticoagulant treatment in racial/ethnic minority patients with AF. Our findings are particularly notable given this population’s access to health care (ie, all included patients were recruited from medical clinics).
This analysis has several strengths. It is, to our knowledge one of the first studies to compare baseline use of DOACs by race/ethnicity as well as the quality of DOAC use. The data were obtained from a prospectively assembled registry with detailed clinical information and close follow-up, thereby avoiding pitfalls of alternative designs, such as administrative database analyses.42
Limitations
There are also potential limitations to our analyses. First, because this was an observational study, we cannot exclude the possibility of residual or unmeasured confounding. Second, there can be concerns about the representativeness of patients enrolled in registries. The ORBIT-AF II registry sought recruitment sites throughout the United States, but investigator participation was voluntary, and patients had to agree to enter the study through the informed consent process.43 These aspects of study design may raise concerns whether these findings apply to the broad population of patients with AF.44 The proportion of patients in the ORBIT-AF II registry overall who were taking anticoagulants was 89%, higher than that reported from cohorts that were less selective. For example, a recent claims-based study from the Veterans’ Administration reported 63% of patients with AF were taking anticoagulants.25
Similarly, the overall average TTR of patients taking warfarin in the ORBIT-AF II registry, 67%, is higher than the average TTR of 56% reported by the Veteran’s Administration.25 However, despite these higher overall indices of anticoagulation quality, we still observed clear racial disparities in use of anticoagulants in the ORBIT-AF II registry. Notably, the difference between black patients and white patients in TTR in this study (−10%) was very similar to the difference observed in the VA study (−8%).25 As a result, the racial disparities we report appear to be more broadly generalizable.
A third limitation of our analyses is the reduced statistical power of some racial/ethnic comparisons. This issue is common in studies of AF, owing to the overall lower prevalence of AF in racial/ethnic minority populations along with limited representation of such minorities in clinical trials and registries.45 Fourth, patients in the ORBIT-AF II registry were preferentially selected if they were starting a DOAC. This sampling feature increased the proportion using DOACs but still allowed evaluation of racial and ethnic differences in the use of these anticoagulants. Lastly, our measures of socioeconomic status were limited and measures such as zip-code level income may not have fully characterized an individual’s socioeconomic status.
Conclusions
In the ORBIT-AF II registry of patients with AF, we found reduced use of OAC therapy in black patients compared with white patients and Hispanic patients. These differences persisted after controlling for socioeconomic markers and region. The effect was particularly pronounced for DOAC use. We also found that anticoagulation quality in black patients and Hispanic patients was inferior to that that in white patients, with lower TTR values in those taking warfarin and modestly greater underdosing in patients taking DOACs. These results contribute toward understanding racial/ethnic differences in stroke-preventive treatment in patients with AF. Novel approaches are needed to address modifiable causes of racial/ethnic disparities in anticoagulant use, a central issue in improving the overall quality of care for patients with AF.
