Abstract
The C 1 lateral mass screw technique is widely used for atlantoaxial fixation. However, C 2 nerve dysfunction may occur as a complication of this procedure, compromising the quality of life of affected patients. This is a review of the topic of C 2 nerve dysfunction associated with C 1 lateral mass screw fixation and related research developments. The C2 nerve root is located in the space bordered superiorly by the posterior arch of C1, inferiorly by the C2 lamina, anteriorly by the lateral atlantoaxial joint capsule, and posteriorly by the anterior edge of the ligamentum flavum. Some surgeons suggest cutting the C2 nerve root during C1 lateral mass screw placement, whereas others prefer to preserve it. The incidence, clinical manifestations, causes, management, and prevention of C 2 nerve dysfunction associated with C 1 lateral mass screw fixation are reviewed. Sacrifice of the C2 nerve root carries a high risk of postoperative numbness, whereas postoperative nerve dysfunction can occur when it has been preserved. Many surgeons have been working hard on minimizing the risk of postoperative C2 nerve dysfunction associated with C1 lateral mass screw fixation.
Keywords: C2 nerve dysfunction, C1 lateral mass screw, Atlantoaxial fixation, Atlantoaxial instability
Introduction
Posterior atlantoaxial fixation is widely used to treat atlantoaxial instability. C1 screw fixation, which includes the C1 lateral mass technique and C1 pedicle screw techniques, is the main technique used for atlantoaxial fixation1, 2, 3, 4. The C1 lateral mass screw technique was first described by Goel and Laheri in 19445, and popularized by Harms and Melcher, who reported on it in 20016. In 2002, Resnick and Benzel were the first to report C1 pedicle screw fixation7. And in 2003, Tan et al. introduced the C1 pedicle screw technique8. Since then, many studies have demonstrated the superiority of the C1 pedicle screw technique1, 2, 9. However, there is widespread agreement that the height of the C1 pedicle is the factor that most limits achievement of successful C1 pedicle screw fixation10, 11, 12. When the height is less than 4.0 mm, the pedicle is not able to accommodate the 3.5 mm‐diameter screw that is usually used for C1 fixation12. Thus, C1 pedicle screw fixation is not feasible in 8%–53.8% of patients8, 13, 14, 15, 16, 17, 18. Hence, the C1 lateral mass screw technique is still widely used. However, C2 nerve dysfunction may occur as a complication of C1 lateral mass screw fixation, comprising the quality of life of affected patients19, 20, 21, 22, 23. In addition, whether to cut the C2 nerve root during C1 lateral mass screw fixation is still controversial. We here review the topic of C2 nerve dysfunction associated with C1 lateral mass screw fixation and related research developments.
Anatomy
The C2 nerve root is located in the space bordered superiorly by the posterior arch of C1, inferiorly by the C2 lamina, anteriorly by the lateral atlantoaxial joint capsule, and posteriorly by the anterior edge of the ligamentum flavum (Fig. 1). The height of the C2 ganglion is 4.97 ± 0.92 mm on the right side and 4.60 ± 0.84 mm on the left side. The C2 ganglion occupies approximately 50% of the height of the space in the neutral position and approximately 65% in hyperextension with rotation positions24. A large venous plexus, which can cause bleeding, surrounds the C2 nerve root in the space. The C2 nerve root passes inferolateral to the lateral atlantoaxial joint and can be pulled downward during surgical maneuvering25.
Figure 1.
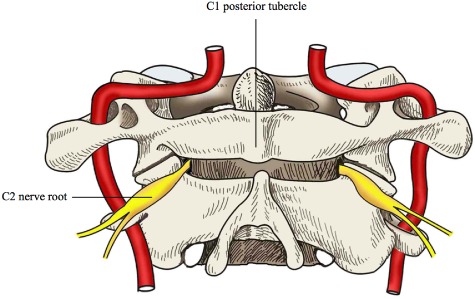
The C2 nerve root is located in the space bordered superiorly by the posterior arch of C1, inferiorly by the C2 lamina, anteriorly by the lateral atlantoaxial joint capsule, and posteriorly by the anterior edge of the ligamentum flavum.
