Abstract
Objective: To investigate the diagnosis and surgical treatment of excessive lateral pressure syndrome of the patellofemoral joint caused by military training.
Methods: Fifteen patients (patient group) and 18 healthy volunteers (control group) were involved in this retrospective study. Radiographs of the knee joints of all patients and volunteers were taken. The bone architecture was assessed, the trochlear angle, coincidence angle and patellofemoral joint index measured in both groups, and the resulting data compared. All 15 patients (17 knees) were treated by lateral collateral retinaculum release. Pre‐ and post‐operative pain was evaluated with a visual analog scale (VAS).
Results: The differences between the two groups in coincidence angle (patient group: 7.67°± 5.81°; control group: −2.2°±−2.71°) and patellofemoral joint index (patient group: 2.49 ± 1.40; control group: 1.25 ± 0.15) were statistically significant. Subchondral bone sclerosis and osteophytosis in the patellofemoral joint were more pronounced in the patient group than in the control group. The VAS was higher preoperatively (7.06 ± 0.85) than postoperatively (6 months postoperatively: 3.87 ± 0.24; 1 year postoperatively: 3.01 ± 0.17), and the differences between preoperative and postoperative were statistically significant.
Conclusions: Apart from the case history, typical symptoms and physical signs, X‐ray examination is the most basic way to diagnose excessive lateral pressure syndrome of the patellofemoral joint, and the patellofemoral joint index is the most reliable for diagnosis. Lateral collateral retinaculum release with a small‐incision is an effective treatment for this disease.
Keywords: Knee joint, Military science, Pain, Patellofemoral joint
Introduction
It is common for young and middle‐aged soldiers to complain about persistent swelling and pain in their knee joints, and “soft leg” symptom also occurs occasionally in this group. Clinically, these patients are usually misdiagnosed as traumatic synovitis or meniscus injury, and therefore treatment has not been effective. In fact, the correct diagnosis is excessive lateral pressure syndrome of the patellofemoral joint. In order to investigate the diagnosis and treatment of this syndrome, which is caused by military training, we collected and analyzed data from 15 patients hospitalized in our institute from May 2006 to May 2008, and compared it with that from 18 normal volunteers.
Materials and Methods
General information
The group of 15 patients (17 knees) was composed of 12 men (14 knees) and 3 women (3 knees). Their ages ranged from 22 to 43 years old with an average age of 27.3 years. All patients had participated in intense military training and sustained varying degrees of knee injuries. The interval between onset of symptoms and attendance at our clinic was averaged 3.7 years. The pain in the patients' knees all occurred in their patellofemoral joints and was accompanied by slight swelling. The pain intensified when the patients bent their knees while carrying a weight. Though some patients had “soft leg” symptoms, the McMurray sign was negative and there were no obvious signs of quadriceps femoris atrophy. All patients had received standard conservative treatments such as non‐steroidal anti‐inflammatory drugs (NSAIDs) and quadriceps femoris exercises, but the results were poor, and eventually surgery was performed on all of them. In addition, we selected 18 normal, healthy volunteers of similar age and gender as a control group. All subjects in this research were soldiers on active duty.
Imaging examination
Anteroposterior, lateral and patella axial X‐ray films were taken of the 17 injured knees of the 15 people in the patient group. Unilateral knee joints of the 18 volunteers in the control group were chosen randomly for the same X‐ray examination. The changes in bone architecture shown on these X‐ray films, such as subchondral bone sclerosis and osteophytosis at the lateral edge of the patellofemoral joint, were assessed. In addition the following indices were measured: trochlear angle (Fig. 1), coincidence angle (Fig. 1), and patellofemoral joint index (Fig. 2).
Figure 1.