eTable 1. Association between Race, Ethnicity and any OAC use at baseline, including demographic and clinical features, enrolling physician specialty, and socioeconomic markers
eTable 2. Association between Race, Ethnicity and DOAC use at baseline among patients on an OAC, including demographic and clinical features, enrolling physician specialty, and socioeconomic markers
eTable 3. Association between Race/Ethnicity and any OAC use, restricted to patients newly diagnosed with atrial fibrillation
eTable 4. Association between Race/Ethnicity and DOAC use among patients on an OAC, restricted to patients newly diagnosed with atrial fibrillation
eFigure. Kaplan-Meier plot representing the time to discontinuation of any oral anticoagulant by race/ethnicity over one year
References
- 1.Magnani JW, Rienstra M, Lin H, et al. Atrial fibrillation: current knowledge and future directions in epidemiology and genomics. Circulation. 2011;124(18):1982-1993. doi: 10.1161/CIRCULATIONAHA.111.039677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370-2375. doi: 10.1001/jama.285.18.2370 [DOI] [PubMed] [Google Scholar]
- 3.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22(3):312-318. doi: 10.1161/01.STR.22.3.312 [DOI] [PubMed] [Google Scholar]
- 4.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly: the Framingham Study. Arch Intern Med. 1987;147(9):1561-1564. doi: 10.1001/archinte.1987.00370090041008 [DOI] [PubMed] [Google Scholar]
- 5.Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation: analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154(13):1449-1457. doi: 10.1001/archinte.1994.00420130036007 [DOI] [PubMed] [Google Scholar]
- 6.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955-962. doi: 10.1016/S0140-6736(13)62343-0 [DOI] [PubMed] [Google Scholar]
- 7.Alonso A, Agarwal SK, Soliman EZ, et al. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2009;158(1):111-117. doi: 10.1016/j.ahj.2009.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magnani JW, Norby FL, Agarwal SK, et al. Racial differences in atrial fibrillation-related cardiovascular disease and mortality: the Atherosclerosis Risk in Communities (ARIC) study. JAMA Cardiol. 2016;1(4):433-441. doi: 10.1001/jamacardio.2016.1025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross JS, Halm EA, Bravata DM. Use of stroke secondary prevention services: are there disparities in care? Stroke. 2009;40(5):1811-1819. doi: 10.1161/STROKEAHA.108.539619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borzecki AM, Bridgers DK, Liebschutz JM, Kader B, Kazis LE, Berlowitz DR. Racial differences in the prevalence of atrial fibrillation among males. J Natl Med Assoc. 2008;100(2):237-245. doi: 10.1016/S0027-9684(15)31212-8 [DOI] [PubMed] [Google Scholar]
- 11.Bush D, Martin LW, Leman R, Chandler M, Haywood LJ; NHLBI AFFIRM Investigators . Atrial fibrillation among African Americans, Hispanics and Caucasians: clinical features and outcomes from the AFFIRM trial. J Natl Med Assoc. 2006;98(3):330-339. [PMC free article] [PubMed] [Google Scholar]
- 12.Dewland TA, Olgin JE, Vittinghoff E, Marcus GM. Incident atrial fibrillation among Asians, Hispanics, blacks, and whites. Circulation. 2013;128(23):2470-2477. doi: 10.1161/CIRCULATIONAHA.113.002449 [DOI] [PubMed] [Google Scholar]
- 13.Birman-Deych E, Radford MJ, Nilasena DS, Gage BF. Use and effectiveness of warfarin in Medicare beneficiaries with atrial fibrillation. Stroke. 2006;37(4):1070-1074. doi: 10.1161/01.STR.0000208294.46968.a4 [DOI] [PubMed] [Google Scholar]
- 14.Sholzberg M, Gomes T, Juurlink DN, Yao Z, Mamdani MM, Laupacis A. The influence of socioeconomic status on selection of anticoagulation for atrial fibrillation. PLoS One. 2016;11(2):e0149142. doi: 10.1371/journal.pone.0149142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen AY-J, Yao JF, Brar SS, Jorgensen MB, Wang X, Chen W. Racial/ethnic differences in ischemic stroke rates and the efficacy of warfarin among patients with atrial fibrillation. Stroke. 2008;39(10):2736-2743. doi: 10.1161/STROKEAHA.107.508580 [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez F, Hong C, Chang Y, et al. Limited English proficient patients and time spent in therapeutic range in a warfarin anticoagulation clinic. J Am Heart Assoc. 2013;2(4):e000170-e000170. doi: 10.1161/JAHA.113.000170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Connolly SJ, Ezekowitz MD, Yusuf S, et al. ; RE-LY Steering Committee and Investigators . Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139-1151. doi: 10.1056/NEJMoa0905561 [DOI] [PubMed] [Google Scholar]
