Abstract
Objective: To investigate the efficacy of microendoscopic discectomy (MED) for the treatment of lumbar disc herniation over a five‐year follow‐up period.
Methods: Between January 2000 and December 2002, 275 patients were accepted for MED in our hospital. A retrospective review was carried out on 151 of these cases with a mean of five years follow‐up. The study helped us to assess the efficacy of this technique in the treatment of lumbar disc diseases. Modified MacNab criteria were used to assess the clinical outcome, and the disc‐height ratio was assessed radiographically according to the Mochida's method.
Results: According to the modified MacNab criteria, 78.8% of patients were rated as excellent, 13.2% as good, 4.6% as fair, and 3.3% as poor. Complications included five revision surgeries due to recurrence of herniation, five dural lacerations during operation, and three cases of vertebral/disc infection. The average disc‐height ratio was 76.25%. Approximately 57% of the patients maintained their primary engagement.
Conclusion: MED is both feasible and efficacious for the management of lumbar disc disease. On the basis of the present study it is concluded that MED is better than open discectomy (OD).
Keywords: Diskectomy, Endoscopy, Intervertebral disk displacement, Lumbar vertebrae
Introduction
The technique of microendoscopic discectomy (MED) was initially developed in 1997 when it was a relatively new procedure providing minimally invasive access to the spinal column 1 . The system offers many advantages over other minimally invasive lumbar discectomy techniques. Sofamor Danek (Memphis, TN, USA) has developed the required instruments and technology, enabling surgeons to successfully remove all disc fragments and other pathological material and to decompress lateral recess stenosis, even when undertaking contralateral spinal decompression from an ipsilateral approach.
Materials and methods
Two hundred and seventy‐five patients underwent MED in our hospital between January 2000 and December 2002. Of these, 151 patients were followed up as out‐patients or by phone calls. The remaining patients were not followed up because of changes in their address or telephone number. The five‐year follow‐up study of 151 cases has helped us to determine the efficacy of this system for treating lumbar disc diseases. The procedures were performed by orthopaedic surgeons who have specialized in spinal disorders.
The diagnosis of lumbar disc herniation (LDH) was confirmed in all patients by clinical manifestations, preoperative computed tomography (CT) and/or magnetic resonance imaging (MRI). The MED procedure was utilized for patients with severe leg pain which had not resolved after at least three months of conservative management, the same criterion as is used to select patients for standard discectomy.
One hundred and fifty‐one patients with LDH, including 87 men and 64 women with an average age of 39 years (range, 15–71) underwent MED. The vertebral level affected was L2–3 in 4 patients, L3–4 in 12, L4–5 in 57, and L5–S1 in 85. Seven patients were affected at two levels, two of those were affected at L3–4 and L4–5, and five at L4–5 and L5–S1. According to the modified MacNab classification system 2 , there were 11 cases of protrusion, 75 of subligamentous extrusion, 52 of transligamentous extrusion and 13 of sequestration. Ten of the herniated discs were of the far lateral type, and 45 had concomitant lateral recess stenosis.
All patients presented with low back and/or leg pain. In some patients back pain was more severe than leg pain, while others suffered equally from back and leg pain. All 151 patients manifested motor and/or sensory neurologic deficits, which occurred at each level affected.
The clinical outcomes of all patients were evaluated according to the modified MacNab criteria. One hundred and seven of the 151 patients underwent radiographic assessment after five years and their disc‐height ratio was calculated by measurement on lateral films according to Mochida's method 3 .
Surgical technique
The surgery was performed with the patients in a prone position under epidural anesthesia. A Kirschner wire was passed through the skin approximately one fingerbreadth lateral to the midline of the affected side to the caudal border of the rostral lamina in the appropriate interspace, the placement being confirmed by lateral C‐arm fluoroscopic guidance (Fig. 1). An 18 mm paramedian incision was made (Fig. 2), then dilators were sequentially placed over the Kirschner wire down to the lamina and a working channel placed over the final dilator. A flexible arm, which was fixed to the table, was attached to the tubular retractor to hold it firmly. The sequential dilators were then removed to establish a tubular operative corridor to the lamina and interlaminar space. An endoscope was then inserted into the tubular retractor and secured to the tubular retractor with a locking arm on the ring attachment.
Figure 1.

CT image showing L4–5 disc herniation.
Figure 2.

An 18 mm incision into the paraspinal musculature.
