Abstract
Objective: To study radiographic and clinical outcomes after transforaminal lumbar interbody fusion (TLIF) in order to determine the impact of TLIF on lumbar lordosis, intervertebral height and improvement in clinical outcome measures.
Methods: Forty‐five patients who had undergone a single‐level TLIF procedure for a single‐level degenerative condition were retrospectively reviewed and their clinical histories, degree of pre‐ and post‐operative lumbar lordosis, intervertebral height, and cage position recorded. Clinical assessment included use of modified Odom's criteria and a visual analog scale (VAS) for back and leg pain.
Results: At 21 months, the patients had gained an average of 3.6° of lumbar lordosis and 4.5 mm disc height. Change in disc height was significantly associated with an anterior cage position while lumbar lordosis was unaffected by cage position. A spondylolisthesis subgroup demonstrated 31% reduction in the magnitude of anterior slip. Less lordosis was associated with worse back and leg pain as assessed by VAS and greater disk heights were associated with higher Odom's criteria scores. Patients with persistent leg pain at final follow‐up had less lumbar lordosis and intervertebral height than patients without leg pain.
Conclusions: Intervertebral height and lumbar lordosis reconstruction are important for achieving good surgical results; guidance regarding the likely changes in lumbar lordosis and disk height after TLIF is provided by our findings.
Keywords: Intervertebral disc, Lordosis, Spinal fusion, Spondylolisthesis
Introduction
A common goal of lumbar spinal surgery is to improve or restore sagittal alignment. Loss of lumbar lordosis is common in degenerative lumbar pathology secondary to disk space collapse. Loss of lumbar lordosis associated with positive sagittal balance has been repeatedly identified as a factor which is strongly associated with patient dissatisfaction 1 , 2 , 3 , 4 , 5 and contributes to the development of flat‐back syndrome 6 , 7 , 8 . Additionally, both clinical and biomechanical investigations suggest that restoration of lumbar lordosis may decrease rates of adjacent segment disease (ASD) 9 , 10 , 11 , 12 .
A recent meta‐analysis suggests that circumferential fusion results in higher fusion rates than posterolateral fusion, making use of an intervertebral cage increasingly attractive 13 . For patients with spondylolisthesis, circumferential fusion has been shown to result in both increased fusion rates and improved patient‐reported outcomes 13 . Restoration of disk height with an intervertebral device can increase lumbar lordosis through differential distraction of the anterior column and can also indirectly decompress the neural foramen, further relieving lateral recess and/or foraminal stenosis. Numerous strategies for providing intervertebral structural support have been developed with varying cage designs and surgical approaches including anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion, transforaminal lumbar interbody fusion (TLIF) and lateral transpsoas interbody fusion. Given the importance of sagittal alignment and nerve root decompression, in order to optimize preoperative planning spinal surgeons require accurate guidance regarding the effect a given procedure will have on lumbar lordosis and intervertebral height.
The purpose of this investigation was to study a cohort of patients who had undergone single‐level TLIF to answer the following research questions:
-
1
How does TLIF affect lumbar lordosis and does lordosis vary with cage position and spinal level?
-
2
How effectively does TLIF increase disk height and does intervertebral height vary with cage position and level?
-
3
For the subset of patients with spondylolisthesis, what percentage of vertebral body translation is corrected through ligamentotaxis associated with TLIF cage placement?
-
4
Does improvement in lumbar lordosis and increased disk height result in better clinical outcomes?
Materials and methods
This study conforms to the provisions of the Declaration of Helsinki and was approved by the Institutional Review Board, who granted a waiver of informed consent. We retrospectively identified all patients who had undergone a single‐level TLIF procedure for the treatment of a single‐level degenerative lumbar condition between February 2004 and May 2006 at a single institution. Patients were eligible for inclusion if they had undergone single‐level TLIF (Leopard cage, DePuy Spine, Raynham, MA, USA) with posterior instrumentation (Expedium system, DePuy Spine) performed under the same anaesthetic, both preoperative and postoperative standing radiographs had been taken and they had attended for at least 1 year of postoperative follow‐up. Patients were excluded if they had undergone previous spinal instrumentation and/or fusion of the spinal segment instrumented on this most recent surgery. TLIF was performed by one of two senior attending spine surgeons using cages without any built‐in lordotic angulation of the cage endplates. Discectomy was performed using chondrotomes, curved and straight curettes and serial blunt dilators. Shavers were not used, the intention being to avoid injury to the vertebral endplates.
