Abstract
Objective
To evaluate the effect of surgical treatment on health related quality of life (HRQOL) and radiographic variables in patients with adult scoliosis.
Methods
Sixty‐eight patients with adult spinal deformities underwent radiographic analysis. The enrollment criteria were as follows: age older than 18 years, adult degenerative or progressive idiopathic scoliosis (Cobb angle >10°), and surgical treatment within one year before this study was undertaken. The following variables were measured: curve type, apical level, curve magnitude, coronal and sagittal balance using a C7 plumb line (C7PL) and gravity line, lateral intervertebral olisthesis, lumbar lordosis, sacral slope and pelvic tilt. HRQOL was assessed by the Oswestry Disability Index (ODI). Both preoperative and postoperative data were collected and changes in radiographically assessed variables and ODI scores attributable to surgery calculated; correlations between these changes were then assessed. The radiographically assessed variables and ODI scores were analyzed with SigmaStat (SPSS, Chicago, IL, USA). The level of statistical significance was set at P < 0.05.
Results
Surgical treatment resulted in improvements in ODI scores and several radiographically assessed variables, including sagittal balance, lumbar lordosis, lateral olisthesis and coronal Cobb angle. Only sagittal balance expressed as C7PL was correlated to both preoperative and postoperative ODI. Gravity line, an alternative measurement of spinal balance, did not provide better correlations with HRQOL than C7PL.
Conclusions
Spinal balance assessed by gravity line did not provide a better correlation with HRQOL than C7PL. Loss of sacral slope and retroverted pelvis are commonly seen in adult scoliosis and are not significantly changed by surgical treatment, including restoration of lumbar lordosis and sagittal balance.
Keywords: Adult spinal deformity, Gravity line, Quality of life
Introduction
Adult spinal deformity may involve both the deformity itself and degeneration in the spine. Although there are many different causes of adult spinal deformity, most patients can be categorized as having adult scoliosis of adolescent onset (ASAO) or de novo degenerative scoliosis (DDS). ASAO is an idiopathic type of scoliosis that begins to develop in adolescence and progresses with age. Unlike ASAO, DDS is usually secondary to degenerative diseases, especially diseases of the disc. In both types of scoliosis, the curves may progress as the patient ages. The prevalence of asymptomatic adult scoliosis varies between 2%–32%1. The prevalence of adult deformity can be as high as 60% in persons aged more than 60 years2. With the aging population of modern society, adult deformity has becoming a significant healthcare problem. Although most adult patients with spinal deformity have only cosmetic concerns or minor symptoms that can be addressed by conservative treatments, many patients need surgical intervention because of disabling pain, progressing curves and cardiopulmonary symptoms. Surgical treatment has been shown to provide significant improvements in the deformities, pain and fatigue, and the ability to perform physical and positional tasks3.
Compared with adolescent idiopathic scoliosis, there is little published research and clinical data on adult scoliosis. Systematic classifications of adult deformity have only recently been proposed4, 5. Several radiographically assessed variables, namely sagittal balance6, 7, apical level of the major curve4, lumbar subluxation8 and lumbar lordosis9, have been identified as the most significant factors that affect patients’ health status. These variables have been incorporated into the classification system as modifiers for guiding surgery and predicting treatment outcome. However, most of these variables have only been correlated with preoperative health status. Few studies have reported how these radiographically assessed variables influence treatment outcomes in patients with adult scoliosis. The purpose of this study was to evaluate changes in these variables following spinal surgery and their correlation with patients’ health status.
In addition to the routine radiographically assessed variables listed in the previous paragraph, the gravity line (GL) position relative to spinal anatomy has been introduced for assessing spinal balance. Because the spine bears upper body weight, this measurement has physical significance. Many studies have suggested it differs from the C7 plumb line (C7PL). Because spinal balance has been shown to be one of the most significant predictors of patients’ health status6, 7, it is potentially a useful measurement. However, it is unclear whether the GL provides a better guide than the C7PL for surgical decision making. A recent study has shown that a GL greater than 5 cm is correlated with poor health status10. In this study, the GL was also measured both preoperatively and postoperatively to determine whether it correlates better than the other measures with the patient's health status.