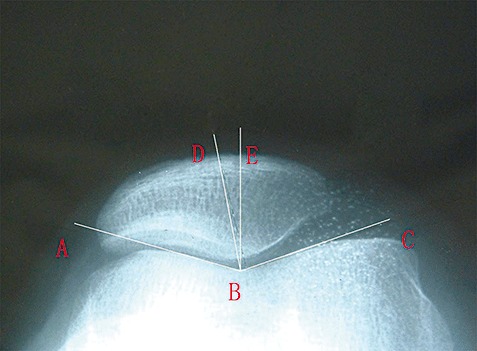
Trochlear angle and coincidence angle. The trochlear angle 1 , 2 : on an X‐ray film of the patellar axis, the trochlear angle is formed by the combination of two lines. The first line (AB) runs from the highest point of the inner side of the angle of the thighbone to the thighbone trochlea; the other one (BC) runs from the highest point on the outer side of the angle of the thighbone to the thighbone trochlea, thus angle ABC is the trochlear angle. Coincidence angle 1 , 2 : this is formed by drawing the bisector BE of the trochlear angle, and then drawing a line BD from the vertex of the trochlear angle to the lowest point of the patellar ridge, thus angle DBE is the coincidence angle. If the lowest point of patellar ridge falls outside the bisector, the coincidence angle is positive; if not, it is negative. The coincidence angle shows the relationship between the patella and the thighbone trochlea.
Figure 2.
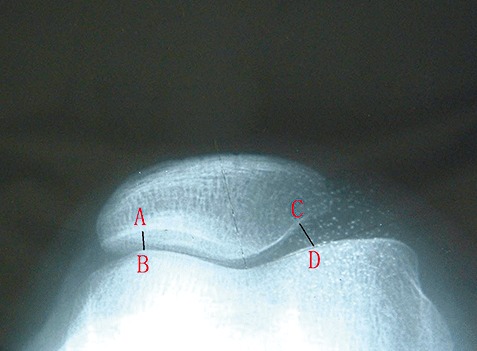
Patellofemoral joint index. Patellofemoral joint index 1 , 3 : the ratio of the lengths of the medial interspace (CD) and lateral interspace (AB) of the patellar joint (i.e. CD/AB). Normally, the medial interspace of the patella joint is bigger than the lateral interspace. An increase in the patellofemoral joint index means that the medial interspace of the patellar joint gets wider, and this shows that the patella is inclining outward.
Surgical treatment
Under lumbar anesthesia, all patients underwent surgical release of the lateral collateral retinaculum of the affected knee through a small incision. First, a pneumatic tourniquet was tied around the top of the thigh, and a 2cm longitudinal skin incision made on the outer and upper edge of the patella. Then, through this incision, the subcutaneous tissue above the lateral collateral retinaculum was dissected with hemostatic forceps; a 2 to 3 cm longitudinal cut was made in the retinaculum on the outer and upper edge of the patella with an electrotome; then a knife holder with a No.12 sickle‐shaped blade was used to enter the patellofemoral joint cavity along the incision in the lateral collateral retinaculum right above the lateral edge of the patella and to cut upwards to release the lateral collateral retinaculum. The release extended a little beyond the upper and lower edges of the patella such that the patella could easily be pushed inwards afterwards; care was taken not to sever the tendon of vastus lateralis lest the patella be dislocated inwards as a result of over‐release 4 . Finally, a drainage tube was inserted after loosening the pneumatic tourniquet, and the knee joint was dressed with a pressure bandage after suturing the skin incision.
Postoperative management
Quadriceps femoris exercises under supervision were encouraged on the first postoperative day. Three days after the operation, the dressing was changed and continuous passive movement exercises for the knee were added. Two weeks later, the stitches were taken out and the patients encouraged to walk with crutches.
Pain evaluation
The pain in the patients' knees was evaluated with visual analogue scales (VAS) at the following points: pre‐operatively, and six and twelve month postoperatively.
Statistical analysis
The trochlear angle, coincidence angle, and patellofemoral joint index of the knee joints in both groups were compared with Student's t‐test, and P‐values <0.05 was considered statistically significant. Changes in bone architecture in both groups were statistically analyzed with “Fisher's exact test”, and P‐values <0.01 were considered statistically significant. The VAS before and after surgery was statistically analyzed with Student's t‐test, and differences were considered significant at P < 0.05.