Forty‐five patients were identified using the criteria listed above. Relevant patient variables, medical and surgical history, and implants used were recorded from the patients' hospital and office charts. Preoperative, immediate postoperative, and most recent postoperative standing lumbar anteroposterior (AP), neutral lateral and flexion and extension lateral radiographs were reviewed to obtain the following measurements: degree of lumbar lordosis from L2 to S1, posterior disk height, distance of the interbody cage from the front of the disk space, and vertebral body translation for patients with spondylolisthesis(Fig. 1). Cage position and vertebral body translation were measured as a percentage of the anteroposterior diameter of the cranial vertebral body to allow for variation in vertebral size. Cage position was measured using metallic markers within the cage that demarcated its anterior border and was measured with reference to the distance from the anterior border of the adjacent vertebra. Successful fusion was assumed where previously described radiographic criteria were met 14 , 15 , 16 : bridging trabecular bone present between vertebrae, no radiolucent halos surrounding pedicle screws on anteroposterior and lateral radiographs, and less than 3 mm of translation and 5° of angulation on flexion/extension lateral radiographs.
Figure 1.
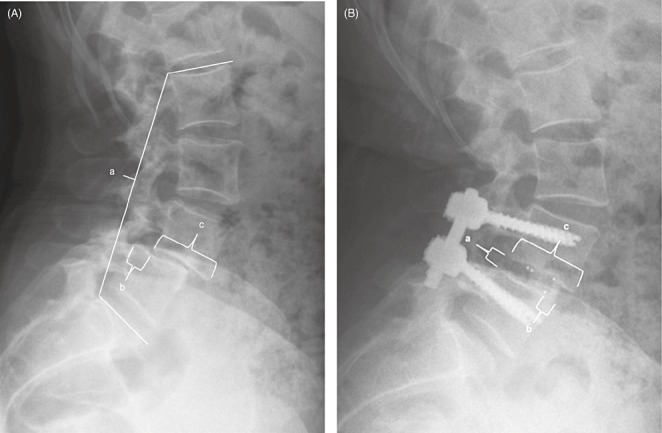
(A) Preoperative and (B) postoperative lateral radiographs demonstrating the various measurements used. (A) Preoperative measurements as follows: (a) L2‐S1 lordosis; (b) amount of anterolisthesis; and (c) cranial vertebral body width. (B) Postoperative measurements as follows: (a) posterior disc height; (b) distance of cage from anterior aspect of vertebral body; and (c) cranial vertebral body width.
The clinical outcome was assessed using questionnaires that included modified Odom's criteria 17 , a visual analog scale (VAS) for back and leg pain, and patient satisfaction questions.
Statistical analysis
Statistical analysis was performed with SPSS 16.0 (SPSS, Chicago, IL, USA). Comparison of means was performed using Student's t‐test between two groups and analysis of variance when more than two groups were compared for continuous variables that passed the Shapiro‐Wilk test for normality. Preoperative and postoperative values from the same patients were compared using a paired Student's t‐test. Comparison of means for continuous variables that did not pass the Shapiro‐Wilk test for normality or non‐parametric variables was performed between two groups using the Mann‐Whitney U‐test and between more than two groups using the Kruskal‐Wallis test. Association between variables was assessed using Pearson's correlation coefficient for continuous, normal variables and Spearman's correlation coefficient for non‐parametric variables (both correlation coefficients denoted by ρ). Statistical significance was assumed for P values < 0.05 in all cases.
