Abstract
Objective: To observe and evaluate the long‐term results of minimal incision osteotomy for hallux abducto valgus.
Methods: From February 1995 to May 1999, 372 cases (705 feet) with hallux abducto valgus were treated with minimal incision osteotomy. Seventy‐nine patients (150 feet) were followed up for more than five years (mean 7.5; range, 5.3–13.2 years) after surgery. The preoperative and postoperative hallux abducto valgus angles (HVA), intermetatarsal angles (IMA), tibial sesamoid position (TSP), American Orthopaedic Foot And Ankle Society (AOFAS) score, range of movement of the first metatarsophalangeal joint and lateral metatarsalgia were observed, measured and evaluated.
Results: Based on clinic curative effect evaluation criterion, 56 feet (37.3%) were excellent, 88 feet (58.7%) good, 6 feet (4.0%) fair. The postoperative mean AOFAS score was 84.20 ± 4.32 points. The mean HVA decreased from 33.28o to 12.31o and the mean IMA1‐2 from 11.75o to 6.80o. The TSP was corrected from an average preoperative grade of 4.29 to a grade of 3.07 by final follow‐up. There was no nonunion or delayed union, no avascular necrosis, no infection, and no hallux varus. Numbness in the big toe was found in 4 feet (2.7%). The range of motion of the first metatarsophalangeal joint decreased from 70.20o to 69.53o. Of 97 feet (64.7%) with pre‐operative 2–5 metatarsalgia, this had disappeared in 35 feet, improved in 54 feet and was aggravated in 8 feet postoperatively.
Conclusion: Minimal incision osteotomy is a simple and reliable technique for treating hallux abducto valgus with minimal complications.
Keywords: Hallux valgus; Surgical procedures, minimally invasive; Treatment outcome
Introduction
Minimal incision osteotomy, which is adopted by many hospitals in China, has a positive effect in the short‐ and midterm 1 , 2 . However, so far as the present authors know, its long‐term outcome has not yet been reported. What is the long term effect of minimal incision osteotomy on hallux abducto valgus? Does it recur or not? These are the questions which need to be answered. In order to evaluate its long‐term effect, all data on patients who were followed up for more than five years after minimal incision osteotomy in our hospital was reviewed. The data on 79 patients (150 feet) were collected and analyzed.
Materials and methods
General data
From February 1995 to May 1999, 705 feet of 372 patients with hallux abducto valgus were treated by minimal incision osteotomy. One hundred and fifty feet of 79 cases, in whom complete data was collected, were followed up for more than five years. There were 45 feet with slight deformity, 60 with moderate deformity and 45 with severe deformity in this group. The age of the patients ranged from 13 to 75 years, with an average age of 47 years. There were 73 female patients with 140 feet and 6 male patients with 10 feet. Seventy‐one cases had both feet treated and eight had one foot treated.
Surgical procedure
A curved incision of about 1 cm was made on the proximal medial side of the proximal phalanx of the hallux, then the articular capsule was separated with a periosteal detacher and the osteophyte on the medial head of the metatarsal abraded with a high speed drill, after which the medial side of the metatarsal head was trimmed with an osteotribe.
Next an incision was made about 0.5 cm from the medial side of the first metatarsal neck and an oblique osteotomy performed. Complete flushing was required to ensure no bone debris remained in the articular capsule. The distal metatarsal head was pushed laterally by the width of the bone cortex, preventing the distal osteotomy block from moving to the dorsal side. A bandage was applied starting from the first and second toe web and then crossing the ankle to form an “8” shape. The hallux was stabilized at a varus position of 5o by adhesive plaster, also in an “8” shape.
During the operation, osteotomy of the neck of the metatarsal was performed if metatarsalgia had been reported on the other metatarsal head; interdigital arthroplasty was performed if a hammer toe was found and osteotomy on the metatarsal was required if a bunionette had formed.
Clinical and radiographic evaluation
X‐ray measurements
These included hallux abducto valgus angles (HVA), intermetatarsal angles (IMA) (Fig. 1), the interval between the first and second metatarsal heads, the length of the gap between the first and second metatarsal, the width of the first metatarsal head and the tibial sesamoid bone position (TSP). The method of measuring TSP was designed to identify the relative position of the tibial sesamoid by observing its relationship with the axis of the first metatarsal
3
. The site of the sesamoid, ranging from the its normal position to the fibular side, is divided into seven positions which are marked separately by  to
to  as follows and measured by corresponding statistical data 1 to 7.
as follows and measured by corresponding statistical data 1 to 7.  indicates the position of the tibial sesamoid is normal and
indicates the position of the tibial sesamoid is normal and  means the most severe dislocation (Fig. 2).
means the most severe dislocation (Fig. 2).
