Abstract
Objective: To compare the immediate stability of different fixation techniques for the direct repair of spondylolytic defects in the pars interarticularis.
Methods: Eight fresh‐frozen and thawed calf cadaveric lumbar spines were used for mechanical testing. A modified Scott, screw‐rod‐hook, screw‐rod construct fixation and Buck techniques were applied to calf lumbar spines in which bilateral spondylolytic defects had been created in the L4 vertebra. The multidirectional flexibility of each specimen was measured under flexion/extension, right/left lateral bending, and right/left axial rotation.
Results: After creating a pars interarticularis defects at L4, the range of movement (ROM) at both the L3‐L4 and L4‐L5 levels were increased under all loading conditions. Each fixation technique significantly increased stability and almost restored intervertebral rotation mobility to normal levels. Under flexion‐extension, the screw‐rod‐hook and screw‐rod construct techniques of fixation provided more rotational stability than did the other two techniques (P < 0.05). The screw‐rod‐hook, screw‐rod construct and Buck techniques also provided more flexion/extension stability than the modified Scott technique.
Conclusion: The current study has shown that the ROM at the involved and upper adjacent level of spondylolysis is greater than in the intact spine. All four fixation techniques accorded with spinal biomechanical principles and restored intervertebral rotation displacements under flexion, rotation and bending loads to the intact condition. The screw‐rod‐hook and screw‐rod construct fixation techniques provided more stability than did the modified Scott and Buck techniques, and are therefore good prospects for direct repair.
Keywords: Biomechanics, Lumbar vertebrae, Spondylolysis
Introduction
Lumbar spondylolysis is not an infrequent finding, having been reported in approximately 6% of the adult population 1 . Meanwhile, it is a common cause of low back pain in children, adolescents and young adults 2 . For patients in whom conservative treatment has failed, surgery is the next available option. Posterior or posterolateral fusion of the involved segments has been considered to be the usual method of surgical treatment of spondylolysis. Unfortunately, this method results in a loss of movement at the fused level, and potentially increases movement of, and loading on, the adjacent segments, which can eventually lead to adjacent level arthrosis and symptomatic degeneration warranting additional surgery in 16.5% of patients at 5 years and 36.1% at 10 years 3 . Therefore, reconstruction of the pars interarticularis seems a logical and less aggressive approach for symptomatic patients who display no associated subluxation or degenerative disc diseases, as it provides consolidation of the isthmus, restoring the anatomy and stability of the spine and preserving its mobility 4 .
Since Buck first described the direct repair of isthmic defect by internal fixation 5 , several methods for stabilizing a lumbar pars defect have been described, including wires, hooks, and screw‐rod combinations. Several investigators have analyzed the clinical effectiveness of these systems. However, the primary focus of these studies has been to review the clinical results of each method, and few comprehensive biomechanical studies have been reported in detail.
Deguchi et al. only compared the biomechanical performance of some traditional fixation techniques, including the Scott, Buck, modified Scott and screw‐rod‐hook techniques, in calf vertebral L4‐L5 segments after L4 bilateral spondylolysis 6 . They found that fixation techniques could restore intervertebral rotational displacements under flexion and torsional loading to the intact condition, and that screw‐rod‐hook fixation allowed the least amount of movement across the defect during flexion. However, no comprehensive biomechanical comparison of those different fixation techniques in calf L3‐L4 and L4‐L5 simultaneously has been reported. Besides, some new fixation techniques have arisen for direct repair of spondylolysis 7 . So it is necessary to provide a biomechanical basis for the clinical application of these techniques.
Materials and methods
Eight lumbar spines were obtained from calf cadavers and frozen at −20°C until the day before testing. All specimens were examined by computerized tomography to exclude occult fracture or abnormality. The specimens were thawed at room temperature for 24 h and then the muscular tissue was stripped carefully to preserve the spinal ligaments and facet joint capsules. Bilateral 2‐mm‐wide spondylolytic defects were made in L4 using an oscillating saw. The L2 and L6 vertebrae were fixed with a polyester resin and the spines tested at L3‐4 and L4‐5 simultaneously.
Spinal structures were tested as follows: (i) intact spine; (ii) bilateral pars defects on the L4 laminae; (iii) modified Scott technique (wire loops with a tension of 150 N around a 4.5 mm cortical screw placed into both pedicles and tightened under the spinous process; (iv) screw‐rod‐hook technique (pedicle screws in L4 connected to upgoing sublaminar offset hooks placed at L4 across the defects with 150 Nm compression, [Texas Scottish Rite Hospital, Sofamor Danek, Memphis, TN, USA]); (v) screw‐rod construct fixation (pedicle screws in L4 connected to a rod folded into a ‘V’ under the spinous process (Sofamor Danek); and vi) Buck technique (4.0 mm cortical screws placed across the defect with manual compression) (Fig. 1).
