Abstract
Objective: To evaluate the feasibility and clinical efficacy of bilateral decompression via unilateral fenestration (BDUF) with mobile microendoscopic discectomy (MMED) for lumbar spinal stenosis.
Methods: From June 2007 to June 2009, 32 patients were treated by the technique of BDUF with MMED for lumbar spinal stenosis in our hospital. All patients complained of bilateral sciatic neuralgia and intermittent claudication that was dominant in one limb. CT scan and MRI revealed disc herniation and bilateral stenosis of the spinal canal. Patients with bilateral severe osseous stenosis and multilevel stenosis were excluded.
Results: The procedure was technically successful in all patients, bilateral decompression and spinal canal enlargement being achieved by unilateral fenestration. The mean operative time was 70 min (range, 50–100 min), with a mean blood loss of 150 ml (range, 50–350 ml). No significant complication was noted; dural tears were encountered in only two patients without obvious side effects. The patients were followed up for 3 to 24 months (mean, 12 months) and the clinical results were excellent in 21 cases and good in 11 cases according to the MacNab scale.
Conclusion: The procedure of BDUF can be performed in conjunction with the MMED technique for lumbar spinal stenosis with good clinical results; however, severe bilateral osseous stenosis may be not suitable for this technique.
Keywords: Endoscopy, Intervertebral disk displacement, Lumbar vertebrae
Introduction
Microendoscopic discectomy (MED), with its smaller blood loss and faster recovery, has become a popular procedure for lumbar disc herniation and lumbar spinal stenosis 1 . However, bilateral stenosis is common in patients with lumbar spinal stenosis. With the advancement of the MED technique, bilateral decompression via unilateral fenestration (BDUF) can be completed via a unilateral approach with preservation of contralateral structures such as the lamina, the facet and the paraspinal muscle. Biomechanics experiments have proved that the stability of BDUF is superior to that of bilateral fenestration 2 . In addition, the mobile microendoscopic discectomy (MMED) technique can more consistently achieve sufficient decompression. 3
Materials and methods
Case data
From June 2007 to June 2009, 32 patients with lumbar spinal stenosis were treated by BDUF using the MMED technique. They included 14 men and 18 women, with a mean age of 65 years (range, 56–74 years). All patients complained of bilateral sciatic neuralgia and intermittent claudication that was dominant in one limb. The course of disease ranged from 3 months to 6 years with a mean of 0.9 years. Preoperative CT scans and MRI revealed disc herniation and bilateral canal stenosis which were in accordance with the clinical presentations. Twenty‐five patients had stenosis at one level and seven at two.
Instruments of MMED
The mobile microendoscopic system (Endospine, Karl Storz, Tuttlingen, Germany) is movable, that is, the cone‐shaped operating tube and working insert are not fixed to the operation table and can remain erect and well‐balanced in the operative field. The working insert has three channels: an 8 mm working channel, a 4 mm suction channel, and a 4 mm telescope channel, and an adjustable nerve retractor in the medial groove (1, 2). There is an angle of 12° between the working channel and the telescope channel, and the telescope, being at 0°, is closer to the surgical field than that of the Medtronic METRX MED system (Medtronic, Sofamor Danek, Memphis, TN, USA). During surgery the operating tube and working insert can be moved and adjusted by surgical instruments and/or suction, resulting in spontaneous movement of surgical vision and field, which is convenient for accessing the decompression field.
Figure 1.

The cone‐shaped operating tube and working insert showing its three channels.
Figure 2.

The operating tube and working insert can be moved and adjusted by surgical instruments and/or suction.