Patients and Methods
This is an institutional review board approved retrospective study of 68 consecutive patients with adult scoliosis attending a single institution within the past two years. The enrollment criteria were as follows: age older than 18 years, adult degenerative or progressive idiopathic scoliosis (Cobb angle >10°), and surgical treatment within one year before this study was undertaken. The exclusion criteria were neuromuscular, congenital, or post‐traumatic scoliosis. The 68 patients comprised 50 women and 18 men of mean age 58.5 ± 13.8 years (range, 20–88 years). Twenty‐one patients had idiopathic scoliosis and 47 degenerative scoliosis. The mean follow‐up time was 7.9 months (range, 6–14 months). Twenty‐seven patients had undergone osteotomy procedures (Smith–Petersen osteotomy or pedicle subtraction osteotomy); their mean age was 57.7 ± 11.0 years (range, 23–73 years). The remaining patients had undergone either posterior only or combined anterior and posterior instrumentation. Thirty‐nine of the patients (57%) had undergone surgery prior to the surgery required for enrollment in this study.
All patients had full spine posteroanterior (PA) and lateral standing radiographs. GL position relative to each subject's spinal anatomy was assessed with a force plate that measured the ground reaction forces during radiographic acquisition10. A moving radio‐opaque marker that was automatically driven by the force plate placed a triangular mark on each X‐ray image. The position of this mark indicated the instantaneous location of the GL when the radiograph was taken. The coronal and sagittal balance measured by GL was referenced to the vertical line running through the center of one (or two) femoral head centers (CFH) as defined by O'Brian11. Spinal balance measured by C7PL was referenced to the traditional landmark, namely, the center sacral vertical line (CSVL) in the coronal plane and posterosuperior corner of S1 in the sagittal plane. Other deformity and pelvic variables measured in this study included Cobb angle, lumbar lordosis, coronal lateral olisthesis, sacral slope, and pelvic tilt. Most of these were measured using the techniques described in the Radiographic Measurement Manual11. Measurement of lateral olisthesis has been described elsewhere12. The measurement methods are shown in Table 1.
Table 1.
Radiologically assessed variables of balance derived from measurements on lateral and posteroanterior radiographs
| Variable | Description |
|---|---|
| Sagittal balance | Assessment from lateral radiograph |
| Sagittal C7PL (mm) | Distance between C7P and posterosuperior corner of S1 vertebral body * |
| Sagittal GL (mm) | Distance between GL and posterosuperior corner of S1 vertebral body * |
| Sagittal GL–CFH (mm) | The horizontal distance between the GL and the center of the bicoxofemoral axis† |
| Lumbar lordosis Cobb angle (°) | The angle between the superior end plate of T12 and the superior end plate of S1 |
| Coronal balance | Assessment from posteroanterior radiograph |
| Coronal C7PL (mm) | Distance between C7PL and central sacral vertebral line‡ |
| Coronal GL (mm) | Distance between GL and central sacral vertebral line‡ |
| Coronal GL–CFH (mm) | The horizontal distance between the GL and the center of the bicoxofemoral axis§ |
| Lateral olisthesis (mm) | Relative to the lower vertebral body, the upper vertebral body lateral slip distance |
| Pelvic variables | Assessment from lateral radiograph |
| Pelvic incidence (PI, °) | Angle between the line perpendicular to the S1 end plate at its midpoint and the line connecting this point to the middle axis of the femoral heads |
| Sacral slope (SS, °) | Angle between the line connecting the superior end plate of S1 and a horizontal line |
| Pelvic tilt (PT, °) | Angle between the line connecting the midpoint of the sacral plate to the middle axis of femoral heads and a vertical line |
Note: *, positive when in front of the posterosuperior corner of the S1 vertebral body; †, positive when in front of the CFH, negative when behind the CFH; ‡, positive when to the right of the central sacral vertebral line; §, positive when to the right of the CFH. CSVL, central sacral vertebral line; SSVL, sagittal sacral vertical line (posterosuperior corner of S1 vertebral body).
