Key Points
Question
Does prolonged and exclusive breastfeeding reduce the risk of asthma and atopic eczema and improve lung function in adolescence?
Findings
In this adolescent follow-up of a cluster randomized trial in Belarus, which assessed the effect of a breastfeeding promotion intervention vs usual care among 13 557 participants, there was a 54% reduction in atopic eczema on skin examination but no significant effect on lung function (spirometry) and self-reported asthma diagnosis and symptoms of atopic eczema and wheezing in the past year.
Meaning
Promotion of prolonged and exclusive breastfeeding may reduce the risk of atopic eczema risk in adolescence.
Abstract
Importance
Atopic diseases, including asthma and atopic eczema, are the most common chronic conditions of childhood.
Objective
To investigate whether an intervention to promote prolonged and exclusive breastfeeding protects against asthma, atopic eczema, and low lung function in adolescence.
Design, Setting, and Participants
Follow-up of the Promotion of Breastfeeding Intervention Trial (PROBIT), a cluster randomized trial in 30 Belarusian maternity hospitals and affiliated polyclinics; recruitment of 17 046 healthy term infants took place from June 15, 1996, to December 31, 1997. Data analysis was conducted from May 9, 2016, to April 21, 2017. The primary analytic approach was by modified intention-to-treat analysis.
Interventions
Randomization to receive a breastfeeding promotion intervention vs usual care.
Main Outcomes and Measures
Spirometry and flexural eczema on standardized skin examination by study pediatricians were the primary outcomes; secondary outcomes were self-reported asthma diagnosis ever, and wheezing and flexural eczema symptoms in the previous year.
Results
A total of 13 557 (79.5%) participants were followed up from September 15, 2012 to July 15, 2015. The intervention (7064 [79.7%]) and control (6493 [79.4%]) groups were similar at follow-up (3590 [50.8%] and 3391 [52.2%] male; mean [SD] age, 16.2 [0.6] and 16.1 [0.5] years, respectively). In the intervention group, 0.3% (21 of 7064) had flexural eczema on skin examination and mean (SD) forced expiratory volume in the first second of expiration/forced vital capacity (FEV1/FVC) ratio z score was −0.10 (1.82), compared with 0.7% (43 of 6493) and 0.35 (1.34), respectively, in the control group. In modified intention-to-treat analysis, accounting for clustering by polyclinic, a 54% lower risk of flexural eczema on skin examination was observed in the intervention compared with the control group (odds ratio [OR], 0.46; 95% CI, 0.25 to 0.86). Self-reported flexural eczema symptoms in the past year (OR, 0.57; 95% CI, 0.27 to 1.18), asthma (OR, 0.76; 95% CI, 0.47 to 1.23), and wheezing in the past year (OR, 0.66; 95% CI, 0.37 to 1.18) were less frequently reported in the intervention compared with the control group, but 95% CIs were wide and included the null. There was no significant difference in the FEV1/FVC ratio z score (β −0.15; 95% CI, −0.76 to 0.45). All results were similar with additional adjustment for baseline characteristics, on instrumental variable analysis, and with multiple imputation among all 17 046 randomized participants.
Conclusions and Relevance
A breastfeeding promotion intervention reduced flexural dermatitis risk but had no detectable effect on lung function or questionnaire-derived measures of atopic eczema or asthma in adolescence in a setting where atopic eczema and allergies are rare.
Trial Registration
clinicaltrials.gov Identifier: NCT01561612
This follow-up to a randomized clinical trial evaluates the effect of intervention promoting breastfeeding at the child’s birth on asthma, atopic eczema, and lung function after 16 years.
Introduction
Many allergy organizations, ministries of health, and the World Health Organization recommend between 4 and 6 months of exclusive breastfeeding to aid the prevention of allergy and associated illnesses.1 These recommendations are largely based on cross-sectional studies that have shown contradictory results.2,3,4,5,6 Infancy and early childhood are also critical periods for lung function development, which is linked to asthma. Low lung function at birth is associated with asthma,7 and the onset of asthma in childhood is associated with low lung function through adult life.8 There is some evidence that breastfeeding could influence lung development in childhood and subsequent lung function, but results of observational studies have been inconsistent.9
Methodologic shortcomings might explain some of these contradictions. Observational studies are prone to confounding, in particular because of substantial differences between mothers who do and do not choose to breastfeed, making it difficult to determine whether the observational associations of breastfeeding duration with child health outcomes are causal or have alternative explanations.
The unbiased effects of breastfeeding can probably be convincingly demonstrated only in a randomized clinical trial. While it is not feasible to randomize healthy term infants to be breastfed or bottle fed, it is possible to randomize mother-child pairs to a breastfeeding promotion intervention. The Promotion of Breastfeeding Intervention Trial (PROBIT) is a large, cluster randomized clinical trial of breastfeeding promotion carried out in Belarus.10,11 The randomization achieved marked differences in breastfeeding exclusivity and duration.12 Follow-up of the PROBIT trial participants thus offers a unique opportunity to test the long-term effects of breastfeeding on childhood outcomes, including asthma, lung function, and atopic eczema.
Methods
Study Design
The PROBIT trial design has been described in detail previously.12 In brief, 34 maternity hospitals and 1 each of their affiliated polyclinics (outpatient clinics where children are followed up for routine health care) were paired and randomly assigned to receive either a breastfeeding promotion intervention (experimental group) or continuation of the prevailing maternity hospital and polyclinic practices (control group). Cluster randomization was preferred over individual randomization, because randomizing individual women within the same maternity hospital to different interventions would have led to contamination between the 2 treatment groups and a consequent dilution of the effect of the intervention. After randomization, 2 hospitals refused to participate, and a third randomized site was removed from the trial because of documented falsification of outcome data during infant follow-up.13 These reductions left 16 intervention and 15 control sites in the trial. Recruitment for PROBIT began on June 15, 1996, and continued until December 31, 1997. While it was not possible to blind study staff to the status of each site because they were implementing the intervention, PROBIT participants were blinded to their randomization status.
The 16-year follow-up was approved by the Belarusian Ministry of Health. Ethical approval was obtained from the McGill University Health Centre Research Ethics Board, the institutional review board at Harvard Pilgrim Health Care, and the Avon Longitudinal Study of Parents and Children Law and Ethics Committee. Parents provided written informed consent and children provided written assent for the adolescent follow-up. There was no financial compensation.
Participants
Mothers were eligible for participation if they initiated breastfeeding on admission to the postpartum ward, had no illnesses that would contraindicate breastfeeding or severely compromise its success, and had given birth to a healthy singleton infant of at least 37 completed weeks of gestation, 2500-g birth weight, and an Apgar score of 5 at 5 minutes. Study staff estimated that only 1% to 2% of eligible women declined participation. Since all enrolled women had initiated breastfeeding, the experimental intervention was designed to increase the duration and exclusivity of breastfeeding.
