Abstract
Injury of the ulnar collateral ligament (UCL) of thumb can be incapacitating if untreated or not treated properly. This injury is notorious for frequently being missed by inexperienced health care personnel in emergency departments. It has frequently been described in skiers, but also occurs in other sports such as rugby, soccer, handball, basketball, volleyball and even after a handshake. The UCL of the thumb acts as a primary restraint to valgus stress and is injured if hyperabduction and hyperextension forces are applied to the first metacarpophalangeal joint. The diagnosis is best established clinically, though MRI is the imaging modality of choice. Many treatment options exist, surgical treatment being offered depending on various factors, including timing of presentation (acute or chronic), grade (severity of injury), displacement (Stener lesion), location of tear (mid‐substance or peripheral), associated or concomitant surrounding tissue injury (bone, volar plate, etc.), and patient‐related factors (occupational demands, etc.). This review aims to identify the optimal diagnostic techniques and management options for UCL injury available thus far.
Keywords: Gamekeeper's thumb, Skier's thumb, Thumb injury, Ulnar collateral ligament
Introduction
Collateral ligament injuries have been noted in all digits of the hand, but occur more commonly in the ulnar and radial collateral ligaments of the thumb1. Campbell coined the term “Gamekeeper's thumb”2, having noticed this injury in gamekeepers who sustained chronic valgus strain injury of their thumbs when breaking rabbit necks. However, Gerber et al. popularized the term “skier's thumb” for the acute counterpart of this injury because it is prevalent among skiers3. Injury of the ulnar collateral ligament (UCL) of the thumb can be incapacitating if untreated or not treated properly. It is notorious for being frequently missed by inexperienced health care personnel in emergency departments3. Furthermore, there is no consensus on diagnosis and management of this injury. This review aims to determine the optimal diagnostic techniques and management options for UCL injury available thus far.
Anatomy
The metacarpophalangeal (MCP) joint is a diarthrodial joint, permitting predominantly flexion‐extension movements. The varus‐valgus laxity at this joint varies among normal thumbs and also with the arc of flexion‐extension. The collateral ligaments, UCL, and radial collateral ligament (RCL) (Fig. 1), provide stability against valgus and varus stress, respectively. The UCL, a proper collateral ligament, is the chief restraint to valgus stress during MCP joint flexion4 and an accessory collateral ligament5, which along with the volar plate serves as the primary valgus restraint during MCP joint extension. In addition to these static stabilizers of the MCP of thumb, restraint to valgus stress is imparted by extrinsic and intrinsic muscles that act as dynamic stabilizers. These extrinsic muscles include the extensor pollicis brevis, extensor pollicis longus, and flexor pollicis longus. The intrinsic muscles include the adductor pollicis, abductor pollicis brevis, and the flexor pollicis brevis.
Figure 1.
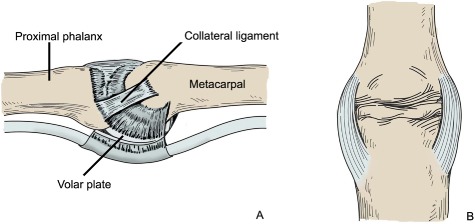
Diagrammatic representation of (A) lateral and (B) anteroposterior projections illustrating the ulnar collateral ligament attachments across the metacarpophalangeal joint.
Mechanism of Injury and Epidemiology
As mentioned in the anatomy section, the UCL is the primary restraint to valgus stress. Hyperabduction and hyperextension forces applied to the MCP joint are the usual causes of this stress. Such forces occur, for example, in a fall on an outstretched hand or when trying to grasp an object during a fall, leading to UCL tears. This injury has been noted most often in skiers2, but also occurs in other sports such as rugby, soccer, handball, basketball, volleyball, and even after a handshake6, 7, 8. A video analysis study found that most injuries sustained during skiing were associated with “jumping”, whereas thumb injuries were associated with “riding on rollers”9. First‐day participation and age less than 16 years have also been implicated as risk factors for injuries sustained in snow sports10. Furthermore, a cohort study noted sex differences in the incidence of hand/wrist/finger injuries in skiers, male subjects sustaining injuries more often than their female counterparts11. In another study UCL injury was most commonly associated with “falls”12.
Although UCL injury is more commonly seen than its counterpart, RCL injury13, problematic joint arthrosis, and laxity can occur in inadequately treated cases of traumatic rupture of the RCL14. Most UCL tears occur at the point of distal attachment to the proximal phalanx (distal avulsion). However, proximal avulsion, proximal and distal bony avulsion, isolated mid‐substance tears, and mid‐substance tears with bony avulsion do also occur15. Heim and Kratz described a rare variation of this injury wherein the extensor pollicis longus tendon gets interposed between the torn edges of UCL (instead of the usually seen adductor aponeurosis interposition)16.
