Abstract
This cost-effectiveness study evaluates use of the recombinant adjuvanted zoster subunit vaccine among patients 50 years and older.
In 2017, the Advisory Committee on Immunization Practices (ACIP) voted to recommend a new recombinant adjuvanted zoster subunit vaccine (RZV) over the live attenuated zoster vaccine (ZVL) and to lower the vaccination age to 50 years. They also recommended that previously vaccinated individuals receive an immediate booster with RZV.1 We evaluated the cost-effectiveness of these recommendations.
Methods
We used our previous Markov model2 to compare costs and quality-adjusted life-years (QALYs) for RZV vs no vaccination with variation of vaccination age from 50 to 59 years. We then adapted the model structure3 to include an RZV booster 0 to 10 years after ZVL administered at 60, 70, and 80 years of age. Patients began the first model in the unvaccinated state and the second in the ZVL vaccinated state and underwent lifelong follow-up. In each yearly cycle, patients undergo transitional events, including herpes zoster infection and related complications, before entering the next cycle. This study used data extracted from the literature; therefore, institutional review board was not needed.
We calculated the incremental cost-effectiveness ratio (ICER) with willingness-to-pay thresholds of $50 000/QALY and $100 000/QALY. We conducted base-case, 1-way, and probabilistic sensitivity analyses from the societal perspective, using TreeAge Pro 2017 software (version R2.1; TreeAge Software, Inc). Costs, adjusted for inflation, were expressed in 2016 US dollars. Costs and QALYs were discounted at 3% per year. Model inputs have been described in detail previously.2,4
Results
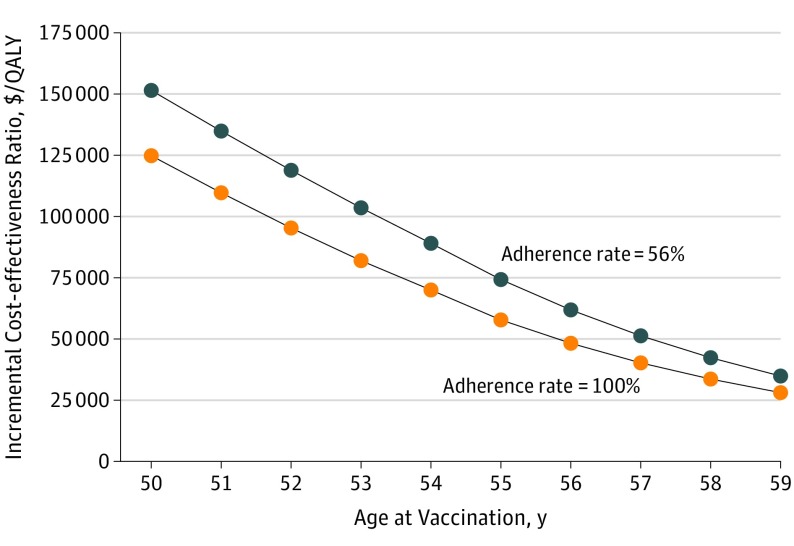
At 50 years of age, RZV had an ICER of $151 430/QALY, which declined below $100 000/QALY at 53.2 years and below $50 000/QALY at 57.1 years (Figure 1). Higher adherence to the second dose made RZV cost-effective at younger ages. Varying the following inputs produced an ICER below $100 000/QALY: probability of postherpetic neuralgia lasting at least 12 months, QALY loss due to herpes zoster infection, efficacy waning rate, and cost of RZV. In the probabilistic sensitivity analysis, RZV at 50 years of age had only a 23% chance of being cost-effective.
Figure 1. Incremental Cost-effectiveness Ratio of RZV Compared With No Vaccination.
Data are stratified by age at vaccination with different adherence rates to 2 doses of RZV. QALY indicates quality-adjusted life-year; RZV, recombinant adjuvanted zoster vaccine.
