Key Points
Question
Does acupuncture increase the likelihood of a live birth in women undergoing in vitro fertilization?
Findings
In this randomized clinical trial of 824 women, the rate of live births was 18.3% among women who received acupuncture vs 17.8% among women who received a sham acupuncture control, a nonsignificant difference.
Meaning
These findings do not support the use of acupuncture when administered at the time of ovarian stimulation and embryo transfer to improve the rate of live births.
Abstract
Importance
Acupuncture is widely used by women undergoing in vitro fertilization (IVF), although the evidence for efficacy is conflicting.
Objective
To determine the efficacy of acupuncture compared with a sham acupuncture control performed during IVF on live births.
Design, Setting, and Participants
A single-blind, parallel-group randomized clinical trial including 848 women undergoing a fresh IVF cycle was conducted at 16 IVF centers in Australia and New Zealand between June 29, 2011, and October 23, 2015, with 10 months of pregnancy follow-up until August 2016.
Interventions
Women received either acupuncture (n = 424) or a sham acupuncture control (n = 424). The first treatment was administered between days 6 to 8 of follicle stimulation, and 2 treatments were administered prior to and following embryo transfer. The sham control used a noninvasive needle placed away from the true acupuncture points.
Main Outcomes and Measures
The primary outcome was live birth, defined as the delivery of 1 or more living infants at greater than 20 weeks’ gestation or birth weight of at least 400 g.
Results
Among 848 randomized women, 24 withdrew consent, 824 were included in the study (mean [SD] age, 35.4 [4.3] years); 371 [45.0%] had undergone more than 2 previous IVF cycles), 607 proceeded to an embryo transfer, and 809 (98.2%) had data available on live birth outcomes. Live births occurred among 74 of 405 women (18.3%) receiving acupuncture compared with 72 of 404 women (17.8%) receiving sham control (risk difference, 0.5% [95% CI, −4.9% to 5.8%]; relative risk, 1.02 [95% CI, 0.76 to 1.38]).
Conclusions and Relevance
Among women undergoing IVF, administration of acupuncture vs sham acupuncture at the time of ovarian stimulation and embryo transfer resulted in no significant difference in live birth rates. These findings do not support the use of acupuncture to improve the rate of live births among women undergoing IVF.
Trial Registration
anzctr.org.au Identifier: ACTRN12611000226909
This randomized clinical trial compares the effects of true vs sham acupuncture on live births among women undergoing assisted reproduction with in vitro fertilization.
Introduction
Complementary therapies are widely used by individuals undergoing assisted reproductive technology.1,2,3 Acupuncture is a frequently used adjunctive treatment during in vitro fertilization (IVF). Acupuncturists from the United Kingdom4 and Australia5 indicate use during IVF is a frequent reason for women seeking treatment. Research has focused on evaluating the effects of acupuncture administered prior to and following an embryo transfer.
Early studies suggested a potential benefit from acupuncture in improving IVF outcomes6,7,8; however, with an increased number of randomized clinical trials (RCTs), evidence of an effect from acupuncture compared with controls has become less clear. Systematic reviews, including a Cochrane review of 14 trials, found no statistically significant difference in clinical pregnancy or live birth rates compared with a control.9,10 However, there are significant methodological limitations affecting the quality of evidence. Some trials were at risk of selection bias. All trials reported on clinical pregnancy; only 5 RCTs using sham acupuncture reported on the key outcome of live birth.11,12,13,14,15 Overall, the study sample sizes were small, and there was significant study heterogeneity. These limitations have hampered development of recommendations for clinical practice and highlighted the need for a well-designed RCT to address the issues.9,10 The objective of this multicenter RCT was to assess the effect of acupuncture vs sham acupuncture during IVF on live birth rates.
Methods
Study Design
Recruitment of eligible women was undertaken at 16 IVF centers in Australia and New Zealand. The trial protocol is available in Supplement 1 and has been published.16 Ethical approval was obtained from the Western Sydney University Human Ethics Committee and at the respective sites. Women gave written informed consent.
Participants
Inclusion criteria were women aged 18 to 42 years undergoing a fresh IVF or intracytoplasmic sperm injection cycle and not using acupuncture. Exclusion criteria were women undergoing a frozen embryo transfer, previous randomization to the study, planning preimplantation genetic diagnosis, or receiving donor eggs. We made one change to the protocol after commencing the study, which was approved by all ethics committees. We initially included only women with recurrent IVF failure and unsuccessful clinical pregnancies from 4 IVF centers. However, these women were high current users of acupuncture, and in June 2013, following a review by the data and safety monitoring committee, a decision was made to revise the inclusion criteria to increase eligibility to the trial by removing the criteria requiring women to have previous failed IVF cycles and poor treatment outcomes, and to increase the number of recruitment sites.
Seventy-eight women who met the study inclusion criteria but declined the trial were invited to participate in a nonrandomized treatment-as-usual group. Data from this group of women will be reported separately. Enrollment commenced June 29, 2011, and ceased October 23, 2015, due to the end of funding for recruitment. Follow-up of live births was completed in August 2016.
Randomization and Blinding
The randomization sequence was computer generated and was undertaken using the method of minimization17 stratified by the number of previous embryo transfer cycles (0-1, 2-6, and >6), woman’s age (<38 and 38-42 years), and study site. The algorithm was configured to incorporate a window of 3 to minimize forcing of treatment allocations. Allocation concealment was ensured by use of an interactive centralized telephone computer program administered by the National Health and Medical Research Council Clinical Trials Centre, Sydney, Australia. Study participants, fertility specialists and nurses, and the analyst were blinded to group allocation. The clinical trial coordinator and acupuncturists were not blinded to group allocation. Study site research nurses who were blind to group allocation enrolled women into the study and collected clinical outcome data. Blinding was maintained until completion of analysis.