Results
Patient characteristics
The 45 patients in this study included 23 men and 22 women with an average age of 47.3 years (range, 25–77). Nine patients had undergone surgery for degenerative disk disease, 20 for Grade I degenerative or isthmic spondylolisthesis, 10 for recurrent herniated nucleus pulposus and 6 for lumbar stenosis with degenerative scoliosis. Two patients had undergone fusion at L2‐L3 (4%), 3 at L3‐L4 (7%), 22 at L4‐L5 (49%), and 18 at L5‐S1 (40%). Autologous bone grafting was used in 15 patients while the remaining 30 patients underwent surgery using bone morphogenetic protein; discussion of the off label nature of bone morphogenetic protein had been included in their informed consent.
Radiographic outcomes
Radiographic follow‐up averaged 21.2 months; final follow‐up 96% of patients had achieved spinal fusion according to the criteria described above. Preoperative lumbar lordosis averaged 39.2° (range, 5°–56°). Initial postoperative lumbar lordosis averaged 43.9° (range 10°–65°) and lumbar lordosis at most recent follow‐up averaged 42.8° (range, 11°–65°) (Table 1). Average lumbar lordosis measurements on preoperative, immediate postoperative and final postoperative radiographs were all statistically significantly different from one another (P < 0.001) based on pairwise analysis using Student's t‐test, a method which helped to analyze the effect of surgery despite a wide variation in preoperative lordosis. Lordosis at final follow‐up did not correlate with surgical level (P= 0.82), sex (P= 0.72), cage position (P= 0.45), or age (P= 0.73). Similarly, change in lordosis did not vary significantly with spinal level (P= 0.50), sex (P= 0.24), cage position (P= 0.23) or age (P= 0.28).
Table 1.
Average radiographic measurements
| Variable | Preoperative | Immediate postoperative | Final postoperative | P value* |
|---|---|---|---|---|
| Entire Cohort | ||||
| Lumbar lordosis | 39.2° | 43.9° | 42.8° | P < 0.001 |
| Disc height (mm) | 5.3 | 10.3 | 9.8 | P < 0.001 |
| Spondylolisthesis subgroup | ||||
| Percent translation | 20% | — | 13.6% | P < 0.001 |
Denotes significance level between preoperative and final postoperative measurements.
Preoperative disk height averaged 5.3 mm (range, 1–12 mm). Postoperative disk height averaged 10.3 mm (range, 6–14 mm) initially, and 9.8 mm (range, 6–14 mm) at most recent follow‐up (Table 1) after an average cage subsidence of 0.5 mm/level. Three patients (6.7%) had subsidence of 2 mm or more. Average disk height measurements between preoperative, immediate postoperative and final postoperative radiographs were all statistically significantly different from one another (P < 0.001) based on analysis using the paired Student's t‐test. Final disk height was 1 mm greater in men than in women (P= 0.01), a finding which is mitigated by the fact that preoperative disk height was also greater in men by about 1 mm. Disk height at final follow‐up did not vary significantly by spinal level (P= 0.47), age (P= 0.9) or cage position (P= 0.68). Change in disk height was significantly positively correlated with anteroposterior cage position (ρ=−0.37, P= 0.01). The negative value of the correlation means that the more anteriorly a cage is situated (lower value of cage position based on our convention), the greater the expected postoperative increase in disk height. Change in disk height was not significantly associated with spinal level (P= 0.77), sex (P= 0.66), or age (P= 0.21).
Spondylolisthesis subset
The subset of patients with spondylolisthesis had greater preoperative, immediate postoperative and final postoperative lordosis by ∼6° at each time point (P < 0.01) compared to the greater cohort but a similar amount of increase in lordosis associated with surgery (4.3° for spondylolisthesis patients vs. 3.7° overall, P= 0.59). Disk height was similar in patients with spondylolisthesis and patients without spondylolisthesis at all time points (P > 0.15), as was overall change in disk height (P= 0.25) and cage placement (P= 0.5). Preoperative slip percentage averaged 20% and this decreased to 13.6% postoperatively (P < 0.001), representing an improvement of 31% (Table 1). There was no significant association between slip improvement and age (P= 0.63), sex (P= 0.29), or cage position (P= 0.18). There were no significant differences between patients with degenerative spondylolisthesis and those with isthmic spondylolisthesis in any variable (P > 0.10 for all comparisons).