All patients completed Oswestry Disability index (ODI) questionnaires to assess their preoperative and postoperative health related quality of life (HRQOL). The radiographically assessed variables and ODI scores were analyzed with SigmaStat (SPSS, Chicago, IL, USA). Analysis of correlations between all radiologically assessed variables and ODI scores was performed using Pearson coefficients. Preoperative and postoperative ODI scores and radiographically assessed variables were compared with Student's paired t‐test. The level of statistical significance was set at P < 0.05.
Results
Using the apical level as the criterion for classification of adult spine deformity4, one patient had type I, three type II, four type III, 29 type IV and 31 type V. Hence, the majority of patients had either lumbar or thoracolumbar apical levels. The mean preoperative ODI score was 50.6 ± 16.8 and the postoperative ODI score 41.1 ± 19.6; this decrease was statistically significant according to Student's paired t‐test (P ≤ 0.001). Forty‐six patients (68%) had sagittal imbalance of more than 4 cm. Of these patients, 26 had undergone either Smith–Peterson osteotomy or pedicle subtraction osteotomy. The mean sagittal balance measured by C7PL had improved from 115 mm to 63.7 mm in the 26 patients who had undergone these osteotomy procedures. Other surgical treatments were posterior fusion and combined anterior and posterior fusion. The mean Cobb angle had decreased from 26° preoperatively to 10.7° postoperatively.
Lateral olisthesis had decreased from 4.9 mm to almost zero in most patients. Most patients had lost the sacral slope and retroverted pelvis (high pelvic tilt). Although the sacral slope increased postoperatively, the difference was very small (less than 2° on average). There was almost no change in pelvic tilt after surgery. All preoperative and postoperative measurements of radiographically assessed variables are shown in Table 2.
Table 2.
Mean value (standard deviation) of radiologically assessed variables for all patients (mean ± s.d.)
| Variable | Preoperative | Postoperative | P value |
|---|---|---|---|
| Sagittal balance | |||
| Sagittal C7PL (mm) | 84.5 ± 80.3 | 56.7 ± 64.7 | 0.001 |
| Sagittal GL–CFH (mm) | 12.0 ± 44.4 | −4.8 ± 25.3 | 0.002 |
| Coronal balance | |||
| Coronal C7PL (mm) | 8.7 ± 34.0 | 9.1 ± 25.6 | 0.88 |
| Coronal GL–CFH (mm) | −2.3 ± 29.5 | −1.2 ± 17.5 | 0.72 |
| Pelvic variables | |||
| Sacral slope (°) | 27.8 ± 9.6 | 29.4 ± 8.7 | 0.01 |
| Pelvic tilt (°) | 25.9 ± 9.6 | 25.8 ± 8.4 | 0.84 |
| Other variables | |||
| Cobb angle (°) | 26.0 ± 18.6 | 10.7 ± 13.8 | 0.001 |
| Lumbar lordosis (°) | 35.6 ± 19.6 | 42.0 ± 17.1 | 0.01 |
| Coronal lateral olisthesis (mm) | 4.9 ± 6.1 | 0.1 ± 0.01 | 0.001 |
Pearson correlation was performed to assess correlations between the radiographically assessed variables and ODI scores. Only sagittal balance by C7PL was significantly correlated with ODI score both pre‐ and post‐operatively. However, the correlation was weak, both r values being less than 0.3. The GL was correlated only with ODI score postoperatively. The coronal balance measured either by C7PL or GL was not correlated with ODI score. The correlation data are shown in Table 3. In addition, none of the radiographic changes were correlated with improvement in ODI score. These findings suggest that correction of these radiographically assessed variables is not necessarily associated with relief of symptoms.
Table 3.