Intervention
The experimental intervention included 10 steps that maternity hospitals must implement to become certified as “baby-friendly.”14 Clinical leaders, usually the chief obstetrician and pediatrician from each of the intervention maternity hospitals and polyclinics, received the 18-hour Baby-Friendly Hospital Initiative lactation management training course, which was organized by the European Regional Office of the World Health Organization. The course emphasized methods to maintain lactation, promote exclusive and prolonged breastfeeding, and resolve common problems. Full implementation of the experimental intervention required 12 to 16 months to train midwives, nurses, and physicians in the provision of care to study mothers and infants during labor, delivery, and the postpartum hospital stay, as well as pediatricians and nurses working at the polyclinics. Monitoring visits were conducted before and during recruitment and follow-up to ensure adherence to and maintenance of the randomized interventions.12
PROBIT Follow-up and Data Quality Assurance
Mother-infant pairs were initially followed up for 12 months from the time of birth, including regular skin assessments for atopic eczema. The primary trial outcome was the risk of 1 or more episodes of gastrointestinal tract infection. The risk of atopic eczema was an important secondary outcome during the initial follow-up and was based on a physical examination at each follow-up visit at the polyclinic affiliated with the maternity hospital. The second follow-up was carried out in 2002 to 2005, when the children were aged 6½ years, and included the International Study for Asthma and Allergies in Childhood (ISAAC) questionnaire to elicit asthma and atopic eczema symptoms, as well as skin-prick tests. The third follow-up was conducted at age 11½ years (2008-2010) but did not include atopy-related outcomes. The present article focuses on the follow-up at 16 years between September 15, 2012, and July 15, 2015, when atopic eczema was once more assessed through physician-conducted skin examination of all participants (primary outcome), the ISAAC questionnaire was completed for self-reported symptoms of asthma and eczema (secondary outcomes), and lung function was measured by spirometry (primary outcome).
Quality assurance was achieved through ongoing data monitoring, as described previously.15 We held an initial workshop during which all participating polyclinic pediatricians were trained in spirometry by the study pediatric pulmonologist (A.J.H.) and in skin examination by the study dermatologist (C.F.) and then formally examined in a written, skills-based test for the diagnosis of atopic eczema. The performance of spirometry and the accuracy of the pediatricians’ diagnosis of atopic eczema was re-examined halfway through the study through a refresher training workshop, directly followed by a further written skills-based test, which all pediatricians successfully passed.
The quality assurance processes raised concerns about the validity of data collected at the 16-year follow-up from 1 polyclinic, and the 16-year data from this clinic were therefore not included in the analyses. In the remaining 30 polyclinics (15 in the intervention group, 15 in the control group), the children were seen at the 16-year visits by 36 research pediatricians: 1 in each of 24 polyclinics and 2 in each of the remaining 6 high-volume clinics.
Atopic Eczema and Asthma Assessments at 16 Years
At the in-person follow-up visit, all children were physically examined for evidence of flexural dermatitis in the following 5 body areas: (1) around the eyes, (2) the neck, (3) at the front of the elbows, (4) behind the knees, and (5) at the front of the ankles, using the validated ISAAC Phase Two skin examination protocol, which is based on the UK refinement of the Hanifin & Rajka consensus diagnostic criteria.16 Like the ISAAC questions, the UK diagnostic criteria focus on flexural involvement to enhance the specificity of the diagnosis. Many other skin diseases are nonflexural but pruritic, such as scabies and fungal infections, and are frequent in low-income country settings. Participants were categorized as having atopic eczema if they had a typical erythematous rash with surface changes (eg, fine scaling, vesicles, oozing, crusting, or lichenification) in any of the abovementioned flexural areas.
In addition to the skin examination, children self-reported their atopic eczema and asthma symptoms in the past 12 months on the ISAAC questionnaire. The instrument was identical to the one used at age 6½ years in the PROBIT cohort,17 but at 6½ years the parent was the respondent. The questions relevant to atopic eczema were: “Have you ever had an itchy rash that was coming and going for at least 6 months?” (yes/no for atopic eczema symptoms ever), “Have you had this itchy rash at any time in the past 12 months?” (yes/no for atopic eczema symptoms past year), and “Has this itchy rash at any time affected any of the following places: folds of the elbows, behind the knees, in front of the ankles, around the neck, or eyes?” (yes/no for flexural eczema past year). Atopic eczema severity was assessed by asking “Has this rash cleared completely at any time during the past 12 months?” and “In the past 12 months, how often, on average, have you been kept awake at night by this itchy rash?” (never in the past 12 months, less than 1 night per week, and 1 or more nights per week). Asthma symptoms were sought through responses to the questions: “Have you ever had asthma?” (yes/no for asthma ever), “Have you had wheezing/whistling in the chest in the past 12 months?” (yes/no for wheezing in the past 12 months), and “Have you had an attack of asthma in the past 12 months?” (yes/no for asthma attack in the past 12 months).
Lung Function Measurements at 16 Years
Lung function was measured by spirometry according to standards recommended by the American Thoracic Society/European Respiratory Society task force18 (Micro 1 handheld spirometer; CareFusion UK). Each spirometer was calibrated at the beginning of each testing session using a 3-L calibration syringe according to the manufacturer’s instructions. The calibration procedure was repeated if results differed by more than 3.5% of the calibrated value. If calibration to within these limits could not be achieved, the spirometer was replaced. Spirometry was avoided within 3 weeks of a reported respiratory infection or a course of oral corticosteroids. Participants were asked to omit long-acting bronchodilators for 48 hours and short-acting bronchodilators for 12 hours prior to the study visit. Pediatricians measured the participant’s height to the last completed millimeter using a stadiometer and weight with an electronic digital scale (Tanita TBF 300GS body-fat analyzer; Tanita Inc). Spirometry was performed in the seated position and participants wore nose clips during each forced expiratory maneuver. Following a demonstration from the tester, participants were instructed to fill their lungs and to blow as hard and fast as possible into the mouthpiece with verbal encouragement from the tester to maintain the breath for as long as possible. Up to 8 attempts were permitted to achieve 3 blows that fulfilled the spirometer’s inbuilt start of test, time to peak flow, and duration criteria.
Lung Function Data Cleaning and Transformation
The results of each accepted blow were analyzed to select the 2 attempts for each participant with the highest forced vital capacity (FVC) that was reproducible to within 0.15 L. Forced expiratory volume in the first second of expiration (FEV1) and FVC were selected from the blow with the higher FVC of the 2 attempts. With application of these criteria, 1374 results (704 in the intervention and 670 in the control group) were excluded from analysis. Lung function variables (FEV1, FVC, and FEV1/FVC ratio) were adjusted for age, height, and sex of the participant using Global Lung Initiative algorithms19 to derive z scores for each.
