Abstract
In the realm of orthopaedics, the terrible triad of the elbow is infamous, not simply because the prognosis is poor for most patients, but also, maybe to a greater extent, because the unique name of this malady attracts considerable attention and interest in both doctors and patients. The adjective terrible is bestowed on an elbow triad that comprises three coexisting complicated traumas; namely, radial head and ulnar coronoid process fractures and posterior dislocation of the elbow joint. In this review, the classification, treatment principles and prognosis for different forms of management of the radial head and ulnar coronoid process fractures and the ligaments lesions are introduced sequentially and various surgical procedures and their efficacy are discussed. This triad has long given orthopedic surgeons headaches. Nonetheless, in recent years a series of anatomical mechanical studies on the elbow joint have been published and there have been several breakthroughs in surgical techniques for managing this elbow triad. This review examines some memorable millstones and unveils trends in the current clinical norm for this triad. The accomplishments achieved recently have reportedly resulted in enhanced prognoses in the last two or three years compared with previous years. It is therefore high time to revise our thoughts about the justice and accuracy of defining this triad of the elbow as terrible. Lastly, we may safely conclude that the terrible triad of the elbow is much less terrible than previously, provided the commonly approved clinical approaches are undertaken.
Keywords: Denomination, Elbow, Terrible triad
Introduction
Among the variety of disease designations, the terrible triad of the elbow looms large and is eye‐catching because the term “terrible” is rarely seen in medical terminology no matter how intimidatingly severity a disorder is. Therefore, patients and even doctors may harbor doubts about what this so‐called terrible triad is, just how terrible it is, and whether it is possible to achieve a satisfactory prognosis. To answer such these questions, the relevant basic anatomical features of the elbow joint are described first, after which we dive deeper into its definition, classification and treatment principles. Lastly, we shed light on the rationality of the designation “the terrible triad”.
Anatomy
Enveloped by a common joint capsule, the elbow joint comprises three sub‐joints, namely the humeroradial, humeroulnar and superior radioulnar joints. The humerus, radius, ulnar and related capsules and ligaments make up these sub‐joints, which allow the elbow to perform flexion, extension, pronation and supination1 (Figs. 1A, B). Located at the anterior facet of the proximal end of the ulnar, the coronoid process is a triangular‐shaped protrusion and plays a major role in keeping the elbow stable because it slides into the coronoid fossa of humerus when the forearm is in flexion.
Figure 1.
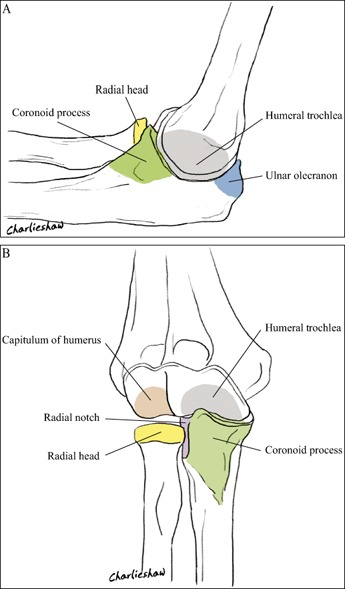
(A) Medial view of the elbow bone structures. (B) Anterior view of the elbow bone structures.
Apart from bony structures, several ligaments also contribute to elbow stability; these include the medial collateral ligament complex (MCLC) and the lateral collateral ligament complex (LCLC). The MCLC is composed of three small ligaments that travel in different directions: the anterior medial collateral ligament, the posterior medial collateral ligament and Cooper's ligament (Fig. 2A), whereas the LCLC is made up of four small ligaments: the lateral ulnar collateral ligament (LUCL), the lateral radial collateral ligament (LRCL), the annular ligament and the accessory lateral ligament2 (Fig. 2B,C). The stability of the elbow largely depends on the functions of the radial head, coronoid process of the ulnar, LCLC and anterior medial collateral ligament3.
Figure 2.