The dorsal ramus of the C2 nerve emerges between the C1 posterior arch and C2 lamina, below the inferior oblique which it supplies, receives a connection from the C1 nerve dorsal ramus, and divides in to a large medial and smaller lateral branch. The medial branch, termed the great occipital nerve, ascends between the inferior oblique and semispinalis capitis, pierces the latter and the trapezius near their occipital attachments and is then joined by a filament from the medial branch of the third dorsal ramus. Ascending with the occipital artery, it divides into branches that connect with the lesser occipital nerve and supply the skin of the scalp as far anteriorly as the vertex26.
Management of the C2 Nerve Root during C1 Lateral Mass Screw Placement
Some surgeons suggest cutting the C2 nerve root during C1 lateral mass screw placement27, 28, 29, 30, 31, 32, whereas others prefer to preserve it33, 34, 35, 36, 37.
Cutting the C2 Nerve Root
In their initial study, Goel et al. used a screw–plate system for atlantoaxial fixation38. To leave enough space for the upper part of the plate, they chose a lower screw entry point than the later Harms technique. Because the screw and plate were placed where the C2 nerve root and its surrounding venous plexus lie, cutting the C2 nerve root was unavoidable (Fig. 2).
Figure 2.
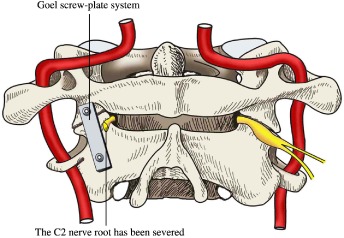
The Goel technique uses the screw‐plate system for atlantoaxial fixation; cutting the C2 nerve root is unavoidable.
Subsequently, cutting the C2 nerve root during C1 lateral mass screw placement was generally recommended. It was believed that cutting it simplified surgical maneuvering and resulted in less blood loss, shorter operative time and a lower screw malposition rate. Aryan et al. reported using a modified Harms technique for atlantoaxial fixation that used a screw–rod system and in which cutting the C2 nerve root was avoidable; however, they still cut it27. In their series, only one of 121 patients developed occipital neuralgia. However, they did not report how many patients had numbness in the region innervated by the C2 nerve. In their meta‐analysis, Elliot et al. found that sacrifice of the C2 nerve root resulted more frequently in postoperative numbness (11.6% vs. 1.3%) but less frequently in neuralgia (0.3% vs. 4.7%), was associated with less blood loss (213 mL vs. 417 mL) and shorter operative time (118 min vs. 132 min) than when the C2 nerve root was preserved2. They concluded that cutting the C2 nerve root during C1 lateral mass screw placement resulted in better outcomes, even though 11.6% of the patients have postoperative numbness, an outcome that is unacceptable to some patients. Both Squires and Molinari29 and Hamilton et al.28 reported that, in elderly patients, C1 lateral mass screw placement with intentional cutting of the C2 nerve root resulted in satisfactory outcomes, albeit with postoperative numbness. Recently, Patel et al. have reported the clinical outcomes of routinely cutting the C2 nerve root during C1 lateral mass screw placement in children. None of their 15 cases C2 developed nerve dysfunction39.
Preserving the C2 Nerve Root
If they elect to preserve the C2 nerve root, surgeons have to face problems such as damage to the C2 nerve root, severe bleeding from the associated venous plexus and inadequate exposure.
With Harms technique, the entry point for the C1 screw is the midpoint of the posterior inferior part of the C1 lateral mass6. For atlantoaxial fixation, they use a screw–rod system that looks like a viaduct and allows the C2 nerve root to pass through the “arch of the viaduct” (Fig. 3). The C1 screw they use is a partially threaded one: the 8 mm unthreaded portion of the screw stays above the bony surface of the lateral mass, minimizing the risk of irritation to the C2 nerve root. Since then, many authors have reported their own modified C1 screw entry points8, 11, 13, 40. Modifications that heighten the screw entry point minimize the risk of damage to the C2 nerve root. With these modifications of the original technique, more and more surgeons are tending to preserve the C2 nerve root during C1 lateral mass screw fixation.