Figure 1.
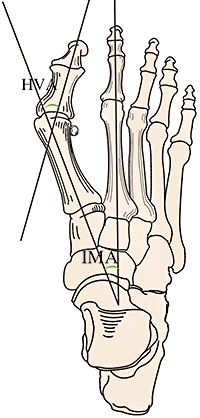
Diagram illustrating HVA and IMA. HVA, hallux abducto valgus angles; IMA, intermetatarsal angles.
Figure 2.
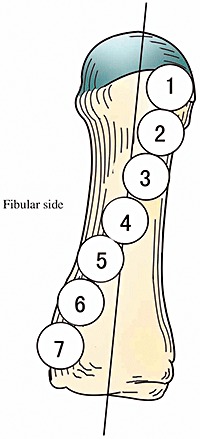
TSP grading method: from  to
to  indicates the position of tibial sesamoid gradually moving outwards.
indicates the position of tibial sesamoid gradually moving outwards.  means normal tibial sesamoid position;
means normal tibial sesamoid position;  means the lateral side of the sesamoid is tangential to the axis of the first metatarsal;
means the lateral side of the sesamoid is tangential to the axis of the first metatarsal;  means the axis passes through the 1/3 of the sesamoid on the fibular side;
means the axis passes through the 1/3 of the sesamoid on the fibular side;  means the sesamoid is on the central axis;
means the sesamoid is on the central axis;  means the axis passes through the 1/3 of the sesamoid on the tibial side;
means the axis passes through the 1/3 of the sesamoid on the tibial side;  means the tibial side of the sesamoid tangential to the axis of the first metatarsal;
means the tibial side of the sesamoid tangential to the axis of the first metatarsal;  means the most serious dislocation of the tibial sesamoid.
means the most serious dislocation of the tibial sesamoid.
Clinical evaluation
The data collected included the hallux metatarsophalangeal‐interphalangeal scale of the American Orthopaedic Foot And Ankle Society (AOFAS) score 4 , the range of movement (ROM) of the first metatarsophalangeal joint (plantar flexion plus dorsal flexion), hallux position, hallux rotation, and callus under the second and third metatarsal heads (or metatarsalgia).
Standards for clinical therapeutic effect evaluation
The evaluation of therapeutic effect is based on the standards reported by Wen et al., which are as follows: excellent: hallux valgus deformity has been corrected, bunion is no longer present, HVA angle < 20°, IM angle < 9°; fine: hallux valgus deformity has been corrected, bunion is no longer present, HVA angle between 20° and 25°, IM angle between 9° and 12°; poor: the symptoms still exist, HVA angle and IM angle are not significantly better than before 2 .
Statistical analysis
The SPSS 12.0 (SPSS, Chigago, IL, USA) statistical database package was applied for data analysis. Preoperative and postoperative data were compared by Student's t‐test or non‐parameter test. P < 0.05 was considered significant.
Results
All patients were treated by minimal incision osteotomy. In addition, osteotomy on the neck of the metatarsal bone was performed in four feet (2.7%); bunionette varus osteotomy and straightening in three feet (2.0%) and proximal interdigital arthroplasty for hammer toe in three feet (2.0%).
The follow‐up time ranged from 5.3 to 13.2 years, with an average of 7.5 years. There was no nonunion or delayed union of the osteotomized end, no avascular necrosis of the first metatarsal head, no infections and no hallux varus. Numbness on part of the medial side of the hallux was found in four feet.
Postoperatively an excellent result was achieved in 56 feet (37.3%), good in 88 feet (58.7%), and inadequate in 6 feet (4.0%). The excellent to good rate was 96.0%. A typical case is shown in Fig. 3a–f. The postoperative AOFAS score was 84.20 ± 4.32 points.
Figure 3.