Data Management
Audit visits were conducted to assess interobserver reproducibility of the outcome data—an important step—given that blinding of pediatricians to the experimental vs control randomized group assignment was not feasible. For each pediatrician in the 24 lower-volume polyclinics, 4 children were randomly selected to return for remeasurement of all variables. For the 6 higher-volume clinics with 2 study pediatricians, 3 children per pediatrician were selected. Thus, a total of 132 children were audited. To ensure that all children seen in follow-up were eligible for the repeated measurements, the selection was carried out after completion of primary data collection, a mean of 1.2 years (range, 0.02-2.5 years) after the initial clinic visit. The audit was carried out by 1 of 3 Minsk-based pediatricians not involved in primary data collection. They were blinded to the measures obtained at the initial visit but not to experimental vs control status.
Study Power
The original sample size for PROBIT was based on power to detect a difference in gastrointestinal tract infections in infancy.12 For this analysis we calculated power based on the available sample size. For the categorical atopic eczema outcome at the 16-year follow-up (flexural eczema on skin examination), the study had 94% power at the 5% significance level to detect a 50% reduction in atopic eczema prevalence between the 2 study groups, similar to PROBIT I.12 This is a large effect compared with other prevention trials, such as the Barrier Enhancement Eczema Prevention trial, which reported 90% power at the 5% significance level to detect a relative reduction in atopic eczema of 30%—a reduction deemed clinically significant.20 As for lung function, the minimal detectable difference in FEV1 or FVC at the 1% significance level with 90% power was 0.04 SD units based on the sample size available.
Statistical Analysis
Because PROBIT is a randomized trial, the primary analytic approach was by modified intention-to-treat (ITT), excluding 1 study center, as described above. We accounted for possible nonindependence of measurements within individual hospitals and their affiliated polyclinic sites (clustering) using mixed effect models. We used the GLIMMIX and MIXED procedures within SAS, version 9.3 (SAS Institute) software for binary outcomes to estimate odds ratios (ORs) (95% CIs). The results are presented for the simple cluster-adjusted model, as well as after additional adjustment for stratum-level (urban vs rural and East vs West Belarus) and for individual-level (child age at follow-up, sex, birth weight, and maternal and paternal educational level) covariates (prespecified secondary analyses). For asthma and lung function models, we also adjusted for length of gestation. To determine whether results differed in boys vs girls, we conducted mixed models that included multiplicative interaction terms for the sex of the child. In a post hoc sensitivity ITT analysis, we used multiple imputation to investigate whether loss to follow-up influenced the results, generating plausible values of missing 16-year outcomes for all 17 046 randomized participants. We used SAS multiple imputations (Proc MI) to impute 20 values for each missing observation and combined multivariable modeling estimates using Proc MI ANALYZE in SAS.21 Data analysis was conducted from May 9, 2016, to April 21, 2017.
The modified ITT analysis may underestimate the effect of the true exposures of interest (breastfeeding exclusivity and duration), owing to overlap in breastfeeding between the randomized groups (many intervention mothers did not exclusively breastfeed for 3 or 6 months, and some control mothers did). Therefore, in a prespecified secondary analysis, we applied instrumental variable methods to estimate the effects of the difference in breastfeeding exclusivity and duration achieved between the 2 randomized groups (≥3 months vs <3 months exclusive breastfeeding, as in the other PROBIT phases12) with the study outcomes. Unlike propensity score matching, this approach uses randomization status as an instrument, assuming that randomization status is independent of any confounders of the exposure-outcome relationships and related to the outcome only via the exposure (breastfeeding duration and exclusivity).22 Effects of exclusive breastfeeding for 3 months or longer using instrumental variable analysis was also estimated after accounting for clustering and further adjusting for strata and individual-level covariates. We used the ivprobit procedure in Stata/SE, version 14 (StataCorp) for binary lung function outcomes and then calculated ORs to be consistent with the primary modified ITT analysis by multiplying the PROBIT estimates by 1.6. The validity of this multiplication has been demonstrated both statistically and empirically.23
To assess whether we could reproduce the inverse associations of increased duration and exclusivity of breastfeeding with outcomes reported in previous observational studies, we also conducted observational analyses (ie, disregarding randomization status) in which we estimated associations of the duration of any or exclusive breastfeeding on the same outcomes, also accounting for clustering and the same baseline characteristics as in the expanded mixed models described above, using multiple logistic regression analysis. Duration of any and exclusive breastfeeding was classified as less than 3 months (reference) or 3 or more months. We used World Health Organization definitions14 for this categorization in which infants were considered as exclusively breastfed for 3 or 6 months if they received no solid food, nonbreast milk, or water or other liquids (other than vitamins or medications) at all visits up to and including the 3- and 6-month visits. They were considered predominantly breastfed at these ages if they received no solid food or nonbreast milk; juices, water, teas, and other liquids were permitted in this category.
Finally, we carried out a post hoc sensitivity analysis in which we stratified the results by whether the children correctly identified their trial group to determine whether this knowledge biased any of the measured outcomes. Furthermore, we examined whether those reporting asthma symptoms had reduced lung function to validate the questionnaire-derived findings. We did not conduct any repeated-measures analyses, because methods of assessment for outcomes differed over time. We ran additional models adjusted for pregnancy smoking status, child smoking status ever and current, and household smoking. Adding these covariates did not appreciably change the results.