Figure 3.
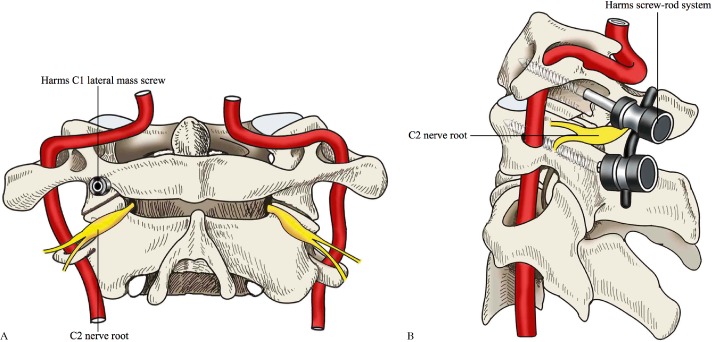
Harms C1 lateral mass screw technique (A) A screw–rod system is used, allowing preservation of the C2 nerve root. (B) The C2 nerve root passes through the “arch of the viaduct” of the screw–rod system.
C2 Nerve Dysfunction Associated with C1 Lateral Mass Screw Fixation
Incidence
The incidence of C2 nerve dysfunction after atlantoaxial fixation is not clear, reported rates ranging from 0–33%1, 6, 38, 40. Goel et al. cut the C2 nerve root during C1 screw placement; 18/160 patients in their study reported postoperative sensory loss in the distribution of the C2 nerve38. They did not specifically ask about postoperative numbness in the distribution of the C2 nerve during follow‐up. It is possible that patients were so satisfied with their limb function that they ignored anesthesia in the occipital scalp. Thus, the incidence of postoperative C2 nerve dysfunction is likely greater than the reported incidence. In Harms and Melcher's study, no C2 nerve dysfunction was reported in a cohort of 37 patients6. It may make more sense to discuss the incidence according to the specific circumstances. Elliott et al.'s meta‐analysis showed that 11.6% of patients in whom the C2 nerve root has been sacrificed experience postoperative C2 numbness, whereas only 0.3% experience C2 neuralgia. However, 4.7% of patients who have undergone C1 screw placement with preservation of the C2 nerve root experience postoperative C2 neuralgia and 1.3% experience C2 numbness2.
Clinical Manifestations
The clinical manifestations of C2 nerve dysfunction are sensory changes in the distribution of the C2 nerve, including neuralgia, numbness, dysesthesia and paresthesia1, 2, 20, 27, 30, 38. In addition, some patients report indescribable discomfort in the occipital region28, 30.
Causes of Injury to the C2 Nerve Root
The mechanism of C2 nerve dysfunction associated with C1 lateral mass screw fixation is poorly understood23. However, possible causes are as follows: (i) transection of the C2 nerve root; however, the effects of this are unclear41; (ii) excessive caudal retraction during exposure of the C1 lateral mass screw entry point22; (iii) damage to the C2 nerve root during management of bleeding from the associated venous plexus1; (iv) reduction of C1 onto C2 21, 22; and (v) impingement or irritation from the C1 lateral mass screw6, 20, 23.
Management and Prognosis
There are currently no clear guidelines for the management of C2 nerve dysfunction associated with C1 lateral mass screw fixation. Medication is often used1, 20, 21, 22. If the symptoms are severe and do not respond satisfactorily to medication, repeated C2 ganglion blocks can be tried21. In cases with severe or persisting symptoms, some authors recommend extraction of the screw19, 23, which can achieve good results23, but sometimes fails to do so22.
Symptoms of C2 nerve dysfunction often subside spontaneously19; however, in some cases medication, C2 ganglion block, or even screw extraction are needed21, 23. Of note, even after removal of the instrumentation, the pain still persists in some cases22.
Prevention
Sacrifice of the C2 nerve root carries a high risk of postoperative numbness, whereas postoperative nerve dysfunction can occur when it has been preserved. Many surgeons have been working hard on minimizing the risk of postoperative C2 nerve dysfunction associated with C1 lateral mass screw fixation.