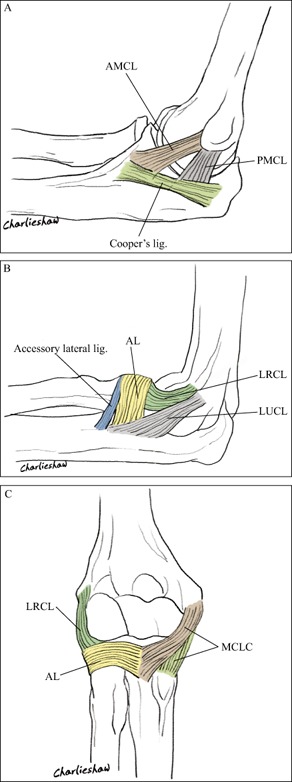
(A) Medial view of the elbow ligaments. Lig., ligament. (B) Lateral view of the elbow ligaments: AL, annular ligament; lig., ligament. (C) Anterior view of the elbow ligaments. AL, annular ligament.
Definition, Classification and Treatment Principles of the Terrible Triad
Definition and Injury Mechanism of the Terrible Triad
The terrible triad of the elbow is defined as the combination of fractures of the radial head and ulnar coronoid process and dislocation of the elbow joint4 (Fig. 3), and is often associated with collateral ligaments injuries. Hotchkiss introduced this concept 19965; Zhang et al. were the first to introduce it to China in 20056. This injury is commonly seen in accidents that involved great force, such as vehicle crashes or falls from heights. The olecranon process of the ulna is most likely to glide out of the trochlea of humerus and thus dislocate posteriorly, causing successive injuries to muscles, ligaments and joint capsules7. The injury is most likely to occur when the following three factors are present simultaneously: the elbow joint is in extension and abduction, the forearm is in supination, and a great force is imposed in an axial direction. Egol et al. described consecutive injuries to the LCLC, anterior and posterior capsules and MCL in the terrible triad injury8. Jeong et al. have reported that almost all patients with dislocation of the elbow joint have some degree of tearing of the MCLC and LCLC9.
Figure 3.
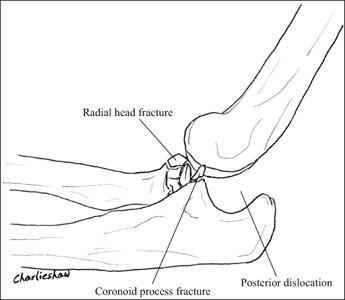
Bone destruction in the terrible triad injury: the terrible triad of the elbow is defined as a combination of radial head and ulnar coronoid process fractures and the dislocation of the elbow joint.
Classification and Treatment Principles of Radial Head Fractures
According to the Mason–Johnson classification, there are four types of radial head fractures10. Type I are non‐displaced radial head fractures (or small marginal fractures); Type II are partial articular fractures with displacement (>2 mm); Type III are comminuted fractures involving the entire radial head; and Type IV are fractures of the radial head with dislocation of the elbow joint. To make it more useful clinically, Hotchkiss modified the Mason–Johnson classification as follows11. Type I are non‐displaced or minimally displaced fractures of the head or neck, intra‐articular displacement is usually <2 mm or they are marginal lip fractures; Type II are displaced (usually >2 mm) fractures of the head or neck (angulated) in which motion is characteristically mechanically blocked or incongruous, these can usually be fixed surgically; and Type III are severely comminuted fractures of the radial head and neck, for which radial head excision or replacement is needed. In this modified version of Mason–Johnson classification, type II and type III are the more frequently found in the terrible triad injury.
Ring et al. performed radial head repair on five patients and radial head resection on four patients with the terrible triad injury12. All four patients treated by resection of the radial head re‐dislocated after operative treatment, whereas four of the five patients who underwent radial head repair achieved satisfactory prognoses with follow‐up of two to seven years. Thus, Ring et al. concluded that preservation of the radial head is important for both acute and long‐term stability and that radial head excision should be performed only in patients with grossly comminuted fractures or with low demands on their upper extremities. For patients with grossly comminuted radial head fractures in whom radial head replacement cannot be achieved, Zhang et al. proposed repairing and fixing the radial head by Kirschner wire to re‐establish elbow stability rather than implementing radial head resection at an early stage13. Leigh and Ball compared radial head repair (13 patients) and radial head replacement groups (11 patients) with a mean duration of 41 months follow‐up and reported that a good range of movement and stability was achieved in both groups at short‐term follow‐up with operative repair or replacement of the radial head to restore stability through radiocapitellar contact, operative repair or replacement of the coronoid, and lateral ligament repair14. Watters et al. retrospectively reviewed 39 patients with a mean duration of 24 months follow‐up and noted that there was no significant difference between those treated with internal fixation or radial head arthroplasty in terms of clinical outcome measures, elbow stability, radiographic evidence of arthrosis, complications and reoperation rates15. He also pointed out that, because these injuries are commonly seen in younger patients, longer‐term studies are needed to determine whether the apparent benefits of radial head arthroplasty are offset by late complications of arthroplasty, such as loosening. Hartzler et al. collected kinematic data on six fresh‐frozen cadaveric upper extremities and concluded that both monopolar and bipolar radial head prostheses are effective in improving valgus and external rotation laxity to the elbow, regardless of coronoid status16.