Clinical Features
In acute cases there is history of trauma along with complaints of pain and difficulty in movement of the thumb. There may be associated bruising, swelling at the base of the thumb and rotational deformity17. In chronic cases there may be weakness of thumb‐index pinch grip and instability. Thumb‐index pinch weakness leads to marked limitation of basic activities of daily living18. As noted by Razza et al., “Pulling with pinch grips is an action frequently used in either occupational or daily living activities, especially in situations where the object is too small, the access to the object is restricted, the use of tools is prevented and in situations such as pulling strips out of long‐life packaging, removing seals from flask lids, tearing a plastic bag, etc”19. However, the position of the other fingers has a significant effect on the strength of this grip, for example when the other fingers are flexed; the thumb‐index pinch grip is maximal20. Instability or laxity of the thumb MCP joint is another feature associated with UCL injury. Such laxity or instability has frequently been used to assist diagnosis of UCL injury, as stated in the diagnosis section.
Diagnosis
Clinical Examination
In cases of acute injury, clinical examination reveals tenderness at the base of thumb. Furthermore, there may be bruising and swelling. Chronic cases usually show laxity/instability of the thumb MCP joint21. Patients usually complain of weakness of thumb‐index pinch grip22. Long term laxity of the MCP joint may eventually lead to premature arthritis23. Occasionally the torn UCL may displace proximally to lie superficial to the overlying adductor aponeurosis and present as a tender swelling at the base of thumb on the ulnar side (Stener lesion). Another reason for such a swelling is excessive granulation tissue formation at the site of ligament injury24. Historically, presence of the Stener lesion has been used as a deciding factor in offering surgical treatment. The question arises: Why is differentiating displaced from non‐displaced UCLs of paramount importance? As explained by Haramati et al., “Since the UCL is a capsular ligament, non‐displaced ligamentous rupture can often be treated conservatively, as is currently done in the treatment of medial collateral ligament tears in the knee. Therefore, the ability to distinguish between displaced and non‐displaced UCL tears is of great clinical importance”25.
Stress Test
Because abduction stress testing of the MCP joint of thumb to demonstrate its stability may be painful in cases of acute injury, use of local anesthesia is advocated26. After stabilizing the metacarpal, radial stress is applied to the proximal phalanx, both in 30° flexion and extension positions of the MCP, until a firm end point occurs. Complete UCL tears lack solid end point. Partial tears usually have a firm endpoint; the resultant metacarpal‐phalangeal angle can be measured and compared with that of the opposite side. A deviation of 35° on the affected side or a difference of 15° between the affected and opposite sides in flexion denotes a tear of the primary UCL and in extension a tear of the accessory part of the UCL.
X‐ray films
Anteroposterior and lateral X‐ray films of the thumb are taken to rule out any associated bony injuries. Associated bony avulsion fractures are seen in 20%–30% of UCL ruptures15. The position of an avulsed bony fragment usually indicates the position of the distal end of the UCL27. Indications for surgical treatment based on imaging include avulsion fractures with displacement of greater than 5 mm or any fracture involving 25% or more of the MCP joint surface28. Stress X‐ray films of the thumb MCP joint have also been used for diagnosis29, 30. However, there is concern that this maneuver can further damage the already injured UCL and create difficulties in interpretation of these films. Some authors consider the presence of bony avulsion a contraindication to valgus stress testing and hence recommend taking X‐rays prior to performing this maneuver for fear of displacement31, 32. Other authors argue that, in the case of associated undisplaced fractures, the injury force is always greater than the force applied during clinical testing, thus allaying any fear of displacement15, 33. A recent cadaver study concluded that correctly performed stress test examinations do not cause Stener lesions34. Thirkannad and Wolff described the “Two Fleck Sign”, wherein two bony fragments are present: one of them is usually obvious and denotes an undisplaced avulsion fracture whereas the other, which is frequently missed during initial X‐ray evaluation, denotes a Stener lesion27. These authors emphasize the “need to look for a second fragment of bone in every instance where an apparently undisplaced fracture is noted at the base of the proximal phalanx”. They believe that this second fragment probably indicates the whereabouts of the distal end of the ulnar collateral ligament and may identify Stener lesions. Gurdezi and Mokdescribed the “sag sign”, which is visible on lateral X‐ray films in cases of UCL tears and denotes a “volar subluxation of the proximal phalanx in relation to the metacarpal at the metacarpophalangeal joint”35. A recent study found that the presence of an exostosis at the metacarpal neck is a useful sign for differentiating chronic from acute UCL tears in the absence of a conclusive history and examination36.