Surgical technique
The procedure was carried out under general anaesthesia with the patients in the prone position. The intervertebral space affected by stenosis was located with a special localizing device under C‐arm fluoroscopy. A 2 cm‐incision was made beside the spinous process on the side of dominant symptoms. Sharp incision of the fascia and subcutaneous tissue was performed, bipolar coagulation being used for hemostasis. The scissors were inserted beside the spinous process in the direction of the disc space and the paraspinal muscle distracted. A 12‐mm chisel was used to dissect the paraspinal muscle from the lamina. A small roll of gauze with suture was slipped proximally to turn back the paraspinal muscles and the operating tube installed with an obturator. Then the obturator was removed and the soft tissue in the operating tube was cleaned out under direct vision with a rongeur. Thus the inferior border of the upper lamina and the medial margin of the articular process were exposed, as well as the interlaminar space and ligament flavum. Next the working insert was installed into the operating tube and the direction of endoscopic vision adjusted according to the patient's requirements direction.
The inferior border of the upper lamina and the medial margin of the articular process were resected until the attachment of the ligament flavum had been exposed. In cases of severe hyperplasia, a high speed burr was used. The ligament flavum was removed with a Kerrisson rongeur and the dural sac exposed. Once the nerve root had been exposed beside the dural sac, decompression was performed along it until the superior border of lower lamina had been reached. Then an enlarged fenestration was completed by partial laminotomy. The dural sac and nerve root were protected with cotton or a nerve retractor and the disc exposed. Discectomy, including removal of any fragmented nucleus in the intervertebral space, was performed with a rongeur, after that the disc space was rinsed with saline water using a special irrigator.
After sufficient decompression had been achieved ipsilaterally, two wads of cotton were inserted under the base of the spinous process in both cephalad and caudal directions to protect the dural theca. Then the fundus of the spinous process was resected with a Kerrisson rongeur or high‐speed burr, and a working space was made between the dural theca and the contralateral lamina. Meanwhile, the operating tube was tilted to the opposite side, exposing the contralateral canal clearly under endoscopic vision. Then the contralateral ligament flavum and the inferior part of proximal lamina were undercut with a Kerrisson ronguer until the contralateral nerve root had been released (3, 4). After contralateral decompression, the field was rinsed, and the wads of cotton removed.Bleeding from the venous plexus was controlled by bipolar coagulation. The operating tube and small roll of gauze were removed, suction inserted routinely and the incision closed.
Figure 3.
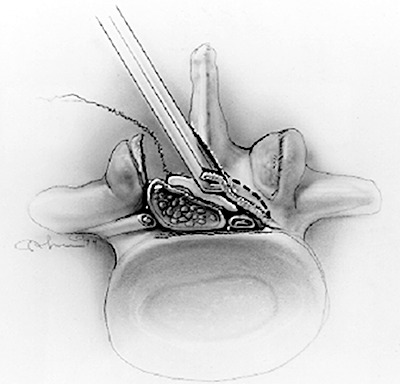
The contralateral ligament flavum and lamina are undercut with a Kerrison rongeur while the dural sac is protected by wads of cotton.
Figure 4.
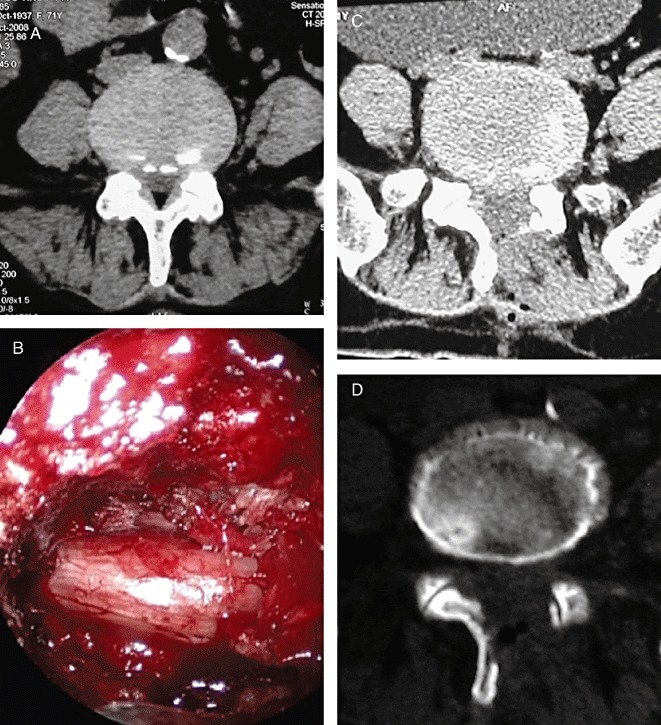
A. 72‐year‐old woman with L4,5 bilateral stenosis, her symptoms were completely resolved after BDUF with MMED. A. Preoperative CT scan revealing bilateral stenosis. B. Intraoperative endoscopic vision showing the contralateral nerve root after bilateral decompression. C, D. Postoperative CT scans revealing bilateral decompression and enlargement of the canal and intact contralateral structure.
