Abstract
This case series examines a noninvasive method of measuring and differentiating collateral and new vessels of the optic disc.
Collateral vessels and new vessels are 2 distinct processes that occur on the optic disc in retinal vascular disorders. Morphological differences between these 2 phenomena have been described previously using multiple imaging modalities.1,2,3 Studies using invasive methods have reported increased preretinal oxygen tension in eyes with new vessels.4 However, to our knowledge, noninvasive oximetry measurements of disc collateral vessels or new vessels have not been reported to-date. A noninvasive method of quantifying and differentiating these 2 processes will add value in understanding the mechanisms of the consequences of retinal vascular diseases. We hypothesized that blood in disc collateral vessels in venous occlusion should have a lower oxygen saturation compared with blood in disc new vessels given that collateral vessels develop to bypass an obstruction in the venous circulation unlike the development of new vessels, which is a proliferative process driven by hypoxia.5,6
Methods
To test this hypothesis, from January 1, 2016, to July 1, 2016, we retrospectively reviewed consecutive patients with a diagnosis of central retinal vein occlusion and proliferative diabetic retinopathy who had retinal oximetry measurements (Oxymap T1; Oxymap). Eyes with optic disc collateral vessels due to central retinal vein occlusion and eyes with disc new vessels due to proliferative diabetic retinopathy were identified. Collateral vessels and disc new vessels were confirmed by fluorescein angiography. Patients with poor-quality imaging were excluded. This study was approved by the Research Governance Committee of Moorfields Eye Hospital for the analysis of anonymized data, and written patient informed consent was obtained. The 35° disc-centered retinal oximetry measurements were used for analysis, and the minimum pixel tolerance was set at 6 pixels. The evaluated area was over the optic disc and excluded the central 50 μm. Oximetry measurements of disc collateral vessels and disc new vessels were recorded. Oximetry measurements were obtained by two of us (L.N. and C.S.), and the mean values were reported. An independent, unpaired, 2-tailed t test was used to compare means between the 2 groups. Intraclass correlation coefficient was used to assess intergrader agreement between the investigators. Statistical significance was set at 2-sided P = .05.
Results
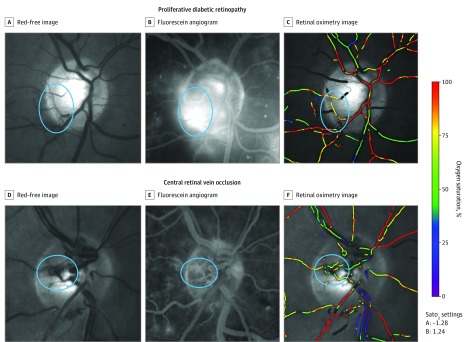
Three eyes with disc collateral vessels secondary to central retinal vein occlusion and 6 eyes with disc new vessels due to proliferative diabetic retinopathy were studied. Disc new vessels have a saturation of 83.14%, whereas disc collateral vessels have an average oxygen saturation of 66.92% (Figure). The difference between the 2 was 16.22% (95% CI, 4.14-28.30; P = .02). The intraclass correlation coefficient between the 2 graders was 0.899.
Figure. Oximetry of Disc New Vessels in Proliferative Diabetic Retinopathy and Disc Collateral Vessels in Central Retinal Vein Occlusion.
Red free (A), fluorescein angiography showing active leakage (B), and retinal oximetry imaging (C) of an eye with active proliferative diabetic retinopathy with disc new vessels. Red free (D), fluorescein angiography showing no leakage (E), and retinal oximetry imaging of an eye with central retinal vein occlusion and disc collateral vessels. The area of new vessels or disc collateral vessels is circled in all images. The panel on the right is the oxygen-saturation color bar. Sato2 indicates oxygen saturation.
Discussion
To our knowledge, this case series is the first report of noninvasive oximetry measurements of disc collateral vessels and new vessels in the literature. It is not surprising that the disc collateral vessels exhibit lower values because of their venous occlusion origin. However, disc new vessels appear to have significantly higher saturations. Diabetic microvascular changes predominantly occur on the venous end of capillaries, and earlier reports have highlighted that retinal neovascularization is nearly always of venous origin.6 The higher oxygen-saturation values of the new vessels in our study suggest that these new vessels either are of arterial origin or are venous but carry blood of higher oxygen saturation because of a direct shunt from the arteries. Limitations of this study include the small number of participants in our series and the comparison of new vessels in diabetic retinopathy with collateral vessels in retinal vein occlusion. This noninvasive clinical finding supports the notion that new vessels are rich in oxygen. This difference between collateral vessels and new vessels can be used to help differentiate the 2 in a clinical setting.
References
- 1.Singh A, Agarwal A, Mahajan S, et al. Morphological differences between optic disc collaterals and neovascularization on optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol. 2017;255(4):753-759. [DOI] [PubMed] [Google Scholar]
- 2.de Carlo TE, Bonini Filho MA, Baumal CR, et al. Evaluation of preretinal neovascularization in proliferative diabetic retinopathy using optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina. 2016;47(2):115-119. [DOI] [PubMed] [Google Scholar]
- 3.Muqit MMK, Stanga PE. Fourier-domain optical coherence tomography evaluation of retinal and optic nerve head neovascularisation in proliferative diabetic retinopathy. Br J Ophthalmol. 2014;98(1):65-72. [DOI] [PubMed] [Google Scholar]
- 4.Lange CAK, Stavrakas P, Luhmann UFO, et al. Intraocular oxygen distribution in advanced proliferative diabetic retinopathy. Am J Ophthalmol. 2011;152(3):406-412.e3. [DOI] [PubMed] [Google Scholar]
- 5.Henkind P, Wise GN. Retinal neovascularization, collaterals, and vascular shunts. Br J Ophthalmol. 1974;58(4):413-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patz A. Retinal neovascularisation: early contributions of Professor Michaelson and recent observations. Br J Ophthalmol. 1984;68(1):42-46. [DOI] [PMC free article] [PubMed] [Google Scholar]