Interventions
Women were recruited at the time of the decision to undergo an IVF or intracytoplasmic sperm injection cycle, and randomization occurred prior to commencement of follicle-stimulation protocols. It was intended that all women receive standard ovarian stimulation, egg retrieval, fertilization, and embryo transfer as determined by their treating clinician. Following randomization, women made an appointment with the study acupuncturist onsite at the IVF centers or nearby. The first treatment was administered between days 6 and 8 of ovarian stimulation, and 2 treatments were given on the day of embryo transfer. The acupuncturists had a minimum of 2 years clinical experience, held membership with a national professional association, and in Australia, were registered with the national Australian Health Practitioner Regulation Agency. All acupuncturists were trained in the treatment protocol with annual refresher training provided. Practitioner notes were reviewed following the participant’s last treatment to assess treatment fidelity.
The acupuncture protocol was developed using a Delphi method, with treatment characteristics retained on reaching 80% group consensus.18 The treatment strategy was based on traditional Chinese medicine. Acupuncture points were located on the innervation areas to the uterus and ovaries in the abdominal muscles and in the leg to stimulate blood flow to the uterus, and in areas located on the arms and legs that inhibit the central nervous system outflow and the biological stress response. The first treatment involved core points Guilai ST-29, Guanyuan Ren-4, Qihai Ren-6, Sanyinjiao SP-6, and Xuehai SP-10. In addition, up to 5 additional points based on the traditional Chinese medicine diagnosis were selected from a standardized protocol. Manual acupuncture was applied, the needling sensation de qi was attained, and needles were restimulated midway through the 25-minute treatment.
On the day of embryo transfer, an initial treatment was administered within 1 hour prior to embryo transfer and comprised points Guilai ST-29, Diji SP-8, Xuehai SP-10, Taichong LR-3, Guanyuan Ren-4; 1 point from Shenmen HT-7, Neiguan PC-6, or YinTang; and auricular point Zhigong. Following embryo transfer, the second acupuncture treatment was administered including points Baihui DU-20, Taixi KD-3, Zusanli ST-36, Sanyinjiao SP-6, Neiguan PC-6, and auricular point ShenMen. Needles were applied using the Park device,19 comprised of a plastic ring and a guide tube, with a double-sided adhesive ring to facilitate maintenance of blinding for the participant.
The sham control group received noninsertive acupuncture using the Park sham needle supported by the Park device.19 This needle has a retractable needle shaft and a blunt tip. Acupuncturists were instructed to lightly place the sham needle to the surface of the skin with no manipulation of the needle to minimize any physiological effect.20 The sham needle can lead to weak physiological effects but has been shown to stimulate different brain activity than acupuncture.21 To minimize physiological effects, we used sham points at locations away from known acupuncture points and with no known function.22 Sham points were described in relation to anatomical landmarks. Sham acupuncture was administered at 6 points for each of the treatments. Needle placement duration was the same as for the acupuncture group.16 Additional details on the interventions, which followed STRICTA guidelines,23 are provided in eMethods, eTable 1, and eFigure 1 in Supplement 2.
Outcomes
The primary outcome was a live birth, defined as the delivery of 1 or more living infants at greater than 20 weeks’ gestation or birth weight of at least 400 g. Prespecified secondary outcomes were miscarriage, clinical pregnancy, anxiety, quality of life, infertility self-efficacy, and adverse events. The definition of clinical pregnancy was amended post hoc to the definition used by the National Perinatal Epidemiology and Statistics Unit, defined as evidence on ultrasonography of an intrauterine sac with or without a fetal heart.24 The prespecified outcomes quality of life, infertility self-efficacy, and anxiety are not reported in this article.
Post hoc secondary outcomes included total dose of follicle-stimulating hormone, numbers of oocytes aspirated and fertilized, stage of embryo development at transfer, pregnancy loss (defined as termination, ectopic pregnancy, stillbirth, and neonatal death), gestational age, birth weight, congenital abnormality, and days in the nursery of the infant. Clinical outcomes were collected when the outcome of the IVF cycle was known and continued until delivery. Adverse events from the intervention were collated from the acupuncturists and from women completing self-report questionnaires following embryo transfer and at 2 and 14 weeks from trial entry.
Baseline characteristics, including sociodemographic characteristics, were collected to describe the diversity of the study population. Race/ethnicity was assessed using predetermined fixed options and determined by the participant. Blinding to group allocation was assessed through questioning participants about their perceived group allocation following the last treatment and at 2 weeks after embryo transfer. Blinding was assessed using the Bang blinding index.25 This index is scaled to an interval of −1 to 1, with 1 being complete lack of blinding, 0 being consistent with perfect blinding, and −1 indicating guessing.
Study Power
Combining pilot data, evidence from the systematic reviews and clinical advice, we estimated that a 7–percentage point or greater increase in the proportion of live births would be clinically important.8,10 To obtain 80% power at a 5% significance level for a 2-sided test, we assumed a proportion of 13.4%8 live births in the control group and 20.4% live births in the acupuncture group, requiring 449 participants per group. We estimated 30% attrition from the study, with loss arising from canceled cycles or no embryo transfer and study withdrawal. In total, 1168 women were required.