Ultrasound
Ultrasound (US) is an excellent and cost‐effective modality for diagnosing UCL tears because it allows direct visualization of the entire UCL and surrounding structures. It locates the torn end of the UCL in almost 90% of cases37. A normal UCL shows an echolucent, convex‐shaped appearance extending from the metacarpal head to the base of proximal phalanx37. As described by Hergan et al., the sonographic picture in cases of undisplaced UCL tears shows a “normal‐positioned UCL surrounded by inhomogeneous or echolucent areas due to hematoma, effusion, and edema. In the displaced type, the UCL cannot be seen in its normal position. Usually, an ill‐defined echolucent area close to the head/neck of the first metacarpal bone represents the displaced UCL”37. Identification of a tadpole image during US suggests a displaced UCL, which requires surgical management38. Based on subsequent surgical findings, US reportedly has 94% positive predictive value (80%), sensitivity of 83%, and specificity of 75%39. These authors reported that US performed soon after presentation is a valuable adjunct to clinical examination in differentiating displaced from non‐displaced UCL tears. Another study by Schnur et al. found a positive predictive value of 87.5% for US diagnosis of UCL injury in patients who underwent surgical exploration32. Measuring on US, Koslowsky et al. found a difference of 2.25 ± 0.46 mm between normal and injury groups in the distance between the innominate tubercle of the first metacarpal and the base of the proximal phalanx of the MCP joint and opined that this may be sufficient to diagnose a UCL tear without direct observation of the UCL40. However, Susic et al. reported that US is inadequate for identifying dislocated UCL tears and advised exploration in cases with clinical instability41. A recent retrospective review found that non‐visualization of UCL fibers and presence of a heterogeneous mass proximal to MCP joint on ultrasound were 100% accurate in differentiating displaced from non‐displaced full‐thickness UCL tears42. The advantages of US are that it is dynamic, safe, and quick and can be readily performed in the emergency department43. Its drawbacks include patient discomfort in acute cases35 and difficulty in locating the torn UCL when it is thin or in cases more than one week old where scar tissue or ligament shrinkage pose difficulties37. Furthermore it requires an experienced sonographer with sound knowledge of hand anatomy and pathology32.
MRI
MRI is considered by some as the best modality for evaluating UCL injuries44. Like US, MRI allows direct visualization of the UCL and surrounding structures and is safe and non‐invasive; however, it is more costly and less readily available. One study reported that MRI has a sensitivity of 96% and specificity of 95% in diagnosing UCL tears45. Modern MR scanners and appropriate MR coils are now available for evaluating small structures such as the UCL46. The MRI findings of normal and torn UCLs as described by Lohman et al.44 are shown in Table 1. The authors also noted that MRI coronal sequences are optimal for viewing the UCL; however, differentiating Stener from non‐Stener lesions is not always possible by MRI in chronic UCL rupture with excessive scarring. Stener lesions typically have a “yo‐yo on a string” appearance47. MRI has been recommended for assessing graft integrity in cases of suspected post‐operative graft failure48.
Table 1.
MRI findings of normal and torn UCLs
| UCL | MRI findings |
|---|---|
| Normal | Situated immediately adjacent to the ulnar side of the metacarpophalangeal joint, smooth, homogeneous, hypointense structure extending from the distal metacarpal to proximal phalanx |
| Acute rupture | Gap easily identifiable, edema around the ligament and at the rupture site |
| Chronic rupture | Scarring looks like an irregular area of decreased signal intensity, gap between the torn ends not easily identifiable |
Arthrography
Arthrography involves distension of the MCP joint by injecting contrast material and then visualizing the joint by X‐ray or MRI (MR‐arthrography). UCL injuries are diagnosed by direct visualization of any focal defect or by extravasation of contrast from the joint, suggesting rents in the ligaments46. Another indirect finding on arthrography suggestive of UCL tear is demonstration of the heads of the adductor pollicis muscle49.
The various modalities used for diagnosis of UCL injury are presented in Table 2.
Table 2.
Various modalities for diagnosing UCL injury
| Modality | Advantages | Drawbacks |
|---|---|---|
| Plain X‐ray films | Cheap, readily available, can rule out bony injury | Inability to visualize the UCL, differentiate displaced from non‐displaced UCLs or grade the injury |
| Stress X‐ray films | In evaluating joint stability, can diagnose partial tears (see text) | Uncomfortable for patient (may require local anesthesia), inherent risk of increased displacement (controversial), unable to differentiate between displaced and non‐displaced UCLs |
| US | Simple, non‐invasive, cost‐effective(compared with MRI), direct visualization of UCL, less time‐consuming than MRI | Somewhat uncomfortable (requires some stress to be applied to the UCL), requires experienced sonographer and optimal hardware |
| MRI | Non‐invasive, direct visualization of UCL and surrounding structures, ability to differentiate displaced from non‐displaced tears as well as grading(severity), aids in planning and selecting surgical approach, high sensitivity and specificity | Cost, availability, motion artifact (apprehensive patients with acute injury) |
| Arthrography | Direct visualization (by joint distension), indirect visualization (by extravasation of contrast) | Time consuming, contrast complications, invasive, does not assess surrounding structures (unlike MRI), difficulty in interpretation of results |
Management
Injuries of the UCL can be managed conservatively or surgically, depending on various factors that primarily include: (i) timing of presentation (acute or chronic); (ii) grade (severity of injury); (iii) displacement (Stener lesion); (iv) location of tear (mid‐substance or peripheral); (v) associated or concomitant surrounding tissue injury (bone, volar plate, etc.); and (vi) patient related factors (occupational demands, etc.)
