Key Points
Question
How did cost-related medication nonadherence change among adult survivors of stroke after the implementation of the Affordable Care Act?
Findings
In this study of data from a nationally representative sample of 13 930 survivors of stroke in the United States, an absolute decrease of 5.7% in cost-related medication nonadherence among survivors of stroke aged 45 to 64 years was associated with the implementation of the Affordable Care Act.
Meaning
Expansion of Medicaid coverage in more states is likely to further improve medication affordability and adherence for adult survivors of stroke.
Abstract
Importance
Among adults with chronic disease, survivors of stroke have high out-of-pocket financial burdens. The US government enacted the Affordable Care Act (ACA) in 2010 and implemented the law in 2014 to provide more low-income adults with health insurance coverage.
Objective
To assess whether ACA implementation is associated with cost-related nonadherence (CRN) to medication among adult survivors of stroke.
Design, Setting, and Participants
This study analyzed data from the 2000 to 2016 National Health Interview Survey, an in-person household survey of the noninstitutionalized US population conducted annually by the National Center for Health Statistics. Conducted at the University of Michigan Medical School, Ann Arbor, from July 24, 2017, to February 28, 2018, the study had a sample of 13 930 survivors of stroke. Analyses were stratified by age (45-64 years vs ≥65 years). Time was treated as a continuous variable and as a categorical variable across 4 periods (2000-2005, historical control; 2006-2010, economic recession and peak unemployment; 2011-2013, before ACA implementation; and 2014-2016, after ACA implementation). Percentages are weighted to reflect US population estimates.
Main Outcomes and Measures
The primary outcome was the self-report of CRN, defined as the inability to afford prescribed medications within the past 12 months.
Results
Among the 13 930 total survivors of stroke, 38.1% were aged 45 to 64 years (50.5% were female and 49.5% were male, with a mean [SE] age of 56.0 [0.10] years), and 61.9% were aged 65 years or older (54.9% were female and 45.1% were male, with a mean [SE] age of 76.2 [0.09] years). From 2011 to 2013 through 2014 to 2016, Medicaid increased (from 24.0% [95% CI, 21.0%-27.2%] in 2011-2013 to 30.8% [95% CI, 27.3%-34.6%] in 2014-2016; P < .001) and uninsurance decreased (from 13.7% [95% CI, 11.3%-16.4%] to 6.8% [95% CI, 5.3%-8.8%]; P < .001) among survivors of stroke aged 45 to 64 years. Among survivors aged 45 to 64 years, CRN increased over time before ACA implementation (from 18.6% [95% CI, 16.5%-20.9%] in 2000-2005, to 22.6% [95% CI, 19.7%-25.9%] in 2006-2010, to 23.8% [95% CI, 20.7%-27.3%] in 2011-2013) and decreased after ACA implementation to 18.1% (95% CI, 15.4%-21.3%; P = .01) in 2014 to 2016. The period after ACA implementation was associated with lower odds of CRN after adjustment for sociodemographics, year, and clinical factors (odds ratio [OR], 0.63; 95% CI, 0.47-0.85). The difference was attenuated after further adjustment for health insurance coverage (OR, 0.76; 95% CI, 0.56-1.03).
Conclusions and Relevance
After the ACA implementation, health insurance coverage increased and CRN decreased among adult survivors of stroke, suggesting that further expansion of Medicaid coverage is likely to be advantageous for survivors.
This study investigates whether the US Affordable Care Act is associated with medication affordability and adherence among middle-aged to older adults who have had a stroke.
