Abstract
Objective: To investigate the clinical diagnosis and arthroscopic treatment of acetabular labral tears.
Methods: Twenty‐one patients with unilateral acetabular labral tears hospitalized from November 2008 to December 2009 were included in this retrospective study. A definitive diagnosis was made preoperatively on the basis of physical examination, plain radiography and magnetic resonance arthrography (MRA). All cases were treated with arthroscopic surgeries: labral debridement (14 cases), labral debridement plus femoral osteoplasty (5 cases), and labral repair plus osteoplasty (2 cases). All patients were followed‐up and the results evaluated using the visual analogue scale (VAS) and Harris hip score.
Results: A positive flexion, abduction and internal rotation (FADIR) impingement sign was found in all 21 affected hips, a positive flexion, abduction and external rotation (FABER) impingement sign in 15, and a positive McCarthy test in 9. Plain radiography showed 11 cases had cam type impingement, in 6 of whom it was combined with pincer type impingement; and 2 cases had acetabular retroversion alone. Labral tears were observed on MRA in all cases and were all confirmed by arthroscopy. All patients were followed up for an average of 11.6 months (range, 6 to 19 months). The VAS decreased from (5.3 ± 1.3) preoperatively to (1.4 ± 0.9) 6 months postoperatively. The mean Harris hip score improved from (63 ± 9) preoperatively to (84 ± 10) 6 months postoperatively. All these differences were statistically significant.
Conclusions: Acetabular labral injury is closely correlated with femoro‐acetabular impingement. Impingement tests and MRA have high sensitivity and accuracy in clinical diagnosis of labral tears. Arthroscopic debridement, repair and osteoplasty for labral tears results in a good early outcome.
Keywords: Acetabulum, Arthrography, Arthroscopy, Wounds and injuries
Introduction
Acetabular labral injury is one of the most common reasons for pain in the hip. Over the last decade, the diagnosis and arthroscopic management of labral tears and femoro‐acetabular impingement (FAI) has evolved substantially due to improvement in clinical diagnostic tools, surgical techniques, and instrumentation for hip arthroscopy. Arthroscopic debridement or repair/reattachment has been reported to be a reliable and minimally invasive procedure provided strict indications are observed 1 . However, some doctors are still either unclear or sceptical about the diagnosis and treatment of acetabular labral tears, especially in regard to the clinical outcomes of arthroscopic treatment. In order to clarify diagnostic methods and assess the outcome of arthroscopic treatment for acetabular labral tears, we carried out this retrospective study.
Materials and Methods
From January 2008 to December 2009, 21 patients with unilateral acetabular labral tears were treated in our hospital, including 9 men and 12 women with an average age of 37.1 years (range, 17 to 65 years). One patient had fallen from a height, fourteen had been subject to hip joint sprain and the remaining six patients had no clear history of trauma. All patients complained of a definite pain around the hip joint, most commonly in the groin area. Fifteen patients had varying frequencies of hip locking or catching and nine complained of medial knee pain. The average time from onset of symptoms to diagnosis was 12.4 months (range, 3 to 54 months).
Physical examination
Physical examination included measurement of range of movement (ROM) and specific provocative tests. Flexion, adduction and abduction, as well as internal and external rotation, were evaluated and recorded. The anterior impingement test was performed with the patient supine. The hip was placed in 90° of flexion and then adduction and internal rotation (FADIR), or flexion, abduction and external rotation (FABER) applied. These tests are considered positive if they elicit hip or groin pain. The McCarthy test was also performed. The hip was placed in flexion and was then extended in external or internal rotation. The test is positive if pain or snapping is reproduced during this forced movement of hip.
Imaging assessment
Plain radiography
The joint space was measured and the acetabulum evaluated for both degree of cover of the femoral head (center edge angle) and the degree of acetabular tilt on anteroposterior (AP) radiographs. Cross‐table and frog‐leg lateral radiographs were used to assess the anterior femoral head‐neck morphology, and to measure the α angle (Fig. 1). Pincer type impingement is considered to be present when coxa profunda, retroversion of the acetabulum (cross‐over sign), or a center edge angle >40° are found. The cam type impingement sign is positive when the α angle >50°.
Figure 1.