Figure 1.

Six sequential states. (a) Intact specimen of calf lumbar spine. (b) Specimen with defects. (c) Specimen instrumented by the modified Scott technique. (d) Specimen instrumented by the screw‐rod‐hook technique. (E) Specimen instrumented by the screw‐rod construct technique. (F) Specimen instrumented by the Buck screw technique.
The biomechanical tests were performed by Spine 2000 (Southern Medical University, Guangzhou, China) with a specially designed bending grip (Fig. 2). The bending grip allows the application of pure unconstrained moments surrounding any axis in the transverse plane, along with a pure axial force and torques along and surrounding the longitude in the axis of the spine, and is governed by the basic materials tester. The Spine 2000 testing apparatus consists of mounting grips that allow sagittal rotation around the center of the two ends of the vertebral bodies. This system allows a constant bending moment to be applied uniformly over the length of the spine, resulting in a pure flexion and extension load, while maintaining axial load and zero axial torsional load. Separate nondestructive tests were performed for lateral flexion, flexion‐extension, axial torsion (10 Nm) without axial compression, and intervertebral rotation of the L3‐L4 and L4‐L5 mobile segments, and the results measured by Spine 2000.
Figure 2.

Spine 2000, made in the Southern Medical University of China, including computer driven scan and mounting plates. These allowed for pure moment application of sagittal and axial rotation. The scan was mounted anteriorly across the L3‐L4 and L4‐L5 intervertebral discs and measured sagittal and axial rotation. Six small tridimensional iron boxes were used in the transverse processes as marked for scanning in lateral bending and torsion, and three in flexion‐extension.
Each spine was ultimately fitted with all instrumentation systems. The tension in the spinal cables was determined using an atlas cable tensioning device. This device was also used to compress the screw‐rod‐hook system, using a compression cable. This ensured that each cable had uniform tension, and was tensioned symmetrically. The pedicle screws were placed lateral to the facet, entering the pedicle at the junction of the superior articular process and the midpoint of the pedicle. All through the destabilizing and restabilizing procedures, great care was taken to avoid damaging the bilateral L3‐L4 and L4‐L5 facet joints, and the capsules overlying the facets were left intact. The specimens were kept moist by saline spraying during biomechanical testing to prevent autolysis and air exposure from influencing the biomechanical behavior. Each test was performed for over five full sinusoidal loading cycles, and the data on intervertebral ROM at L3‐L4 and L4‐L5 from the fifth cycle collected and analyzed.
Statistical analysis
Statistical testing was performed for flexion, extension and torsion for each loading mode. Covariance was used to determine whether there was any significant difference between any of the fixation techniques in intervertebral rotation. Multiple nonparametric Wilcoxon signed rank tests were performed on the rank flexion, extension and torsion to determine whether a significant difference existed between pairs of instrumented spines and their intact or spondylolytic control specimens. Significance for global and individual comparisons was deemed to be when P < 0.05. All statistical analyses were performed with the commercially available SPSS 11.5 (SPSS, Chicago, IL, USA).
Results
Each specimen was proved to be intact with respect to bones and ligaments. Catastrophic failure did not occur in any of the movement segments or in any of the instruments throughout the biomechanical testing. The mean values of the intervertebral range of movement (ROM) in L3‐L4 and L4‐L5 as measured by Spine 2000 are shown in Table 1.
Table 1.
Intervertebral ROM in L3‐L4 and L4‐L5 of intact and spondylolytic calf lumber spines with and without instrumentation under flexion‐extension, lateral flexion and rotation ( , °)
, °)
| Configuration | Intact | Defect | M‐Scott | S‐R‐H | S‐R | Buck | |
|---|---|---|---|---|---|---|---|
| L3–L4 | Flexion‐extension | 10.48 ± 1.50 | 15.24 ± 2.53* | 11.99 ± 1.60** | 11.38 ± 1.55 | 11.47 ± 1.74 | 11.49 ± 1.39 |
| Lateral flexion | 15.67 ± 2.79 | 16.27 ± 2.92 | 15.92 ± 2.73 | 15.92 ± 2.86 | 16.07 ± 2.95 | 15.90 ± 2.77 | |
| Rotation | 9.19 ± 1.04 | 15.70 ± 2.08* | 9.48 ± 1.15 | 9.72 ± 0.95 | 9.76 ± 1.02 | 9.79 ± 1.23 | |
| L4–L5 | Flexion‐extension | 10.16 ± 1.71 | 13.43 ± 2.09* | 10.98 ± 1.76** | 10.33 ± 2.15 | 10.34 ± 1.95 | 10.35 ± 1.74 |
| Lateral flexion | 14.98 ± 1.53 | 15.67 ± 1.70 | 15.22 ± 1.56 | 15.22 ± 1.56 | 15.27 ± 1.55 | 15.30 ± 1.67 | |
| Rotation | 8.36 ± 1.54 | 12.44 ± 3.20* | 8.90 ± 1.37 | 8.44 ± 1.23 | 8.88 ± 1.26 | 8.97 ± 1.44 |
Significant difference between defect and the others (P < 0.05).