Statistical Analysis
An intention-to-treat analysis was planned; however, analysis was performed on a cohort excluding women who withdrew consent for use of their data and excluding those for whom data on live birth were not available. The characteristics of the women randomized to each treatment group were summarized using counts and percentages for categorical variables and means and SDs for numeric variables.
For the primary analysis, we first compared the proportions of women with live births or each secondary outcome in the 2 groups for all participants using risk differences (RDs) and relative risks (RRs) with associated 95% CIs and a hypothesis test for no effect. Twenty-four women no longer met the inclusion criteria between randomization and commencement of IVF treatment (ie, conceived naturally or discontinued IVF) and were classified as postrandomization exclusions. However, we were able to obtain data on live births for 9 of these women, and on clinical pregnancy from 14 women. These data were included in the analysis of these outcomes.
To assess the effect of missing data, we performed post-hoc sensitivity analyses, fitting best- and worst-case scenarios. For the best-case scenario, we assumed all unknown events in the acupuncture group were positive (live birth, successfully pregnant) and those in the sham acupuncture group were negative. For the worst-case scenario, we assumed none of the women with missing data in the acupuncture group became pregnant, and all of the women with missing data in the sham acupuncture group did become pregnant. A post-hoc–adjusted analysis was performed for the stratification variables using a log-binary mixed model with study center as a random effect. Exploratory analyses investigated the differences between study centers in the risk of live births visually as a forest plot with the associated I2 statistic quantifying the level of unexplained variation between centers.
We performed an exploratory per-protocol analysis examining the outcomes for women undergoing an embryo transfer (excluding women with canceled cycles). In this group, we also investigated the influence of potential outcome modifiers including cleavage vs blastocyst embryo stage of development, previous number of IVF cycles, and number of treatment sessions received on selected clinical outcomes between study groups. The number of treatment sessions attended was classified as those with 0 to 1 vs 2 or more, reflecting a maximum of 3 treatments administered, 2 of which were delivered on the day of embryo treatment. No adjustment was made for the multiple comparisons undertaken in the post-hoc analysis. Two-sided P < .05 indicated statistical significance. SAS version 9.4 (SAS Institute) and STATA 14 (StataCorp) were used for statistical analyses.
An independent expert data and safety monitoring committee met annually to monitor safety and advise on trial design decisions. This committee was composed of independent members with clinical and statistical expertise who had no conflicts of interest and no involvement in the running of the trial. The data and safety monitoring committee charter included prespecified stopping rules. Because of slow recruitment, an unplanned futility analysis of all clinical outcomes was undertaken in July 2015. Advice from the committee was presented to the study investigators, and a recommendation was made to continue to the end of funding period for recruitment.
Results
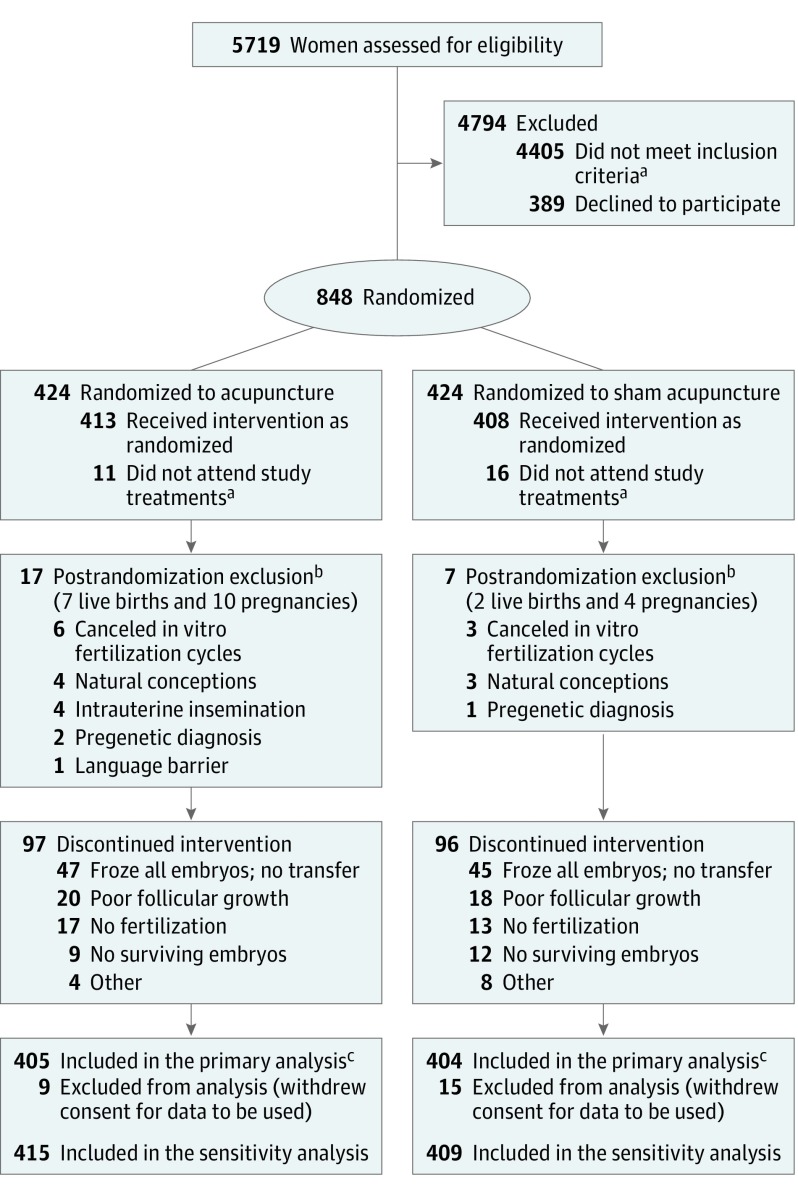
A total of 848 women intending to undergo a fresh IVF cycle were randomized to the trial (424 acupuncture; 424 sham control) by the end of the funding period (Figure). Twenty-four women withdrew consent for their data to be used in the analysis. Prior to receiving their first study treatment, 24 women were excluded due to noncommencement of their IVF cycle or insufficient English to complete all measures. Some data became available from these 24 women (9 for live births and 14 for clinical pregnancy). Data were analyzed from 809 women (405 acupuncture; 404 sham control) for the primary analysis of the primary outcome of live birth and from 824 women (415 acupuncture; 409 sham control) for the sensitivity analysis. Data were analyzed from 814 women (408 acupuncture; 406 sham control) for the analysis of the secondary outcome of clinical pregnancy and from 824 (415 acupuncture; 409 sham control) for the sensitivity analysis. Cancelation of the IVF cycle (failed stimulation, no oocyte retrieval or embryo transfer) was reported for 193 women. Therefore, 607 women received the intended treatment of embryo transfer (301 acupuncture; 306 sham control).