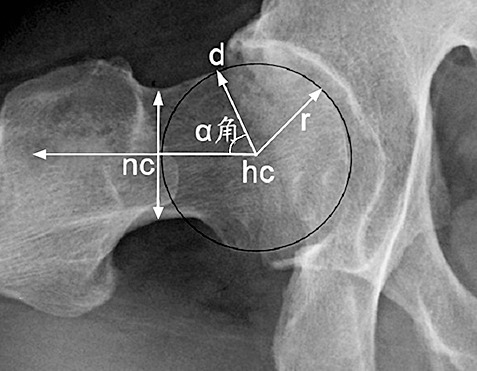
Measurement of the α angle on X‐ray film. d: the critical point where the distance between the anterior border of the neck and the center of the head just exceeds the head radius; hc: center of the head; nc: midpoint of the femoral neck at its narrowest point; r: radius of the head.
Magnetic resonance arthrography
Puncture was performed on the suspected hip under fluoroscopy guidance, and then 8 to 20 mL diluted gadopentetate dimeglumine (Beijing Beilu Pharmaceutical, Beijing, China) was injected into the hip joint at a concentration of 2.5mmol.L−1. MRI carried out 20 minutes after the contrast agent had been injected. The magnetic resonance scanning was performed using a 1.5T Philips Intera inager (Philips Medical Systems, Best, the Netherlands) with phased array wrap coil. Coronal, sagittal, axial oblique (along the long axis of the femoral neck) and radial images at fat suppression T1‐weighted scan were obtained. The sites of acetabular labral tears were recorded using a “clock‐face” system. The labral tears were classified according to the report of Czerny et al. (0‐IIIB stages) 2 .
Surgical technique
An epidural or general anesthesia was used. The patient was placed in a supine position on a surgical traction table. The leg to be operated on was positioned in 0° of flexion, 0° of abduction and neutral rotation. The opposite leg was positioned in 40° of abduction, 0° of flexion and neutral rotation. Fluoroscopy was used to obtain an AP view of the hip. Gentle traction (10 to 20 kg) was applied through the hip, with moderate counter‐traction through the contralateral hip. The joint space was assessed with fluoroscopy to achieve approximately 10 to 12mm of distraction. The traction arm was marked and then the traction was released.
The arthroscopy devices were connected after skin sterilizing and draping. Traction was applied again up to the marked point. Anterolateral and anterior portals were established under fluoroscopy. After a capsulectomy had been performed, the central compartment, including the acetabular labrum, articular cartilage and ligament of the head of the femur, was examined. The torn labrum was debrided if it was severely degenerated, frayed or had completely detached. Any osteophytes on the acetabular rim were simultaneously resected. Tears with enough healthy tissue were repaired. After the bone of the acetabular rim had been refreshed, the torn labrum was reattached using suture anchors with circumferential capture. Other pathologies, including tear of the ligament of the head of the femur and cartilage degeneration, were also treated by debridement. The traction was then released and the peripheral compartment examined. Where applicable, a dynamic arthroscopic examination was performed to confirm a pre‐operative diagnosis of cam impingement lesion. Once an area of cam impingement had been identified at the femoral head‐neck junction, a round burr was used to restore the normal anatomical bony architecture of the junction. The bone resection was carried out under fluoroscopy.
In total, 14 cases were treated by labral debridement, five by labral debridement plus head‐neck junction osteoplasty, and two by labral repair plus osteoplasty.
Postoperative management
In the first 2 weeks after surgery, a rotation‐preventing shoe was used while lying in bed. Partial weight‐bearing with the aid of crutches was encouraged in the first week. A slow progression to full strength and weight‐bearing was permitted 4 weeks after surgery in patients who had undergone debridement only. For those who had undergone osteoplasty, an additional 2 weeks was imposed. A full return to sporting activity was permitted 3 to 4 months postoperatively.
Changes in symptoms, including relief of hip pain and locking, recovery of ability to undertake sporting activity and hip function were assessed by telephone follow‐up and out‐patient interview. The Harris hip score and visual analogue scale (VAS) were used to evaluate the function of the hip.
Statistical analysis
SPSS statistic software (version 13.0, SPSS, Chicago, IL, USA) was used for data analysis. Comparison of bilateral ROM, pre‐ and post‐operative Harris hip score and VAS were performed with a paired Student's t‐test. All reported P‐values are two‐tailed, with an α level of 0.05 indicating significance.
Results
Findings on physical examination
The affected hip had a reduced ROM in all directions, flexion and internal rotation being the most significantly reduced. Compared to the opposite hip, loss of ROM was (10°± 6°, t= 7.385, P= 0.000) in flexion and (6°± 3°, t= 9.154, P= 0.001) in internal rotation. A positive FADIR impingement sign was observed in all 21 patients (100%), and the FABER sign was positive in 15 cases (15/21, 71%). A positive McCarthy test was also detected in 9 patients (9/21, 43%).