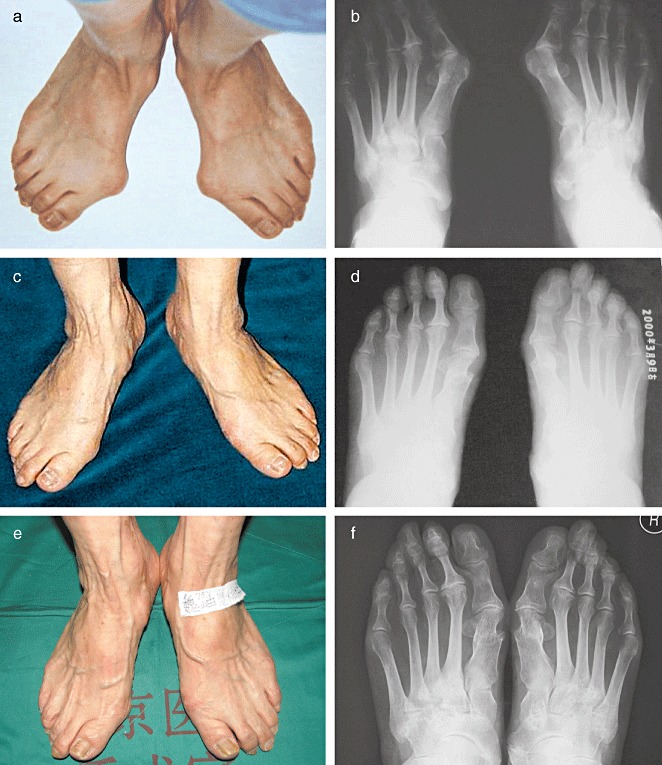
Woman, 79 years old. (a) Preoperative appearance; (b) Preoperative X‐ray film. HVA: left 48°, right 45°; IMA: left 16°, right 16°. (c) Postoperative appearance after 5 years. (d) X‐ray film 5 years postoperatively. HVA: left 18°, right 19°; IMA: left 4°, right 6°. (e) Postoperative appearance after 10 years. (f) X‐ray film 10 years postoperatively. HVA: left 19°, right 19°; IMA: left 6°, right 6°.
There were significant differences between preoperative and postoperative imaging observation indicators. Similar outcomes were found in the ROM of the first metatarsophalangeal joint (Table 1).
Table 1.
Comparison of preoperative and postoperative X‐ray measurements and joint function evaluation (n= 150)
| Observation indicators | Preoperative | Postoperative | t | P |
|---|---|---|---|---|
| HVA (°) | 33.28 ± 9.59 | 12.31 ± 4.64 | −10.63 | < 0.01 |
| IMA (°) | 11.75 ± 2.89 | 6.80 ± 1.95 | −10.46 | < 0.01 |
| Interval between first and second metatarsal head (cm) | 1.14 ± 0.26 | 0.96 ± 0.25 | −8.81 | < 0.01 |
| Length gap between first and second metatarsal (cm) | 0.39 ± 0.26 | 0.59 ± 0.26 | −8.46 | < 0.01 |
| Width (cm) | 2.11 ± 0.29 | 1.60 ± 0.30 | 20.27 | < 0.01 |
| TSP | 4.29 ± 1.06 | 3.07 ± 0.95 | −8.76 | < 0.01 |
| Plantarflexion plus dorsiflexion (°) | 70.20 ± 12.82 | 69.53 ± 12.03 | −2.66 | 0.078 |
With regard to the position of the hallux, all patients had hallux abducto valgus to some extent preoperatively, postoperatively 142 halluces (94.7%) had came back to a normal position and slight valgus remained in 8 feet (5.3%).
With regard to rotation of the hallux, 54 halluces (36.0%) were in a neutral position and 96 (64.0%) in a pronated position preoperatively; all 96 feet (100%) had been rectified to a neutral position postoperatively.
With regard to metatarsalgia of the second and third metatarsal heads, 97 feet (64.7%) were affected by metatarsalgia preoperatively; in 35 of those feet (23.3%) the pain had completely resolved, in 54 (36.0%) it was relieved, and in 8 (5.3%) there was no improvement or even worse pain postoperatively.
Discussion
The long‐term effect of minimal incision osteotomy for hallux abducto valgus
During long‐term follow‐up, the good and excellent rate was 96.0%, which is similar to the reported short‐ or midterm curative effect 1 , 2 . After surgery, the AOFAS score reached 84.20 ± 4.32. The mean HVA angle reduced by 20.97° compared with that before surgery, and the IMA by 4.95°. The first metatarsal was shortened by 0.2 cm on average and the TSP reduced by 1.22, the ROM of the first metatarsophalangeal joint reduced by 0.67°. Meanwhile, the surgery rectified the rotation of the hallux well. The incidence of metatarsalgia was considerably lower. The evidence indicates that the long‐term therapeutic effect of this technique is positive.