Classification and Treatment Principles of Coronoid Process Fractures
Coronoid process fractures are almost always accompanied by other severe elbow joint injuries17, and the Regan–Morrey classification18 is commonly adopted in clinical practice. Type I is avulsion of the tip of the process; in Type II the fragment involves ≤50% of the process; and in Type III the fragment involves >50% of the process (Fig. 4). The fractures are further subclassified into A and B groups according to whether the patient does or does not have elbow joint dislocation. Of these type I fractures are most commonly associated with the terrible triad injury19.
Figure 4.

Regan–Morrey classification for coronoid process fractures: Type I, avulsion of the tip of the process; Type II, fragment involving ≤50% of the process; Type III, fragment involving >50% of the process.
O'Driscoll et al. classified coronoid fracture into the following three types according to the distribution of the fracture lines20. Type I are transverse fractures of the coronoid tip in which the fracture lines are confined to the coronoid tip and do not extend past the sublimus tubercle. Type II are fractures of the anteromedial facet in which the fracture lines run past the coronoid tip and the anteromedial facet. Type III are large fractures involving ≥50% of the coronoid height in which the fracture lines travel into the body and basal part of the coronoid (Fig. 5). Mellema et al. collected 110 computed tomography data from patients with coronoid fractures and found out that 47 of them had terrible triad injuries, the fractures were type I of the O’ Driscoll classification in 42 of the 4721.
Figure 5.
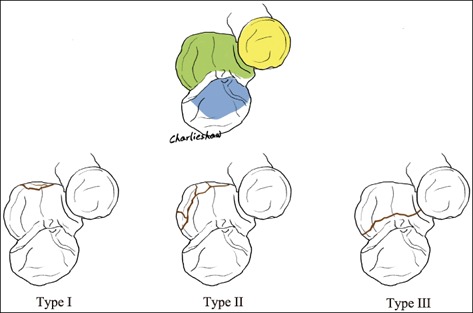
O’Driscoll classification for coronoid process fractures: Type I, transverse fractures of the coronoid tip in which the fracture lines are confined to the coronoid tip; Type II, fractures of the anteromedial facet in which the fracture lines run past the coronoid tip and the anteromedial facet; and Type III, large fractures involving ≥50% of the coronoid height in which the fracture lines travel into the body and basal part of the coronoid.
O'Driscoll et al. reported that Regan–Morrey type I coronoid process fractures have little impact on elbow stability compared with the normal elbow20. Cohen proposed that there is no need to further repair Regan–Morrey type I coronoid process fractures beyond reconstructing the stability of the radial head and LCLC22. Nevertheless, Zeiders and Patel have suggested that repairing Regan–Morrey type I coronoid process fractures is as important as repairing Regan–Morrey type II and type III fractures23. Morrey stated that elbow instability occurs when there is ≥50% bone loss from the coronoid process24. Morrey has also suggested that, even when 50% of the coronoid process has been retained, elbow stability is rare if there is also a bone defect of the radial head25. With Morrey type II and type III coronoid process fractures, fixation to the coronoid process in an adverse direction with two or three lag screws is recommended. For repairable comminuted coronoid process fractures, the coronoid process should be repaired with relatively larger fracture fragments from the articular facet and the anterior support of the coronoid process should be restored to prevent re‐dislocation of the elbow joint. For unrepairable comminuted coronoid process fractures in which radial head resection is required, the resected radial head can be utilized to restore the coronoid process26, 27, 28, 29. Papatheodorou et al. considered that coronoid process fixation is unnecessary for Regan–Morrey type I and II fractures if elbow stability has already been achieved by radial head repair or replacement and reconstruction of the LUCL30.