Results
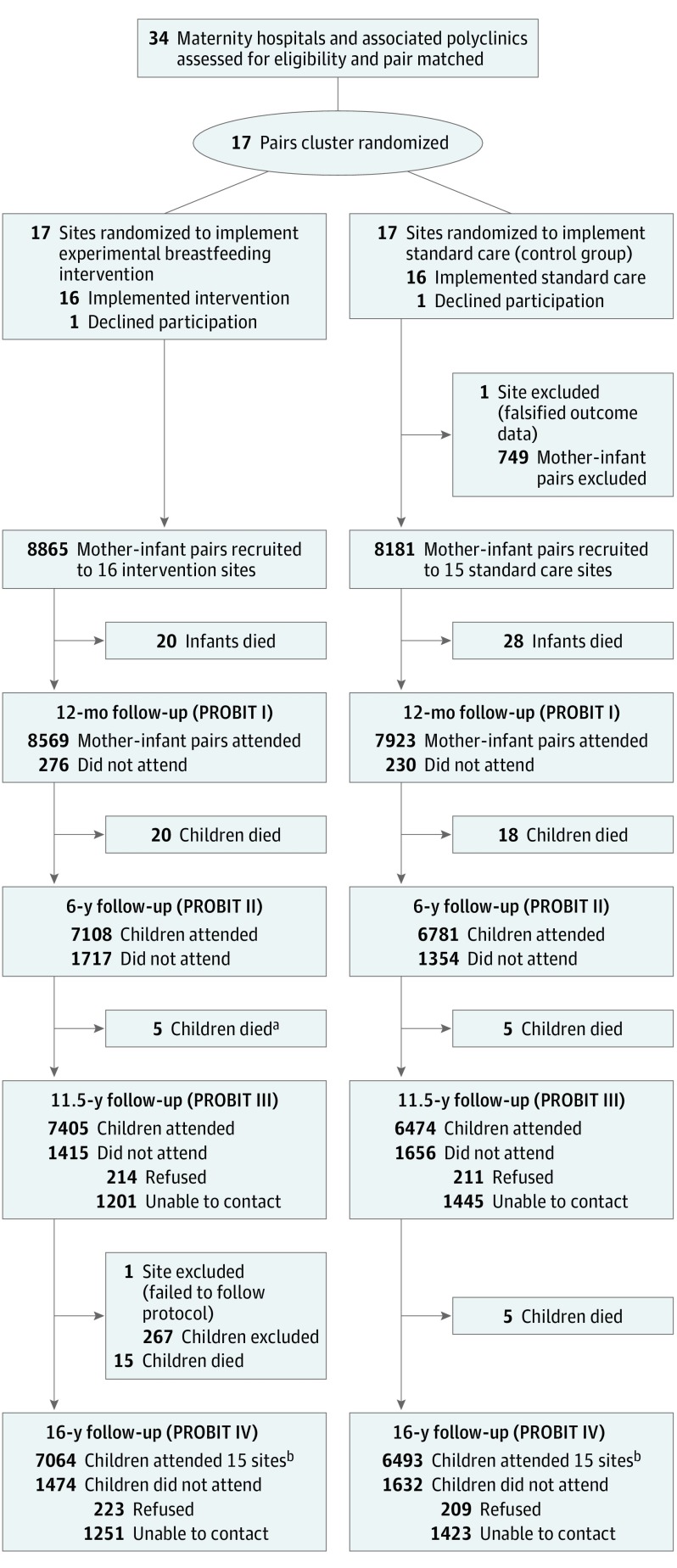
A total of 17 046 mother-infant pairs (8865 [52.0%] intervention and 8181 [48.0%] controls) were enrolled during their postpartum stay. The Figure shows the numbers of infant-mother pairs born at 31 maternity hospitals (16 intervention, 15 control) and followed up at polyclinics randomized to breastfeeding promotion (median cluster size, 501; range, 240-1180) vs usual care (median cluster size, 461; range, 232-940) who participated in the PROBIT IV follow-up. A total of 13 557 adolescents (6981 [51.5%] boys) were examined in the 30 included polyclinics at a median (SD) age of 16.1 (0.54) years (range, 14.8-18.9 years), representing 79.5% of the 17 046 children originally randomized. Asthma and atopic eczema outcomes were available for all participants who were followed up at 16 years.
Figure. Flowchart of Study Sites and Participants.
aDuring Promotion of Breastfeeding Intervention Trial (PROBIT) III, 6 deaths were reported in the intervention arm. Data checking during PROBIT IV found that 1 of these children had been incorrectly reported as dead and data were amended.
bOf the 13 557 children seen at PROBIT IV, 12 072 were seen at both PROBIT II and III, 274 were not seen at either PROBIT II or III, 449 were seen at PROBIT II but not at PROBIT III, and 762 were seen at PROBIT III but not at PROBIT II.
Cleaning of lung function data resulted in 12 183 participants (6360 [52.2%] intervention and 5823 [7.8%] controls) with valid measurements. Of the 3489 participants who were not followed up at 16 years, 116 (3.3%) had died since randomization, 2674 (76.6%) were lost to follow-up, 267 (7.7%) were excluded from 1 clinic that deviated from the study protocol, and 432 (12.4%) were unable or unwilling to come for their visit (Figure). Follow-up rates were similar overall in the experimental (79.7%) and control (79.4%) polyclinics, although they varied by polyclinic from 41.4% to 98.1%.
Participant Characteristics
The intervention (7064 of 8865 [79.7%]) and control (6493 of 8181 [79.4%]) groups were similar at follow-up (3590 [50.8%] and 3391 [52.5%] male; mean [SD] age, 16.2 [0.6] and 16.1 [0.5] years). Other sociodemographic characteristics were comparable between the 2 groups, except for overrepresentation of urban residence in Western Belarus in the intervention group and of advanced secondary/partial university education in the control group (Table 1). Similar results for the population with valid lung function measurements are reported in eTable 1 in the Supplement. We also collected information on parental history of allergic diseases (atopic eczema, asthma, and hay fever) during the 12-month follow up of PROBIT. The intervention group had slightly more mothers and fathers who reported atopy vs the control group (5.2% [463 of 8865] compared with 3.5% [290 of 8181], respectively), and this difference persisted into the adolescent follow-up (χ2 P < .001). However, adjusting for family history of atopy did not alter the risk estimates.