Clinical outcomes
Overall, the average postoperative Odom's criteria score was 3.0 for the general cohort and 2.9 in patients with spondylolisthesis. In total, 32 patients (71.4%) had either “excellent” or “good” outcomes. The average final back pain VAS score was 2.3 (standard deviation, 2.6) and average final leg pain VAS score was 2.0 (standard deviation, 3.0).
Using Spearman's correlation, Odom's criteria score correlated significantly with final disk height (ρ= 0.33, P= 0.05) meaning patients with greater disk heights tended to do better. However,s leg pain VAS scores demonstrated a strong trend toward being negatively correlated with final disk height but this trend failed to reach significance (ρ=−0.32, P= 0.06). Both back and leg pain VAS scores demonstrated significant negative correlations with lumbar lordosis (ρ=−0.42, P= 0.01 and ρ=−0.36, P= 0.03, respectively), meaning that patients with greater lumbar lordosis at final follow‐up had significantly less back and leg pain. Patients with continued leg pain at final follow‐up had smaller disk heights (difference = 1.5 mm, P= 0.03) and less lordosis (difference = 9°, P= 0.01) than patients whose pain had resolved by final follow‐up. Although final lordosis and disc heights were associated with improved results, changes in lordosis and disk height did not have statistically significant relationships with any of the outcome measures.
Discussion
Transforaminal lumbar interbody fusion increased lumbar lordosis by 3.6° on average and disk height by 4.5 mm on average, both significant differences. Although lumbar lordosis did not change with cage position, anterior cage placement was significantly correlated with increased disk height at most recent follow‐up. Patient variables such as sex and age did not affect the amount of lumbar lordosis or disk height achieved. Patients with greater final lumbar lordosis and disk height had better outcomes as assessed by Odom's criteria and lack of persistent postoperative leg and back pain. However, perioperative change in lordosis and change in disk height were not associated with improved results.
Previous studies have provided guidance on the amount of lordosis that can be expected after TLIF. Hsieh et al. found that TLIF actually slightly decreased lumbar lordosis as measured by both overall lumbar lordosis and local disk angle 18 . This was in contrast to patients in the same series treated with ALIF, which increased overall lumbar lordosis by 6.2°. Lee et al. reported segmental increase in lordosis of 2° but a non‐significant overall increase in lumbar lordosis of only 1.5° after TLIF 19 . Finally, Kim et al. found a non‐significant increase in segmental lordosis of 2° and a significant overall lumbar lordosis of 3° after TLIF in 25 patients 20 . While these series reported only modest changes in lumbar lordosis after TLIF, Janannathan et al. reported an average increase in lumbar lordosis of 19° after TLIF at an average of 1.25 levels/patient 21 . This is substantially larger than reported in any other series and is attributed by the authors to far anterior placement of interbody grafts and a surgical technique which frequently incorporated bilateral facetectomies to allow for greater restoration of lordosis, a technique which was not routinely performed in our patients.
Posterior disk height increased an average of 4.5 mm in our series, an important radiographic variable because of the prospect for indirect foraminal decompression with distraction across the disk space. Between initial follow‐up and final follow‐up, patients lost 0.5 mm of disk space height. In comparison, Hsieh et al. described an average posterior disk height increase of 0.8 mm per level but did not measure subsidence between initial and final follow‐up 18 . Kim et al. found overall disk space increases of 1.8 mm per level after an initial subsidence of 0.75 mm from that shown on immediate postoperative radiographs 20 . Janannathan et al. described a net average disk space increase of 2.3 mm per level at final follow‐up after subsidence of 0.7 mm 21 . We suspect that a concerted effort to aggressively restore disk height and decompress the neural foramen via cage selection is responsible for the relatively large magnitude of the disk height restoration in our study.
