Introduction
Synovial sarcoma is an uncommon malignant tumor with an annual incidence of 2.57 per 100 000. According to the database of the Memorial Sloan‐Kettering cancer center on 3400 sarcoma patients from 1982 to 1997, synovial sarcoma accounts for about 13% of all soft tissue sarcomas of the extremities 1 . Unlike other soft tissue sarcomas, synovial sarcoma is always seen in young patients aged from 15 to 40 years, with a slight male dominance. Since it was first reported in 1865 2 , synovial sarcoma has been found to occur mainly in the vicinity of the large proximal joints, although the head and neck region, lung, pleura, mediastinum, cardiac tissue, kidney, retroperitoneum, skin, abdominal wall, chest wall, and bone marrow have also been reported to have been involved 3 .
The cause of synovial sarcoma still remains unclear. A case of synovial sarcoma with an extremely prolonged course is presented here and the possible causes discussed with the purpose of highlighting the potential occurrence of this disease.
Case report
A 46‐year‐old man presented to the authors' hospital with pain and swelling on the medial side of the left foot. When he was 26 years old, a pain had suddenly developed in his left foot without any obvious cause. The pain always occurred when he got cold and could be relieved by soaking in hot water. Five years later, the patient went to a local clinic as the pain had become more severe and was occurring more frequently than before. He was treated with Ibuprofen, and the pain was relieved. At the age of 43 years, he had a surgical excision with a diagnosis of synovial cyst because his symptom could not be controlled by drugs. One year later, because of recurrence of symptoms, he underwent another surgical excision, and pathological examination resulted in a diagnosis of nodular synovitis. However, his symptoms were not eliminated, and affected him repeatedly after the second operation. He described that his foot gradually became more enlarged and swollen, and that this was accompanied by unendurable pain while weight bearing in the last few months before admission to the authors' hospital.
On admission, physical examination revealed a small, tender, circumscribed, hard mass on the medial side of the swollen left foot. The skin was not involved, neither was venous dilatation found. The blood supply and sensation in the toes of the left foot were normal, while movement was impaired. No enlarged local lymph nodes were found. Radiographs showed bony erosion and periosteal reaction in the medial aspect of the second metatarsal and the proximal aspect of the first metatarsal bones (Fig. 1). No obvious abnormalities were found on chest radiograph. Incision biopsy and MRI of the left foot were performed. A large lobulated soft tissue mass measuring 7 cm × 5.5 cm × 6 cm was identified. The mass straddled the first to the fourth metatarsal bone (Fig. 2a,b). The histology result was consistent with synovial sarcoma (Fig. 3). Immunochemistry results of epithelial membrane antigen (EMA) staining (Fig. 4a) and video intensification microscopy (VIM) (Fig. 4b) were positive and those of CD‐34, CD‐68, CD‐117, Actin, Des, S‐100 were all negative, which further supported the diagnosis. The patient underwent left proximal tibial amputation. After the operation, he received adjuvant chemotherapy with Adriamycin and Ifosfamide. One year after surgery neither metastasis nor recurrence has yet been found, and the patient continues to attend for follow up.
Figure 1.

Dorsoplantar and medial oblique radiographs of the left forefoot show bony erosion and periosteal reaction in the medial aspect of the second metatarsal shaft (small arrow) and the proximal medullary canal of the first metatarsal shaft (large arrow). No obvious calcification is seen in the soft tissues.
Figure 2.

MRI of the left foot: (a) T1‐weighted MRI shows a low signal mass; (b) T2‐weighted MRI shows a lobulated mass with high signal and obscure boundary.
Figure 3.
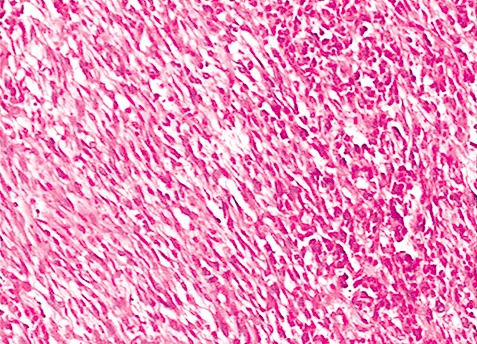
Microscopy shows that the tumor tissue consists of abundant spindle cells. Most cells are arranged in bundles, with darkly stained round or ovoid nuclei. Epithelioid cells are also seen in local regions.
Figure 4.
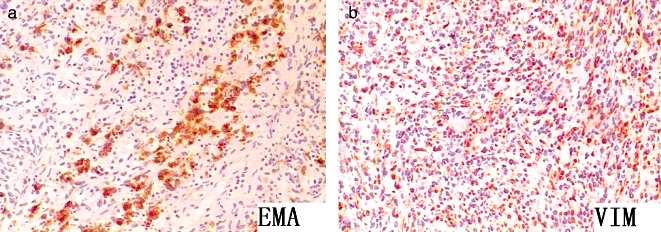
Microscopy shows positivity of tumor cells. Both are at magnification ×100 (a) EMA and (b) VIM stain.
Discussion
Synovial sarcoma is a relatively rare form of soft tissue sarcoma 4 , 5 . Though called “synovial sarcoma”, there is no convincing evidence that it always originates from synovial tissue, and less than 10% of these tumors occur intra‐articularly 4 . Immunochemistry and ultrastructural research has revealed that synovial sarcoma derives from as yet unknown multipotent stem cells capable of differentiating into mesenchymal and/or epithelial structures and lacking synovial differentiation 6 , 7 , 8 .
Synovial sarcoma can be classified histologically into four types, namely biphasic spindle‐cell, monophasic spindle‐cell, monophasic epithelioid, and poorly differentiated. The biphasic and monophasic spindle‐cell types are dominant, and the poorly differentiated type has the worst prognosis.