Table 1. Characteristics of 13 557 Children Enrolled in the PROBIT Trial With Outcome Data at 16 Years.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Total (n = 13 557) |
Intervention (n = 7064) |
Control (n = 6493) |
|
| Measured at Child’s Birth | |||
| Maternal age, y | |||
| <20 | 1820 (13.4) | 979 (13.9) | 841 (13.0) |
| 20-34 | 11 173 (82.4) | 5792 (82.0) | 5381 (82.9) |
| ≥35 | 564 (4.2) | 293 (4.1) | 271 (4.2) |
| Maternal education | |||
| Completed university | 1842 (13.6) | 1002 (14.2) | 840 (12.9) |
| Advanced secondary or partial university | 6925 (51.1) | 3365 (47.6) | 3560 (54.8) |
| Common secondary | 4318 (31.9) | 2406 (34.1) | 1912 (29.4) |
| Incomplete secondary | 472 (3.5) | 291 (4.1) | 181 (2.8) |
| Paternal education | |||
| Completed university | 1737 (12.8) | 936 (13.3) | 801 (12.3) |
| Advanced secondary or partial university | 6205 (45.8) | 2910 (41.2) | 3295 (50.7) |
| Common secondary | 4883 (36.0) | 2828 (40.0) | 2055 (31.6) |
| Incomplete secondary or unknown | 732 (5.4) | 390 (5.5) | 342 (5.3) |
| Stratum-level variable | |||
| East/urban | 4150 (30.6) | 2215 (31.4) | 1935 (29.8) |
| East/rural | 2152 (15.9) | 1075 (15.2) | 1077 (16.6) |
| West/urban | 3524 (26.0) | 2296 (32.5) | 1228 (18.9) |
| West/rural | 3731 (27.5) | 1478 (20.9) | 2253 (34.7) |
| No. of other children in household | |||
| 0 | 7707 (56.8) | 4152 (58.8) | 3555 (54.8) |
| 1 | 4717 (34.8) | 2365 (33.5) | 2352 (36.2) |
| ≥2 | 1133 (8.4) | 547 (7.7) | 586 (9.0) |
| Maternal smoking during pregnancy | |||
| No | 13 287 (98.0) | 6898 (97.7) | 6389 (98.4) |
| Yes | 270 (2.0) | 166 (2.3) | 104 (1.6) |
| Child sex | |||
| Female | 6576 (48.5) | 3474 (49.2) | 3102 (47.8) |
| Male | 6981 (51.5) | 3590 (50.8) | 3391 (52.2) |
| Birthweight, mean (SD), kg | 3.44 (0.42) | 3.44 (0.42) | 3.44 (0.42) |
| Gestation length, mean (SD), wk | 39.4 (1.0) | 39.4 (1.0) | 39.3 (1.0) |
| Measured in Child’s First Yeara | |||
| Duration of exclusive breastfeeding, mo | |||
| <3 | 9861 (73.2) | 3821 (54.7) | 6040 (93.1) |
| 3 to <6 | 3126 (23.2) | 2727 (39.0) | 399 (6.2) |
| ≥6 | 484 (3.6) | 437 (6.3) | 47 (0.7) |
| Duration of any breastfeeding, mo | |||
| <3 | 4692 (34.8) | 2085 (29.8) | 2607 (40.2) |
| 3 to <6 | 3105 (23.0) | 1590 (22.7) | 1515 (23.4) |
| ≥6 | 5676 (42.1) | 3315 (47.4) | 2361 (36.4) |
Abbreviation: PROBIT, Promotion of Breastfeeding Intervention Trial.
Denominators based on number reported.
Modified ITT Analyses
Of 7064 children in the intervention group, 21 (0.3%) had signs of flexural eczema on skin examination at the 16-year follow-up (primary outcome), compared with 43 of 6493 (0.7%) participants in the control group (difference, −0.4%; 95% CI, −0.60 to −0.16). This difference corresponded to a 54% lower risk in the intervention compared with control group (cluster-adjusted OR, 0.46; 95% CI, 0.25 to 0.86), with a very similar estimate after further adjustment for baseline factors and age at follow-up (adjusted OR, 0.46; 95% CI, 0.25 to 0.83) (Table 2). The OR was of similar magnitude, but with lower precision, for the questionnaire-derived flexural eczema symptoms (secondary outcomes): flexural eczema in the past year (32 of 7064 [0.5%] vs 45 of 6493 [0.7%]; cluster-adjusted OR, 0.57; 95% CI, 0.27 to 1.18), persistent flexural eczema in the past year (cluster-adjusted OR, 0.48; 95% CI, 0.22 to 1.04), and sleep-disturbed flexural eczema in the past year (cluster adjusted OR, 0.54; 95% CI, 0.23 to 1.28). Effect sizes were similar for boys and girls (all interaction P values >.26).
Table 2. Modified Intention-to-Treat Analysis Comparing Atopic Eczema and Asthma Outcomes in Intervention vs Control Group.
| Variable | No. (%) | OR (95% CI) | ||
|---|---|---|---|---|
| Intervention (n = 7064) | Control (n = 6493) | Cluster Adjusted | Further Adjusteda | |
| Atopic eczema | ||||
| Flexural eczema on skin examination | 21 (0.3) | 43 (0.7) | 0.46 (0.25 to 0.86) | 0.46 (0.25 to 0.83) |
| Flexural eczema past year | 32 (0.5) | 45 (0.7) | 0.57 (0.27 to 1.18) | 0.55 (0.27 to 1.14) |
| Persistent flexural eczema past year | 10 (0.1) | 19 (0.3) | 0.48 (0.22 to 1.04) | 0.47 (0.22 to 1.03) |
| Sleep-disturbed flexural eczema past year | 13 (0.2) | 24 (0.4) | 0.54 (0.23 to 1.28) | 0.55 (0.22 to 1.39) |
| Asthma | ||||
| Ever asthma | 108 (1.5) | 110 (1.7) | 0.76 (0.47 to 1.23) | 0.77 (0.47 to 1.24) |
| Wheezing in past 12 mo | 431 (6.1) | 419 (6.5) | 0.66 (0.37 to 1.18) | 0.61 (0.34 to 1.07) |
| Asthma attack in past 12 mo | 29 (0.4) | 24 (0.4) | 1.01 (0.54 to 1.89) | Did not converge |
Abbreviation: OR, odds ratio.
Adjusted for stratum-level variables (urban vs rural and East vs West Belarus), and for child age at follow-up, sex, birthweight, and maternal and paternal education. Asthma and lung function models were also adjusted for gestational age at birth.
There was no evidence of a protective effect of breastfeeding on the secondary asthma outcomes (Table 2). Asthma ever was reported in 1.5% (108 of 7064) of the intervention group and 1.7% (110 of 6493) of the control group (cluster-adjusted OR, 0.76; 95% CI, 0.47-1.23). Wheezing in the past year was less frequently reported in the intervention compared with the control group (cluster-adjusted OR, 0.66; 95% CI, 0.37-1.18), but the 95% CI was wide and crossed 1.0. There was no significant difference in reported asthma attacks in the past 12 months between the intervention and control groups. The effect estimates for asthma ever and wheezing in the past 12 months were similar after further adjustment for baseline variables.
The FEV1, FVC, and FEV1/FVC ratio were each lower in the intervention than the control group (Table 3). Mean (SD) FEV1% predicted was 91.5 (19.0) in the intervention group and 98.4 (13.3) in the control group. The 95% CIs excluded the null in both cluster-adjusted analyses and following additional adjustment for baseline variables, which only marginally changed the effect estimates (Table 3). However, the FEV1/FVC ratio z score β had a wide 95% CI, including the null: −0.15 (95% CI, −0.76 to 0.45) and −0.16 (95% CI, −0.76 to 0.45), respectively. The FEV1 and FVC at audit visits were strongly correlated with the original polyclinic measurements (FEV1: Pearson r, 0.84; 95% CI, 0.77 to 0.89 and FVC: Pearson r, 0.90; 95% CI, 0.85 to 0.93). In addition, lung function was correlated with height (FEV1: Pearson r, 0.57 and FVC: r, 0.67) and showed expected associations with reported asthma categories (eTable 2 in the Supplement).