Introduction
Among adults younger than 65 years with chronic disease, survivors of stroke have high out-of-pocket financial burdens, with half of these individuals spending more than 10% of disposable income on health care services in 2003.1 Prescription drug costs drive out-of-pocket financial burdens for survivors of stroke.1 Survivors take a mean (range) number of 11 (3-27) different medications.2
Medication nonadherence is often associated with cost (cost-related nonadherence [CRN]) as well as death, recurrent cardiovascular disease events, health declines, and worse quality of life among patients with cardiovascular disease.3,4 Adult survivors of stroke aged 45 to 64 years have greater CRN than older survivors aged 65 years or older.5 From 2000 to 2010, these disparities widened because medication costs increased, more adults experienced poverty, and more adults younger than 65 years were uninsured.5 In 2014, the US government implemented the Affordable Care Act (ACA), enabling low-income adults younger than 65 years to buy qualified health plans on the ACA marketplace with financial assistance. Some states also expanded Medicaid eligibility to include more low-income adults.
Little is known about how these health insurance changes have affected the ability of survivors of stroke to afford medications. In this study, we examined temporal trends in health insurance coverage status and CRN by age in a national sample of survivors of stroke in the United States. We had 2 research questions: After ACA implementation, (1) How did the uninsured rate change among survivors of stroke younger than 65 years? (2) Did medication CRN change among survivors of stroke younger than 65 years and survivors older than 65 years?
Methods
The University of Michigan Institutional Review Board ruled this study exempt because the research used publicly available data and the information was recorded in such a manner that participants cannot be identified directly or through identifiers linked to the participants. From July 24, 2017, to February 28, 2018, we studied participants in the 2000 to 2016 National Health Interview Survey (NHIS). The nationally representative NHIS is an ongoing, in-person household survey of the civilian, noninstitutionalized US population conducted annually by the National Center for Health Statistics.6 The adult sample in the 2000 to 2016 NHIS had a conditional response rate of 74% to 84%.6 We obtained the NHIS data from the Integrated Public Use Microdata Series (http://www.ipums.org). See eAppendix in the Supplement for further details of our methods.
We identified survivors of stroke as respondents reporting a physician diagnosis of stroke.7,8 The sample included 13 930 survivors of stroke with information on CRN and all covariates, representing an estimated 5.1 million survivors in the United States. Of these, 38.1% were aged 45 to 64 years, representing 2 million survivors, and 61.9% were aged 65 years or older, representing 3.1 million survivors. Each participant was surveyed once during the study period (2000-2016).
The primary outcome was the self-report of CRN (response to “During the past 12 months, was there any time when you needed prescription medicines, but didn’t get them because you couldn’t afford them?”). We stratified the analyses by age (45-64 years vs ≥65 years) because US adults generally qualify for Medical health insurance at age 65 years. We treated time as a continuous variable and a categorical variable with 4 periods: 2000 to 2005 (historical control), 2006 to 2010 (period of economic recession and peak unemployment in the United States), 2011 to 2013 (before ACA implementation), and 2014 to 2016 (after ACA implementation). We examined the frequency of health insurance coverage status and CRN before and after ACA implementation using χ2 test for trend.
We used multivariable logistic regression to estimate the association of the ACA and time with CRN after adjusting for patient factors selected according to the Andersen Behavioral Model.9 Model A included pre-ACA and post-ACA implementation and year. Model B included all covariates except health insurance coverage. Model C added health insurance coverage to model B. The ACA-by-time interaction term was not statistically significant in those aged 45 to 64 years (P = .55) or in those aged 65 years or older (P = .07); thus, the final models did not include this term and instead relied on a categorical variable to represent time-varying ACA implementation. P values were calculated using 2-sided Wald χ2 or Wald χ2 test for trend. P < .05 indicated statistical significance. All analyses used SAS-callable SUDAAN software, version 11 (Research Triangle Institute) to obtain proper variance estimates for the complex NHIS sampling design and results that were weighted to reflect national population estimates.