Although cage position was not associated with changes in lumbar lordosis, anterior positioning of cages was associated with greater gains in intervertebral disk space height. This is somewhat counterintuitive because we measured disk height in the posterior portion of the disk. Thus it could be expected that posterior placement of cages might have a more immediate and local effect on the posterior disk space. Surgeons are likely reluctant, however, to place cages posteriorly, where they might impinge on neural elements or lead to increasing kyphosis. Cages, therefore, tend to be placed in the anteroposterior middle of the vertebral body, where the concavity of adjacent endplates reduces the effective distraction across the disk space, or anteriorly, where the cage has the benefit of being at the edge of both concavities and can more effectively distract the intervertebral space and increase segmental lordosis. Another explanation for this finding is that when greater distraction can be achieved with a laminar spreader, larger cages can be placed in more anterior positions within the disc space. Thus, these two technical factors are linked and together result in a greater increase in disc height when a (larger) cage has been placed more anteriorly.
The subgroup of patients with spondylolisthesis achieved equivalent results to the remaining cohort despite the approximately 10° greater lumbar lordosis in this subset at all time points. In addition to gaining 4.3° of lordosis and 4.2 mm of intervertebral height through the procedure, patients with spondylolisthesis had an average reduction of vertebral body translation at the instrumented level of ∼2.7 mm, representing 31% of their preoperative listhesis. This finding is consistent with the findings of Kwon et al. who described a cohort of 35 patients with degenerative spondylolisthesis treated with single level TLIF with 36% reduction in preoperative listhesis 22 .
This study demonstrates the importance of intervertebral height and lumbar lordosis for achieving good surgical results. Patients with greater lumbar lordosis had significantly less back and leg pain at final follow‐up and those with greater intervertebral disk space height had significantly higher scores on modified Odom's criteria and less leg pain. At the same time, our results highlight the difficulty faced by spinal surgeons treating patients with substantial loss of lumbar lordosis and disk height through degenerative disease processes. While final lumbar lordosis and disk height were associated with improved results, the size of perioperative increases in lordosis and disk height had no significant associations, suggesting that patients with greatly decreased lordosis and intervertebral disk space height will be less likely to achieve satisfactory postoperative results. In this respect, our inclusion of patients who underwent fusion at a single level is a limitation of the study. Patients who undergo multilevel operations are more likely to have larger improvements in postoperative lumbar lordosis than has been shown in our single‐level study. A study design incorporating multilevel surgery would allow for greater restoration of lordosis and increase the likelihood of showing a significant association between improvement in lumbar lordosis and clinical outcome.
In conclusion, we sought to identify patient‐ and technique‐dependent factors associated with increases in intervertebral disk space height and lumbar lordosis and to provide guidance as to the likely extent of increases in lumbar lordosis and disk height after single‐level TLIF. Patient variables were not associated with improved radiographic or clinical outcomes. Whereas measures of lumbar lordosis were independent of cage position, anterior cage position was associated with greater postoperative intervertebral disk height. Greater final lumbar lordosis and intervertebral disk height were both associated with improved clinical outcomes, reinforcing the importance of restoring these variables at the time of spinal reconstruction.
Disclosure
The authors have no financial conflicts of interest relevant to the subject of this manuscript.