It has been clearly demonstrated by cytogenetic and molecular genetic research that translocation of t(X; 18) is associated exclusively with synovial sarcoma 4 . However, the cause remains unknown.
Most patients describe an episode of trauma prior to the diagnosis of synovial sarcoma, though a causative connection has not been definitely identified. Sen and Dooley believed that trauma was coincidental and not a causative factor, even though these tumors are found more often in the lower extremities. They thought that trauma probably caused hemorrhage in the lesion, making the tumor larger and therefore more noticeable to the patient 9 . In aretrospective study, 71.4% (10/14) patients had a history of trauma, including torsional injuries and blunt trauma 10 . The time from trauma to the diagnosis of tumor was between 3 and 9 months. In this case, although the patient denied a trauma history, he had undergone surgical excisions 1 and 3 years prior to presenting to the authors' hospital. Thus, the possibility of trauma evoking his tumor cannot be excluded.
Synovial sarcoma always presents in adolescents or adults younger than 40 years of age. Most commonly, it starts as a slowly enlarging, deep‐seated, painful mass. In this case, the age of initial onset was 26 and thus in the high incidence age group, though no definite diagnosis was made at that time. Local recurring synovial sarcoma is common, usually being evident within 2 years of surgery, but can be delayed by up to 10 years postoperatively 3 . Three years before admission to the authors' hospital, the patient described here had a surgical excision, which may be considered to have been a local resection of preexisting tumor tissue. There was no chemotherapy or radiotherapy postoperatively, and the symptom recurred one year later, which is in accordance with previous reports. Thus, the possibility of the tumor having been present over a prolonged period cannot be excluded.
As far as the authors know, no cases of synovial sarcoma case with a history of synovial cyst or nodular synovitis have been reported, nor has there been a case of cancer developing in a synovial cyst or nodular synovitis. In the present case, the patient described a period of 20 years during which a cyst or inflammation might have been persistently present and causeing physical or inflammatory stimulation. Though no relationship can definitely be identified, the possibility of prolonged pre‐existing stimulation as a causative factor for synovial sarcoma cannot be excluded.
Synovial sarcoma has an unfavorable prognosis; the estimated 10‐year survival rate of patients younger than 20 years being about 90%, whereas it is only 25% in patients over 40 years old 1 . Because of its low incidence, insidious position and atypical symptom, misdiagnosis and delayed diagnosis are common. Synovial sarcoma of the foot has been diagnosed as acute gouty arthritis, Morton's neuroma, trapped nerve and tarsal tunnel syndrome 3 , 11 , 12 . A definite diagnosis relies on biopsy. It is important to consider the possibility of synovial sarcoma, especially in patients with a history of trauma, surgery, and other synovial lesions. Early diagnosis and treatment can lead to an improved prognosis.
Disclosure
The authors state that they have no actual or potential conflict of interest.
References
- 1. Aljubran A, Tulba A, Akhtar S. Metastatic synovial sarcoma of the foot to the throat. Am J Clin Oncol, 2008, 31: 205–206. [DOI] [PubMed] [Google Scholar]
- 2. Simon G. Exstirpation einer sehr grossen, mit dicken Stiele angewachsenen Kneigelenkmaus mit gluklichem Erfolge. Archiv Fur Klin Chir, 1865, 6: 573–576. [Google Scholar]
- 3. Du Y, Pullman‐Mooar S, Schumacher HR. Synovial sarcoma of the foot mimicking acute gouty arthritis. J Rheumatol, 2005, 32: 2006–2008. [PubMed] [Google Scholar]
- 4. Betal D, Babu R, Mehmet V. Monophasic synovial sarcoma of the pharynx: A case report. Int Semin Surg Oncol, 2009, 6: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armstrong AV Jr, Aedo A, Phelps S. Synovial sarcoma: A case report. Clin Podiatr Med Surg, 2008, 25: 167–181. [DOI] [PubMed] [Google Scholar]
- 6. Sandberg AA, Bridge JA. Updates on the cytogenetics and molecular genetics of bone and soft tissue tumors. Synovial sarcoma. Cancer Genet Cytogenet, 2002, 133: 1–23. [DOI] [PubMed] [Google Scholar]
- 7. Hirsch RJ, Yousem DM, Loevner LA, et al Synovial sarcomas of the head and neck: MR findings. Am J Roentgenol, 1997, 169: 1185–1188. [DOI] [PubMed] [Google Scholar]
- 8. Company Campins MM, Morales R, Dolz C, et al Primary monophasic synovial sarcoma of the duodenum confirmed by cytogenetic analysis with demonstration of t(X;18): A case report. J Gastrointestin Liver Dis, 2009, 18: 89–93. [PubMed] [Google Scholar]
- 9. Sen SK, Dooley WT. Synovial sarcoma. J Natl Med Assoc, 1987, 79: 1089–1090. [PMC free article] [PubMed] [Google Scholar]
- 10. Scully SP, Temple HT, Harrelson JM. Synovial sarcoma of the foot and ankle. Clin Orthop Relat Res, 1999, 364: 220–226. [DOI] [PubMed] [Google Scholar]
- 11. Ueo T, Yamamuro T, Kodama Y, et al An unusual cause of Morton's syndrome—A synovial sarcoma: Report of a case. J Foot Surg, 1979, 18: 23–25. [PubMed] [Google Scholar]
- 12. Brewster MB, Power D, Sumathi VP. Delayed diagnosis of synovial sarcoma of the foot. Orthopedics, 2008, 31: 175. [DOI] [PubMed] [Google Scholar]