Results
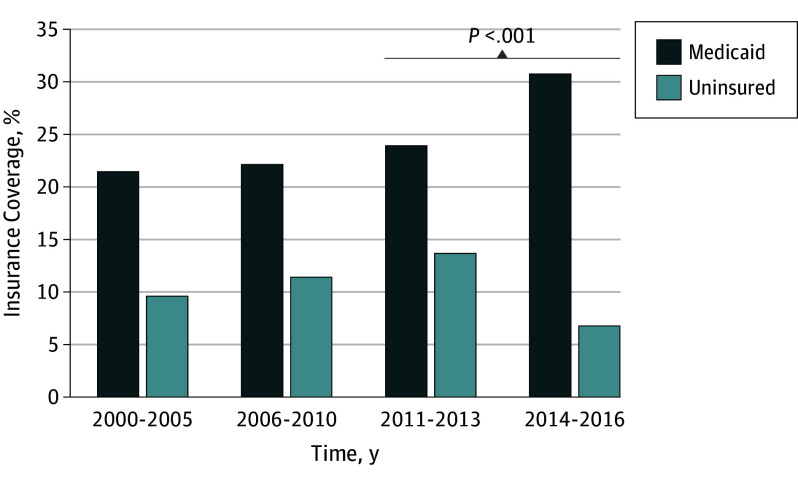
Among the 4926 survivors of stroke aged 45 to 64 years, 50.5% were female and 49.5% were male, with a mean (SE) age of 56.0 (0.10) years. Among the 9004 survivors of stroke aged 65 years or older, 54.9% were female and 45.1% were male, with a mean (SE) age of 76.2 (0.09) years. (See eTable in the Supplement for participant characteristics by age group and time.) In the 45- to 64-year group, Medicaid coverage was relatively stable over time before ACA implementation and increased significantly after ACA implementation (from 24.0% [95% CI, 21.0%-27.2%] in 2011-2013 to 30.8% [95% CI, 27.3%-34.6%] in 2014-2016; P < .001; Figure 1). In addition, uninsurance increased over time before ACA implementation and decreased significantly after ACA implementation (from 13.7% [95% CI, 11.3%-16.4%] in 2011-2013 to 6.8% [95% CI, 5.3%-8.8%] in 2014-2016; P < .001; Figure 1), representing approximately 30 000 survivors of stroke gaining health insurance coverage after the ACA was implemented. Private health insurance coverage did not change substantially after ACA implementation in survivors of stroke younger than 65 years (eTable in the Supplement). From 2000 to 2005 through 2014 to 2016, private and Medicare health insurance coverage decreased and Medicare only coverage increased in survivors of stroke aged 65 years or older (eTable in the Supplement).
Figure 1. Changes in Medicaid Coverage and Uninsurance by Time Among Survivors of Stroke Aged 45-64 Years.
Medicaid coverage increased after Affordable Care Act implementation from 24.0% (95% CI, 21.0%-27.2%) in 2011 to 2013 to 30.8% (95% CI, 27.3%-34.6%) in 2014 to 2016 (P < .001). Data from National Center for Health Statistics.6
Among survivors of stroke aged 45 to 64 years, CRN increased over time before ACA implementation (from 18.6% [95% CI, 16.5%-20.9%] in 2000-2005, to 22.6% [95% CI, 19.7%-25.9%] in 2006-2010, to 23.8% [95% CI, 20.7%-27.3%] in 2011-2013) and decreased after ACA implementation to 18.1% [95% CI, 15.4%-21.3%]; P = .01) in 2014 to 2016 (Figure 2). Conversely, CRN remained relatively stable over time among survivors aged 65 years or older (from 7.0% [95% CI, 6.0%-8.0%] in 2000-2005, to 6.1% [95% CI, 5.0%-7.3%] in 2006-2010, to 5.6% [95% CI, 4.5%-6.8%] in 2011-2013, to 6.3% [95% CI, 5.1%-7.8%] in 2014-2016; Figure 2).
Figure 2. Changes in Medication Cost-Related Nonadherence (CRN) by Time and Age Among Survivors of Stroke.