Conservative Management
The indications for conservative management include partial, non‐displaced UCL tears presenting early. Associated fractures, if undisplaced, can also be managed conservatively. Non‐operative treatment typically includes immobilization for 4–6 weeks in plaster or a splint. The thumb should be immobilized in a position of mild flexion and slight ulnar deviation at the MCP joint. The interphalangeal joint is usually kept free to allow movement. Physiotherapy is started as soon as the immobilization has been removed, starting with range of motion exercises followed by grip strengthening exercises. Compared to a standard thumb spica plaster cast, a splint allows some movement, such as flexion and extension, while simultaneously restricting abduction. A randomized controlled trial comparing plaster with splints in subjects with UCL tears found both modalities to be equally effective with regard to outcome measures like “stability, range of motion, strength of the injured thumb and length of sick leave”50. However, patients favored splint over plaster because of the former's superior comfort. In addition to standard thumb spica casts, a variety of other casts and splints for this injury have been described. These include glove spica casts51, modified thumb spica casts52, hinged MCP joint splints53 and modified thumb spica splints54. McCue et al. use a taping method whereby they first immobilize the thumb MCP using a tape and then include the index finger to prevent abduction of the thumb24. One laboratory study cautioned that excessive strain on the UCL could be avoided by not immobilizing the MCP joint in excessive flexion or starting unrestricted early mobilization55. There is no consensus regarding the optimal treatment for UCL tears associated with avulsion fractures. Both operative and conservative treatments have been advocated56, 57. Complete UCL tears are usually associated with gross instability and traditionally have been managed surgically; however, some authors have reported encouraging results with non‐operative treatment58. In the presence of bony avulsion, we treat acute UCL injuries surgically only if they are unstable on stress testing and if there is any radiological evidence of displacement. Even minimal displacement has been associated with rotational deformity56.
Surgical Management
Surgery is usually required for injuries of the thumb UCL characterized by: (i) Stener lesions; (ii) displaced unstable bony avulsion; (iii) chronicity; (iv) acute tears with gross instability; and (v) associated volar plate injury. Surgical options include repair (early or late), reconstruction, arthrodesis, and arthroplasty.
Repair
The UCL is frequently avulsed from its distal attachment. Historically, securing it to its normal anatomical position at the base of proximal phalanx has been performed using wire or suture pull out techniques through a bone tunnel. The non‐absorbable sutures are passed through this tunnel and then tied to the bone tunnel or over a button on the radial side. Another option is to directly suture the UCL to the periosteal tissue of the proximal phalangeal base, provided secure fixation is possible. Suture anchors as a repair fixation modality have become popular because they obviate the need for drilling a bone tunnel or exposing the suture material as required in suture/wire pull‐out techniques59. A variety of suture anchors are commercially available. Both the primary and accessory parts of the UCL are repaired, followed by repair of the volar plate and dorsal capsule if required. For mid‐substance tears direct repair using absorbable33 or non‐absorbable sutures60 has been advocated. Some authors prefer additional repair stability in the form of k‐wire passed across the MCP joint21. Haddock et al. described a new technique for repair of chronic UCL tears involving condylar shaving on the ulnar side of metacarpal and proximal phalanx along with double breasting of the UCL61.
Reconstruction
Reconstruction of the UCL is usually performed in cases of failed primary repair or late presentation where the torn ligament ends are not identifiable or have shrunk, thus preventing a late repair. Prior radiological assessment of the MCP joint is important to identify any degenerative changes which, if present, will make the reconstruction futile. Reconstruction can be performed using a local graft or a free graft from a distant site. It can be dynamic (using a local musculotendinous unit) or static (using a local or free graft). Materials which have been used as graft materials for either dynamic or static reconstruction of the UCL include the palmaris longus62, adductor pollicis63, extensor pollicis brevis23, 64, bone periosteum flap65 and bone periosteum bone (BPB) graft66. For static reconstruction, grafts have been used in various configurations. Arthroscopic reduction and internal fixation of UCL tears with bony avulsion has also been advocated. The procedure allows for derotation of the displaced avulsed bone fragment and anatomic restoration of the UCL. Two small cases series have reported acceptable results with this technique67, 68. As noted by Badia, the advantages of an arthroscopic technique over open repair include faster rehabilitation, shorter surgical and tourniquet times, better cosmesis, and decreased postoperative inflammatory responses67. Injury to the superficial branch of radial nerve during portal placement is a potential risk69.
Post‐operative care after repair or reconstruction includes immobilization using a plaster cast or splint, depending on the physician's choice. However, removable functional splints provide for easy post‐operative wound care. Immobilization is continued for 4–6 weeks and followed by staged range of motion exercises and grip strengthening exercises. Complications of surgery include neuropraxia (sensory branch of the radial nerve), stiffness, persistent pain, persistent weakness of grip, and cold intolerance. A recent study noted specific activities that may be affected, including opening jars, lifting weights in the gym, riding a motorcycle and using a tennis or badminton racket12. Functional outcomes that should be assessed include tip, tripod, and key pinch strength as measured by pinch gauge; power grip as measured by dynamometer; stability of MCP joint as measured by metacarpal‐phalangeal angle during stress testing; and range of motion as measured by goniometer. The ultimate aim of successful treatment is improvement in quality of life (no persistent pain, instability, weakness of pinch strength, stiffness or arthritis). Many validated scales/instruments are available for assessing functional outcomes after treatment. They include DASH (Disabilities of the Arm, Shoulder and Hand) and Quick DASH70, Buck–Gramko71, Kapandji index72 and Michigan hand outcome score73.