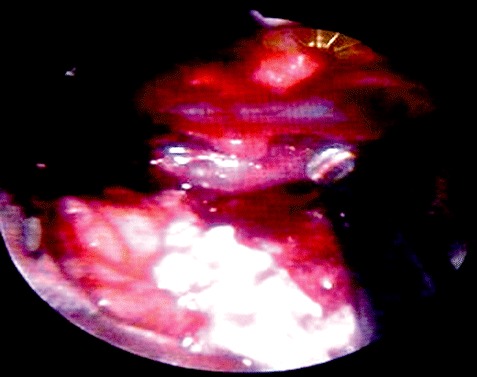
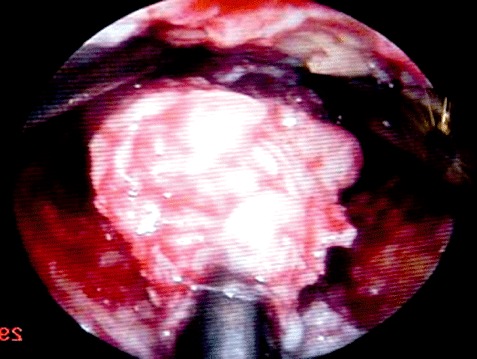
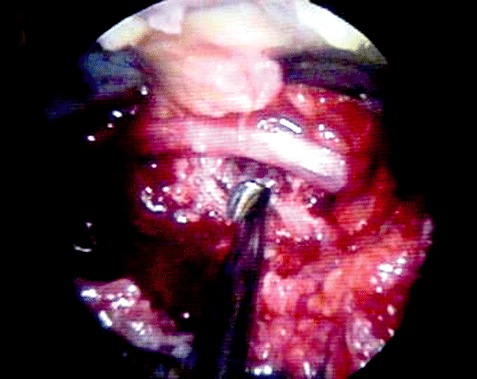
Next the ligamentum flavum was opened with an up‐ward angled curette. The ligament was penetrated with the curette using a twisting motion, then peeled back caudally and dorsally (Fig. 3). The dura and traversing nerve root were then identified and the nerve root retracted medially with a dissector or suction retractor. The ventral epidural space was then explored (Fig. 4). After protecting the nerve root with suction retractor, the herniated disc was removed with a pituitary rongeur in a standard fashion (Fig. 5). Then work was performed both within and external to the disc just as occurs during a standard open microdiscectomy. Once the nerve root had been decompressed, the disc space was thoroughly irrigated (Fig. 6). The flexible arm assembly was then loosened and the tubular retractor slowly removed. Any bleeding in the paraspinal musculature was controlled with bipolar forceps. The cases with two levels affected were treated through a single tubular path. To accomplish this, the channel had to be adjusted and the appropriate target confirmed.
Figure 3.

The ligamentum flavum is opened.
Figure 4.
The dura and traversing nerve root are identified.
Figure 5.
The herniated disc is removed.
Figure 6.
The nerve root is decompressed and the disc space thoroughly irrigated.
During the first two weeks, all patients had to undergo intensive trunk stabilization. The timing of ambulation depended on the ability of patients to participate in the rehabilitation program, rather than on the number of days postoperative. The average time to achieve ambulation was 3.5 days.
Each of the cases was followed in detail postoperatively by phone calls or office visits. One hundred and fifty‐one patients were followed up for five years after surgery.
Results
According to the modified MacNab criteria, by the end of the fifth year, 119 patients (78.8%) were rated as excellent, 20 (13.2%) as good, 7 (4.6%) as fair and 5 (3.3%) as poor. At final follow‐up, seven patients still had neurologic deficits. There were no cases of permanent iatrogenic nerve damage.
Five of the 151 cases (3.3%), all of whom were adult men under 50 years of age, required revision surgery due to recurrence of disc herniation at the same level. In all of these cases standard discectomy was performed. The length of time between the two operations ranged from 1.5 to 4.5 years, with an average of 2.8 years.
Five cases experienced intraoperative dural laceration, which was resolved by applying fibrin glue through the tubular retractor. Drainage was placed percutaneously and removed after 1–2 days.
In addition, vertebral/disc infection was diagnosed postoperatively in three cases. Besides clinical manifestations and blood tests, the most appropriate diagnostic procedure is MRI. All three patients underwent debridement about 1 to 4 weeks later after the diagnosis had been confirmed. Staphylococci were cultured from specimens from all three patients. Then antibiotics to which the pathogenic organisms were sensitive were administered continuously intravenously for 2–3 weeks until the concentration of C‐reactive protein (CRP) and leucocyte counts were normal.
The average disc‐height ratio of the 107 patients who underwent postoperative radiographic assessment was 76.25%. No patients developed instability or spondylosis.
Approximately 57% of the patients were able to resume their former recreational and occupational activities, including 13 athletes, 22 drivers and 27 builders. The average time between surgery and return to these activities was 2.5 months (range, 1–14 months). Furthermore, most of them had complained chiefly of leg pain.
Some of the potential complications of MED are not significantly different to those of standard microdiscectomy. Risks specific to MED include instrument malfunction, such as bending, fragmentation, loosening and/or breakage.
Discussion
The MED system, a unique approach to the surgical management of lumbar disc disease which combines the reliability of an open microsurgical technique with the advantages of a minimally invasive approach, was introduced in 1997. In 1998 the first 100 cases were reported to have had good results due to the smaller incision and reduction in tissue trauma 1 . MED is unique in that far lateral pathology can be directly visualized and removed through a 15 mm paramedian incision 4 . So MED gained attention in the following years, during which there were more reports of its favourable outcomes 5 . Now that eight years have passed, prospective, randomized clinical studies are necessary to verify the long‐term outcomes (over five years) of this form of surgery.