Table 3. Modified Intention-to-Treat Analysis Comparing Lung Function Outcomes in Intervention vs Control Group.
| Lung Function | Mean (SD) | β (95% CI) | ||
|---|---|---|---|---|
| Intervention (n = 7064) | Control (n = 6493) | Cluster-Adjusted | Further Adjusteda | |
| FEV1 z score | −0.70 (1.57) | −0.13 (1.12) | −0.43 (−0.78 to −0.08) | −0.39 (−0.74 to −0.04) |
| FVC z score | −0.45 (1.26) | −0.27 (1.12) | −0.23 (−0.60 to 0.13) | −0.19 (−0.56 to 0.17) |
| FEV1/FVC z score | −0.10 (1.82) | 0.35 (1.34) | −0.15 (−0.76 to 0.45) | −0.16 (−0.76 to 0.45) |
| FEV1/FVC × 100 | 0.85 (0.15) | 0.89 (0.09) | −2.03 (−6.34 to 2.29) | −2.03 (−6.36 to 2.30) |
Abbreviations: FEV1, forced expiratory volume in the first second of expiration; FVC, forced vital capacity.
Adjusted for stratum-level variables (urban vs rural and East vs West Belarus), and for child age at follow-up, sex, birthweight, and maternal and paternal education. Asthma and lung function models were also adjusted for gestational age at birth.
Instrumental Variable, Observational, and Sensitivity Analyses
Instrumental variable analysis confirmed an inverse association between exclusive breastfeeding for 3 months or longer vs exclusive breastfeeding for less than 3 months and flexural eczema on skin examination (cluster-adjusted OR, 0.34; 95% CI, 0.13-0.85); additional adjustment for baseline characteristics yielded similar results (OR, 0.34; 95% CI, 0.16-0.72) (Table 4). As in the modified ITT analysis, the risk estimates for questionnaire-derived flexural eczema symptoms in the past year were less precise (cluster-adjusted OR, 0.55; 95% CI, 0.19-1.60; after additional adjustment for baseline characteristics: OR, 0.56; 95% CI, 0.22-1.38) (Table 4). The reduced lung function seen in modified ITT became nonsignificant in the instrumental variable analysis (eTable 3 in the Supplement), which also confirmed no evidence of associations between exclusive breastfeeding for 3 or more months compared with less than 3 months and questionnaire-derived asthma outcomes. Wider 95% CIs in instrumental variable analyses are expected because of the increased variance introduced by using randomization status (intervention vs control group) as a predictor of breastfeeding.
Table 4. Instrumental Variable and Observational Associations of Duration and Exclusivity of Breastfeeding (≥3 Months vs <3 Months) With Atopic Eczema, Lung Function, and Asthma Outcomes.
| Variable | Instrumental Variable Analysis, OR (95% CI) | Observational Analysis, OR (95% CI) | ||
|---|---|---|---|---|
| Cluster Adjusted | Further Adjusteda | Cluster Adjusted | Further Adjusteda | |
| Flexural eczema on skin examination | 0.34 (0.13 to 0.85) |
0.34 (0.16 to 0.72) |
0.70 (0.36 to 1.36) |
0.64 (0.33 to 1.25) |
| Flexural eczema past year | 0.55 (0.19 to 1.60) |
0.56 (0.22 to 1.38) |
0.89 (0.50 to 1.60) |
0.85 (0.47 to 1.53) |
| Persistent flexural eczema past year | 0.40 (0.14 to 1.12) |
0.39 (0.15 to 1.01) |
0.71 (0.29 to 1.75) |
0.70 (0.28 to 1.72) |
| Sleep disturbed flexural eczema past year (ever) | 0.41 (0.13 to 1.23) |
0.46 (0.17 to 1.25) |
0.96 (0.41 to 2.23) |
0.98 (0.41 to 2.30) |
| Wheezing past 12 mo | 0.86 (0.44 to 1.68) |
0.73 (0.38 to 1.40) |
1.02 (0.85 to 1.24) |
1.03 (0.85 to 1.24) |
| Ever asthma | 0.85 (0.39 to 1.85) |
0.82 (0.41 to 1.63) |
0.99 (0.70 to 1.39) |
0.98 (0.70 to 1.38) |
| Asthma attack in past 12 mo | 1.14 (0.50 to 2.59) |
1.06 (0.51 to 2.18) |
1.35 (0.75 to 2.44) |
Did not converge |
Abbreviation: OR, odds ratio.
Adjusted for stratum-level variables (urban vs rural and East vs West Belarus), and for child age at follow-up, sex, birthweight, and maternal and paternal education. Asthma and lung function models were also adjusted for gestational age at birth.
In the observational analysis (exclusive breastfeeding ≥3 months vs <3 months, reference), the magnitude of the protective effect was not as large as the ITT effect (flexural eczema on skin examination: cluster-adjusted OR, 0.70; 95% CI, 0.36-1.36; after additional adjustment for baseline characteristics: cluster-adjusted OR, 0.64; 95% CI, 0.33-1.25; flexural eczema symptoms in the past year: cluster-adjusted OR, 0.89; 95% CI, 0.50-1.60; after additional adjustment for baseline characteristics: OR, 0.85; 95% CI, 0.47-1.53). We observed no evidence of an association comparing any breastfeeding for 3 months or longer vs less than 3 months (reference) (flexural eczema on skin examination: cluster-adjusted OR, 0.94; 95% CI, 0.56-1.56; after additional adjustment for baseline characteristics: OR, 0.88; 95% CI, 0.52-1.47; flexural eczema symptoms in the past year: cluster-adjusted OR, 1.26; 95% CI, 0.77-2.06; after additional adjustment for baseline characteristics: OR, 1.18; 95% CI, 0.72-1.93). Similarly, for asthma outcomes, the observational effects were closer to the null than the estimates from the instrumental variables analysis, with no evidence that exclusive breastfeeding for 3 or more months was associated with ever asthma (cluster-adjusted OR, 0.99; 95% CI, 0.70-1.39), wheezing in the past 12 months (cluster-adjusted OR, 1.02; 95% CI, 0.85-1.24), or asthma attacks in the past 12 months (cluster-adjusted OR, 1.35; 95% CI, 0.75-2.44). Likewise, observational analyses showed no associations between exclusive breastfeeding for 3 or more months and lung function variables.
Finally, the post hoc sensitivity analysis suggested that the protective effect of prolonged exclusive breastfeeding was unlikely to have been biased by nonblinding of the participating adolescents. In the 9581 participants (70.7%) who did not identify their trial group correctly, the protective effect remained large (flexural eczema on skin examination: cluster-adjusted OR, 0.44; 95% CI, 0.22-0.88; flexural eczema symptoms past year: cluster-adjusted OR, 0.57; 95% CI, 0.28-1.16). In the 3893 (28.7%) participants who correctly identified their trial group, the corresponding effect was, if anything, weaker (flexural eczema on skin examination: cluster-adjusted OR, 0.72; 95% CI, 0.18-2.92; flexural eczema symptoms past year: cluster-adjusted OR, 1.10; 95% CI, 0.24-5.13). In a logistic regression analysis including intervention (yes/no), correctly identifying trial group (yes/no), and an interaction term between the 2 factors, the interaction P values were 0.61 for flexural eczema on skin examination and 0.28 for flexural eczema past year, respectively.