Arthrodesis/Arthroplasty
Untreated or inadequately treated UCL injuries with persistent laxity usually develop progressive premature arthritis23 with or without chronic volar subluxation. As mentioned earlier, in this situation with persistent pain and limitation of joint movement, repair, and reconstruction are not helpful. Hence some authors have advocated arthrodesis6, 24, 63 or arthroplasty60, 74. In a recent study of subjective outcomes after arthrodesis of the MCP joint, the authors concluded that arthrodesis is best reserved for elderly patients with painless instability75.
Conclusions
Tears of the UCL of the thumb are small but incapacitating injuries. Inexperienced clinicians can easily miss them and inadequate or delayed treatment can result in chronic disability. The diagnosis is best established clinically; however, MRI is the imaging modality of choice. Many treatment options exist, surgical treatment being offered depending on various factors, including severity of injury and chronicity. The best treatment option is still not clear and requires further research.
Disclosure: There are no conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject of the manuscript.
References
- 1. Musharafieh RS, Bassim YR, Atiyeh BS. Ulnar collateral ligament rupture of the first metacarpophalangeal joint: a frequently missed injury in the emergency department. J Emerg Med, 1997, 15: 193–196. [DOI] [PubMed] [Google Scholar]
- 2. Campbell CS. Gamekeeper's thumb. J Bone Joint Surg Br, 1955, 37: 148–149. [DOI] [PubMed] [Google Scholar]
- 3. Gerber C, Senn E, Matter P. Skier's thumb. Surgical treatment of recent injuries to the ulnar collateral ligament of the thumb's metacarpophalangeal joint. Am J Sports Med, 1981, 9: 171–177. [DOI] [PubMed] [Google Scholar]
- 4. Heyman P, Gelberman RH, Duncan K, Hipp JA. Injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Biomechanical and prospective clinical studies on the usefulness of valgus stress testing. Clin Orthop Relat Res, 1993, 292: 165–171. [PubMed] [Google Scholar]
- 5. Minami A, An KN, Cooney WP 3rd, Linscheid RL, Chao EY. Ligamentous structures of the metacarpophalangeal joint: a quantitative anatomic study. J Orthop Res, 1984, 1: 361–368. [DOI] [PubMed] [Google Scholar]
- 6. Rettig AC. Athletic injuries of the wrist and hand part ii: overuse injuries of the wrist and traumatic injuries to the hand. Am J Sports Med, 2004, 32: 262–273. [DOI] [PubMed] [Google Scholar]
- 7. Moutet F, Guinard D, Lebrun C, Bello‐Champel P, Massart P. Metacarpophalangeal thumb sprains based on experience with more than 1000 cases. Ann Hand Surg, 1989, 8: 99–109. [DOI] [PubMed] [Google Scholar]
- 8. Dey R, Green AD. The danger in a handshake‐an unusual case of ulnar collateral ligament rupture injury. Injury, 2003, 34: 535–536. [DOI] [PubMed] [Google Scholar]
- 9. Bakken A, Bere T, Bahr R, Kristianslund E, Nordsletten L. Mechanisms of injuries in world cup snowboard cross: a systematic video analysis of 19 cases. Br J Sports Med, 2011, 45: 1315–1322. [DOI] [PubMed] [Google Scholar]
- 10. Langran M, Selvaraj S. Snow sports injuries in Scotland: a case‐control study. Br J Sports Med, 2002, 36: 135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Westin M, Alricsson M, Werner S. Injury profile of competitive alpine skiers: a five‐year cohort study. Knee Surg Sports Traumatol Arthrosc, 2012, 20: 1175–1181. [DOI] [PubMed] [Google Scholar]
- 12. Venus MR, Chester DL. Outcomes in repair of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Eur J Plast Surg, 2012, 35: 735–740. [Google Scholar]
- 13. Horch RE, Dragu A, Polykandriotis E, Kneser U. Radial collateral ligament repair of the thumb metacarpophalangeal joint using the abductor pollicis brevis tendon. Plast Reconstr Surg, 2006, 117: 491–496. [DOI] [PubMed] [Google Scholar]
- 14. Doty JF, Rudd JN, Jemison M. Radial collateral ligament injury of the thumb with a Stener‐like lesion. Orthopedics, 2010, 33: 925. [DOI] [PubMed] [Google Scholar]