The long‐term results of standard lumbar discectomy are not very satisfactory. Over one‐third of patients are dissatisfied with the results, and over a quarter complain of significant residual pain 6 . In one study, 40 of 531 patients required a second operation for recurrent sciatica, giving a revision rate of 7.9% over a period of 16 years 7 . In another study in which patients who had undergone standard discectomy for LDH were followed up for over 10 years, 9 of 72 cases (12.5%) required revision surgery 8 . Therefore we are satisfied with the 7.3% rate of reoperation in the present study, two‐thirds being due to recurrent disc herniation and the rest to infection.
It is very rare for vertebral/disc infection to occur after MED. There is a paucity of literature on such infection as a complication of MED. The frequency of such infection in patients who have undergone MED is probably similar to that after open discectomy (OD).
Because it is less traumatic, MED allows an early return to work, as previously reported 9 . Compared with traditional discectomy techniques, this minimally invasive method of lumbar discectomy reduces tissue trauma. The magnitude of trauma is more important than the length of the skin incision in minimally invasive surgery. A difference in the systemic cytokine response supports the contention that the MED procedure is less traumatic 10 . A significant difference in mean operative blood loss for the two groups has also been observed 11 . Mechanically elicited electromyogram (EMG) activity in muscle groups innervated by the lumbar nerve roots has been recorded during the dynamic stages of surgery. These show that the endoscopic technique is superior to the open surgical technique in that it produces less irritation of the nerve roots 12 . However Isaacs et al. have reported that with respect to average operative time, mean blood loss, and length of hospital stay, there is no statistical difference between MED and OD groups 13 . Although morbidity is decreased in the MED group, a few technical problems remain to be solved.
MED is an effective microendoscopic system for treating LDH. It has a good long‐term outcome, and the endoscopic approach allows smaller incisions and reduced tissue trauma compared with standard open microdiscectomy. But MED has a steep learning curve 14 ; the surgeon should undergo training before applying MED techniques. On the basis of the results of a five‐year follow‐up, we conclude that MED is both feasible and efficacious for the management of lumbar disc disease.
References
- 1. Smith MM, Foley KT. Microendoscopic discectomy (MED): the first 100 cases. Neurosurgery, 1998, 43: 702. [Google Scholar]
- 2. MacNab I, Negative disc exploration. An analysis of the causes of nerve‐root involvement in sixty‐eight patients. J Bone Joint Surg, 1971, 53A: 891–903. [PubMed] [Google Scholar]
- 3. Mochida J, Nishimura K, Nomura T, et al. The importance of preserving disc structure in surgical approaches to lumbar disc herniation. Spine, 1996, 21: 1556–1564. [DOI] [PubMed] [Google Scholar]
- 4. Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far‐lateral lumbar disc herniation. Neurosurg Focus, 1999, 7: E5. [DOI] [PubMed] [Google Scholar]
- 5. Sasaoka R, Nakamura H, Konishi S, et al. Objective assessment of reduced invasiveness in MED compared with conventional one‐level laminotomy. Eur Spine J, 2006, 15: 577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Loupasis GA, Stamos K, Katonis PG, et al. Seven‐ to 20‐year outcome of lumbar discectomy. Spine, 1999, 24: 2313–2317. [DOI] [PubMed] [Google Scholar]
- 7. Morgan‐Hough CV, Jones PW, Eisenstein SM. Primary and revision lumbar discectomy. A 16‐year review from one centre. J Bone Joint Surg Br, 2003, 85: 871–874. [PubMed] [Google Scholar]
- 8. Yorimitsu E, Chiba K, Toyama Y, et al. Long‐term outcomes of standard discectomy for lumbar disc herniation: a follow‐up study of more than 10 years. Spine, 2001, 26: 652–657. [DOI] [PubMed] [Google Scholar]
- 9. Nakagawa H, Kamimura M, Uchiyama S, et al. Microendoscopic discectomy (MED) for lumbar disc prolapse. J Clin Neurosci, 2003, 10: 231–235. [DOI] [PubMed] [Google Scholar]
- 10. Huang TJ, Hsu RW, Li YY, et al. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res, 2005, 23: 406–411. [DOI] [PubMed] [Google Scholar]
- 11. Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: comparison of microendoscopic discectomy and Love's method. Spine, 2001, 26: 1599–1605. [DOI] [PubMed] [Google Scholar]
- 12. Schick U, Döhnert J, Richter A, et al. Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur Spine J, 2002, 11: 20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Isaacs RE, Podichetty V, Fessler RG. Microendoscopic discectomy for recurrent disc herniations. Neurosurg Focus, 2003, 15: E11. [DOI] [PubMed] [Google Scholar]
- 14. Ikuta K, Arima J, Tanaka T, et al. Short‐term results of microendoscopic posterior decompression for lumbar spinal stenosis. Technical note. J Neurosurg Spine, 2005, 2: 624–633. [DOI] [PubMed] [Google Scholar]