Assessment and Treatment Principles of Ligament Injuries
In terrible triad injuries, injury of the LCLC often occurs at its origin at the lateral condyle of the humerus; other parts of the LCLC tear less frequently31. Schemitsch et al. reported that both the LUCL and LRCL are equally indispensable for elbow stability; thus, both require repair and reconstruction32. The anterior band of the MCLC plays an essential role in valgus stability of the elbow33, whereas the posterior band of the MCLC is critical in maintaining elbow posterolateral rotation stability34. Whether elbow stability has been achieved should be checked intraoperatively after repairing the coronoid process, radial head and LCLC. It is unnecessary to repair the MCLC if elbow stability has been achieved and there is no posterior dislocation or subluxation when the forearm is in pronation, supination, flexion and extension3. Mild postoperative valgus instability is not an indication for reoperation because it is usually compensatory33. If posterior or posterolateral elbow instability is noticed, the coronoid process, radial head and LCLC should be examined to ascertain whether they have been fully repaired. If they have, the pronator muscles and MCLC should be repaired through a medial surgical approach. If instability persists, hinged external fixation should be applied35. Jeong et al. have suggested that the LCLC and pronator muscles should be repaired at the same stage9.
Prognosis of Terrible Triad Injuries and Conclusion
The “terrible triad of the elbow” is a notorious combination of elbow dislocation and fractures of the coronoid process and radial head that has historically been difficult to manage and had an unsatisfactory prognosis36, 37, 38, almost unavoidably causing long‐standing postoperative pain, elbow instability and a range of complications. With recent developments in pathology, anatomy and biomechanics of the elbow joint, a standard management protocol has gradually been established. This protocol focuses on reduction and internal fixation of the coronoid process, radial head repair or replacement and repair of the LCLC. MCLC repair or hinged external fixation is further required if there is still elbow instability after the standard protocol has been implemented. Chen et al. performed a meta‐analysis of 312 such cases and reported satisfactory functional outcomes with Mayo elbow performance scores of 78–95 points, the Broberg–Morrey scores of 76–90 points and DASH scores of 9–31 points39. These findings are similar to those previously reported by Rodriguez‐Martin who studied 137 cases and found mean Mayo scores of 85.6 points, mean Broberg–Morrey scores of 85 points and average flexion of 132.5° with forearm rotation of 135.5°35. Zhang et al. followed a standard protocol in 14 cases with 18.7 months follow‐up and reported that 71.4% of Mayo elbow performance scores, 78.6% of Broberg–Morrey scores and 78.6% of DASH scores reached the good level40. Fitzgibbons et al. retrospectively reviewed 11 cases of terrible triad injuries with a mean postoperative follow‐up of 38 months and reported no instances of elbow instability; mean disabilities of the arm, shoulder and hand (DASH) scores being 19.7 points, mean visual analog scale 2.2 points and average flexion arcs 112° at the end of follow‐up41. Zhang et al. treated 21 cases of terrible triad injuries with a modified surgical technique including fixation or replacement of the radial head and repair of the LCLC through a lateral approach, and simultaneous fixation of the coronoid process and repair of the common flexor muscle and the MCLC through an anteromedial approach. The mean Mayo elbow performance scores were 95 points after a 32 months follow‐up (19 cases ranked excellent and two ranked good), and the mean flexion and mean rotation arcs were 126° and 139°, respectively42.
Based on these widely acknowledged data, Rodriguez‐Martin et al. have come up with the following eleven suggestions for the diagnosis and treatment of terrible triad injuries35:
Computed tomography with three dimensional reconstructions can be helpful in ascertaining the type of injury.
Prior to surgery, all equipment potentially needed for the reconstruction must be prepared, including screws, suture anchors, plates, prosthesis, external fixators and so on.
A posterior skin incision that allows accesses to both medial and lateral aspects of the elbow is most widely chosen.
Postoperative ulnar nerve dysfunction symptoms can be prevented by performing anterior ulnar nerve transposition.
Structures are repaired from deep to superficial from the coronoid process and radial head to the lateral collateral ligament.
Attempts should be made to to preserve the radial head, otherwise radial head arthroplasty should be performed.
Stability should be evaluated intraoperatively after reconstruction. If the elbow dislocates in 30°–45° of extension, the medial collateral ligament should be repaired. A dynamic external fixator should be applied if instability persists.
If the joint does not reach its congruency, the previous steps from step five onward should be repeated.
Motion must be started a few days postoperatively; varus stress should be avoided during early motion.
A functional elbow with an average flexion of approximately 110° can be expected if these protocols are followed.
Possible postoperative joint stiffness, prosthesis removal or ulnar nerve symptoms may require additional procedures; however, arthritis is usually tolerable.