References
- 1. Schwab FJ, Smith VA, Biserni M, et al Adult scoliosis: a quantitative radiographic and clinical analysis. Spine, 2002, 27: 387–392. [DOI] [PubMed] [Google Scholar]
- 2. Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop, 2003, 32: 77–82. [PubMed] [Google Scholar]
- 3. Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg, 2003, 11: 174–183. [DOI] [PubMed] [Google Scholar]
- 4. Berven SH, Deviren V, Mitchell B, et al Operative management of degenerative scoliosis: an evidence‐based approach to surgical strategies based on clinical and radiographic outcomes. Neurosurg Clin N Am, 2007, 18: 261–272. [DOI] [PubMed] [Google Scholar]
- 5. Ploumis A, Liu H, Mehbod AA, et al A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine, 2009, 34: 1581–1584. [DOI] [PubMed] [Google Scholar]
- 6. Kostuik JP, Maurais GR, Richardson WJ, et al Combined single stage anterior and posterior osteotomy for correction of iatrogenic lumbar kyphosis. Spine, 1988, 13: 257–266. [DOI] [PubMed] [Google Scholar]
- 7. La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am, 1988, 19: 383–393. [PubMed] [Google Scholar]
- 8. Swank SM, Mauri TM, Brown JC. The lumbar lordosis below Harrington instrumentation for scoliosis. Spine, 1990, 15: 181–186. [DOI] [PubMed] [Google Scholar]
- 9. Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J, 2001, 10: 314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen WJ, Lai PL, Tai CL, et al The effect of sagittal alignment on adjacent joint mobility after lumbar instrumentation—a biomechanical study of lumbar vertebrae in a porcine model. Clin Biomech (Bristol, Avon), 2004, 19: 763–768. [DOI] [PubMed] [Google Scholar]
- 11. Kim KH, Lee SH, Shim CS, et al Adjacent segment disease after interbody fusion and pedicle screw fixations for isolated L4‐L5 spondylolisthesis: a minimum five‐year follow‐up. Spine, 2010. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 12. Umehara S, Zindrick MR, Patwardhan AG, et al The biomechanical effect of postoperative hypolordosis in instrumented lumbar fusion on instrumented and adjacent spinal segments. Spine, 2000, 25: 1617–1624. [DOI] [PubMed] [Google Scholar]
- 13. Kwon BK, Hilibrand AS, Malloy K, et al A critical analysis of the literature regarding surgical approach and outcome for adult low‐grade isthmic spondylolisthesis. J Spinal Disord Tech, 2005, 18: S30–S40. [DOI] [PubMed] [Google Scholar]
- 14. Brodsky AE, Kovalsky ES, Khalil MA. Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine, 1991, 16 (Suppl. 6): S261–S265. [DOI] [PubMed] [Google Scholar]
- 15. McAfee PC, Boden SD, Brantigan JW, et al Symposium: a critical discrepancy—a criteria of successful arthrodesis following interbody spinal fusions. Spine, 2001, 26: 320–334. [DOI] [PubMed] [Google Scholar]
- 16. Burkus JK, Dorchak JD, Sanders DL. Radiographic assessment of interbody fusion using recombinant human bone morphogenetic protein type 2. Spine, 2003, 28: 372–377. [DOI] [PubMed] [Google Scholar]
- 17. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc, 1958, 166: 23–28. [DOI] [PubMed] [Google Scholar]
- 18. Hsieh PC, Koski TR, O'Shaughnessy BA, et al Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine, 2007, 7: 379–386. [DOI] [PubMed] [Google Scholar]
- 19. Lee DY, Jung TG, Lee SH. Single‐level instrumented mini‐open transforaminal lumbar interbody fusion in elderly patients. J Neurosurg Spine, 2008, 9: 137–144. [DOI] [PubMed] [Google Scholar]
- 20. Kim SB, Jeon TS, Heo YM, et al Radiographic results of single level transforaminal lumbar interbody fusion in degenerative lumbar spine disease: focusing on changes of segmental lordosis in fusion segment. Clin Orthop Surg, 2009, 1: 207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jagannathan J, Sansur CA, Oskouian RJ Jr, et al Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery, 2009, 64: 955–963. [DOI] [PubMed] [Google Scholar]
- 22. Kwon BK, Berta S, Daffner SD, et al Radiographic analysis of transforaminal lumbar interbody fusion for the treatment of adult isthmic spondylolisthesis. J Spinal Disord Tech, 2003, 16: 469–476. [DOI] [PubMed] [Google Scholar]