Preoperative and postoperative correlationd between ODI scores and radiographically assessed variables
| Radiographically assessed variable versus ODI score | Pre‐operative | Post‐operative | Change versus ΔODI | |||
|---|---|---|---|---|---|---|
| P | r | P | r | P | r | |
| Sagittal balance | ||||||
| C7PL | 0.03 | 0.27 | 0.03 | 0.28 | 0.47 | −0.09 |
| GL–CFH | 0.64 | 0.06 | 0.03 | 0.26 | 0.88 | −0.02 |
| Coronal balance | ||||||
| C7PL (abs) | 0.18 | 0.16 | 0.37 | 0.10 | 0.92 | 0.01 |
| GL–CFH (abs) | 0.45 | 0.09 | 0.57 | 0.07 | 0.69 | −0.05 |
| Pelvic variables | ||||||
| Sacral slope | 0.82 | −0.03 | 0.47 | −0.09 | 0.44 | −0.10 |
| Pelvic tilt | 0.06 | 0.23 | 0.73 | 0.04 | 0.08 | 0.21 |
| Other variables | ||||||
| Cobb angle | 0.03 | −0.26 | 0.40 | −0.10 | 0.81 | −0.03 |
| Lumbar lordosis | 0.67 | 0.05 | 0.004 | −0.35 | 0.54 | −0.08 |
| Coronal olisthesis | 0.16 | −0.17 | — | — | 0.22 | 0.15 |
Change/ΔODI refers to the correlation between changes in radiologically assessed variables and in ODI scores as a result of surgery. Abs, absolute values.
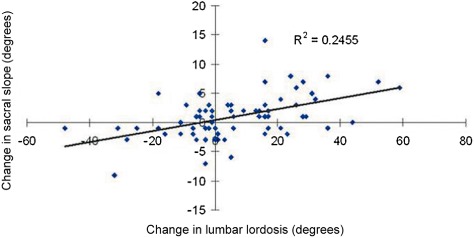
Spinal balance was assessed both by C7PL and GL. Because published reports suggest that spinal balance is the most significant radiographic variable, these values are presented in greater detail here. The coronal data are presented in Fig. 1A and B and the sagittal data in Fig. 2A and B. In the coronal plane, both preoperative and postoperative C7PL values were rather scattered. The standard deviation of the GL was much smaller postoperatively, approximately half of its preoperative value. In the coronal plane, the GL appeared to converge to the CFH after surgery. This means that the gravitational balance, that is, the weight distribution on the hips and legs, was improved after surgery. However, this change did not appear to correlate with ODI scores. In the sagittal plane (shown in Fig. 2A and B), C7PL values were also scattered. Although statistically significant, the correlation between C7PL and ODI score is weak. The GL was much more concentrated around the CFH, especially postoperatively (Fig. 2B). This is because the upper body is supported by the legs through the hip joints. However, this measure of gravitational balance was only weakly correlated with ODI scores postoperatively.
Figure 1.

(A) Coronal C7 plumb line (C7PL) versus Oswestry Disability Index (ODI) scores. Both preoperative and postoperatively C7PL was scattered. (B) Coronal gravity line (GL)‐femoral head centers (CFH) versus ODI scores. The GL converges to CFH postoperatively.
Figure 2.
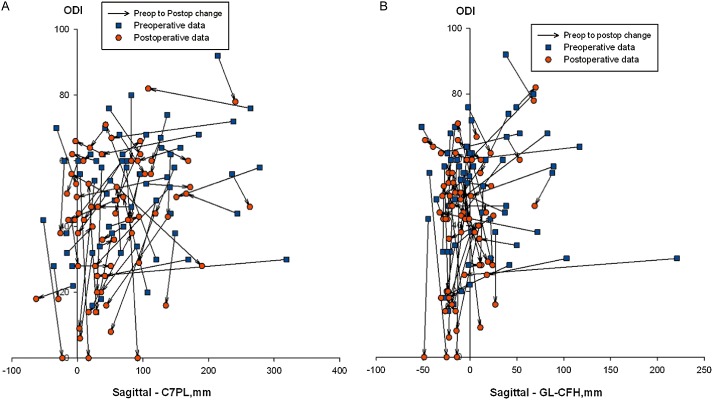
(A) Sagittal C7 plumb line (C7PL) versus Oswestry Disability Index (ODI) scores. Both preoperative and postoperatively C7PL was scattered. (B) Sagittal gravity line (GL)‐femoral head centers (CFH) versus ODI scores was much more concentrated around CFH postoperatively.