- 18.Giugliano RP, Ruff CT, Braunwald E, et al. ; ENGAGE AF-TIMI 48 Investigators . Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093-2104. doi: 10.1056/NEJMoa1310907 [DOI] [PubMed] [Google Scholar]
- 19.Granger CB, Alexander JH, McMurray JJV, et al. ; ARISTOTLE Committees and Investigators . Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992. doi: 10.1056/NEJMoa1107039 [DOI] [PubMed] [Google Scholar]
- 20.Patel MR, Mahaffey KW, Garg J, et al. ; ROCKET AF Investigators . Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-891. doi: 10.1056/NEJMoa1009638 [DOI] [PubMed] [Google Scholar]
- 21.Lip GYHH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest. 2010;137(2):263-272. doi: 10.1378/chest.09-1584 [DOI] [PubMed] [Google Scholar]
- 22.Steinberg BA, Shrader P, Thomas L, et al. ; ORBIT-AF Investigators and Patients . Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II registry. J Am Coll Cardiol. 2016;68(24):2597-2604. doi: 10.1016/j.jacc.2016.09.966 [DOI] [PubMed] [Google Scholar]
- 23.Piccini JP, Fraulo ES, Ansell JE, et al. Outcomes registry for better informed treatment of atrial fibrillation: rationale and design of ORBIT-AF. Am Heart J. 2011;162(4):606-612.e1. doi: 10.1016/j.ahj.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 24.Rosendaal FR, Cannegieter SC, van der Meer FJ, Briët E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69(3):236-239. doi: 10.1055/s-0038-1651587 [DOI] [PubMed] [Google Scholar]
- 25.Yong C, Azarbal F, Abnousi F, et al. Racial differences in quality of anticoagulation therapy for atrial fibrillation (from the TREAT-AF Study). Am J Cardiol. 2016;117(1):61-68. doi: 10.1016/j.amjcard.2015.09.047 [DOI] [PubMed] [Google Scholar]
- 26.Thomas KL, Piccini JP, Liang L, et al. ; Get With the Guidelines Steering Committee and Hospitals . Racial differences in the prevalence and outcomes of atrial fibrillation among patients hospitalized with heart failure. J Am Heart Assoc. 2013;2(5):e000200. doi: 10.1161/JAHA.113.000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katz DF, Maddox TM, Turakhia M, et al. Contemporary trends in oral anticoagulant prescription in atrial fibrillation patients at low to moderate risk of stroke after guideline-recommended change in use of the CHADS2 to the CHA2DS2-VASc score for thromboembolic risk assessment: analysis from the National Cardiovascular Data Registry’s Outpatient Practice Innovation and Clinical Excellence Atrial Fibrillation Registry. Circ Cardiovasc Qual Outcomes. 2017;10(5):e003476. doi: 10.1161/CIRCOUTCOMES.116.003476 [DOI] [PubMed] [Google Scholar]
- 28.Patel PA, Zhao X, Fonarow GC, et al. Novel oral anticoagulant use among patients with atrial fibrillation hospitalized with ischemic stroke or transient ischemic attack. Circ Cardiovasc Qual Outcomes. 2015;8(4):383-392. doi: 10.1161/CIRCOUTCOMES.114.000907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baik SH, Hernandez I, Zhang Y. Evaluating the initiation of novel oral anticoagulants in Medicare beneficiaries. J Manag Care Spec Pharm. 2016;22(3):281-292. doi: 10.18553/jmcp.2016.22.3.281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Golwala H, Jackson LR II, Simon DN, et al. ; Outcomes Registry for Better Informed Treatment for Atrial Fibrillation (ORBIT-AF) Registry . Racial/ethnic differences in atrial fibrillation symptoms, treatment patterns, and outcomes: insights from Outcomes Registry for Better Informed Treatment for Atrial Fibrillation Registry. Am Heart J. 2016;174:29-36. doi: 10.1016/j.ahj.2015.10.028 [DOI] [PubMed] [Google Scholar]