Results
Image parameters
The differences between the two groups in coincidence angle and patellofemoral joint index were statistically significant (Table 1). No loose body was seen on the X‐ray films of any of the knee joints. Subchondral bone sclerosis and osteophytosis in the patellofemoral joint were more pronounced in the patient group than in the control group (Table 2, Fig. 3).
Table 1.
Comparison between patient and control groups of image variables of the knee joint
| Groups | N | Trochlear angle | Coincidence angle | Patellofemoral joint index |
|---|---|---|---|---|
| Patient group | 15 cases (17 knees) | 132.44°± 10.21° | 7.67°± 5.81° | 2.49 ± 1.40 |
| Control group | 18 cases (18 knees) | 136.8°± 4.87° | −2.2°±−2.71° | 1.25 ± 0.15 |
| t | — | 0.887 | 4.318 | 2.633 |
| P | — | 0.392 | 0.001 | 0.030 |
Table 2.
Comparison between the two groups of bone architecture changes in the knee joint on X‐ray films
| Groups | n | Subchondral bone sclerosis | Osteophytosis |
|---|---|---|---|
| Patient group | 15 case (17 knees) | 9 (knees) | 13 (knees) |
| Control group | 18 case (18 knees) | 2 (knees) | 3 (knees) |
| P | — | 0.012 | 0.001 |
Figure 3.

X‐ray film of the knee joint of one patient. Subchondral bone sclerosis and osteophytosis at the lateral edge of the patellofemoral joint can be seen.
Pain score
The preoperative VAS (7.06 ± 0.85) was higher than that postoperatively (6 months postoperatively: 3.87 ± 0.24; 1 year postoperatively: 3.01 ± 0.17), and the differences between preoperative and 6 months postoperatively and 1 year postoperatively were statistically significant (t= 13.988, P=0.000; t= 18.085, P=0.000, respectively).
Discussion
Excessive lateral pressure syndrome of the patellofemoral joint is one of the common causes of pain in the knee joint, the pain characteristically being vague and difficult to locate. The pain often intensifies after activities which put extra pressure on the knee joints, such as climbing stairs, crouching or bending the knees for a long time. According to some scholars, it is overload on the lateral articular facet of the patella and excessive exterior stretching that causes knee pain in patients with excessive lateral pressure syndrome of the patellofemoral joint. Overload on the subchondral bone induced by a conduction abnormality of patellofemoral joint load is the main source of pain in the patellofemoral joint 5 . Factors which can cause excessive lateral pressure syndrome of the patellofemoral joint are either congenital or postnatal. Abnormal growth of the patella, such as trochlea shallow patella inclining exteriorly, or enlargement of the Q angle 6 , 7 , are congenital factors. Disorders of the patellofemoral joint can result in premature excessive lateral pressure syndrome of the patellofemoral joint and cause pain in it. Acquired factors, such as tension of the lateral collateral retinaculum caused by injury or overfatigue 6 , 7 and muscle force imbalance of the vastus medialis and vastus lateralis, can result in the patella inclining outwards, osteophytosis in the lateral edge of the trochlea and/or patella and subchondral bone sclerosis.