- 15. Hintermann B, Holzach PJ, Schutz M, Matter P. Skier's thumb‐the significance of bony injuries. Am J Sports Med, 1993, 21: 800–804. [DOI] [PubMed] [Google Scholar]
- 16. Heim D, Kratz M. The skier's thumb: ulnar displacement of the extensor pollicis longus tendon–a new type? Eur J Trauma, 2001, 27: 340–344. [Google Scholar]
- 17. Theumann NH, Pessis E, Lecompte M, et al MR imaging of the metacarpophalangeal joints of the fingers: evaluation of 38 patients with chronic joint disability. Skeletal Radiol, 2005, 34: 210–216. [DOI] [PubMed] [Google Scholar]
- 18. Rajkumar P, Premkumar R, Richard J. Grip and pinch strength in relation to function in denervated hands. Indian J Lepr, 2002, 74: 319–328. [PubMed] [Google Scholar]
- 19. Razza BM, Paschoarelli LC, Silva DC. Pulling strength with pinch grips: a variable for product design In: Salvendy G, Soares MM, Rebelo F, Karwowski V, eds. Advances in Usability Evaluation Part 1. Boca Raton, FL, USA: CRC Press, 2012; 428–437. [Google Scholar]
- 20. Hook WE, Stanley JK. Assessment of thumb to index pulp to pulp pinch grip strengths. J Hand Surg Br, 1986, 11: 91–92. [DOI] [PubMed] [Google Scholar]
- 21. Baskies MA, Lee SK. Evaluation and treatment of injuries of the ulnar collateral ligament of the thumb metacarpophalangeal joint. Bull NYU Hosp Jt Dis, 2009, 67: 68. [PubMed] [Google Scholar]
- 22. Samora JB, Harris JD, Griesser MJ, Ruff ME, Awan HM. Outcomes after injury to the thumb ulnar collateral ligament‐a systematic review. Clin J Sport Med, 2013, 23: 247–254. [DOI] [PubMed] [Google Scholar]
- 23. Sakellarides HT, DeWeese JW. Instability of the metacarpophalangeal joint of the thumb. Reconstruction of the collateral ligaments using the extensor pollicis brevis tendon. J Bone Joint Surg Am, 1976, 58: 106–112. [PubMed] [Google Scholar]
- 24. McCue FC 3rd, Hakala MW, Andrews JR, Gieck JH. Ulnar collateral ligament injuries of the thumb in athletes. Am J Sports Med, 1974, 2: 70–80. [DOI] [PubMed] [Google Scholar]
- 25. Haramati N, Hiller N, Dowdle J, et al MRI of the Stener lesion. Skeletal Radiol, 1995, 24: 515–518. [DOI] [PubMed] [Google Scholar]
- 26. Heyman P. Injuries to the ulnar collateral ligament of the thumb metacarpophalangeal joint. J Am Acad Orthop Surg, 1997, 5: 224–229. [DOI] [PubMed] [Google Scholar]
- 27. Thirkannad S, Wolff TW. The “two fleck sign” for an occult Stener lesion. J Hand Surg Eur Vol, 2008, 33: 208–211. [DOI] [PubMed] [Google Scholar]
- 28. Richard JR. Gamekeeper's thumb: ulnar collateral ligament injury. Am Fam Physician, 1996, 53: 1775. [PubMed] [Google Scholar]
- 29. Louis DS, Huebner JJ Jr, Hankin FM. Rupture and displacement of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. Preoperative diagnosis. J Bone Joint Surg Am, 1986, 68: 1320–1326. [PubMed] [Google Scholar]
- 30. Abrahamsson SO, Sollerman C, Lundborg G, Larsson J, Egund N. Diagnosis of displaced ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Hand Surg Am, 1990, 15: 457–460. [DOI] [PubMed] [Google Scholar]
- 31. Anderson D. Skier's thumb. Aust Fam Physician, 2010, 39: 575–577. [PubMed] [Google Scholar]
- 32. Schnur DP, DeLone FX, McClellan RM, Bonavita J, Witham RS. Ultrasound: a powerful tool in the diagnosis of ulnar collateral ligament injuries of the thumb. Ann Plast Surg, 2002, 49: 19–23. [DOI] [PubMed] [Google Scholar]
- 33. Tsiouri C, Hayton MJ, Baratz M. Injury to the ulnar collateral ligament of the thumb. Hand, 2009, 4: 12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Adler T, Eisenbarth I, Hirschmann MT, Müller Gerbl M, Fricker R. Can clinical examination cause a Stener lesion in patients with skier's thumb? A cadaveric study. Clin Anat, 2012, 25: 762–766. [DOI] [PubMed] [Google Scholar]
- 35. Gurdezi S, Mok D. “SAG SIGN”—a simple radiological sign for detecting injury to the thumb ulnar collateral ligament. J Bone Joint Surg Br, 2010, 92 (Suppl. II): S352. [Google Scholar]