Postoperative management
The patients were allowed to walk 48 h after the suction had been removed. Patients were rechecked as outpatients at 3 months, 6 months and every year. The clinical results were evaluated according to the scale of MacNab, (i.e. excellent: the symptom has completely disappeared and the patient is able to return to their original work and activities; good: occasional pain, capable of light work; fair: symptoms partially resolved with persistent pain, not capable of work; poor: nerve root pain, requiring further surgery) 4 .
Results
The procedure was technically successful in all patients, bilateral nerve decompression and spinal canal enlargement being achieved by unilateral fenestration. No significant complication was noted; a dural theca tear was encountered in only two patients without obvious side‐effects. The mean operative time was 70 min (range, 50–100 min), with a mean blood loss of 150 ml (range, 50–350 ml).
The postoperative CT scans revealed bilateral enlargement of the spinal canal with sufficient decompression, and confirmed that contralateral structures, such as laminae, facets and paraspinal muscles, were intact (Fig. 4).
Postoperatively the mean hospital stay was 7 days (range, 5–12 days), without limitation of activities. The patients were followed up for 3–24 months (mean, 12 months) and the clinical results were excellent in 21 cases and good in 11 according to the MacNab scale.
Discussion
Lumbar spinal stenosis, which is usually caused by degeneration and hyperplasia of the intervertebral structures, such as protrusion and bulging of the disc, thickening of the ligament flavum, and hyperplasia of the zygapophysial joints and laminae is very common in clinical practice. Such stenosis occurs mainly at the level of the intervertebral space (i.e. the disc and interlaminar space, mainly involving the disc, ligament flavum, and articular process) and rarely at the pedicle level. Surgical management of lumbar spinal stenosis has in the past included total laminectomy and semi‐laminectomy; however removal of the posterior vertebral arc can result in many complications, such as iatrogenic instability, epidural scar adhesion, and lumbar failure syndrome. In recent years, pedicle instrumentation has been widely used to prevent the iatrogenic instability which can be caused by laminectomy. However this procedure requires wider dissection of the paraspinal muscles, and carries an increased risk of complications related to the internal implant, as well as of accelerated degeneration of the adjacent segment.
Nowadays, it is advocated that decompression be achieved by limited surgery which targets only the stenosis; for example, just the disc, ligament flavum, and medial part of the zygapophysial joints may be resected, preserving the normal structure. With development of the MED technique, its indications have evolved from disc herniation to lumbar stenosis 1 , 3 . Lumbar spinal stenosis often involves the canal bilaterally, symptoms being dominant on one side. With the MED technique, the stenosis is often decompressed via a bilateral approach, which of course increases operation time and blood loss. Therefore the technique of BDUF was suggested in order to decrease the complexity of the procedure and preserve the contralateral structure. A biomechanical experiment performed by Hamasaki et al. confirmed that BDUF preserves 80% of preoperative stability and is superior to bilateral fenestration 2 . Many other researcher have also reported that sufficient contralateral decompression can be completed with BDUF, especially for moderate degenerative stenosis 5 , 6 , 7 .
Because the commonly used METRX MED system is attached to the operating table, the field of vision is fixed. In addition manipulation of the instruments is constrained by the fixed working tube. The instruments, sharing as they do a common tube, can obstruct each other, often making it difficult to decompress the canal, especially in patients with obvious hyperplasia. The mobile MED (MMED) system has effectively overcome these limitations. Both the operating tube and the visual field can be moved by surgical instruments and/or suction as needed, and manipulation of the instruments is not constrained by the working tube, making it easier to decompress the canal.