The disorders in this group of patients are all related to injuries and over‐fatigue sustained during military training and have a relatively long history. The disorders were initiated by direct force on, or sprain of, knee joints, but the degree of disorder was not necessarily determined by the severity of the injury. These patients often complained that their affected knees were continuous swollen and painful, especially after intense military training, and in some cases they could barely support their body weight. Thus the disorder is easily diagnosed as traumatic synovitis in the knee joint or meniscus injury. Clinically, traumatic synovitis often has a relatively short history of swelling and pain in the knee joints after injuries or intense exercise, an obviously swollen joint and a positive floating patella test without definite changes on X‐ray films, obvious heightening of tension in the lateral collateral retinaculum and patellar tenderness. Patients with meniscus injury usually have an obvious history of forcibly twisting their knee joints; the McMurray sign test is positive; most of them also suffer from trick knees, and those with a longer history of such illness may have muscular atrophy of their quadriceps femoris. However, in this study, most patients experienced pain in their patellofemoral joints, swelling of the knee joint was seldom seen, and the floating patella test and McMurray sign test were both negative. Moreover, there was no obvious muscular atrophy of the quadriceps femoris, and signs like tangible thickening in the lateral collateral retinaculum, increase of tension and decrease of the inward degree of excursion of the patella were often seen. The degree of pain in the patellofemoral joints was not increased when commencing the McMurray test, but the semi‐squat test, which increases the load when bending the knee, could cause or intensify pain in the patellofemoral joints. Inability of the legs to bear the body weight may be caused by functional restriction of the quadriceps femoris, which is a consequence of the pain.
X‐ray examination of the knee joint is an important adjunctive measure in the diagnosis of excessive lateral pressure syndrome of the patellofemoral joint. The patellofemoral joint index is the angle of outward inclination of the patella; the coincidence angle is the angle of outward movement of the patella; and the trochlear angle expresses any abnormal dysplasia of the trochlea groove 8 . According to some foreign scholars, patients with excessive lateral pressure syndrome of the patellofemoral joint often have changes in indices like the coincidence angle and patellofemoral index. However, because of ethnic differences in the morphology of knee joints, there are major differences in their biodynamic features. The diagnostic standards for X‐ray films of people of other ethnicities do not fit Chinese patients. Our research collected variables and indices from X‐ray films of Chinese patients' knee joints, which makes the findings more applicable to other Chinese patients. Our research revealed that there was no statistically significant difference between the patient and control groups in the trochlear angle, whereas between these two groups differences in coincidence angle and patellofemoral index were statistically significant. That is, the degrees to which the patella inclines or moves outwards was significantly greater in the patient group than in the control group. Meanwhile, subchondral bone sclerosis and osteophytosis at the lateral edge of the patellofemoral joint in the patient group were more pronounced than in the control group. Therefore, in addition to paying attention to the typical clinical symptoms and physical sign of patients, X‐ray examination is essential for the diagnosis of excessive lateral pressure syndrome of the patellofemoral joint. Of all the data revealed by X‐ray examination, the patellofemoral index is relatively easy to measure and to use in assessing how severely the patella inclines outwards. In comparison, the coincidence angle and trochlear angle are relatively complex to measure and interpret. All of these variables need to be measured with great caution, so as not to make errors. Therefore they are not easy to implement widely in clinical practice. These two indices can be used to exclude the possibility of congenital dysplasia of the patellofemoral joint. On lateral and axial X‐ray films, any evidence of osteophytosis at the lateral edge of the patella and trochlear or subchondral bone sclerosis should be specially evaluated. Anteroposterior and lateral X‐ray films can also reveal whether there are any loose bodies.
Conservative treatments for excessive lateral pressure syndrome of the patellofemoral joint include NSAIDs, physiotherapy and quadriceps femoris exercises. Medical treatment and physiotherapy can alleviate local pain and swelling. In regard to the quadriceps femoris exercises, it is common and useful to straighten and raise the leg; however, it is more efficacious to strengthen the vastus medialis 9 , because this can rectify the imbalance between the vastus medialis and vastus lateralis. If conservative treatments are not as efficacious as expected, lateral collateral retinaculum release can be considered and performed, but the indications for surgery should be carefully assessed 10 . Lateral collateral retinaculum release is applicable in patients with distinct pain in the patellofemoral joints or thickening of the lateral collateral retinaculum with normal joint cartilage. In this study, conservative treatments were ineffective in all patients, and lateral collateral retinaculum release through a small incision was performed on them, resulting in relief of their knee pain. This operation involves minimal trauma and disruption of the knee joints. In the early stages, knee joint exercises are helpful in normalizing knee function. We believe that over‐release can dislocate the patella inwards, to prevent this the extent of release should be a little longer than the upper and lower edge of the patella and the tendon of vastus lateralis should not be severed. During the operation, the retinaculum on the outer and the upper edge of patella is incised longitudinally for 2 to 3 cm with an electrotome, after which the external upper artery of the knee can be electrocoagulated, and the knee joint bandaged with a thick pressure dressing for three days in order to prevent hematoma formation. Knee joint exercises in the early stage can prevent e formation of scar tissue on the released part of the lateral collateral retinaculum; meanwhile, it is necessary to continue the quadriceps femoris exercises, which are of vital importance in normalization of knee joint function and prevention of recurrence of symptoms.