Imaging results
Plain radiography
No patient had significant joint space narrowing or signs of hip dysplasia. Eleven patients (11/21, 52%) had cam type impingement with an average α angle of 65.7° (58°–75°), of which six (6/21, 29%) were complicated by simultaneous pincer type impingement (one with retroversion of the acetabulum, five with coxa profunda). Two cases (2/21, 9%) showed pincer type impingement only (Fig. 2). No bony abnormalities were found in the remaining 8 cases (8/21, 38%).
Figure 2.

AP radiograph of the right hip. A cross‐over sign indicating retroversion of the acetabulum is shown (dashed line).
Magnetic resonance arthrography
Infiltration of contrast agent into the acetabulum‐labrum transitional zone was observed in the anterior superior quadrant in all patients (100%). One (1/21, 5%) was complicated by an abnormal signal indicating inferoposterior labrum. According to the classification of Czerny et al. 2, two cases were IIA, twelve IIIA and seven IIIB. All labral tears could be seen on the axial oblique and radial images (Fig. 3). Labral lesions could be seen on the coronal images in 15 cases (15/21, 71%), and 7 (7/21, 33) were visible on the sagittal images.
Figure 3.
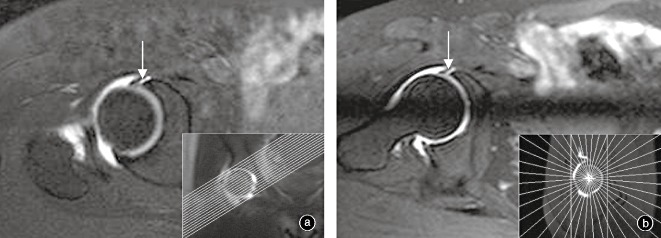
(a) Axial oblique and (b) radial MRA images of the hip. Arrows show infiltration of the contrast agent into the acetabulum‐labrum junction, which indicates labral tears (Czerny IIIA).
Arthroscopy findings
Under arthroscopy, various types of labral tears were detected in the anterior superior area of the acetabula of all patients. This demonstrated that the accuracy of the impingement test and magnetic resonance arthrography (MRA) was 100%. Two (2/21, 9%) of them had partial labral tears and 19 (19/21, 90%) full‐thick labral tears. The torn labra were either degenerated or frayed, and in 11 cases (11/21, 52%) there was a flap with a fully detached end of torn labrum. One case (1/21, 5%) was complicated by a partial labral tear in the inferoposterior region. Other pathologies included tears of the ligament of the head of the femur in four cases (4/21, 19%), degeneration of articular cartilage both in the head and on the acetabular side, and various degree of synovial proliferation (Fig. 4).
Figure 4.
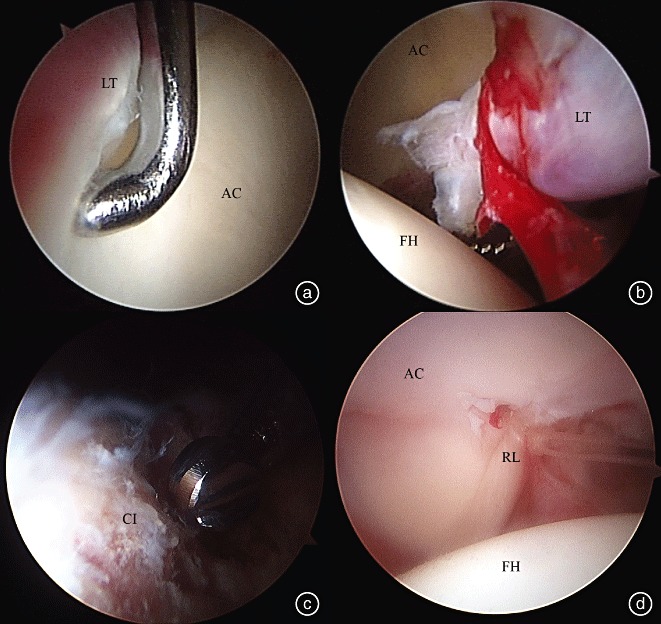
Arthroscopic findings and treatment of labral tears. (a) Partial labral tear; (b) Full‐thickness labral tear with a totally separated flap; (c) Osteoplasty of the head‐neck junction; (d) Repaired labrum. AC, acetabular cartilage; CI, cam type osteophyte in head‐neck junction; FH, femoral head; LT, labral tears; RL, repaired labrum.