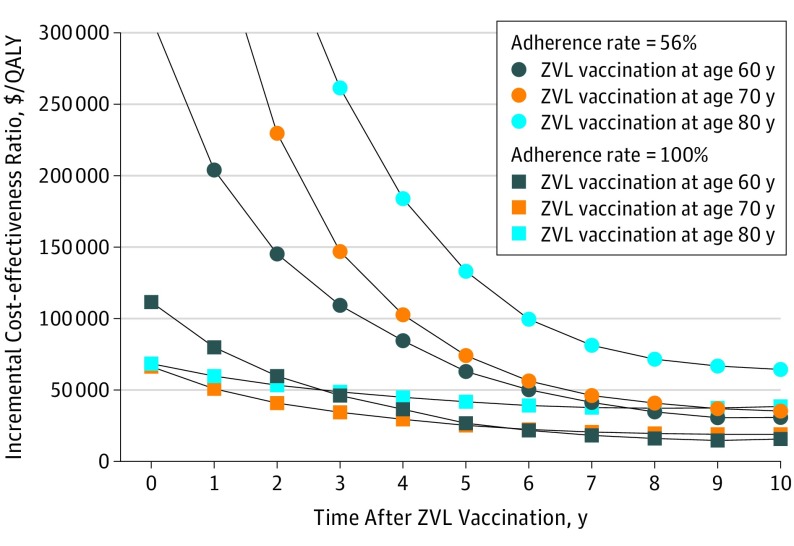
The immediate RZV booster had an ICER of greater than 100 000/QALY at all ages (Figure 2). In people vaccinated with ZVL at 60 years of age, a booster was cost-effective at thresholds of $50 000/QALY and $100 000/QALY after 6 and 4 years, respectively. If adherence was 100%, immediate revaccination would be reasonable. Only changes in the efficacy-waning rate of RZV produced ICERs of less than $100 000/QALY. In the probabilistic sensitivity analysis, the immediate booster had a 9% chance of being cost-effective; the 5-year booster had a 75% chance.
Figure 2. Cost-effectiveness of an RZV Booster Compared With No Booster by Time After ZVL Vaccination at Different Ages.
Adherence rates for 2 doses of RZV were assumed to be 56% and 100%. QALY indicates quality-adjusted life-year; RZV, recombinant adjuvanted zoster vaccine; and ZVL, live attenuated zoster vaccine.
Discussion
The recommendation by the ACIP was informed by the Centers for Disease Control and Prevention model, which assumed a high probability of postherpetic neuralgia and 100% adherence.1 In this modeling study, we found that neither ACIP recommendation would be cost-effective, unless adherence to the 2-dose regimen approached 100%. Using a more realistic estimate, we found it cost-effective to begin vaccination at 55 years of age and offer ZVL recipients a booster after 5 years. This discrepancy highlights the cautions required in interpreting cost-effectiveness findings and the importance of scrutinizing underlying assumptions.
Adherence of 100% is unlikely for several reasons. The coverage of single-dose ZVL was only 30% in 2015, partly owing to cost.5 At $280 for the series, RZV is now the most expensive adult vaccine. Reimbursement will also be an issue, especially in people 65 years or older, because Medicare covers zoster vaccine under part D with substantial copayments.6 The 2-dose regimen will require an additional office visit, potentially resulting in extra work loss. Finally, the 6% of patients with a severe local reaction after the first dose may be particularly hesitant to return.
Conclusions
The new recommendations of the ACIP for RZV do not appear to be cost-effective unless 100% of patients receive both doses. Given our best estimates, vaccination with RZV at 55 years of age and a booster at least 5 years after ZVL would offer better value. Clinicians may consider vaccination earlier for patients who are very likely to comply with a second dose. In all cases, efforts should be made to enhance compliance with the full series.
References
- 1.Dooling KL, Guo A, Patel M, et al. . Recommendations of the Advisory Committee on Immunization Practices for use of herpes zoster vaccines. MMWR Morb Mortal Wkly Rep. 2018;67(3):103-108. doi: 10.15585/mmwr.mm6703a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Le P, Rothberg MB. Cost-effectiveness of the adjuvanted herpes zoster subunit vaccine in older adults. JAMA Intern Med. 2018;178(2):248-258. doi: 10.1001/jamainternmed.2017.7431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le P, Rothberg MB. Cost effectiveness of a shingles vaccine booster for currently vaccinated adults in the US. Am J Prev Med. 2017;53(6):829-836. doi: 10.1016/j.amepre.2017.08.029 [DOI] [PubMed] [Google Scholar]
- 4.Le P, Rothberg MB. Cost-effectiveness of herpes zoster vaccine for persons aged 50 years. Ann Intern Med. 2015;163(7):489-497. doi: 10.7326/M15-0093 [DOI] [PubMed] [Google Scholar]
- 5.Williams WW, Lu PJ, O’Halloran A, et al. . Surveillance of vaccination coverage among adult populations—United States, 2015. MMWR Surveill Summ. 2017;66(11):1-28. doi: 10.15585/mmwr.ss6611a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hurley LP, Lindley MC, Harpaz R, et al. . Barriers to the use of herpes zoster vaccine. Ann Intern Med. 2010;152(9):555-560. doi: 10.7326/0003-4819-152-9-201005040-00005 [DOI] [PubMed] [Google Scholar]