CRN increased over time before Affordable Care Act (ACA) implementation (from 18.6% [95% CI, 16.5%-20.9%] in 2000-2005, to 22.6% [95% CI, 19.7%-25.9%] in 2006-2010, to 23.8% [95% CI, 20.7%-27.3%] in 2011 to 2013 and decreased after ACA implementation (to 18.1% [95% CI, 15.4%-21.3%]; P = .01) in 2014-2016. Data from National Center for Health Statistics.6
The ACA was associated with lower odds of CRN among survivors aged 45 to 64 years but not among those aged 65 years or older after adjustment for sociodemographics and clinical factors (odds ratio [OR], 0.63 [95% CI, 0.47-0.85]; model B, Table). This difference was attenuated after further adjustment for health insurance coverage (OR, 0.76 [95% CI, 0.56-1.03]; model C, Table).
Table. Association of Affordable Care Act (ACA) Implementation With Cost-Related Medication Nonadherence Among Survivors of Strokea,b.
| Variable | OR (95% CI) | |||||
|---|---|---|---|---|---|---|
| Survivors Aged 45-64 y | Survivors Aged ≥65 y | |||||
| Model A (n = 4926)c | Model B (n = 4926)d | Model C (n = 4926)e | Model A (n = 9004)c | Model B (n = 9004)d | Model C (n = 9004)e | |
| ACA implementation | 0.61 (0.46-0.81) | 0.63 (0.47-0.85) | 0.76 (0.56-1.03) | 1.17 (0.85-1.63) | 1.24 (0.89-1.73) | 1.24 (0.89-1.73) |
| Year-by-year increase | 1.04 (1.01-1.06) | 1.04 (1.01-1.06) | 1.03 (1.00-1.05) | 0.98 (0.96-1.01) | 0.99 (0.96-1.01) | 0.98 (0.95-1.00) |
| Log likelihood | 5021.6 | 4601.2 | 4296.4 | 4233.3 | 3884.7 | 3826.80 |
Abbreviation: OR, odds ratio.
Analyses accounted for the complex sampling design and used proper variance estimations to produce results that were weighted to reflect national population estimates.
Data from National Center for Health Statistics.6
Model A included time-varying ACA implementation and year.
Model B included the covariates in model A as well as age, race, Hispanic ethnicity, sex, annual household income, educational level, health status, functional disability, modified Charlson comorbidity score, and region. This model did not include health insurance coverage.
Model C included the covariates in model B plus health insurance coverage.
Discussion
In this nationally representative sample, the ACA was associated with a significant reduction in CRN among survivors of stroke aged 45 to 64 years; an absolute decrease in CRN of approximately 6% was seen from 2011 to 2013 through 2014 to 2016. This reduction in CRN was attenuated after accounting for health insurance coverage. Among survivors of stroke aged 45 to 64 years, total health insurance and Medicaid coverage each increased by approximately 7% after ACA implementation.
Our findings that health insurance coverage increased among survivors of stroke after the ACA was implemented are consistent with reports regarding patients with cancer.10 This study extends previous work by estimating the association of ACA implementation with CRN in survivors of stroke. The results suggest that federal and state programs to improve health insurance availability and access to care may have reduced CRN for some survivors. At the time of this study, 34 states and the District of Columbia have expanded Medicaid coverage. However, survivors who live in states that did not expand Medicaid coverage are likely to have lower health insurance rates and higher out-of-pocket medical expenses than those who live in states with Medicaid coverage expansion.11
Despite federal and state programs, medication is still unaffordable for many survivors of stroke. We found that approximately 18% of survivors aged 45 to 64 years were unable to afford their medications in 2014 to 2016. In general, CRN prevents patients who have had a stroke from getting effective secondary prevention treatments. Indeed, CRN is more frequent for medications that prevent and treat cardiovascular disease than for medications that relieve symptoms.12 In addition to affordable health insurance and prescription drug coverage, effective interventions to further reduce CRN include generic medications,13 lower drug prices and co-payments,14 and free medications that prevent the recurrence of cardiovascular disease events.15
Limitations
This study has several limitations. First, self-reported data, including stroke history, may limit validity; however, extant reports suggest the high accuracy of self-reported stroke events (sensitivity rates, 80%-98%), even in older persons with a disability.7,8 Second, we did not measure potential confounders, including stroke features (severity or timing) and medication-taking attitudes or behaviors. Third, these results are generalizable only to noninstitutionalized survivors of stroke. Last, we were unable to examine participants’ state of residence or recurrent stroke events because the NHIS does not provide these data.