Figure. Flow of Participants Randomized to Acupuncture vs Sham Acupuncture.
aReasons for which women did not meet inclusion criteria or did not attend study treatments are not available.
bPostrandomization exclusions did not receive treatment because following randomization, they did not meet the eligibility criteria, ie, their type of treatment changed or they got pregnant naturally; therefore, there was no need for in vitro fertilization or acupuncture. However, some of their data were included in the sensitivity analysis.
cPrimary analysis excludes women who withdrew consent for data to be used and those excluded postrandomization; included are the cases with live births.
Baseline demographics are shown in Table 1 and were balanced between groups. The mean (SD) age was 35.4 (4.3) years, 245 women (29.7%) underwent their first IVF cycle, and 588 women (71.4%) had experienced infertility for longer than 2 years. The delivery of treatments by acupuncturists was balanced between groups. Adherence to the intervention by women was balanced between groups, 538 (65.5%) received 3 treatments, 32 (3.9%) received 2 treatments, and 210 (25.5%) received 1 treatment only. Seventy-eight acupuncturists provided a median of 8 treatments to the treatment group, and 82 acupuncturists provided a median of 7.5 to the sham control group.
Table 1. Baseline Characteristics of Trial Participantsa.
| Characteristic | No./Total No. (%) | |
|---|---|---|
| Acupuncture | Sham Acupuncture Control | |
| Age, mean (SD), y | 35.4 (4.3) | 35.5 (4.3) |
| Duration of infertility, y | ||
| <2 | 113/414 (27.3) | 119/406 (29.3) |
| 2-5 | 198/414 (47.8) | 195/406 (48.0) |
| >5 | 103/414 (24.9) | 92/406 (22.7) |
| Fertility diagnosis | ||
| Male factor | 130/415 (31.3) | 117/409 (28.6) |
| Tubal | 28/415 (6.8) | 40/409 (9.8) |
| Unexplained | 155/415 (37.4) | 147/409 (35.9) |
| Endometriosis | 39/415 (9.4) | 50/409 (12.2) |
| Other includes polycystic ovarian syndrome | 117/415 (28.2) | 113/409 (27.6) |
| Parity | ||
| Nulliparous | 303/414 (73.0) | 303/408 (74.3) |
| No. of prior IVF cycles | ||
| 0 | 127/414 (30.7) | 118/409 (28.9) |
| 1 | 102/414 (24.6) | 105/409 (25.6) |
| ≥2 | 185/414 (44.7) | 186/409 (45.5) |
| BMI, mean (SD) | 25.8/413 (5.5) | 26.0/406 (5.8) |
| Previous acupuncture use | 225/413 (54.5) | 200/407 (49.1) |
| Current smoker | 16/415 (3.9) | 16/407 (3.9) |
| Employed full time | 244/412 (59.2) | 250/407 (61.3) |
| Highest education | ||
| Primary or high school | 53/415 (12.8) | 76/409 (18.6) |
| Vocational (noncompulsory) or university | 362/415 (87.2) | 333/409 (81.4) |
| Race/ethnicity | ||
| White | 314/415 (75.6) | 322/407 (79.1) |
| Asian | 70/415 (16.9) | 56/407 (13.8) |
| Otherb | 31/415 (7.5) | 29/407 (7.1) |
| Acupuncture treatments received | ||
| 0 | 24/413 (5.8) | 17/408 (4.2) |
| 1 | 109/413 (26.4) | 101/408 (24.7) |
| 2 | 16/413 (3.9) | 16/408 (3.9) |
| 3 | 264/413 (63.9) | 274/408 (67.2) |
| No. of treatments provided within study | 933 | 955 |
| No. of acupuncturistsc | 78 | 82 |
| Treatments per practitioner, median (IQR) | 9 (4-18) | 7.5 (3-17) |
| Maximum treatments by one individual (% of total) | 69 (7.4) | 66 (6.9) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range; IVF, in vitro fertilization.
Nine women and 15 women in the acupuncture and sham acupuncture groups, respectively, withdrew consent for use of their data.
Other includes aboriginal and Torres Strait Islander, Maori, and Polynesian.