Clinical results and complications
There was 100% follow‐up after operation with a mean follow‐up period of 11.6 months (6 to 19 months). Hip pain had completely disappeared in 11 cases (11/21, 52%) and was significantly relieved in 10 (10/21, 48%) by the end of follow‐up. Symptoms of hip locking resolved completely. The mean VAS decreased from (5.3 ± 1.3) preoperatively to (1.4 ± 0.9) 6 months postoperatively (t= 17.135, P= 0.001). The Harris hip score improved from (63 ± 9) preoperatively to (84 ± 10) 6 months postoperatively (t=−11.723, P= 0.003).
Injury to the lateral femoral cutaneous nerve occurred in one patient (1/21, 4.8%), presenting as skin numbness in the lateral thigh and disappearing spontaneously 3 months postoperatively. No injuries to vessels, infection, fractures, perineal damage, lower extremity or deep vein thrombosis occurred.
Discussion
Clinical diagnosis
The causes of acetabular labral tears have been described as traumatic, congenital (such as acetabular dysplasia or coxa profunda), degenerative and idiopathic. Most labral tears treated clinically are caused by minor injuries from sporting or even routine activities 3 , 4 . Only one patient in this study had a clear history of major injury; the others reported only minor injuries such as twisting or slipping or even no history of any specific traumatic event. The most common symptom of acetabular labral tears is hip pain (mainly located in the inguinal region) and locking. Symptoms like clicking, snapping, locking, and so called dead‐leg sign are more specific to this diagnosis.
Once the acetabular labrum has been injured, the ROM of the hip can be reduced in all directions to various levels. The results of this study demonstrate that the range of flexion and internal rotation is significantly reduced due to labral tears, which are most likely to occur in the anterosuperior region. Impingement and compression can occur in the anterosuperior labrum and initiate pain while the hip is in flexion or internal rotation, especially when flexion is combined with internal rotation. The impingement tests are specific provocative maneuvers which can elicit pain consistent with a labral tear or an impingement lesion, and they are the most frequent and important signs for labral tears 5 . The FADIR and FABER tests may recreate groin pain or mechanical symptoms. Both of these maneuvers can load the hip joint anterosuperiorly, which is the most common location for labral tears. According to Philippon et al., the positive rates for FADIR and FABER tests in patients with labral tears are 99% and 97%, respectively 6 . In this study, a positive FADIR impingement sign was seen in 100% of patients, and a positive FABER sign in 97%. All labral tears were confirmed by arthroscopy, demonstrating that the impingement test is extremely accurate in the diagnosis of labral tears. The McCarthy test for acetabular labral tears 7 was developed earlier than the FADER and FABER tests. Although a positive McCarthy test is not very common in labral lesions, it has a high specificity. The McCarthy test was positive in 43% of patients in this study, most of whom had mechanical symptoms like locking or catching. Optimally, a clinical examination should be performed in a systematic fashion so that an accurate diagnosis can be achieved. A complete examination of the surrounding structures should be performed carefully to distinguish between intra‐ and extra‐articular lesions, and to accurately assess any abnormalities of the abdomen, pelvis, lumbar spine and sacroiliac joint.
Imaging diagnosis
It is widely recognized that FAI caused by abnormal morphology of the head‐neck junction or/and acetabulum has a close relationship with labral tears. A large percentage of patients with labral tears are found to have concurrent FAI, and most patients with FAI visit their doctors because of the occurrence of labral tears 3 , 4 , 5 . In case with no calcification or ossification, labral tissue is radioparent. Therefore, the main contribution of plain radiography is to determine the morphology of the head‐neck junction, the coverage of the femoral head and the tilt of the acetabulum. Abnormal findings on plain X‐ray films include reduced head‐neck offset, increased α angle, or specific deformities such as pistol grip, all of which have been linked to cam type FAI. Plain radiographs may show coxa profunda, protrusion of the acetabulum (with an increased center‐edge angle) and retroversion of the acetabulum (in which a so called cross‐over sign is visible on AP radiography), all of which indicate pincer type FAI 8 . It is worth noting that, to accurately evaluate the true acetabulum tilt angle pelvic, AP radiographs must be taken in the standard position with the central beam directed to the mid‐point between both anterior superior iliac spines and the superior border of the pubic symphysis.