Gunnarsson et al. used partially threaded C1 screws with smooth shanks to reduce irritation to the C2 nerve root; however, 3/25 patients still reported postoperative C2 neuralgia in their case series20.
In their case report, Rhee et al. provided several tips on how to prevent this complication. First, avoid intraoperative hyperextension of the neck21. Second, place the head of the C1 screw sufficiently dorsally to leave enough space in the foraminal area for the C2 nerve root. Third, use partially threaded C1 screws with smooth shanks to minimize the chance of irritation to the C2 nerve root. Fourth, if the surrounding tissue looks tense around the C1 screw, perform additional mobilization of the C2 nerve root. Fifth, use a higher entry point and insert the C1 lateral mass screw via the posterior arch if it can accommodate it. Finally, carefully place fusion materials on the C1–C2 posterior arches.
Pan et al. reported using a 3–5 mm diameter bone wax column to protect both the venous sinus and the C2 nerve root during surgical maneuvering1. In their study, none of the 22 patients who underwent C1 lateral mass screw placement with this modified technique developed postoperative numbness, whereas 4/12 patients who underwent screw placement with Harms technique reported postoperative C2 nerve dysfunction.
In 2013, Lee et al. reported a modification of C1 lateral mass screw insertion, which is also called the notching technique, designed to avoid postoperative C2 nerve dysfunction11. They insert the C1 screw at the junction of the C1 posterior arch and the midpoint of the posterior inferior portion of the C1 lateral mass with a notch at the entry point to facilitate screw insertion. The notch allows the screw to be placed farther away from the C2 ganglion than with the Harms technique and provides a screw trajectory that is less cranially tilted. Only 1/12 cases had mild postoperative unilateral C2 neuralgia, which had resolved 6 weeks after surgery.
Recently, Huang et al. proposed a preoperative measure, the height for screw index, as a predictor of C2 nerve dysfunction in patients who undergo C1 lateral mass screw fixation3. The height for screw index is defined as the difference in height between C2 ganglion and its corresponding foramen and is measured on CT images. This is the first detailed preoperative evaluation designed to prevent C2 nerve dysfunction; however, this evaluation is not feasible in approximately 46% of patients because of failure to distinguish the C2 ganglion on CT images. Another recent study by Huang et al. showed that if there is a medullary canal in the C1 pedicle, it is possible to finish C1 pedicle screw fixation in the atlas, the pedicle height of which is less than 4 mm; this finding has changed the traditional view that C1 pedicle fixation can be performed only when the C1 pedicle is more than 4 mm high4. In these patients, C1 pedicle fixation rather than C1 lateral mass screw fixation can be performed to avoid postoperative C2 nerve dysfunction.
Disclosure: The submitted manuscript does not contain information regarding medical equipment. This work is not supported by any foundation and does not directly or indirectly have any formal relationships with business groups.
References
- 1. Pan J, Li L, Qian L, Tan J, Sun G, Li X. C1 lateral mass screw insertion with protection of C1–C2 venous sinus: technical note and review of the literature. Spine (Phila Pa 1976), 2010, 35: E1133–E1136. [DOI] [PubMed] [Google Scholar]
- 2. Elliott RE, Tanweer O, Frempong‐Boadu A, Smith ML. Impact of starting point and C2 nerve status on the safety and accuracy of C1 lateral mass screws: meta‐analysis and review of the literature. J Spinal Disord Tech, 2013, 35 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Huang DG, Hao DJ, Jiang YH, et al The height for screw index (HSI) predicts the development of C2 nerve dysfunction associated with C1 lateral mass screw fixation for atlantoaxial instability. Eur Spine J, 2014, 23: 1092–1098. [DOI] [PubMed] [Google Scholar]