Post Hoc Multiple Imputation Analyses
The multiple imputation analyses, based on the sample of 17 046 participants originally enrolled at birth, yielded similar results to those of the modified ITT analyses presented above, although the lung function results lost statistical significance in the fully adjusted model (eTable 4 in the Supplement).
Discussion
There was an approximate 50% reduction in the odds of flexural eczema on skin examination at age 16 years in adolescents born to mothers and infants who attended maternity hospitals and polyclinics randomized to the intervention, compared with those who received standard care. In contrast, no evidence was found for an association between the intervention and self-reported atopic eczema symptoms in the past year or with asthma outcomes (asthma ever or symptoms in the past 12 months). For lung function, there was a negative association between the intervention and FEV1, FVC, and FEV1/FVC ratio in modified ITT analysis, which lost statistical significance in the multiple imputation, instrumental variable, and observational analyses. The conclusions were similar after using instrumental variable and multiple imputation analyses for all other outcomes, and the results for atopic eczema are in keeping with the findings previously reported for the first year of life.12
Strengths and Limitations
The strengths of the PROBIT study include the cluster randomized design, reducing vulnerability to bias and confounding, compared with observational studies. The follow-up rate of 79.5% at 16 years from randomization at birth is high compared with other long-term follow-up studies and makes attrition (selection) bias unlikely, which is also underlined by the similarity of characteristics at follow-up between the 2 randomized groups and the comparable findings in the multiple imputation analysis. Another strength of the study is the use of lung function testing and physician skin examination for atopic eczema using validated, standardized protocols, rather than relying on questionnaire-derived outcomes alone, which results in the misclassification of some atopic eczema cases and consequently weakens associations, as confirmed here. In addition, those who reported wheezing in the past year and a diagnosis of asthma had reduced lung function, providing additional validity to the questionnaire-based outcomes. The robustness of the 16-year follow-up phase with regard to atopic eczema is strengthened further by the stronger inverse association observed in instrumental variable analysis, which accounts for nonadherence to the intervention. In addition, the sensitivity analysis shows that bias due to nonblinding of participants to the randomized trial group is an unlikely explanation of these findings.
Limitations of the study include the remaining possibility that pediatricians’ knowledge of the treatment allocation may have led to unconscious bias in their skin examination. One study center had to be excluded because of concerns about the validity of the data collected. Although the overall follow-up rates were similar between the intervention and control groups (79.7% and 79.4%, respectively), there were differences between the polyclinics, ranging between 41.4% and 98.1%. However, this was equally the case in the intervention and control groups. In addition, the multiple imputation results were consistent with the modified ITT analysis, and all analyses account for clustering within clinics.
A further limitation was the inability to conduct comprehensive quality assurance of measured lung function variables due to technical limitations of the equipment used in the field. However, repeated training was provided throughout the fieldwork, in addition to quality control visits, and by applying a strict threshold of acceptability of lung function results. Lung function could also have been influenced by growth patterns in early childhood,24 but no association was found between lung function measured in adolescence and contemporaneous body mass index, with the latter also being positively associated with rapid early growth.
In contrast to the results for atopic eczema, no evidence was found to support an association of breastfeeding promotion with asthma, which confirms the previously reported findings from the PROBIT study at age 6.5 years. Some studies that reported a protective association of breastfeeding with asthma have suggested that this effect may be stronger for nonatopic asthma,25 but previous results from PROBIT did not support an association between the study intervention and allergic sensitization at age 6.5 years.17
The contrast of the present results with previously reported protective associations with asthma could also arise from misclassification of wheezing in early life as asthma. Wheezing is common in early childhood and often associated with viral respiratory infections, but the majority of preschool wheezing illness does not evolve into asthma.26 An influence of breastfeeding on reducing the frequency of viral infections in early life could have a protective influence on viral-induced wheezing. It is conceivable that diagnosing preschool wheezing as asthma is less likely in settings such as Belarus that have a low prevalence of asthma in childhood.
In addition to the duration and exclusivity of breastfeeding, the specific foods that infants are being weaned to might also have an effect on atopic eczema, asthma, and lung function risk, but this effect is not something that was investigated in PROBIT. However, a recent randomized clinical trial comparing the sequential introduction of 6 allergenic foods from age 3 months (with partial breastfeeding) vs exclusive breastfeeding for 6 months did not show a difference in the risk of atopic eczema or asthma up to age 3 years.27 Finally, some of the questionnaire-based outcomes relied on participant recall, such as asthma diagnosis ever and itchy rash in the past 12 months that involves the flexures. However, participants reporting a diagnosis of asthma or symptoms of flexural atopic eczema showed reduced lung function and strong correlation with atopic eczema on skin examination, supporting the validity of the questionnaire-derived outcomes.
Although basic health services and sanitary conditions in Belarus are similar to those in North America and Western Europe, some aspects of the Belarusian health care system may limit the generalizability of the findings. For instance, the highly centralized Belarusian health care system undoubtedly helped in the implementation of the experimental intervention, resulting in substantial changes in the exclusivity and duration of breastfeeding in the intervention hospitals and polyclinics within a brief prerecruitment period (12-16 months). In addition, the prolonged (6-7 days) postpartum stay for routine vaginal deliveries exceeds that currently found in the West and may have helped to establish good breastfeeding practices and instill maternal confidence.
Furthermore, atopic eczema is less common in Belarus compared with more developed settings, such as North America and Western Europe. These prevalence differences are likely driven by a range of environmental risk factors linked to an affluent lifestyle, including hygiene-related exposures,28 which may overcome and counteract the protective effect of exclusive breastfeeding found in Belarus.