A total of 84 separate acupuncturists provided their services. The most services any one individual provided was 135 (69 in the acupuncture group and 66 in the sham group); this practitioner provided the maximum number of treatments in both groups.
Primary Outcome
The frequency of live births did not differ statistically between groups in the intention-to-treat analysis: 74 of 405 women (18.3%) randomized to acupuncture had a live birth compared with 72 of 404 (17.8%) in the sham control (RD, 0.5% [95% CI, −4.9% to 5.8%]; RR, 1.02 [95% CI, 0.76 to 1.38]) (Table 2). The likelihood of a live birth was not statistically different between the 2 groups after adjusting for age, number of previous IVF cycles, and participating IVF center (adjusted RR, 1.03 [95% CI, 0.77 to 1.38]).
Table 2. Primary Analysis and Post Hoc Analyses of Live Birth Outcomes.
| No./Total No. (%) | Risk Difference, % (95% CI) |
Relative Risk (95% CI) | Adjusted Modela | |||
|---|---|---|---|---|---|---|
| Acupuncture | Sham Acupuncture Control | Relative Risk Estimate (95% CI) | P Value | |||
| Primary Outcome | ||||||
| Live births among participants in primary analysis cohort | 74/405 (18.3) | 72/404 (17.8) | 0.5 (−4.9 to 5.8) | 1.02 (0.76 to 1.38) | 1.03 (0.77 to 1.38) | .83 |
| Post Hoc Sensitivity Analysis | ||||||
| Best case for acupunctureb | 84/415 (20.2) | 72/409 (17.6) | 2.6 (−2.7 to 8.0) | 1.15 (0.87 to 1.52) | 1.16 (0.87 to 1.53) | .31 |
| Worst case for acupuncturec | 74/415 (17.8) | 77/409 (18.8) | −1.0 (−6.3 to 4.3) | 0.95 (0.71 to 1.26) | 0.96 (0.72 to 1.27) | .75 |
| Post Hoc Exploratory Analyses | ||||||
| Live births among participants receiving an embryo transfer | 73/301 (24.3) | 72/307 (23.5) | 0.8 (−6.0 to 7.6) | 1.03 (0.78 to 1.37) | 1.04 (0.79 to 1.38) | .77 |
Adjusted analysis was performed using a log binary mixed model with the stratification variables (woman’s age and number of prior in vitro fertilization cycles) as fixed effects and study center as a random effect.
Assuming all unknown events in the acupuncture group were positive and those in the sham acupuncture group were negative.
Assuming none of the women with missing data in the acupuncture group became pregnant, and all of the women with missing data in the sham acupuncture group did become pregnant.
Secondary Outcomes
Prespecified
A clinical pregnancy was achieved in 105 of 408 women (25.7%) randomized to acupuncture and 88 of 406 women (21.7%) in the sham control (RD, 4.1 [95% CI, −1.8% to 9.9%]; RR, 1.19 [95% CI, 0.93 to 1.52]) (Table 3). The number of miscarriages among women receiving acupuncture was numerically higher than among women receiving sham control (22.8% vs 11.6%), but this difference was not statistically significant (RD, 11.1% [95% CI, 0.5%-21.8%]; RR, 1.96 [95% CI, 0.99 to 3.88]) (Table 3). Adverse events were reported by 152 women; these were minor and acupuncture specific (discomfort and bruising) and were statistically significantly greater in the acupuncture group for discomfort (10.3% vs 4.9%; RD, 5.4% [95% CI, 1.2% to 9.6%]; RR, 2.11 [95% CI, 1.16 to 3.82]) and bruising (5.0% vs 1.3%; RD, 3.7% [95% CI, 0.9% to 6.5%]; RR, 3.82 [95% CI, 1.28 to 11.39]).
Table 3. Prespecified Secondary Clinical Outcomes by Study Group.
| Prespecified Secondary Outcome | No./Total No. (%) | Risk Difference, % (95% CI) |
Relative Risk (95% CI) | P Valuea | |
|---|---|---|---|---|---|
| Acupuncture | Sham Acupuncture Control | ||||
| Clinical pregnancy among participants in the primary analysis cohort | 105/408 (25.7) | 88/406 (21.7) | 4.1 (−1.8 to 9.9) | 1.19 (0.93 to 1.52) | .17 |
| Post hoc sensitivity analysis | |||||
| Best case for acupunctureb | 112/415 (27.0) | 88/409 (21.5) | 5.5 (−0.3 to 11.3) | 1.25 (0.98 to 1.60) | .07 |
| Worst case for acupuncturec | 105/415 (25.3) | 91/409 (22.3) | 3.1 (−2.8 to 8.9) | 1.14 (0.89 to 1.45) | .30 |
| Post hoc exploratory analyses | |||||
| Clinical pregnancy among participants receiving an embryo transfer | 101/301 (33.6) | 86/307 (28.0) | 5.5 (−1.8 to 12.9) | 1.20 (0.94 to 1.52) | .14 |
| Miscarriage among clinical pregnancy | 23/101 (22.8) | 10/86 (11.6) | 11.1 (0.5 to 21.8) | 1.96 (0.99 to 3.88) | .054 |
| Women who reported any adverse event | 87/301 (28.9) | 65/307 (21.2) | 7.7 (0.9 to 14.6) | 1.37 (1.03 to 1.81) | .03 |
| Tiredness | 44/301 (14.6) | 36/307 (11.7) | 2.9 (−2.5 to 8.3) | 1.25 (0.83 to 1.88) | .29 |
| Discomfort on day of embryo transfer | 31/301 (10.3) | 15/307 (4.9) | 5.4 (1.2 to 9.6) | 2.11 (1.16 to 3.82) | .01 |
| Dizziness or drowsiness | 17/301 (5.7) | 14/307 (4.6) | 1.1 (−2.4 to 4.6) | 1.23 (0.62 to 2.47) | .67 |
| Pain | 15/301 (5.0) | 10/307 (3.3) | 1.7 (−1.4 to 4.9) | 1.53 (0.70 to 3.35) | .29 |
| Bruising | 15/301 (5.0) | 4/307 (1.3) | 3.7 (0.9 to 6.5) | 3.82 (1.28 to 11.39) | .02 |
| Nausea or vomiting | 8/301 (2.6) | 4/307 (1.3) | 1.4 (−0.9 to 3.6) | 2.04 (0.62 to 6.70) | .24 |
| Headaches | 7/301 (2.3) | 7/307 (2.3) | 0.1 (−2.3 to 2.4) | 1.02 (0.36 to 2.87) | .97 |
| Diarrhea | 4/301 (1.3) | 2/307 (0.7) | 0.7 (−0.9 to 2.3) | 2.04 (0.38 to 11.05) | .41 |
| Otherd | 6/301 (1.9) | 5/307 (1.6) | 0.4 (−1.8 to 2.5) | 1.22 (0.38 to 3.97) | .74 |
Testing for evidence of departure from relative risk = 1 using a Wald-type test.