- 4. Huang DG, He SM, Pan JW, et al Is the 4 mm height of the vertebral artery groove really a limitation of C1 pedicle screw insertion? Eur Spine J, 2014, 23: 1109–1114. [DOI] [PubMed] [Google Scholar]
- 5. Goel A, Laheri V. Plate and screw fixation for atlanto‐axial subluxation. Acta Neurochir (Wien), 1994, 129: 47–53. [DOI] [PubMed] [Google Scholar]
- 6. Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976), 2001, 26: 2467–2471. [DOI] [PubMed] [Google Scholar]
- 7. Resnick DK, Benzel EC. C1–C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery, 2002, 50: 426–428. [DOI] [PubMed] [Google Scholar]
- 8. Tan M, Wang H, Wang Y, et al Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976), 2003, 28: 888–895. [DOI] [PubMed] [Google Scholar]
- 9. Richter M, Schmidt R, Claes L, Puhl W, Wilke HJ. Posterior atlantoaxial fixation: biomechanical in vitro comparison of six different techniques. Spine (Phila Pa 1976), 2002, 27: 1724–1732. [DOI] [PubMed] [Google Scholar]
- 10. Ma XY, Yin QS, Wu ZH, et al C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976), 2009, 34: 371–377. [DOI] [PubMed] [Google Scholar]
- 11. Lee SH, Kim ES, Eoh W. Modified C1 lateral mass screw insertion using a high entry point to avoid postoperative occipital neuralgia. J Clin Neurosci, 2013, 20: 162–167. [DOI] [PubMed] [Google Scholar]
- 12. Lin JM, Hipp JA, Reitman CA. C1 lateral mass screw placement via the posterior arch: a technique comparison and anatomic analysis. Spine J, 2013, 13: 1549–1555. [DOI] [PubMed] [Google Scholar]
- 13. Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976), 2005, 30: 1519–1523. [DOI] [PubMed] [Google Scholar]
- 14. Christensen DM, Eastlack RK, Lynch JJ, Yaszemski MJ, Currier BL. C1 anatomy and dimensions relative to lateral mass screw placement. Spine (Phila Pa 1976), 2007, 32: 844–848. [DOI] [PubMed] [Google Scholar]
- 15. Kim JH, Kwak DS, Han SH, Cho SM, You SH, Kim MK. Anatomic consideration of the C1 laminar arch for lateral mass screw fixation via C1 lateral lamina: a landmark between the lateral and posterior lamina of the C1. J Korean Neurosurg Soc, 2013, 54: 25–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gebauer M, Barvencik F, Briem D, et al Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. Eur Spine J, 2010, 19: 85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Blagg SE, Don AS, Robertson PA. Anatomic determination of optimal entry point and direction for C1 lateral mass screw placement. J Spinal Disord Tech, 2009, 22: 233–239. [DOI] [PubMed] [Google Scholar]
- 18. Lee MJ, Cassinelli E, Riew KD. The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine (Phila Pa 1976), 2006, 31: 2798–2801. [DOI] [PubMed] [Google Scholar]
- 19. Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw‐rod system. Eur Spine J, 2007, 16: 479–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gunnarsson T, Massicotte EM, Govender PV, Raja Rampersaud Y, Fehlings MG. The use of C1 lateral mass screws in complex cervical spine surgery: indications, techniques, and outcome in a prospective consecutive series of 25 cases. J Spinal Disord Tech, 2007, 20: 308–316. [DOI] [PubMed] [Google Scholar]
- 21. Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by C1–C2 Harms construct. J Korean Neurosurg Soc, 2008, 43: 111–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Conroy E, Laing A, Kenneally R, Poynton AR. C1 lateral mass screw‐induced occipital neuralgia: a report of two cases. Eur Spine J, 2010, 19: 474–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Myers KD, Lindley EM, Burger EL, Patel VV. C1–C2 fusion: postoperative C2 nerve impingement–is it a problem? Evid Based Spine Care J, 2012, 3: 53–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bilge O. An anatomic and morphometric study of C2 nerve root ganglion and its corresponding foramen. Spine (Phila Pa 1976), 2004, 29: 495–499. [DOI] [PubMed] [Google Scholar]