Significant difference between M‐Scott and the other three instruments (P < 0.05).
S‐R, screw‐rod; S‐R‐H, screw‐rod‐hook.
For all of the uninstrumented spondylolytic spines, the intervertebral rotation in L3‐L4 and L4‐L5 was greater than that in the intact spine. In flexion‐extension, the mean ROM at L3‐L4 increased to 146.3% of that found in the intact condition. In axial rotation, the mean ROM at L3‐L4 was also increased to 170.8%. Concerning the influence of the pars defects on the L4‐L5 motion segment, the mean ROM increased significantly to 132.1% of that found in the intact condition in flexion‐extension and to 148.8% in the axial rotation direction. However, no significant difference was found in lateral flexion (P= 0.472, 3, 4).
Figure 3.
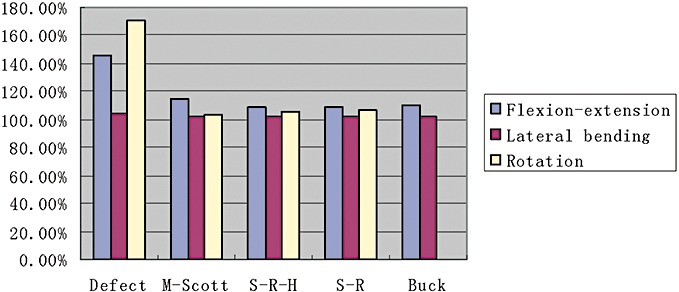
Percent range of motion at L3‐L4 under five different conditions. S‐R, screw‐rod; S‐R‐H, screw‐rod‐hook.
Figure 4.
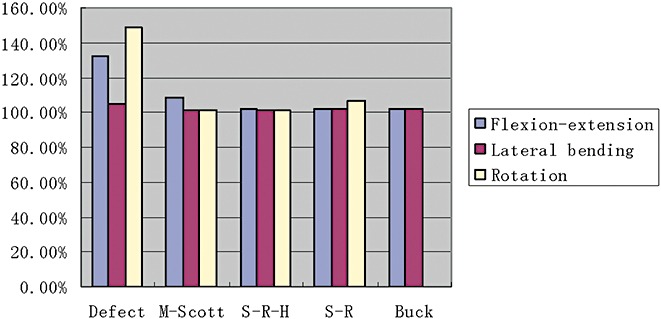
Percent range of motion at L4‐L5 under five different conditions. S‐R, screw‐rod; S‐R‐H, screw‐rod‐hook.
Each fixation technique significantly increased the intervertebral rotational stability to almost intact levels. In flexion‐extension there was no significant difference between the screw‐rod‐hook, screw‐rod construct fixation and Buck fixation techniques (P= 0.846) in the % ROM at both L3‐L4 and L4‐L5. However, these techniques provided more stability than the modified Scott technique (P < 0.05). No significant difference was found among the four fixation techniques in lateral flexion or rotation. However, the screw–rod‐hook and screw‐rod construct fixation techniques were better than the modified Scott and Buck techniques in axial rotation.
Discussion
The precise mechanism of spondylolysis is largely unknown. However, besides anatomic elements, genetic factors and fatigue of the neural arch are regarded as the main causes 8 , 9 . Spondylolysis can be found at any level of the spine; however, the most commonly involved vertebrae are L4 and L5. Although most of those affected by the disorders are asymptomatic, a small number of patients experience chronic low back pain, sometimes radiating to the buttocks or thighs. Fusion of the involved level has been widely accepted as the treatment of choice for symptomatic spondylolysis 2 . However, some investigators believed that intersegmental fusion, because it restrains mobility in the adjacent levels, may result in a significant acceleration of degenerative lesions at those levels 3 , 10 . Reconstruction of the pars interarticularis seems to be a logical and less aggressive approach to restoring the anatomy and stability of the spine for young symptomatic patients 11 .