Assuming all unknown events in the acupuncture group were positive and those in the sham acupuncture group were negative.
Assuming none of the women with missing data in the acupuncture group became pregnant, and all of the women with missing data in the sham acupuncture group did become pregnant.
Other includes sweating, skin irritation, or numbness.
Post Hoc Primary Outcomes
The best-case sensitivity analysis found no difference in live births between groups: 84 of 415 women (20.2%) receiving acupuncture and 72 of 409 (17.6%) in the sham control (RD, 2.6% [95% CI, −2.7% to 8.0%]; RR, 1.15 [95% CI, 0.87 to 1.52]) (Table 2). The worst-case sensitivity analysis found no difference in live births between groups: 74 of 415 women (17.8%) receiving acupuncture and 77 of 409 (18.8%) receiving sham (RD, −1.0% [95% CI, −6.3% to 4.3%]; RR, 0.95 [95% CI, 0.71 to 1.26]). A post hoc analysis of live births per participant receiving an embryo transfer found no difference between groups. No significant heterogeneity was present in the live birth rates between the 2 groups in the trial IVF sites (I2 = 0%; P = .45; eFigure 2 in Supplement 2).
Post Hoc Secondary Outcomes
The transfer of blastocyst or cleavage stage embryos differed significantly between groups, with a higher number of embryo transfers at a blastocyst stage for the sham control (31.3% in acupuncture, 39.4% in sham; RD, −8.0% [95% CI, −14.6% to −1.5%]; RR, 0.80 [95% CI, 0.66 to 0.96]) (eTable 2 in Supplement 2). There were no statistically significant differences between groups in reproductive and birth outcomes.
Exploratory Analysis
In a post hoc exploratory analysis, we examined the primary and secondary outcomes for 607 women undergoing embryo transfer only (eTable 3 in Supplement 2). We found no statistically significant difference in live births and clinical pregnancies between groups of women undergoing a cleavage or blastocyst transfer, 2 or more previous IVF cycles, undergoing IVF for the first time, with 1 previous IVF cycle, or 2 or more or 0 to 1 treatment sessions attended. Adherence to the intervention was high, with 557 women (91%) receiving 2 or more treatment sessions.
Treatment Blinding
A total of 180 women (43%) in the acupuncture group and 142 women (34%) in the sham control thought they received acupuncture, and 168 women (41%) in the sham acupuncture group correctly guessed their group allocation (eTable 4 in Supplement 2). The Bang blinding index suggested women were unblinded in the acupuncture group (0.18; P < .001) but not in the sham control group (0.064; P = .14). The significant unblinding in one group but not the other group is suggestive of an overall response bias.25 A small response bias was found following treatment, with participants believing they were more likely to have received an active treatment rather than a sham treatment (z = 2.086; P = .04), but this was not significant at 2 weeks following embryo transfer (z = 1.96; P = .057). The response bias index remained below the 2 absolute criteria indicating no response bias between the groups.
Discussion
In this randomized clinical trial involving women undergoing IVF, administration of acupuncture vs sham acupuncture around the time of ovarian stimulation and embryo transfer did not result in statistically significantly different live birth rates over 1 year. These findings, along with the finding of no statistically significant increase in clinical pregnancies, do not support the use of acupuncture to improve birth outcomes among women undergoing IVF.
Findings from this trial support a recent guideline from the American Society for Reproductive Medicine26 and 2 high-quality meta-analyses9,10 that found that acupuncture compared with a sham control performed around the time of ovarian stimulation and embryo transfer does not improve live birth rates in IVF. A similar finding of no increase in live births was reported from an RCT of 1000 Chinese women with polycystic ovary syndrome undergoing 4 cycles of ovulation induction following acupuncture.27 The safety of acupuncture as assessed by miscarriage is supported by the findings from the Cochrane systematic review10 and from studies examining outcomes from acupuncture when administered during pregnancy that find no evidence that acupuncture poses any risk to the mother or unborn fetus.28 Mild acupuncture-related adverse events were reported and differed between groups. The profile of these adverse events are similar to those reported in reviews assessing the safety of acupuncture in pregnancy and in the wider population.28,29 The adverse events may have contributed to the finding of partial unblinding.