- 25. Hong X, Dong Y, Yunbing C, Qingshui Y, Shizheng Z, Jingfa L. Posterior screw placement on the lateral mass of atlas: an anatomic study. Spine (Phila Pa 1976), 2004, 29: 500–503. [DOI] [PubMed] [Google Scholar]
- 26. Peter LW. Gray's Anatomy, 37th edn Edinburgh: Churchill Livingstone, 1989; 1125–1130. [Google Scholar]
- 27. Aryan HE, Newman CB, Nottmeier EW, Acosta FL Jr, Wang VY, Ames CP. Stabilization of the atlantoaxial complex via C‐1 lateral mass and C‐2 pedicle screw fixation in a multicenter clinical experience in 102 patients: modification of the Harms and Goel techniques. J Neurosurg Spine, 2008, 8: 222–229. [DOI] [PubMed] [Google Scholar]
- 28. Hamilton DK, Smith JS, Sansur CA, Dumont AS, Shaffrey CI. C‐2 neurectomy during atlantoaxial instrumented fusion in the elderly: patient satisfaction and surgical outcome. J Neurosurg Spine, 2011, 15: 3–8. [DOI] [PubMed] [Google Scholar]
- 29. Squires J, Molinari RW. C1 lateral mass screw placement with intentional sacrifice of the C2 ganglion: functional outcomes and morbidity in elderly patients. Eur Spine J, 2010, 19: 1318–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kang MM, Anderer EG, Elliott RE, Kalhorn SP, Frempong‐Boadu A. C2 nerve root sectioning in posterior C1–2 instrumented fusions. World Neurosurg, 2012, 78: 170–177. [DOI] [PubMed] [Google Scholar]
- 31. Goel A. Cervical ganglion 2 (CG2) neurectomy: a window to the atlantoaxial joint. World Neurosurg, 2012, 78: 78–79. [DOI] [PubMed] [Google Scholar]
- 32. Menezes AH. C2 neurectomy. World Neurosurg, 2012, 78: 80–81. [DOI] [PubMed] [Google Scholar]
- 33. Jeon SW, Jeong JH, Choi GH, Moon SM, Hwang HS, Choi SK. Clinical outcome of posterior fixation of the C1 lateral mass and C2 pedicle by polyaxial screw and rod. Clin Neurol Neurosurg, 2012, 114: 539–544. [DOI] [PubMed] [Google Scholar]
- 34. Wu JC, Tu TH, Mummaneni PV. Techniques of atlantoaxial fixation and the resection of C2 nerve root. World Neurosurg, 2012, 78: 603–604. [DOI] [PubMed] [Google Scholar]
- 35. Vergara P, Bal JS, Hickman Casey AT, Crockard HA, Choi D. C1–C2 posterior fixation: are 4 screws better than 2? Neurosurgery, 2012, 71: 86–95. [DOI] [PubMed] [Google Scholar]
- 36. Joaquim AF, Ghizoni E, Rubino PA, et al Lateral mass screw fixation of the atlas: surgical technique and anatomy. World Neurosurg, 2010, 74: 359–362. [DOI] [PubMed] [Google Scholar]
- 37. Desai R, Stevenson CB, Crawford AH, Durrani AA, Mangano FT. C‐1 lateral mass screw fixation in children with atlantoaxial instability: case series and technical report. J Spinal Disord Tech, 2010, 23: 474–479. [DOI] [PubMed] [Google Scholar]
- 38. Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery, 2002, 51: 1351–1356; discussion 1356–1357. [PubMed] [Google Scholar]
- 39. Patel AJ, Gressot LV, Boatey J, Hwang SW, Brayton A, Jea A. Routine sectioning of the C2 nerve root and ganglion for C1 lateral mass screw placement in children: surgical and functional outcomes. Childs Nerv Syst, 2013, 29: 93–97. [DOI] [PubMed] [Google Scholar]
- 40. Yeom JS, Kafle D, Nguyen NQ, et al Routine insertion of the lateral mass screw via the posterior arch for C1 fixation: feasibility and related complications. Spine J, 2012, 12: 476–483. [DOI] [PubMed] [Google Scholar]
- 41. Elliott RE, Kang MM, Smith ML, Frempong‐Boadu A. C2 nerve root sectioning in posterior atlantoaxial instrumented fusions: a structured review of literature. World Neurosurg, 2012, 78: 697–708. [DOI] [PubMed] [Google Scholar]