Since Buck first described direct repair of an isthmic defect by internal fixation 5 , several methods for stabilizing a lumbar pars defect have been described, including using wires, hooks or screw‐hook combinations, and the good and excellent rates are 79%–100%. Recently, several novel techniques for surgical repair of spondylolysis have been performed in adolescents with excellent clinical results 6 , 9 . However, the primary focus of these studies has been to review the clinical results of each method, and few comprehensive biomechanical studies have been reported in detail.
Some authors have shown the presence of retrolisthesis at the level above the spondylolysis, and commented on its possible contribution to the genesis of pain 12 , 13 . Henson et al. performed discograms on 36 symptomatic patients with L5‐S1 spondylolysis and noted that concordant pain could be induced by injection into the L4‐5 disc in 11 of those cases (30.5%) 12 . Moreover, recent studies using magnetic resonance imaging have also revealed a high incidence of degenerative changes, not only at the involved level but also at the disc superior to the pars defect 14 . In patients with spondylolysis, instability and/or stenosis at the adjacent level above it is a possible cause for persistent low back pain or sciatica, and changes in mobility at the affected lumbar level and the adjacent level above it can be induced by the spondylolysis 6 . Therefore, it is necessary to pay attention to the state of both the affected lumbar level and the level above it.
In 1999, Deguchi et al. compared the biomechanics performance of some traditional fixation techniques including the Scott, Buck, modified Scott and Screw‐rod‐hook techniques in calf L4‐L5 after L4 bilateral spondylolysis 6 . In 2003, Mihara et al. performed a biomechanical study in calf L3‐L4 and L4‐L5 simultaneously after L4 bilateral spondylolysis, however, he focused only on the Buck technique. 15 Besides, screw‐rod construct fixation, a novel fixation technique, has now been developed for direct repair of spondylolysis, and there is no comprehensive biomechanical comparison of those different fixation techniques in calf L4‐L5 and L3‐L4 simultaneously.
In the current study, kinetic changes in mobility of the involved segment after creation of a pars defect were evaluated, and the influence of standard surgical techniques on spondylolysis was assessed. Once a defect has occurred in the pars interarticularis, intervertebral rotation at the L3‐L4 and L4‐L5 levels increases, especially in flexion and torsional loading. As to the mechanism of instability at the upper adjacent segment, it is speculated that the intact ligamentum flavum causes an increased degree of extension at the upper adjacent segment. In addition, the pars defect would also alter its segmental stability because the supraspinous and interspinous ligaments would not effectively limit intervertebral motion 16 . This hypothesis was further supported by this study. Thus, the presence of a lytic defect can accentuate disc degeneration because of increased disc mobility both above and below the defect, and comprehensive biomechanical comparison of those fixation techniques in calf L3‐L4 and L4‐L5 simultaneously therefore became more crucial.
All fixation techniques significantly increased stability and restored intervertebral rotational stability to almost intact levels. The lack of a statistically significant difference in lateral flexion (P, 0.472) indicates that tethering the intact articular ligament between transversus thoracis and disc construct resulted in a greater ability to counter lateral flexion. In the spondylolytic spines with instruments, rotation was improved to almost the intact level. The screw‐rod‐hook, screw‐rod construct, and Buck techniques provided more flexion/extension stability than the modified Scott technique. The reason may be a decline in tension in the wire looping around the pedicle screws and spinous process in some directions. With regard to rotation and lateral flexion, this study revealed no significant differences among the four techniques. However, the screw‐rod‐hook and screw‐rod construct fixation techniques provided more rotational stability than did the other two techniques. In Deguchi testing, the screw‐rod‐hook technique displayed less flexion than the intact spine because of an increase in tension in the yellow ligament due to placing hooks there 6 . However, in the present study the same result was not found, the reason may lie in the different methods of testing.
It has been reported that the Buck technique can produce a good result. However, a significant lateral curve for correct placement of the screw is necessary. The current study also indicates that it is not very promising in regard to torsion. As for the modified Scott's technique, fatigue fracture and poor tension was found. The advantages of the screw‐rod‐hook and screw‐rod techniques, with their excellent ability to stabilize a spondylolysis, are that with these systems the strength of the fixation instruments makes postoperative immobilization unnecessary and decreases the probability of device failure, permitting earlier full weight‐bearing and more rapid rehabilitation than does the modified Scott and Buck technique. Pedicles are placed outside the lytic area and the defect can be filled with bone graft, which is not the case with the Buck technique. In our study screw‐rod construct fixation for treating spondylolysis resulted in excellent stability, a good primary clinical outcome has been also reported by other authors 14 , 17 . However in our experience, with the modified Scott technique tightening of the ‘V’ rod under the spinous process may bring about fatigue fracture of the spinous process after a long time, which can lead to failure of the surgery.