Our results showed that 11 of 21 cases (52%) had cam type impingement and eight (38%) pincer type impingement, of which six (29%) had combined impingement. However, in the remaining 8 patients (38%) no bony abnormalities were observed on plain radiographs. This indicates that patients with symptoms like hip pain and locking may have labral injury in the absence of positive findings on plain X‐ray films. Acetabular labral tears do always mean that FAI is present. In patients with FAI, two‐ and three‐dimensional CT scan can accurately assess any osseous deformities of the acetabulum and proximal femur, and evaluate the amount of resection to be undertaken during hip arthroscopy 9 , 10 .
MRI provides detailed information regarding the soft tissues surrounding the hip, but conventional MRI is not sensitive enough for diagnosis of labral lesions. MRA performed after intra‐articular injection of contrast agent (usually gadolinium‐diethylenetriamine pentaacetic acid) can provide more clear images of the acetabular labrum and might be the most sensitive and specific method for diagnosis of labral tears. The diagnostic rate could be significantly improved by using MRA 11 . Infiltration of contrast agent into the injured area of the labrum is visible on MRA images. In the study of Crzerny et al., labral tears were classified into four stages (0 to III) according to their MRA manifestations 2 . Axial oblique and radial images are more helpful and result in a higher positive rate of diagnosis of labral tears. Our results show that the axial oblique and radial images displayed obvious abnormal signals of labral injuries in all patients, whereas positive signal changes were detected on 71% of coronal images and 33% of sagittal images. The MRA is after all an invasive examination. With the development of MRI techniques, the high tesla scanner and specific sequences can provide more clear images of the labrum and cartilage and their sensitivity may be similar to that of MRA in the diagnosis of labral tears 12 , 13 .
Arthroscopic treatment
Symptoms can be relieved by conservative treatment, including physical therapy, anti‐inflammatory medication and modification of activities, although these treatments do not address the underlying cause. Open surgical dislocation of the hip has played an important role in recognition and treatment of labral tears. It provides an unobstructed view of the femoral head and acetabulum and allows accurate inspection and simultaneous debridement or repair of intra‐articular disorders, and has been reported to produce good results. However, the disadvantages of this procedure include major invasion and a high rate of complications, and reports concerning it have become less frequent. The use of hip arthroscopy appears to have rapidly increased over the decade just past. The central and peripheral compartments of the hip can easily reached be via minimal incisions. The torn labrum can be assessed, debrided, and repaired during arthroscopy, and any osseous deformities dynamically evaluated and reshaped. According to published studies, the outcome of arthroscopic treatment of labral tears is comparable with that of open methods, with the advantage of less invasion. Repair of labral pathology gave a better outcome than debridement, and additional symptomatic improvement may be obtained by the inclusion of femoral osteoplasty 14 , 15 .
The acetabular labrum is a fibrocartilaginous structure that is located circumferentially around the acetabular perimeter and attached to the transverse acetabular ligament posteriorly and anteriorly. Similar to the menisci of the knee, the labrum has limited vascularity and therefore poor healing potential, especially in the articular surface portion. The healing potential of the labrum is greatest at the peripheral capsulolabral junction. Manifestations of a torn labrum include thickening, swelling, degeneration and fraying, or sometimes a flap with a fully detached end. Quite a number of these labral lesions are irreparable. Labral debridement requires short operation and extremity traction times, and can result in excellent clinical outcomes 15 , 16 . Provided the extent of resection of the labrum is limited, the stability of the hip will not be substantially compromised. However, because the acetabular labrum plays a role in limiting expression of fluid from the joint space, its absence results in increased contact pressures are transmitted across the hip joint. Therefore, to preserve healthy acetabular labral tissue with good healing potential, labral repair/reattachment should be performed, and reports of such procedures are increasing 17 . Among the patients in this study, only two with relative healthy labra underwent labral repair.
Decompression of the femoral head‐neck junction (cam osteoplasty) may restore normal head‐neck offset and clearance of the femoral head within the acetabulum during full flexion and rotation. For pincer type impingement, resection of proliferated osseous rim can also be carried out under arthroscopy. In our experience, osteoplasty is not necessary for all osseous abnormalities in the femoral head‐neck junction. According to a radiological study with a minimum of 10 years follow‐up reported by Bardakos and Villar, a pisto‐grip deformity will not inevitably result in aggravation of osteoarthritis in the hip 18 . The individual geometry of the proximal femur and acetabulum partly influences the progression of arthritis in only one‐third of these patients. In our study, 11 cases were found to have an abnormal α angle >50°, however only seven were confirmed to have impingement by dynamic assessment under arthroscopy, and these seven underwent osteoplasty. In the remaining four cases, osteoplasty was not performed.
