Abstract
Importance
Use of laser vitreolysis for symptomatic floaters has increased in recent years, but prospective studies are not available and the complication profile is poorly understood.
Objective
To analyze cases of complications following laser vitreolysis as voluntarily reported to the American Society of Retina Specialists Research and Safety in Therapeutics (ASRS ReST) Committee, an independent task force formed to monitor device-related and drug-related safety events.
Design, Setting, and Participants
A retrospective assessment was performed of all cases of complications following laser vitreolysis that were voluntarily reported by practitioners throughout the United States to the ASRS ReST Committee from the first report on September 19, 2016, through March 16, 2017, the date of data analysis and manuscript writing.
Main Outcomes and Measures
Complications reported to the ASRS ReST Committee following laser vitreolysis were analyzed by type to gain an understanding of the spectrum of potential complications.
Results
A total of 16 complications following laser vitreolysis were reported in 15 patients by 7 US vitreoretinal specialists during the study period. Complications included elevated intraocular pressure leading to glaucoma; cataracts, including posterior capsule defects requiring cataract surgery; retinal tear; retinal detachment; retinal hemorrhages; scotomas; and an increased number of floaters.
Conclusions and Relevance
This report presents a spectrum of complications reported to the ASRS ReST Committee across 6 months. The rate of complications cannot be determined because the denominator of total cases is unknown. Also, these findings cannot determine whether there is a causal association between these complications and laser vitreolysis. Prospective studies are warranted to better understand the efficacy of this procedure and the frequency of attendant complications. Until then, practitioners should be aware of the profile of potential complications to properly inform patients during the consent process. The ASRS ReST Committee will continue to monitor device-related and drug-related adverse events and encourages active surveillance and reporting by all physicians.
This case series analyzes complications following laser vitreolysis as voluntarily reported to the American Society of Retina Specialists Research and Safety in Therapeutics (ASRS ReST) Committee, an independent task force formed to monitor device-related and drug-related safety events.
Key Points
Question
What complications were reported voluntarily to the American Society of Retina Specialists Research and Safety in Therapeutics Committee during a 6-month period in 2016-2017 following laser vitreolysis for the treatment of symptomatic floaters?
Findings
In this case series assessment of 15 patients, complications included glaucoma; cataracts, including posterior capsule defects requiring cataract surgery; retinal tear; retinal detachment; retinal hemorrhages; scotomas; and an increased number of floaters.
Meaning
Ophthalmologists, particularly those offering laser vitreolysis for symptomatic floaters, should be aware of the potential complications associated with this procedure.
Introduction
Nd:YAG laser vitreolysis of symptomatic floaters is not a newly described procedure,1,2,3,4,5 but anecdotal reports suggest that the use of this procedure may be increasing, perhaps owing in part to the marketing of laser systems optimized for vitreolysis. To our knowledge, there are no peer-reviewed prospective trials evaluating this approach, and its efficacy and complication profile are poorly understood.
The American Society of Retina Specialists (ASRS) Research and Safety in Therapeutics (ReST) Committee serves as an independent task force to objectively monitor device-related and drug-related adverse events. Fundamental to the effectiveness of the ASRS ReST Committee is collection and prompt dissemination of information about adverse events that are invariably time sensitive.
During a 6-month period in 2016-2017, the ASRS ReST Committee received reports of complications following laser vitreolysis. In the absence of prospective data, these voluntarily submitted, unsolicited reports may help define a spectrum of associated complications.
Methods
The ASRS ReST Committee collected voluntary, unsolicited reports of all device-related and drug-related adverse events that were submitted from September 19, 2016, through March 16, 2017, through a ReST reporting form on the ASRS website or via personal communication with committee members. Owing to the sensitive nature of procedural complications, only details reported voluntarily without solicitation were analyzed. This study was deemed exempt from institutional review board oversight based on personal communication with the Human Research Protection Program at Allina Health. All patient information was deidentified.