- 36. Hunter AR, Tansey RJ, Muir LT. A radiological sign in chronic collateral ligament injuries of the thumb metacarpophalangeal joint. Hand, 2013, 8: 191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hergan K, Mittler C, Oser W. Pitfalls in sonography of the Gamekeeper's thumb. Eur Radiol, 1997, 7: 65–69. [DOI] [PubMed] [Google Scholar]
- 38. Heim D. The skier's thumb. Acta Orthop Belg, 1999, 65: 440–446. [PubMed] [Google Scholar]
- 39. Jones MH, England SJ, Muwanga CL, Hildreth T. The use of ultrasound in the diagnosis of injuries of the ulnar collateral ligament of the thumb. J Hand Surg Br, 2000, 25: 29–32. [DOI] [PubMed] [Google Scholar]
- 40. Koslowsky TC, Mader K, Gausepohl T, Heidemann J, Pennig D, Koebke J. Ultrasonographic stress test of the metacarpophalangeal joint of the thumb. Clin Orthop Relat Res, 2004, 427: 115–119. [DOI] [PubMed] [Google Scholar]
- 41. Susic D, Hansen BR, Hansen TB. Ultrasonography may be misleading in the diagnosis of ruptured and dislocated ulnar collateral ligaments of the thumb. Scand J Plast Reconstr Surg Hand Surg Suppl, 1999, 33: 319–320. [DOI] [PubMed] [Google Scholar]
- 42. Melville D, Jacobson JA, Haase S, Brandon C, Brigido MK, Fessell D. Ultrasound of displaced ulnar collateral ligament tears of the thumb: the Stener lesion revisited. Skeletal Radiol, 2013, 42: 667–673. [DOI] [PubMed] [Google Scholar]
- 43. Ebrahim FS, De Maeseneer M, Jager T, Marcelis S, Jamadar DA, Jacobson JA. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern‐based approach, and differential diagnosis. Radiographics, 2006, 26: 1007–1020. [DOI] [PubMed] [Google Scholar]
- 44. Lohman M, Vasenius J, Kivisaari A, Kivisaari L. MR imaging in chronic rupture of the ulnar collateral ligament of the thumb. Acta Radiol, 2001, 42: 10–14. [PubMed] [Google Scholar]
- 45. Plancher KD, Ho CP, Cofield SS. Role of MR imaging in the management of “skier's thumb” injuries. Magn Reson Imaging Clin N Am, 1999, 7: 73–84. [PubMed] [Google Scholar]
- 46. Peterson JJ, Bancroft LW, Kransdorf MJ, Berquist TH, Magee TH, Murray PM. Evaluation of collateral ligament injuries of the metacarpophalangeal joints with magnetic resonance imaging and magnetic resonance arthrography. Curr Probl Diagn Radiol, 2007, 36: 11–20. [DOI] [PubMed] [Google Scholar]
- 47. Harper MT, Chandnani VP, Spaeth J, Santangelo JR, Providence BC, Bagg MA. Gamekeeper thumb: diagnosis of ulnar collateral ligament injury using magnetic resonance imaging, magnetic resonance arthrography and stress radiography. J Magn Reson Imaging, 1996, 6: 322–328. [DOI] [PubMed] [Google Scholar]
- 48. Lohman M, Vasenius J, Nieminen O, Kivisaari L. MRI follow‐up after free tendon graft reconstruction of the thumb ulnar collateral ligament. Skeletal Radiol, 2010, 39: 1081–1086. [DOI] [PubMed] [Google Scholar]
- 49. Ganel A, Aharonson Z, Engel J. “Gamekeeper's thumb”. Injuries of the ulnar collateral ligament of the metacarpophalangeal joint. Br J Sports Med, 1980, 14: 92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sollerman C, Abrahamsson SO, Lundborg G, Adalbert K. Functional splinting versus plaster cast for ruptures of the ulnar collateral ligament of the thumb: a prospective randomized study of 63 cases. Acta Orthop Scand, 1991, 62: 524–526. [DOI] [PubMed] [Google Scholar]
- 51. Campbell JD, Feagin JA, Lambert KL, Cunningham R. Ulnar collateral ligament injury of the thumb Treatment with glove spica cast. Am J Sports Med, 1992, 20: 29–30. [DOI] [PubMed] [Google Scholar]
- 52. Primiano GA. Functional cast immobilization of thumb metacarpophalangeal joint injuries. Am J Sports Med, 1986, 14: 335–339. [DOI] [PubMed] [Google Scholar]
- 53. Michaud EJ, Flinn S, Seitz WH Jr. Treatment of grade III thumb metacarpophalangeal ulnar collateral ligament injuries with early controlled motion using a hinged splint. J Hand Ther, 2010, 23: 77–82. [DOI] [PubMed] [Google Scholar]
- 54. Hart RG, Kleinert HE, Lyons KA. Modified thumb spica splint for thumb injuries in the ED. Am J Emerg Med, 2005, 23: 777–781. [DOI] [PubMed] [Google Scholar]
- 55. Adams BD, Muller DL. Assessment of thumb positioning in the treatment of ulnar collateral ligament injuries. Am J Sports Med, 1996, 24: 672–675. [DOI] [PubMed] [Google Scholar]