In our practice, BDUF has been performed in conjunction with the MMED technique for lumbar spinal stenosis. First, the ipsilateral canal was sufficiently decompressed with enlarged fenestration as well as discectomy. Then the dural theca was protected with two wads of cotton and the fundus of the spinal process resected, thus creating a working space between the dural theca and the contralateral lamina. Meanwhile, the operating tube was tilted toward the opposite side and the contralateral canal clearly exposed by endoscopy. Then the contralateral ligament flavum and partial lamina were undercut with a Kerrison rongeur until the contralateral nerve root was released. Because the telescope is movable and close to the surgical field, it could be installed at the fenestration site. Through the space between the dural theca and the contralateral lamina the contralateral canal was then exposed, as clearly as if the opposite canal was being directly visualized. The BDUF was performed in conjunction with the MMED technique in our 32 patients, with a mean operative time of 70 min and mean blood loss of 150 ml. The patients were allowed out‐of‐bed activities within 1–3 days of surgery and excellent or good results were observed in all patients during follow‐up.
However, some limitations of this technique were also revealed in our practice. Vision of the contralateral canal was limited such that, in most cases, only the originating part of the contralateral nerve root could be exposed and released. Accordingly contralateral decompression was generally confined to the central canal and entrance to the lateral canal. To prevent inadvertent nerve injury, generally only a Kerrisson rongeur was used to undercut the ligament flavum and inferior border of the upper lamina. In cases of severe bilateral osseous stenosis, contralateral decompression for hyperplasia of the zygapophysial joints might be difficult and bilateral fenestration is suggested. Therefore, this procedure is suitable for those patients with lumbar spinal stenosis who suffer bilateral sciatic neuralgia and intermittent claudication that is dominant in one limb. In addition, the stenosis should involve two or fewer levels, and the central canal and entrance to the lateral canal should be compromised mainly by the ligament flavum.
Disclosure
This manuscript does not contain information about medical device(s)/ drug(s). No funds were received in support of this work. No benefits of any type have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Xu BS, Destandau J, Xia Q, et al The mobile microendoscopic disectomy for lumbar disc herniation and stenosis (Chin). Zhonghua Gu Ke Za Zhi, 2009, 29: 112–116. [Google Scholar]
- 2. Hamasaki T, Tanaka N, Kim J, et al Biomechanical assessment of minimally invasive decompression for lumbar spinal canal stenosis: a cadaver study. J Spinal Disord Tech, 2009, 22: 486–491. [DOI] [PubMed] [Google Scholar]
- 3. Destandau J. A special device for endoscopic surgery of lumbar disc herniation. Neurol Res, 1999, 21: 39–42. [DOI] [PubMed] [Google Scholar]
- 4. MacNab I. Negative disc exploration. An analysis of the causes of nerve‐root involvement in sixty‐eight patients. J Bone Joint Surg Am, 1971, 53: 891–903. [PubMed] [Google Scholar]
- 5. Palmer S, Turner R, Palmer R. Bilateral decompression of lumbar spinal stenosis involving a unilateral approach with microscope and tubular retractor system. J Neurosurg, 2002, 97 (2 Suppl.): S213–S217. [DOI] [PubMed] [Google Scholar]
- 6. Ji YC, Kim YB, Hwang SN, et al Efficacy of unilateral laminectomy for bilateral decompression in elderly lumbar spinal stenosis. J Korean Neurosurg Soc, 2005, 37: 410–415. [Google Scholar]
- 7. Kim SW, Ju C, Kim CG, et al Minimally invasive lumbar spinal decompression: a comparative study between bilateral laminotomy and unilateral laminotomy for bilateral decompression. J Korean Neurosurg Soc, 2007, 42: 195–199. [Google Scholar]