- 31.Cook NL, Ayanian JZ, Orav EJ, Hicks LS. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation. 2009;119(18):2463-2470. doi: 10.1161/CIRCULATIONAHA.108.825133 [DOI] [PubMed] [Google Scholar]
- 32.Fang MC, Machtinger EL, Wang F, Schillinger D. Health literacy and anticoagulation-related outcomes among patients taking warfarin. J Gen Intern Med. 2006;21(8):841-846. doi: 10.1111/j.1525-1497.2006.00537.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lip GYH, Kamath S, Jafri M, Mohammed A, Bareford D. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke. 2002;33(1):238-242. doi: 10.1161/hs0102.101817 [DOI] [PubMed] [Google Scholar]
- 34.Halbert CH, Armstrong K, Gandy OH Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166(8):896-901. doi: 10.1001/archinte.166.8.896 [DOI] [PubMed] [Google Scholar]
- 35.Borne RT, O’Donnell C, Turakhia MP, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017;17(1):236. doi: 10.1186/s12872-017-0671-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Welch HG, Fisher ES. Income and cancer overdiagnosis—when too much care is harmful. N Engl J Med. 2017;376(23):2208-2209. doi: 10.1056/NEJMp1615069 [DOI] [PubMed] [Google Scholar]
- 37.Pokorney SD, Simon DN, Thomas L, et al. ; Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) Investigators . Patients’ time in therapeutic range on warfarin among US patients with atrial fibrillation: results from ORBIT-AF registry. Am Heart J. 2015;170(1):141-148, 148.e1. doi: 10.1016/j.ahj.2015.03.017 [DOI] [PubMed] [Google Scholar]
- 38.Connolly SJ, Pogue J, Eikelboom J, et al. ; ACTIVE W Investigators . Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008;118(20):2029-2037. doi: 10.1161/CIRCULATIONAHA.107.750000 [DOI] [PubMed] [Google Scholar]
- 39.López-López JA, Sterne JAC, Thom HHZ, et al. Oral anticoagulants for prevention of stroke in atrial fibrillation: systematic review, network meta-analysis, and cost effectiveness analysis. BMJ. 2017;359:j5058. doi: 10.1136/bmj.j5058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shen AY-J, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007;50(4):309-315. doi: 10.1016/j.jacc.2007.01.098 [DOI] [PubMed] [Google Scholar]
- 41.Yao X, Abraham NS, Alexander GC, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. 2016;5(2):e003074. doi: 10.1161/JAHA.115.003074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinn GR, Severdija ON, Chang Y, Dallalzadeh LO, Singer DE. Methodologic differences across studies of patients with atrial fibrillation lead to varying estimates of stroke risk. J Am Heart Assoc. 2018;7(12):e007537. doi: 10.1161/JAHA.117.007537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Steinberg BA, Blanco RG, Ollis D, et al. ; ORBIT-AF Steering Committee Investigators . Outcomes registry for better informed treatment of atrial fibrillation II: rationale and design of the ORBIT-AF II registry. Am Heart J. 2014;168(2):160-167. doi: 10.1016/j.ahj.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.El Emam K, Jonker E, Moher E, Arbuckle L. A review of evidence on consent bias in research. Am J Bioeth. 2013;13(4):42-44. doi: 10.1080/15265161.2013.767958 [DOI] [PubMed] [Google Scholar]
- 45.Jackson LR II, Peterson ED, Okeagu E, Thomas K. Review of race/ethnicity in non vitamin K antagonist oral anticoagulants clinical trials. J Thromb Thrombolysis. 2015;39(2):222-227. doi: 10.1007/s11239-014-1145-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Association between Race, Ethnicity and any OAC use at baseline, including demographic and clinical features, enrolling physician specialty, and socioeconomic markers
eTable 2. Association between Race, Ethnicity and DOAC use at baseline among patients on an OAC, including demographic and clinical features, enrolling physician specialty, and socioeconomic markers
eTable 3. Association between Race/Ethnicity and any OAC use, restricted to patients newly diagnosed with atrial fibrillation
eTable 4. Association between Race/Ethnicity and DOAC use among patients on an OAC, restricted to patients newly diagnosed with atrial fibrillation
eFigure. Kaplan-Meier plot representing the time to discontinuation of any oral anticoagulant by race/ethnicity over one year