The study addressed whether acupuncture was more efficacious than a placebo and specifically examined whether any effect was mediated through the point-specific needle insertion. To do this, a noninsertive needle was used. A recent meta-analysis examining placebo devices as effective control methods in acupuncture clinical trials30 found that these devices are not necessarily inert control interventions. These findings therefore may be explained by potential activity from the sham control. To determine whether any treatment effect in clinical outcomes arises from point-specific needle insertion or from other nonspecific effects, such as the placebo or time and attention from a therapist, would require the inclusion of a no-adjuvant treatment group in the trial design. A usual care–alone group was not included in the RCT due to findings from a previous pilot study8 that women would decline randomization to this design. Therefore, it remains unclear whether there are nonspecific effects from acupuncture or a sham control.
The main strengths of this study were its size, the multicenter design involving fertility units across Australia and New Zealand, and high rates of follow-up and adherence. The treatment protocol was based on best practice and was developed achieving consensus from expert clinicians; it also has broad generalizability to the practice of acupuncture. Blinding was intact in both groups, with the value of less than 2 indicative of unblinding due to a response bias not met by the acupuncture group.25
Limitations
This study has several limitations. First, the planned sample size was not achieved. Women increasingly accessed acupuncture in the community and declined randomization to the study. In response to the slow trial recruitment, the number of sites was increased to 16 IVF units to facilitate recruitment and the restrictive eligibility criteria reduced after 302 women were randomized. The 95% CI of the risk difference for live births excluded the minimal clinically important difference of 7%, suggesting the study was not underpowered. Second, the stage of embryo transfer was not balanced between groups, with a significantly higher number of women undergoing blastocyst transfer in the control group. This is a possible limitation due to blastocyst stage embryo transfer being associated with higher rates of pregnancy and live birth than cleavage stage transfers.31 No explanation for this observation was found and this could have occurred through chance.
Third, the length of the treatment intervention was short. However, earlier clinical trials in which acupuncture was administered only at the time of embryo transfer have reported improved live birth rates while using this short intervention.6,32 In clinical practice, acupuncture treatment is individualized with variation in the dosing characteristics of acupuncture, including more frequent treatment prior to and during the IVF cycle.18 Fourth, women were unavoidably excluded from the intention-to-treat analysis due to withdrawal of consent. In retrospect, tighter inclusion criteria and randomization closer to the onset of the stimulation cycle may have prevented study withdrawals. However, due to the small differences in outcomes, a full intention-to-treat analysis is unlikely to have changed the results. Fifth, multiple secondary outcomes were investigated without correction for multiple comparisons and these analyses should be interpreted as exploratory.
Conclusions
Among women undergoing IVF, administration of acupuncture vs sham acupuncture at the time of ovarian stimulation and embryo transfer resulted in no significant difference in live birth rates. These findings do not support the use of acupuncture to improve the rate of live births among women undergoing IVF.
Trial Protocol
eMethods. Protocol Treatment Interventions
eFigure 1. Location of Sham Ear Points
eFigure 2. Unadjusted Risk Difference of Live Birth by Study Site
eTable 1. Location of Sham Points for the Sham Acupuncture Control
eTable 2. Unadjusted Post-Hoc Secondary Study Outcomes by Study Group
eTable 3. Post Hoc Analyses of Selected Outcomes of Women Who Underwent an Embryo Transfer by Study Group
eTable 4. Assessment of Blinding Using the Bang Blinding Index
eReferences
References
- 1.Stankiewicz M, Smith C, Alvino H, Norman R. The use of complementary medicine and therapies by patients attending a reproductive medicine unit in South Australia: a prospective survey. Aust N Z J Obstet Gynaecol. 2007;47(2):145-149. [DOI] [PubMed] [Google Scholar]
- 2.Smith JF, Eisenberg ML, Millstein SG, et al. ; Infertility Outcomes Program Project Group . Fertility treatments and outcomes among couples seeking fertility care: data from a prospective fertility cohort in the United States. Fertil Steril. 2011;95(1):79-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coulson C, Jenkins J. Complementary and alternative medicine utilisation in NHS and private clinic settings: a United Kingdom survey of 400 infertility patients. J Exp Clin Assist Reprod. 2005;2(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bovey M, Lorenc A, Robinson N. Extent of acupuncture practice for infertility in the United Kingdom: experiences and perceptions of the practitioners. Fertil Steril. 2010;94(7):2569-2573. [DOI] [PubMed] [Google Scholar]
- 5.Smith CA, Armour M, Betts D. Treatment of women’s reproductive health conditions by Australian and New Zealand acupuncturists. Complement Ther Med. 2014;22(4):710-718. [DOI] [PubMed] [Google Scholar]