According to published articles, primary and revision arthroscopy have a similar complication rate, ranging from 1.4% to 5%, which is much lower than that of open surgery. The majority of the complications are associated with patient positioning and traction. Using the anterior portal runs a significant risk of nerve injury due to its proximity to the lateral femoral cutaneous nerve 14 . In this study, injury to the lateral femoral cutaneous nerve occurred in one patient (4.8%), and may have been caused by accidental activation of the foot switch while a flexible probe was being inserted through a metal sleeve in the anterior portal.
In summary, both the impingement test and MRA have high sensitivity and accuracy for the diagnosis of acetabular labral tears. Hip arthroscopy is a minimally invasive and safe procedure and has been proved to produce good results in the treatment of labral tears. Because of the small case numbers and short follow‐up period, the outcomes of our different arthroscopic procedures cannot be compared with one other, and the mid‐ and long‐term results need to be further investigated.
Disclosure
No benefits of any type have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript.
Acknowledgements
This study was supported by the National Nature Science Foundation of China (project number: 30672117).
References
- 1. Wang WG, Li ZR. Advancement in diagnosis and treatment of femoroacetabular impingement (Chin). Zhongguo Gu Yu Guan Jie Wai Ke Za Zhi, 2010, 3: 78–83. [Google Scholar]
- 2. Czerny C, Hofmann S, Urban M, et al MR arthrography of the adult acetabular capsular‐labral complex: correlation with surgery and anatomy. AJR Am J Roentgenol, 1999, 173: 345–349. [DOI] [PubMed] [Google Scholar]
- 3. Keogh MJ, Batt ME. A review of femoroacetabular impingement in athletes. Sports Med, 2008, 38: 863–878. [DOI] [PubMed] [Google Scholar]
- 4. Ganz R, Parvizi J, Beck M, et al Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res, 2003, 417: 112–120. [DOI] [PubMed] [Google Scholar]
- 5. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br, 1991, 73: 423–429. [DOI] [PubMed] [Google Scholar]
- 6. Philippon MJ, Maxwell RB, Johnston TL, et al Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc, 2007, 15: 1041–1047. [DOI] [PubMed] [Google Scholar]
- 7. McCarthy JC, Lee JA. Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin Orthop Relat Res, 2002, 405: 122–128. [DOI] [PubMed] [Google Scholar]
- 8. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol, 2007, 188: 1540–1552. [DOI] [PubMed] [Google Scholar]
- 9. Nötzli HP, Wyss TF, Stoecklin CH, et al The contour of the femoral head‐neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br, 2002, 84: 556–560. [DOI] [PubMed] [Google Scholar]
- 10. Beaulé PE, Zaragoza E, Motamedi K, et al Three‐dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res, 2005, 23: 1286–1292. [DOI] [PubMed] [Google Scholar]
- 11. James SL, Ali K, Malara F, et al MRI findings of femoroacetabular impingement. AJR Am J Roentgenol, 2006, 187: 1412–1419. [DOI] [PubMed] [Google Scholar]
- 12. Mintz DN, Hooper T, Connell D, et al Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy, 2005, 21: 385–393. [DOI] [PubMed] [Google Scholar]
- 13. Potter HG, Schachar J. High resolution noncontrast MRI of the hip. J Magn Reson Imaging, 2010, 31: 268–278. [DOI] [PubMed] [Google Scholar]
- 14. Shindle MK, Voos JE, Nho SJ, et al Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am, 2008, 90 (Suppl 4): 2–19. [DOI] [PubMed] [Google Scholar]
- 15. Beaulé PE, O'Neill M, Rakhra K. Acetabular labral tears. J Bone Joint Surg Am, 2009, 91: 701–710. [DOI] [PubMed] [Google Scholar]
- 16. Liu YJ, Li FX, Wang ZG, et al Arthroscopic debridement for acetabular labral tears: a report of ten cases (Chin). Zhongguo Yun Dong Yi Xue Za Zhi, 2005, 24: 696–698. [Google Scholar]
- 17. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy, 2009, 25: 369–376. [DOI] [PubMed] [Google Scholar]
- 18. Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow‐up. J Bone Joint Surg Br, 2009, 91: 162–169. [DOI] [PubMed] [Google Scholar]