Changes in pelvic variables due to surgical treatment are shown in Figs 3 and 4. The increase of sacral slope was correlated with the improvement of sagittal balance. However, the correlation was weak, the r value being 0.36. The correlation was stronger between the increase in sacral slope and increase in lumbar lordosis, as shown in Fig. 4. Overall, the change in sacral slope was small. Based on the prediction using the linear regression line shown in Fig. 4, to achieve 5° of sacral slope, lumbar lordosis must be improved by more than 40°. Because pelvic incidence does not change postoperatively, the change in sacral slope should be equal in magnitude to the change in pelvic tilt. Because the change in sacral slope was small and there is some radiographic measurement error, no difference was detected between preoperative and postoperative pelvic tilt.
Figure 3.
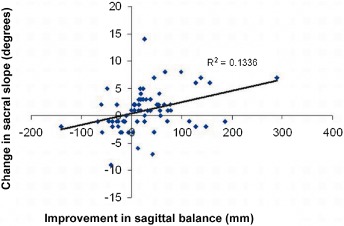
Postoperative improvement in sagittal balance (C7PL) according to change in sacral slope. Improvement refers to a decrease in sagittal balance. Pearson correlation coefficient r = 0.36.
Figure 4.
Postoperative change in sacral slope according to change in lumbar lordosis. Pearson correlation coefficient r = 0.5.
Discussion
Surgical treatment of adult spine deformity is a challenging task for spine surgeons because of its complexity, multiple pathologies and symptoms, and compromised bone density in elderly patients. Several studies have proposed using radiographically assessed variables as surgical guidelines13. Hence, it is important to identify any correlations between clinical health statuses and these radiographic measurements so that treatment outcome can be predicted preoperatively. Recent studies have suggested that sagittal balance, lumbar lordosis, lateral olisthesis and pelvic variables may affect a patient's HRQOL8, 14, 15. However, these studies did not show whether correction of these radiographically assessed variables lead to improved health status postoperatively. In this study, we evaluated how changes in these variables influence the treatment outcome. After all, how much improvement or symptom relief a particular surgery can give a patient is an important factor to consider preoperatively.
In this study, several radiographically assessed variables that have previously been reported to affect HRQOL were measured in patients with adult scoliosis. We found that the sagittal balance measured by C7PL was correlated with both pre‐ and post‐operative ODI score. However, the correlation was weak, the r value being <0.3 using Pearson correlation. Cobb angles were related only to preoperative ODI score (r = −0.25). Lumbar lordosis was correlated only with postoperative ODI score (r = −0.34). None of the changes in radiographically assessed variables was correlated with improvement in ODI scores. In other words, improvement in the radiographically assessed variables did not necessarily lead to better postoperative health status. This finding suggests that treatment of patients with adult scoliosis should not be based only on these variables. Because the responsible pathologies are heterogeneous, radiographically assessed variables should only be used as general guidelines rather than reliable predictors of HRQOL.
Pelvic variables, such as pelvic incidence, sacral slope and pelvic tilt, have been studied primarily in asymptomatic volunteers, patients with adolescent idiopathic scoliosis, and patients with high grade spondylolisthesis16, 17, 18, 19, 20, 21, 22. Only recently have these variables been investigated in adult scoliosis14, 23. Preoperative ODI scores have been correlated with pelvic tilt14. Similar results were obtained in this study; however, the correlation coefficient was low (r = 0.23). Surprisingly, the new data obtained in this study showed no correlation between postoperative pelvic tilt and ODI scores. Hence, according to our findings, pelvic tilt is not a good predictor of surgical outcome. Detailed examination of our data showed that most patients in this study had little change in pelvic tilt postoperatively, even when their sagittal imbalance had been corrected or lumbar lordosis increased. These findings differ from those reported for another type of adult degenerative disease referred to as lumbar degenerative kyphosis, in which a mean correction of 17° in pelvic tilt or sacral slope can be achieved postoperatively24. In developmental high grade spondylolisthesis, pelvic tilt may also increase significantly in patients whose preoperative pelvic tilt is greater than normal. In this cohort of patients, the mean preoperative sacral slope and pelvic tilt were 27.8° and 25.9°, respectively, compared with 42° and 18°, respectively, in asymptomatic elderly subjects (age >70 years)24, and 42° and 12°, respectively, in younger subjects (mean age 30 years)16. Hence, in patients with adult scoliosis, these pelvic parameters can deviate significantly from normal values. Unfortunately, surgical treatment did not correct this problem; in this study, only a few patients had improved pelvic balance postoperatively. It is not known what factors contribute to this lack of improvement; further studies with more subjects are needed to identify those factors.