Calf lumbar spines were used in this study, being chosen because of their similar size and mechanical responses, as compared to the human spine, under a range of loading conditions 18 . Potential weaknesses of this study are that all fixation techniques were performed on the same sample, and the efficiency of fixation would have declined after the first surgery. Therefore, these operations required good surgical skills and the specimens had to be operated on carefully in order to preserve the spinal ligaments and facet joint capsules. In the present study, we designated Buck screw fixation as the least favorable of the four techniques tested because of its high demand for technique.
References
- 1. Fredrickson BE, Baker D, McHolick WJ, et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am, 1984, 66: 699–707. [PubMed] [Google Scholar]
- 2. Hensinger RN. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Am, 1989, 71: 1098–1107. [PubMed] [Google Scholar]
- 3. Ghiselli G, Wang JC, Bhatia NN, et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am, 2004, 86: 1497–1503. [DOI] [PubMed] [Google Scholar]
- 4. Sairyo K, Goel VK, Faizan A, et al. Buck's direct repair of lumbar spondylolysis restores disc stresses at the involved and adjacent levels. Clin Biomech, 2006, 21: 1020–1026. [DOI] [PubMed] [Google Scholar]
- 5. Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br, 1970, 52: 432–437. [PubMed] [Google Scholar]
- 6. Deguchi M, Rapoff AJ, Zdeblick TA. Biomechanical comparison of spondylolysis fixation techniques. Spine, 1999, 24: 328–333. [DOI] [PubMed] [Google Scholar]
- 7. Roca J, Iborra M, Cavanilles‐Walker JM, et al. Direct repair of spondylolysis using a new pedicle screw hook fixation: clinical and CT‐assessed study: an analysis of 19 patients. J Spinal Disord Tech, 2005, 18 (Suppl.): S82–S89. [DOI] [PubMed] [Google Scholar]
- 8. Lindholm TS, Ragni P, Ylikoski M, et al. Lumbar isthmic spondylolisthesis in children and adolescents. Radiologic evaluation and results of operative treatment. Spine, 1990, 15: 1350–1355. [DOI] [PubMed] [Google Scholar]
- 9. Hammerberg KW. New concepts on the pathogenesis and classification of spondylolisthesis. Spine, 2005, 30 (6 Suppl.): S4–S11. [DOI] [PubMed] [Google Scholar]
- 10. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord, 1995, 8: 464–473. [PubMed] [Google Scholar]
- 11. Vathana P, Prasartritha T. A biomechanical study of the surgical repair technique of pars defect in spondylolysis. J Med Assoc Thai, 1998, 81: 824–829. [PubMed] [Google Scholar]
- 12. Henson J, McCall IW, O'Brien JP. Disc damage above a spondylolisthesis. Br J Radiol, 1987, 60: 69–72. [DOI] [PubMed] [Google Scholar]
- 13. Penning L, Blickman JR. Instability in lumbar spondylolisthesis: a radiologic study of several concepts. Am J Roentgenol, 1980, 134: 293–301. [DOI] [PubMed] [Google Scholar]
- 14. Szypryt EP, Twining P, Mulholland RC, et al. The prevalence of disc degeneration associated with neural arch defects of the lumbar spine assessed by magnetic resonance imaging. Spine, 1989, 14: 977–981. [DOI] [PubMed] [Google Scholar]
- 15. Mihara H, Onari K, Cheng BC, et al. The biomechanical effects of spondylolysis and its treatment. Spine, 2003, 28: 235–238. [DOI] [PubMed] [Google Scholar]
- 16. Zhao J, Liu F, Shi HG, et al. Biomechanical and clinical study on screw hook fixation after direct repair of lumbar spondylolysis. Chin J Traumatol, 2006, 9: 288–292. [PubMed] [Google Scholar]
- 17. Ulibarri JA, Anderson PA, Escarcega T, et al. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine, 2006, 31: 2067–2072. [DOI] [PubMed] [Google Scholar]
- 18. Wilke HJ, Krischak S, Claes L. Biomechanical comparison of calf and human spines. J Orthop Res, 1996, 14: 500–503. [DOI] [PubMed] [Google Scholar]