Compared with many other medical terms, the terrible triad of the elbow attracts attention and is relatively easy to remember. On the one hand, it accurately reflects the undesirable outcomes with which this injury has previously been associated. On the other hand, having attracted the attention of both doctors and researchers has had a benefit in terms of stimulating clinical and research interest. As mentioned previously, there has been rapid progress in the diagnosis and treatment of terrible triad injuries in recent years and the prognosis is accordingly much less terrible than it used to be. Thus the term “terrible triad of the elbow’ has morphed into a readily recognized symbol that has somewhat lost its significance. What's more, the word “terrible” probably causes patients and their relatives considerable unnecessary anxiety. Many more serious illnesses such as cancer and some deadly infectious diseases have no emotionally evocative elements in their designations. All in all, the term “terrible triad of the elbow” is no longer accurate. We therefore recommend “the complicated triad injury of the elbow” as a better designation in medical books and records, whereas, because of its conciseness and wide acceptance, the term “terrible triad injury” could still be used in daily and academic communications among medical personnel.
Disclosure: All authors have no financial or personal relationships with other people or organizations that could inappropriately influence this work.
References
- 1. Beals RK. The normal carrying angle of the elbow. A radiographic study of 422 patients. Clin Orthop Relat Res, 1976, 119: 194–196. [PubMed] [Google Scholar]
- 2. Dodds SD, Fishler T. Terrible triad of the elbow. Orthop Clin North Am, 2013, 44: 47–58. [DOI] [PubMed] [Google Scholar]
- 3. Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am, 2004, 86: 975–982. [DOI] [PubMed] [Google Scholar]
- 4. Pugh DM, McKee MD. The “terrible triad” of the elbow. Tech Hand Up Extrem Surg, 2002, 6: 21–29. [DOI] [PubMed] [Google Scholar]
- 5. Rockwood CAGD. Rockwood and Green's Fractures in Adults. Philadelphia: Lippincott Williams & Wilkins, 2006. [Google Scholar]
- 6. Zhang SM, Zhou JQ, Yu GR. Terrible triad of the elbow. Zhongguo Jiao Xing Wai Ke Za Zhi, 2005, 13: 782–785 (in Chinese). [Google Scholar]
- 7. O'Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am, 1991, 73: 440–446. [PubMed] [Google Scholar]
- 8. Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ. Fracture‐dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis, 2007, 65: 263–270. [PubMed] [Google Scholar]
- 9. Jeong WK, Oh JK, Hwang JH, Hwang SM, Lee WS. Results of terrible triads in the elbow: the advantage of primary restoration of medial structure. J Orthop Sci, 2010, 15: 612–619. [DOI] [PubMed] [Google Scholar]
- 10. Bhandari M. Evidence‐Based Orthopedics. Oxford: Wiley‐Blackwell, 2011. [Google Scholar]
- 11. Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg, 1997, 5: 1–10. [DOI] [PubMed] [Google Scholar]
- 12. Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am, 2002, 84: 547–551. [DOI] [PubMed] [Google Scholar]
- 13. Zhang SM, Yu GR, Yuan F, et al Posterior dislocation of the elbow with radial head and ulnar coronoid fractures (terrible triad): a report of 5 cases. Zhongguo Jiao Xing Wai Ke Za Zhi, 2007, 15: 1069–1073 (in Chinese). [Google Scholar]
- 14. Leigh WB, Ball CM. Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elbow Surg, 2012, 21: 1336–1341. [DOI] [PubMed] [Google Scholar]
- 15. Watters TS, Garrigues GE, Ring D, Ruch DS. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res, 2014, 472: 2128–2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hartzler RU, Morrey BF, Steinmann SP, Llusa‐Perez M, Sanchez‐Sotelo J. Radial head reconstruction in elbow fracture‐dislocation: monopolar or bipolar prosthesis? Clin Orthop Relat Res, 2014, 472: 2144–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Budoff JE. Coronoid fractures. J Hand Surg Am, 2012, 37: 2418–2423. [DOI] [PubMed] [Google Scholar]