One of the variables assessed in this study was the GL position relative to spinal and pelvic anatomies. Recently, this means of evaluating spinal balance has interested many surgeons. Many studies have shown that the C7PL, which has traditionally been used for assessing spinal balance, differs from the GL25, 26. Although the GL of a patient cannot be seen or felt directly, it is the vertical line running through the center of the body mass and thus has physical significance. In the coronal plane, the GL position relative to the femoral heads determines how body weight is distributed on each foot. Deviation from the CFH suggests uneven weight distribution on the patient's legs. This also suggests that the sacrum and sacroiliac‐joints are asymmetrically supporting the load. However, the influence of the coronal GL on clinical symptoms has yet to be determined. The results of this study suggest that neither preoperative nor postoperative HRQOL are significantly related to this value. However, it is surprising that in many patients, even though their C7PL deviated from the CSVL, the GL remained centered around the CFH because of compensatory mechanisms. An example of such patients is shown in Fig. 5. The standard deviation of the GL was nearly one half of that of the C7PL. In the sagittal plane, the GL line was also centered on the CFH despite the large scatter of sagittal C7PL. This is because the upper body weight is primarily supported through the hip joint. The greater the distance between the GL and CFH, the larger the muscle force that must be generated to balance the body weight. The surgery appeared to help patients to regain some balance by moving the GL close to the hip joint. However, this variable was not correlated with HRQOL. Hence, we can make no recommendation regarding whether GL measurement can help surgical decision making.
Figure 5.
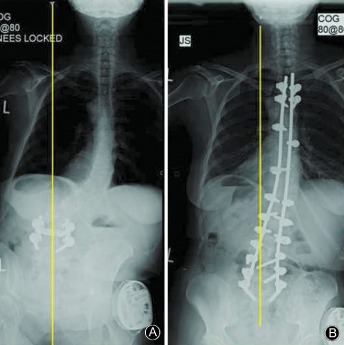
Coronal radiographs of a patient with significant C7PL imbalance: (A) Pre‐operative radiograph, (B) Post‐operative radiograph. The GL is centered near the CFH, indicating symmetric weight distribution on the hips and legs. The GL is shown in yellow.
One limitation of this study is the short follow‐up time: 8 months on average. In a recent study of adult scoliosis, Schwab et al. suggested that radiographic data and clinical outcomes were essentially similar at 2‐year and 1‐year follow‐ups26. Our findings are generally valid for evaluation of short term surgical outcome. Nevertheless, long term outcome should not be predicted based on the results of this study.
Of all the radiographically assessed variables measured in this study, only sagittal balance measured by C7PL was significantly correlated with both preoperative and postoperative ODI scores. Spinal balance measured by GL did not provide better correlation with health status than C7PL. Lost sacral slope and retroverted pelvis are commonly seen in adult scoliosis and are not significantly changed by surgical treatment, including restoration of lumbar lordosis and sagittal balance.
Level of Evidence: Therapeutic Level IV.
Disclosure: No funds were received in support of this work.