- 6.Paulus WE, Zhang M, Strehler E, El-Danasouri I, Sterzik K. Influence of acupuncture on the pregnancy rate in patients who undergo assisted reproduction therapy. Fertil Steril. 2002;77(4):721-724. [DOI] [PubMed] [Google Scholar]
- 7.Dieterle S, Ying G, Hatzmann W, Neuer A. Effect of acupuncture on the outcome of in vitro fertilization and intracytoplasmic sperm injection: a randomized, prospective, controlled clinical study. Fertil Steril. 2006;85(5):1347-1351. [DOI] [PubMed] [Google Scholar]
- 8.Smith C, Coyle M, Norman RJ. Influence of acupuncture stimulation on pregnancy rates for women undergoing embryo transfer. Fertil Steril. 2006;85(5):1352-1358. [DOI] [PubMed] [Google Scholar]
- 9.Manheimer E, van der Windt D, Cheng K, et al. The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: a systematic review and meta-analysis. Hum Reprod Update. 2013;19(6):696-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheong YC, Dix S, Hung Yu Ng E, Ledger WL, Farquhar C. Acupuncture and assisted reproductive technology. Cochrane Database Syst Rev. 2013;7(7):CD006920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andersen D, Løssl K, Nyboe Andersen A, et al. Acupuncture on the day of embryo transfer: a randomized controlled trial of 635 patients. Reprod Biomed Online. 2010;21(3):366-372. [DOI] [PubMed] [Google Scholar]
- 12.Dieterle S, Ying G, Hatzmann W, Neuer A. Effect of acupuncture on the outcome of in vitro fertilization and intracytoplasmic sperm injection: a randomized, prospective, controlled clinical study. Fertil Steril. 2006;85(5):1347-1351. [DOI] [PubMed] [Google Scholar]
- 13.Paulus WE, Zhang M, Strehler E, Seybold B, Sterzik K. Placebo-controlled trial of acupuncture effects in assisted reproduction therapy. Hum Reprod. 2003;18:18-19. [Google Scholar]
- 14.So EW, Ng EH, Wong YY, Lau EY, Yeung WS, Ho PC. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Hum Reprod. 2009;24(2):341-348. [DOI] [PubMed] [Google Scholar]
- 15.So EW, Ng EH, Wong YY, Yeung WS, Ho PC. Acupuncture for frozen-thawed embryo transfer cycles: a double-blind randomized controlled trial. Reprod Biomed Online. 2010;20(6):814-821. [DOI] [PubMed] [Google Scholar]
- 16.Smith CA, de Lacey S, Chapman M, et al. Acupuncture to improve live birth rates for women undergoing in vitro fertilization: a protocol for a randomized controlled trial. Trials. 2012;13(60):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31(1):103-115. [PubMed] [Google Scholar]
- 18.Smith CA, Grant S, Lyttleton J, Cochrane S. Using a Delphi consensus process to develop an acupuncture treatment protocol by consensus for women undergoing Assisted Reproductive Technology (ART) treatment. BMC Complement Altern Med. 2012;12:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct Med. 2002;20(4):168-174. [DOI] [PubMed] [Google Scholar]
- 20.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006;24(1):13-15. [DOI] [PubMed] [Google Scholar]
- 21.Pariente J, White P, Frackowiak RS, Lewith G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005;25(4):1161-1167. [DOI] [PubMed] [Google Scholar]
- 22.Deadman P, Al-Khafaji M, Baker K. A Manual of Acupuncture. East Sussex, England: Journal of Chinese Medicine Publications; 1998. [Google Scholar]
- 23.MacPherson H, Altman DG, Hammerschlag R, et al. ; STRICTA Revision Group . Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med. 2010;28(2):83-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris K, Fitzgerald O, Paul RC, Macaldowie A, Lee E, Chambers GM. Assisted Reproductive Technology in Australia and New Zealand 2014. Sydney, Australia: National Perinatal Epidemiology and Statistics Unit, University of New South Wales; 2016. [Google Scholar]
- 25.Bang H, Ni L, Davis CE. Assessment of blinding in clinical trials. Control Clin Trials. 2004;25(2):143-156. [DOI] [PubMed] [Google Scholar]
- 26.Practice Committee of the American Society for Reproductive Medicine. Electronic address: ASRM@asrm.org; Practice Committee of the American Society for Reproductive Medicine . Performing the embryo transfer: a guideline. Fertil Steril. 2017;107(4):882-896. [DOI] [PubMed] [Google Scholar]
- 27.Wu XK, Stener-Victorin E, Kuang HY, et al. ; PCOSAct Study Group . Effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome: a randomized clinical trial. JAMA. 2017;317(24):2502-2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park J, Sohn Y, White AR, Lee H. The safety of acupuncture during pregnancy: a systematic review. Acupunct Med. 2014;32(3):257-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16(2):91-97. [DOI] [PubMed] [Google Scholar]
- 30.Zhang CS, Tan HY, Zhang GS, Zhang AL, Xue CC, Xie YM. Placebo devices as effective control methods in acupuncture clinical trials: a systematic review. PLoS One. 2015;10(11):e0140825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2016;6(6):CD002118. [DOI] [PubMed] [Google Scholar]
- 32.Westergaard LG, Mao Q, Krogslund M, Sandrini S, Lenz S, Grinsted J. Acupuncture on the day of embryo transfer significantly improves the reproductive outcome in infertile women: a prospective, randomized trial. Fertil Steril. 2006;85(5):1341-1346. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Protocol Treatment Interventions
eFigure 1. Location of Sham Ear Points
eFigure 2. Unadjusted Risk Difference of Live Birth by Study Site
eTable 1. Location of Sham Points for the Sham Acupuncture Control
eTable 2. Unadjusted Post-Hoc Secondary Study Outcomes by Study Group
eTable 3. Post Hoc Analyses of Selected Outcomes of Women Who Underwent an Embryo Transfer by Study Group
eTable 4. Assessment of Blinding Using the Bang Blinding Index
eReferences