The minimal incision osteotomy which was adopted for osteotomy of the neck of the metatarsal bone is not adequate for severe hallux abducto valgus. In this group, all the fair results (6/150) were achieved in cases of severe hallux abducto valgus with an HVA angle > 60°. This indicates that it is very hard to rectify severe deformity to a satisfactory degree. Some patients had degeneration and arthritis in the first metatarsal joint. Surgery cannot relieve the pain from arthritis of the first metatarsal joint and therefore cannot have a beneficial effect in these cases. Therefore suitable cases for this surgical method must be carefully selected. Patients with severe hallux abducto valgus are not suitable for minimal incision osteotomy. However, joint replacement, arthrodesis or Keller's osteotomy could be performed on them instead.
In addition, some of the patients (4/150) had numbness over part of the medial skin of the hallux. This was considered to be a result of cutting the medial cutaneous nerve of the hallux with the curved incision, which is in accordance with the innervation of the medial part of the first metatarsal. The clinical observation was that the numbness gradually disappeared after surgery in most cases.
TSP and hallux abducto valgus
The metatarsal‐sesamoid system plays a vital role in the development of hallux abducto valgus. When hallux abducto valgus occurs and progresses, it results in imbalance of the appendicular muscles of the metatarsal‐sesamoid system, which leads to varus of the first metatarsal and subluxation of the sesamoid 5 . In the treatment of hallux abducto valgus, good recovery of the TSP leads to rebalancing of the soft tissue of the metatarsal‐sesamoid system, resulting in a lower recurrence rate and better clinical effect 2 . The TSP should be regarded as critical evidence in evaluation of the therapeutic effect of surgery. In this group, the TSP was reduced from 4.29 ± 1.06 to 3.07 ± 0.95 postoperatively, which is similar to the results reported by Trnka et al. 6 The position of the sesamoid also recovered in the majority of cases. This could be one of the reasons that the long‐term results were good and the recurrence rate low.
Shortening of the first metatarsal and metatarsalgia
Shortening of the first metatarsal with less load postoperatively is regarded as the main factor leading to aggravation of metatarsalgia 7 , 8 . Currently, no conclusion has been made on the degree of shortening of the first metatarsal that leads to occurrence of metatarsalgia. Turnbull and Grange observed a group of cases after surgery on hallux abducto valgus 9 . The first metatarsal bone was shortened by 0.8 cm on average and no metatarsalgia developed. They therefore suggested that shortening of the first metatarsal does not lead to lateral metatarsalgia. However, Tóth et al. measured 250 cases who underwent the Wilson operation 7 . In these patients, the first metatarsal was shortened by 0.38 cm on average and the degree of shortening was positively related to occurrence of pain. The mean shortening of the first metatarsal was 0.2 cm and the proportion of no pain or relief of pain was 91.8% (89/97). No relief and aggregation of pain occurred in 8.2% of their cases (8/97), which was higher than others have reported 6 , 10 .
A negative correlation was found between the extent of plantar movement and plantar flexion of the distal end of metatarsal bone after osteotomy and the vertex angle of the medial longitudinal arch of feet. That is, adequate plantar movement and plantar flexion of the distal end of the metatarsal can reduce the vertex angle of the medial longitudinal arch of the foot, compensating for the reduction in height of the medial longitudinal arch caused by shortening of the metatarsal, and preventing metatarsalgia 11 . In order to avoid over‐shortening of the first metatarsal bone, minimal incision osteotomy should be conducted once only and repetition of osteotomy avoided. The angle between the osteotomy line and axis of metatarsal on the horizontal plan should be < 30o, otherwise plantar movement and plantar flexion of the distal end of the metatarsal and its accessory structures can result bearing a greater load. The measures mentioned may be the reason for the incidence rate of metatarsalgia being low in this group.