The X‐ray examinations described in this research definitely require high quality X‐ray films, especially for the axis position films. Angle measurement is relatively complex, and for this X‐ray films are less convenient than knee joint CT scans. However, the advantages of X‐ray examination are that it is simple, effective and relatively cheap. Thus it is more easily widely adopted by basic‐level hospitals. Needless to say, these patients can be operated on by arthroscopy 11 , but this requires multiple pieces of expensive equipment. In conclusion, when diagnosing excessive lateral pressure syndrome of the patellofemoral joint caused by military training, it is vital to combine the patient's history with typical clinical symptoms, physical sign and outcomes of X‐ray examination. Otherwise there is a high risk of misdiagnosis and accordingly, of mistreatment. The number of subjects in this research is still insufficient and more cases need to be studied.
Disclosure
No funds were received in support of this work, and there are no competing interests in this research.
References
- 1. Lv HS. Surgery of the Knee, 3rd edn. Beijing: People Medicine Publishing House, 2006; 894, 897, 911–912. [Google Scholar]
- 2. Merchant AC, Mercer RL, Jacobsen RH, et al Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am, 1974, 56: 1391–1396. [PubMed] [Google Scholar]
- 3. Laurin CA, Dussault R, Levesque HP. The tangential X‐ray investigation of the patellofemoral joint: X‐ray technique, diagnostic criteria and their interpretation. Clin Orthop Relat Res, 1979, 144: 16–26. [PubMed] [Google Scholar]
- 4. Hughston JC, Flandry F, Brinker MR, et al Surgical correction of medial subluxation of the patella. Am J Sports Med, 1996, 24: 486–491. [DOI] [PubMed] [Google Scholar]
- 5. Merchant AC. Classification of patellofemoral disorders. Arthroscopy, 1988, 4: 235–240. [DOI] [PubMed] [Google Scholar]
- 6. Fulkerson JP, Hungerford DS. Patellar tilt/compression and the excessive lateral pressure syndrome (ELPS) In: Fulkerson JP, Hungerford DS, eds. Disorders of the Patellofemoral Joint. Baltimore: Williams and Wilkins, 1990; 102–123. [Google Scholar]
- 7. Ye TJ, Zhang XL, Hao S, et al Operative treatment of patellofemoral osteoarthritis (Chin). Guowai Yi Xue Fen Ce(Orthopaedics), 2005, 5: 308–309. [Google Scholar]
- 8. Ma W, Dong TH, Yao FR, et al The diagnosis for the malalignment of the patella of the patellofemoral joint by axial X‐ray with the knee flexing at 15° (Chin). Zhonghua Gu Ke Za Zhi, 2003, 23: 228–229. [Google Scholar]
- 9. McConnell J. The management of chondromalacia patellae: a long‐term solution. Aust J Physiother, 1986, 32: 215–223. [DOI] [PubMed] [Google Scholar]
- 10. Li QY, Lin J, Qiu GX, et al The middle and long term clinical results of patellofemoral arthroplasty for severe patellofemoral osteoarthritis (Chin). Zhonghua Gu Ke Za Zhi, 2010, 30: 541–542. [Google Scholar]
- 11. Zhang J, Wang Y, Hou XK, et al The effect of bipolar radiofrequency technique in the treatment of patellofemoral malalignment (Chin). Zhonghua Gu Ke Za Zhi, 2005, 25: 641–646. [Google Scholar]