Conclusions
Breastfeeding has many undisputed health benefits. However, most evidence is derived from observational studies and long-term follow up data are sparse. A cluster randomized clinical trial with a breastfeeding promotion intervention had a large protective effect on flexural dermatitis risk, but no detectable effect on lung function or questionnaire-derived measures of atopic eczema or asthma in adolescence in a setting where atopic eczema and allergies are rare.
eTable 1. Characteristics of 12 183 Participants With Valid Lung Function Data
eTable 2. Lung Function in Those Who Reported a Diagnosis of Asthma and Wheezing
eTable 3. Instrumental Variable and Observational Associations of Duration and Exclusivity of Breastfeeding (≥3 Months vs <3 Months) With Lung Function Outcomes
eTable 4. Intention-to-Treat Analysis With Multiple Imputation, Comparing Intervention vs Control Groups (N = 17 046)
References
- 1.Fewtrell M, Wilson DC, Booth I, Lucas A. Six months of exclusive breast feeding: how good is the evidence? BMJ. 2010;342:. [DOI] [PubMed] [Google Scholar]
- 2.Fergusson DM, Horwood LJ. Early solid food diet and eczema in childhood: a 10-year longitudinal study. Pediatr Allergy Immunol. 1994;5(6)(suppl):44-. [DOI] [PubMed] [Google Scholar]
- 3.Forsyth JS, Ogston SA, Clark A, Florey CD, Howie PW. Relation between early introduction of solid food to infants and their weight and illnesses during the first two years of life. BMJ. 1993;306(6892):1572-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sears MR, Greene JM, Willan AR, et al. Long-term relation between breastfeeding and development of atopy and asthma in children and young adults: a longitudinal study. Lancet. 2002;360(9337):901-907. [DOI] [PubMed] [Google Scholar]
- 5.Yang YW, Tsai CL, Lu CY. Exclusive breastfeeding and incident atopic dermatitis in childhood: a systematic review and meta-analysis of prospective cohort studies. Br J Dermatol. 2009;161(2):373-383. [DOI] [PubMed] [Google Scholar]
- 6.Dogaru CM, Nyffenegger D, Pescatore AM, Spycher BD, Kuehni CE. Breastfeeding and childhood asthma: systematic review and meta-analysis. Am J Epidemiol. 2014;179(10):1153-1167. [DOI] [PubMed] [Google Scholar]
- 7.Bisgaard H, Jensen SM, Bønnelykke K. Interaction between asthma and lung function growth in early life. Am J Respir Crit Care Med. 2012;185(11):1183-1189. [DOI] [PubMed] [Google Scholar]
- 8.Tai A, Tran H, Roberts M, et al. Outcomes of childhood asthma to the age of 50 years. J Allergy Clin Immunol. 2014;133(6):1572-8.e3. [DOI] [PubMed] [Google Scholar]
- 9.Waidyatillake NT, Allen KJ, Lodge CJ, et al. The impact of breastfeeding on lung development and function: a systematic review. Expert Rev Clin Immunol. 2013;9(12):1253-1265. [DOI] [PubMed] [Google Scholar]
- 10.clinicaltrials.gov Promotion of Breastfeeding Intervention Trial (PROBIT). NCT01561612. https://clinicaltrials.gov/ct2/show/NCT01561612. Accessed October 1, 2017.
- 11.BioMed Central. Promotion of Breastfeeding Intervention Trial. ISRCTN37687716. http://www.isrctn.com/ISRCTN37687716. Accessed October 1, 2017.
- 12.Kramer MS, Chalmers B, Hodnett ED, et al. ; PROBIT Study Group (Promotion of Breastfeeding Intervention Trial) . Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285(4):413-420. [DOI] [PubMed] [Google Scholar]
- 13.Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of breastfeeding intervention trial (PROBIT): a cluster-randomized trial in the Republic of Belarus: design, follow-up, and data validation. Adv Exp Med Biol. 2000;478:327-345. [PubMed] [Google Scholar]
- 14.WHO/UNICEF Protecting, Promoting and Supporting Breastfeeding: The Special Role of Maternity Services. Geneva, Switzerland: World Health Organization; 1989. [Google Scholar]
- 15.Guthrie LB, Oken E, Sterne JA, et al. Ongoing monitoring of data clustering in multicenter studies. BMC Med Res Methodol. 2012;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weiland SK, Björkstén B, Brunekreef B, Cookson WO, von Mutius E, Strachan DP; International Study of Asthma and Allergies in Childhood Phase II Study Group . Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. Eur Respir J. 2004;24(3):406-412. [DOI] [PubMed] [Google Scholar]
- 17.Kramer MS, Matush L, Vanilovich I, et al. ; Promotion of Breastfeeding Intervention Trial (PROBIT) Study Group . Effect of prolonged and exclusive breast feeding on risk of allergy and asthma: cluster randomised trial. BMJ. 2007;335(7624):815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller MR, Hankinson J, Brusasco V, et al. ; ATS/ERS Task Force . Standardisation of spirometry. Eur Respir J. 2005;26(2):319-338. [DOI] [PubMed] [Google Scholar]
- 19.Quanjer PH, Stanojevic S, Cole TJ, et al. ; ERS Global Lung Function Initiative . Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The University of Nottingham. A randomized controlled trial to determine whether application of emollient from birth can prevent eczema from birth in high risk children. http://www.nottingham.ac.uk/research/groups/cebd/ documents/methodological-resources/beep-protocol-final-version-5.0-26october2016-signed.pdf. Published October 26, 2016. Accessed October 3, 2017.
- 21.White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342:d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scosyrev E. Identification of causal effects using instrumental variables in randomized trials with stochastic compliance. Biom J. 2013;55(1):97-113. [DOI] [PubMed] [Google Scholar]
- 23.Rassen JA, Schneeweiss S, Glynn RJ, Mittleman MA, Brookhart MA. Instrumental variable analysis for estimation of treatment effects with dichotomous outcomes. Am J Epidemiol. 2009;169(3):273-284. [DOI] [PubMed] [Google Scholar]
- 24.den Dekker HT, Sonnenschein-van der Voort AMM, de Jongste JC, et al. Early growth characteristics and the risk of reduced lung function and asthma: a meta-analysis of 25,000 children. J Allergy Clin Immunol. 2016;137(4):1026-1035. [DOI] [PubMed] [Google Scholar]
- 25.Nagel G, Büchele G, Weinmayr G, et al. ; ISAAC Phase II Study Group . Effect of breastfeeding on asthma, lung function and bronchial hyperreactivity in ISAAC Phase II. Eur Respir J. 2009;33(5):993-1002. [DOI] [PubMed] [Google Scholar]
- 26.Morgan WJ, Stern DA, Sherrill DL, et al. Outcome of asthma and wheezing in the first 6 years of life: follow-up through adolescence. Am J Respir Crit Care Med. 2005;172(10):1253-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perkin MR, Logan K, Tseng A, et al. ; EAT Study Team . Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med. 2016;374(18):1733-1743. [DOI] [PubMed] [Google Scholar]
- 28.Flohr C, Mann J. New insights into the epidemiology of childhood atopic dermatitis. Allergy. 2014;69(1):3-16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Characteristics of 12 183 Participants With Valid Lung Function Data
eTable 2. Lung Function in Those Who Reported a Diagnosis of Asthma and Wheezing
eTable 3. Instrumental Variable and Observational Associations of Duration and Exclusivity of Breastfeeding (≥3 Months vs <3 Months) With Lung Function Outcomes
eTable 4. Intention-to-Treat Analysis With Multiple Imputation, Comparing Intervention vs Control Groups (N = 17 046)