- 56. Dinowitz M, Trumble T, Hanel D, Vedder NB, Gilbert M. Failure of cast immobilization for thumb ulnar collateral ligament avulsion fractures. J Hand Surg Am, 1997, 22: 1057–1063. [DOI] [PubMed] [Google Scholar]
- 57. Sorene ED, Goodwin DR. Non‐operative treatment of displaced avulsion fractures of the ulnar base of the proximal phalanx of the thumb. Scand J Plast Reconstr Surg Hand Surg, 2003, 37: 225–227. [DOI] [PubMed] [Google Scholar]
- 58. Landsman JC, Seitz WH Jr, Froimson AI, Leb RB, Bachner EJ. Splint immobilization of gamekeeper's thumb. Orthopedics, 1995, 18: 1161–1165. [DOI] [PubMed] [Google Scholar]
- 59. Huber J, Bickert B, Germann G. The Mitek mini anchor in the treatment of the gamekeeper's thumb. Eur J Plast Surg, 1997, 20: 251–255. [Google Scholar]
- 60. Patel S, Potty A, Taylor EJ, Sorene ED. Collateral ligament injuries of the metacarpophalangeal joint of the thumb: a treatment algorithm. Strategies Trauma Limb Reconstr, 2010, 5: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Haddock NT, Beasley RW, Sharma S. Thumb metacarpophalangeal joint ulnar collateral ligament repair with condylar shaving. Tech Hand Up Extrem Surg, 2009, 13: 199–201. [DOI] [PubMed] [Google Scholar]
- 62. Glickel SZ, Malerich M, Pearce SM, Littler JW. Ligament replacement for chronic instability of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. J Hand Surg Am, 1993, 18: 930–941. [DOI] [PubMed] [Google Scholar]
- 63. Neviaser RJ, Wilson JN, Lievano A. Rupture of the ulnar collateral ligament of the thumb (gamekeeper's thumb). Correction by dynamic repair. J Bone Joint Surg Am, 1971, 53: 1357–1364. [PubMed] [Google Scholar]
- 64. Fairhurst M, Hansen L. Treatment of “Gamekeeper's Thumb” by reconstruction of the ulnar collateral ligament. J Hand Surg Br, 2002, 27: 542–545. [DOI] [PubMed] [Google Scholar]
- 65. Strandell G. Total rupture of the ulnar collateral ligament of the metacarpophalangeal joint of the thumb. Results of surgery in 35 cases. Acta Chir Scand, 1959, 118: 72–80. [PubMed] [Google Scholar]
- 66. Wong TC, Ip FK, Wu WC. Bone‐periosteum‐bone graft reconstruction for chronic ulnar instability of the metacarpophalangeal joint of the thumb–minimum 5‐year follow‐up evaluation. J Hand Surg Am, 2009, 34: 304–308. [DOI] [PubMed] [Google Scholar]
- 67. Badia A. Arthroscopic reduction and internal fixation of bony gamekeeper's thumb. Orthopedics, 2006, 29: 675–678. [DOI] [PubMed] [Google Scholar]
- 68. Ryu J, Fagan R. Arthroscopic treatment of acute complete thumb metacarpophalangeal ulnar collateral ligament tears. J Hand Surg Am, 1995, 20: 1037–1042. [DOI] [PubMed] [Google Scholar]
- 69. Ropars M, Fontaine I, Morandi X, Berton E, Kaila R, Darnault P. Preserving the superficial branch of the radial nerve during carpometacarpal and metacarpophalangeal joint arthroscopy: an anatomical study. Surg Radiol Anat, 2010, 32: 271–276. [DOI] [PubMed] [Google Scholar]
- 70. The DASH outcome measure: disabilities of the arm, shoulder and hand. Available from: http://www.dash.iwh.on.ca/home (accessed December 2013).
- 71. Traumascores. Available from: http://www.traumascores.com/index.php/scores2/27‐handgelenk‐und‐hand/65‐64 (accessed December 2013) (In German).
- 72. Lefevre‐Colau MM, Poiraudeau S, Oberlin C, et al Reliability, validity, and responsiveness of the modified Kapandji index for assessment of functional mobility of the rheumatoid hand. Arch Phys Med Rehabil, 2003, 84: 1032–1038. [DOI] [PubMed] [Google Scholar]
- 73. Michigan Hand Outcome Questionnaire. Available from: http://www.orthopaedicscore.com/scorepages/Michigan_Hand_Outcome_Questionnaire.html (accessed December 2103).
- 74. Wood MB, Dobyns JH. Chronic, complex volar dislocation of the metacarpophalangeal joint. J Hand Surg Am, 1981, 6: 73–76. [DOI] [PubMed] [Google Scholar]
- 75. Rigó IZ, Røkkum M. Not all non‐rheumatoid patients are satisfied with thumb metacarpophalangeal joint arthrodesis. J Plast Surg Hand Surg, 2013, 47: 144–146. [DOI] [PubMed] [Google Scholar]