Evaluation of the postoperative effect of surgery for hallux abducto valgus
Evaluation of the postoperative therapeutic effect of surgery for hallux abducto valgus includes not only the appearance of the feet, but also improvement in symptoms and function of the joint. However, these two aspects rarely correlate with each other and that makes evaluation difficult. Mann and Pfeffinger report that, in severe cases of hallux abducto valgus, there is a huge gap between satisfactory rectification of the structural problems, improvement in symptoms and patient satisfaction 12 . The observations of the present authors are the same. Evaluation of the therapeutic effect of surgery on hallux abducto valgus should include not only the appearance of the feet and relevant angle rectification, but also symptom alleviation and functional recovery. X‐ray films are not critical to evaluation of the therapeutic effect, which is also evident from the scoring table for hallux‐metatarsophalangeal‐interdigital of the AOFAS. The surgical technique for severe hallux abducto valgus should be formulated in accordance with the requirements of the patient and individual features of the case. The surgeon should not pay too much attention to rectifying the deformity completely back to normal, but rather should focus on symptom alleviation. Slight postoperative hallux abducto valgus deformity is acceptable. Complete rectification of deformity may require a complicated method and longer surgical time, as well as subsequent damage due to surgery. Although minimal incision osteotomy for hallux abducto valgus with osteotomy of the metatarsal neck is inadequate for rectifying severe deformity, it often achieves a more satisfactory outcome in elderly patients who have high requirements for symptom alleviation but not appearance, because it is a simple method, with a short operative time and is easy to tolerate.
In conclusion, minimal incision osteotomy is a simple method with less complications and positive long‐term therapeutic effect. It is a good and reliable surgical method for hallux abducto valgus.
Disclosure
This research did not involve any personal relationships with other person or organizations that might pose potential conflicts of interest or bias the findings.
Acknowledgments
This study was supported by the National Nature Science Foundational of China (project number: 30772815) and China Academy of Chinese Medical Sciences (project number: CACMS05Y‐0028).
References
- 1. Wen JM, Sang ZC, Lin XX, et al Clinical study of hallux valgus treated by minimal incision and manipulations (Chin). Zhongguo Jiao Jing Wai Ke Za Zhi, 2002, 9: 26–29. [Google Scholar]
- 2. Wen JM, Zhang LR, Weng CH, et al Minimal incision refitting osteotomy to treat recurrent hallux abducto valgus deformity(Chin). Zhonghua Gu Ke Za Zhi, 2001, 21: 143–144. [Google Scholar]
- 3. Gui JC, Gu XJ, Shen HQ, et al First metatarsal‐sesamoid system and hallux abducto valgus (Chin). Zhonghua Gu Ke Za Zhi, 2001, 21: 537–540. [Google Scholar]
- 4. Kitaoka HB, Alexander IJ, Adelaar RS, et al Clinical rating systems for the ankle‐hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int, 1994, 15: 349–353. [DOI] [PubMed] [Google Scholar]
- 5. Ma X, Gu XJ, Chen JS, et al Three dimensional morphological study of the foot transverse arch between normal and hallux abducto valgus foot (Chin). Zhonghua Gu Ke Za Zhi, 1998, 18: 274–277. [Google Scholar]
- 6. Trnka HJ, Mühlbauer M, Zembsch A, et al Basal closing wedge osteotomy for correction of hallux valgus and metatarsus primus varus: 10‐ to 22‐year follow‐up. Foot Ankle Int, 1999, 20: 171–177. [DOI] [PubMed] [Google Scholar]
- 7. Tóth K, Huszanyik I, Kellermann P, et al The effect of first ray shortening in the development of metatarsalgia in the second through fourth rays after metatarsal osteotomy. Foot Ankle Int, 2007, 28: 61–63. [DOI] [PubMed] [Google Scholar]
- 8. Jung HG, Zaret DI, Parks BG, et al Effect of first metatarsal shortening and dorsiflexion osteotomies on forefoot plantar pressure in a cadaver model. Foot Ankle Int, 2005, 26: 748–753. [DOI] [PubMed] [Google Scholar]
- 9. Turnbull T, Grange W. A comparison of Keller's arthroplasty and distal metatarsal osteotomy in the treatment of adult hallux valgus. J Bone Joint Surg Br, 1986, 68: 132–137. [DOI] [PubMed] [Google Scholar]
- 10. Dermon A, Tilkeridis C, Lyras D, et al Long‐term results of Mitchell's procedure for hallux valgus deformity: a 5‐ to 20‐year follow‐up in 204 cases. Foot Ankle Int, 2009, 30: 16–20. [DOI] [PubMed] [Google Scholar]
- 11. Dai HL, Wen JM, Hu HW, et al Relationship among callosities metatarsalgia apex angle of indulging arcus and plantar flexion (shifting) of distal end of metatarsal bone block after minimal incision treatment for hallux valgus (Chin). Zhongguo Gu Yu Guan Jie Sun Shang Za Zhi, 2008, 23: 549–551. [Google Scholar]
- 12. Mann RA, Pfeffinger L. Hallux valgus repair. DuVries modified McBride procedure. Clin Orthop Relat Res, 1991, 272: 213–218. [PubMed] [Google Scholar]