Conclusions
Implementation of the ACA reduced CRN among survivors of stroke aged 45 to 64 years. Of the 16 states without Medicaid coverage expansion, 3 states are currently considering it. Our findings suggest that further expansion of Medicaid coverage is likely to be advantageous for survivors of stroke in those states.
eAppendix. Additional Details on Methods
eTable. Characteristics of Stroke Survivors, by Age Group and Time: National Health Interview Survey, 2000-2016
eReferences
References
- 1.Banthin JS, Bernard DM. Changes in financial burdens for health care: national estimates for the population younger than 65 years, 1996 to 2003. JAMA. 2006;296(22):2712-2719. doi: 10.1001/jama.296.22.2712 [DOI] [PubMed] [Google Scholar]
- 2.Ostwald SK, Wasserman J, Davis S. Medications, comorbidities, and medical complications in stroke survivors: the CAReS study. Rehabil Nurs. 2006;31(1):10-14. doi: 10.1002/j.2048-7940.2006.tb00004.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care. 2010;48(2):87-94. doi: 10.1097/MLR.0b013e3181c12e53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297(10):1063-1072. doi: 10.1001/jama.297.10.1063 [DOI] [PubMed] [Google Scholar]
- 5.Levine DA, Morgenstern LB, Langa KM, Piette JD, Rogers MA, Karve SJ. Recent trends in cost-related medication nonadherence among stroke survivors in the United States. Ann Neurol. 2013;73(2):180-188. doi: 10.1002/ana.23823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Centers for Disease Control and Prevention, National Center for Health Statistics. National Health Interview Survey . https://www.cdc.gov/nchs/nhis/index.htm. Accessed January 30, 2018.
- 7.Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of self-report, hospital discharge codes, and adjudication of cardiovascular events in the Women’s Health Initiative. Am J Epidemiol. 2004;160(12):1152-1158. doi: 10.1093/aje/kwh314 [DOI] [PubMed] [Google Scholar]
- 8.Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc. 2004;52(1):123-127. doi: 10.1111/j.1532-5415.2004.52021.x [DOI] [PubMed] [Google Scholar]
- 9.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302. [PMC free article] [PubMed] [Google Scholar]
- 10.Soni A, Sabik LM, Simon K, Sommers BD. Changes in insurance coverage among cancer patients under the Affordable Care Act. JAMA Oncol. 2018;4(1):122-124. doi: 10.1001/jamaoncol.2017.3176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blavin F, Karpman M, Kenney GM, Sommers BD. Medicaid versus marketplace coverage for near-poor adults: effects on out-of-pocket spending and coverage. Health Aff (Millwood). 2018;37(2):299-307. doi: 10.1377/hlthaff.2017.1166 [DOI] [PubMed] [Google Scholar]
- 12.Williams J, Steers WN, Ettner SL, Mangione CM, Duru OK. Cost-related nonadherence by medication type among Medicare Part D beneficiaries with diabetes. Med Care. 2013;51(2):193-198. doi: 10.1097/MLR.0b013e318270dc52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Medication adherence and use of generic drug therapies. Am J Manag Care. 2009;15(7):450-456. [PMC free article] [PubMed] [Google Scholar]
- 14.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291(19):2344-2350. doi: 10.1001/jama.291.19.2344 [DOI] [PubMed] [Google Scholar]
- 15.Choudhry NK, Avorn J, Glynn RJ, et al. ; Post-Myocardial Infarction Free Rx Event and Economic Evaluation (MI FREEE) Trial . Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365(22):2088-2097. doi: 10.1056/NEJMsa1107913 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Additional Details on Methods
eTable. Characteristics of Stroke Survivors, by Age Group and Time: National Health Interview Survey, 2000-2016
eReferences