- 18. Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am, 1989, 71: 1348–1354. [PubMed] [Google Scholar]
- 19. Doornberg JN, Ring D. Coronoid fracture patterns. J Hand Surg Am, 2006, 31: 45–52. [DOI] [PubMed] [Google Scholar]
- 20. O'Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect, 2003, 52: 113–134. [PubMed] [Google Scholar]
- 21. Mellema JJ, Doornberg JN, Dyer GS, Ring D. Distribution of coronoid fracture lines by specific patterns of traumatic elbow instability. J Hand Surg Am, 2014, 39: 2041–2046. [DOI] [PubMed] [Google Scholar]
- 22. Cohen MS. Fractures of the coronoid process. Hand Clin, 2004, 20: 443–453. [DOI] [PubMed] [Google Scholar]
- 23. Zeiders GJ, Patel MK. Management of unstable elbows following complex fracture‐dislocations—the “terrible triad” injury. J Bone Joint Surg Am, 2008, 90 (Suppl. 4): 75–84. [DOI] [PubMed] [Google Scholar]
- 24. Morrey BF. The Elbow and Its Disorders. Philadelphia: WB Saunders, 2000. [Google Scholar]
- 25. Morrey BF. Current concepts in the management of complex elbow trauma. Surgeon, 2009, 7: 151–161. [DOI] [PubMed] [Google Scholar]
- 26. Manidakis N, Sperelakis I, Hackney R, Kontakis G. Fractures of the ulnar coronoid process. Injury, 2012, 43: 989–998. [DOI] [PubMed] [Google Scholar]
- 27. Alolabi B, Gray A, Ferreira LM, et al Reconstruction of the coronoid using an extended prosthesis: an in vitro biomechanical study. J Shoulder Elbow Surg, 2012, 21: 969–976. [DOI] [PubMed] [Google Scholar]
- 28. Chung CH, Wang SJ, Chang YC, Wu SS. Reconstruction of the coronoid process with iliac crest bone graft in complex fracture‐dislocation of elbow. Arch Orthop Trauma Surg, 2007, 127: 33–37. [DOI] [PubMed] [Google Scholar]
- 29. Kohls‐Gatzoulis J, Tsiridis E, Schizas C. Reconstruction of the coronoid process with iliac crest bone graft. J Shoulder Elbow Surg, 2004, 13: 217–220. [DOI] [PubMed] [Google Scholar]
- 30. Papatheodorou LK, Rubright JH, Heim KA, Weiser RW, Sotereanos DG. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res, 2014, 472: 2084–2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Patterson SD, Bain GI, Mehta JA. Surgical approaches to the elbow. Clin Orthop Relat Res, 2000, 370: 19–33. [DOI] [PubMed] [Google Scholar]
- 32. McKee MD, Schemitsch EH, Sala MJ, O'Driscoll SW. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg, 2003, 12: 391–396. [DOI] [PubMed] [Google Scholar]
- 33. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res, 1991, 265: 187–195. [PubMed] [Google Scholar]
- 34. Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am, 2008, 39: 141–154. [DOI] [PubMed] [Google Scholar]
- 35. Rodriguez‐Martin J, Pretell‐Mazzini J, Andres‐Esteban EM, Larrainzar‐Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop, 2011, 35: 851–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rodriguez‐Martin J, Pretell‐Mazzini J, Cecilia‐Lopez D, Resines‐Erasun C. Medial complex elbow dislocation: an unusual pattern of injury. J Orthop Trauma, 2010, 24: 21–24. [DOI] [PubMed] [Google Scholar]
- 37. Sharma H, Sibinski M, Sherlock DA. Outcome of lateral humeral condylar mass fractures in children associated with elbow dislocation or olecranon fracture. Int Orthop, 2009, 33: 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am, 2005, 87 (Suppl. 1 Pt 1): 22–32. [DOI] [PubMed] [Google Scholar]
- 39. Chen HW, Liu GD, Wu LJ. Complications of treating terrible triad injury of the elbow: a systematic review. PLoS ONE, 2014, 9: e97476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang PX, Xue F, Dang Y, et al Multi‐center clinical retrospective analysis of elbow joint “terror triad” effect treated with operation. Zhongguo Gu Yu Guan Jie Wai Ke, 2010, 3: 275–278. (in Chinese). [Google Scholar]
- 41. Fitzgibbons PG, Louie D, Dyer GS, Blazar P, Earp B. Functional outcomes after fixation of “terrible triad” elbow fracture dislocations. Orthopedics, 2014, 37: 373–376. [DOI] [PubMed] [Google Scholar]
- 42. Zhang C, Zhong B, Luo CF. Treatment strategy of terrible triad of the elbow: experience in Shanghai 6th People's Hospital. Injury, 2014, 45: 942–948. [DOI] [PubMed] [Google Scholar]