References
- 1. Grevitt M, Khazim R, Webb J, Mulholland R, Shepperd J. The short form‐36 health survey questionnaire in spine surgery. J Bone Joint Surg Br, 1997, 79: 48–52. [DOI] [PubMed] [Google Scholar]
- 2. Schwab F, Dubey A, Gamez L, et al Adult scoliosis: prevalence, SF‐36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976), 2005, 30: 1082–1085. [DOI] [PubMed] [Google Scholar]
- 3. Dickson JH, Mirkovic S, Noble PC, Nalty T, Erwin WD. Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am, 1995, 77: 513–523. [DOI] [PubMed] [Google Scholar]
- 4. Schwab F, Farcy JP, Bridwell K, et al A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976), 2006, 31: 2109–2114. [DOI] [PubMed] [Google Scholar]
- 5. Schwab FJ, Lafage V, Farcy JP, Bridwell KH, Glassman S, Shainline MR. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine (Phila Pa 1976), 2008, 33: 2243–2247. [DOI] [PubMed] [Google Scholar]
- 6. Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976), 2005, 30: 682–688. [DOI] [PubMed] [Google Scholar]
- 7. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976), 2005, 30: 2024–2029. [DOI] [PubMed] [Google Scholar]
- 8. Ploumis A, Liu H, Mehbod AA, Transfeldt EE, Winter RB. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine (Phila Pa 1976), 2009, 34: 1581–1584. [DOI] [PubMed] [Google Scholar]
- 9. Schwab F, el‐Fegoun AB, Gamez L, Goodman H, Farcy JP. A lumbar classification of scoliosis in the adult patient: preliminary approach. Spine (Phila Pa 1976), 2005, 30: 1670–1673. [DOI] [PubMed] [Google Scholar]
- 10. Mac‐Thiong JM, Transfeldt EE, Mehbod AA, et al Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis. Spine (Phila Pa 1976), 2009, 34: E519–E527. [DOI] [PubMed] [Google Scholar]
- 11. O'Brien MK. Spinal Deformity Study Group Radiographic Measurement Manual. Memphis, TN: Medtronic Sofamor Danek USA, 2008. [Google Scholar]
- 12. Ploumis A, Transfeldt EE, Gilbert TJ Jr, Mehbod AA, Dykes DC, Perra JE. Degenerative lumbar scoliosis: radiographic correlation of lateral rotatory olisthesis with neural canal dimensions. Spine (Phila Pa 1976), 2006, 31: 2353–2358. [DOI] [PubMed] [Google Scholar]
- 13. Jackson RP, Peterson MD, McManus AC, Hales C. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine (Phila Pa 1976), 1998, 23: 1750–1767. [DOI] [PubMed] [Google Scholar]
- 14. Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976), 2009, 34: E599–E606. [DOI] [PubMed] [Google Scholar]
- 15. Sánchez‐Mariscal F, Gomez‐Rice A, Izquierdo E, Pizones J, Zúñiga L, Alvarez‐González P. Correlation of radiographic and functional measurements in patients who underwent primary scoliosis surgery in adult age. Spine (Phila Pa 1976), 2012, 37: 592–598. [DOI] [PubMed] [Google Scholar]
- 16. Boulay C, Tardieu C, Hecquet J, et al Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J, 2006, 15: 415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Janssen MM, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino‐pelvic alignment in asymptomatic young adults: a three‐dimensional analysis using upright low‐dose digital biplanar X‐rays. Spine (Phila Pa 1976), 2009, 34: E826–E832. [DOI] [PubMed] [Google Scholar]
- 18. Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O'Brien M. Spino‐pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J, 2008, 17: 1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5‐S1 isthmic lysis and low‐grade spondylolisthesis. Spine (Phila Pa 1976), 2006, 31: 2484–2490. [DOI] [PubMed] [Google Scholar]
- 20. Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O'Brien M. The importance of spino‐pelvic balance in L5‐s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine (Phila Pa 1976), 2005, 30 (6 Suppl.): S27–S34. [DOI] [PubMed] [Google Scholar]
- 21. Tanguay F, Mac‐Thiong JM, de Guise JA, Labelle H. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J, 2007, 16: 531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mac‐Thiong JM, Berthonnaud E, Dimar JR 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976), 2004, 29: 1642–1647. [DOI] [PubMed] [Google Scholar]
- 23. Hong JY, Suh SW, Modi HN, Hur CY, Yang JH, Song HR. Correlation of pelvic orientation with adult scoliosis. J Spinal Disord Tech, 2010, 23: 461–466. [DOI] [PubMed] [Google Scholar]
- 24. Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976), 1988, 13: 1317–1326. [PubMed] [Google Scholar]
- 25. Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech, 2003, 16: 44–50. [DOI] [PubMed] [Google Scholar]
- 26. Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine (Phila Pa 1976), 2006, 31: E320–E325. [DOI] [PubMed] [Google Scholar]
- 27. Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age‐related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976), 2006, 31: E959–E967. [DOI] [PubMed] [Google Scholar]