Results
The ASRS ReST Committee received reports of complications in 15 patients following laser vitreolysis. These reports were submitted by 7 clinicians (all retina specialists). The median number of reports per clinician was 1 (range, 1-6). Most patients (14 of 15) were treated with laser vitreolysis elsewhere by a comprehensive ophthalmologist; in 1 case, the reporting retina specialist performed the laser vitreolysis. Geographic location of the adverse events was spread across the United States, with 6 reports from the Northeast, 6 from the West, 2 from the Southeast, and 1 from the Southwest.
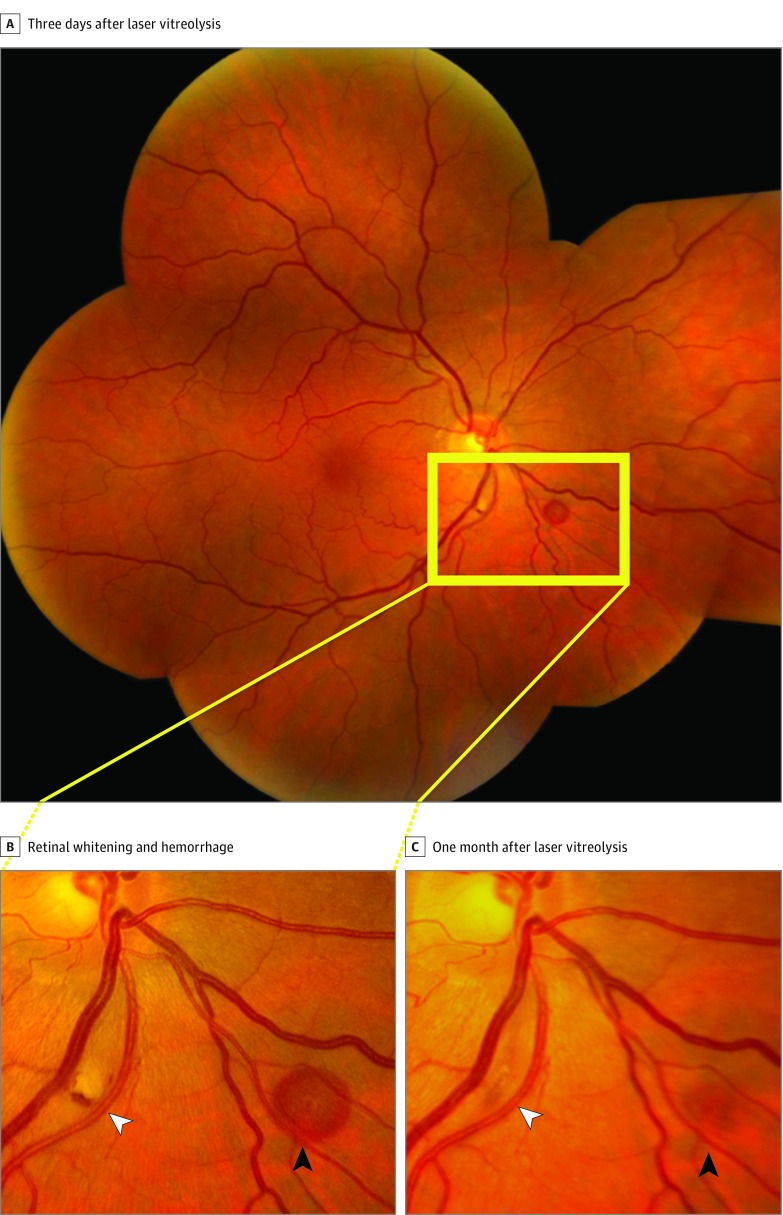
Following laser vitreolysis, 16 complications were reported among the 15 patients. The most frequently reported complications were focal cataracts (5 cases) and prolonged elevation of the intraocular pressure (5 cases). Three of the focal cataracts were within the visual axis, 2 of which had associated posterior capsule rupture. Subsequent cataract extraction was performed in 2 of these cases, while further details were not available for the third. A fourth cataract was reported in the posterior cortex peripherally and was observed. The remaining case did not include details beyond the presence of cataract. Of the 5 cases of prolonged elevation of intraocular pressure, 3 resulted in secondary glaucoma, and trabeculectomy was required in 2 of these cases. Retinal detachment was reported in 2 cases and a retinal tear in 1 case. Laser injury–related transient posterior pole retinal hemorrhages were reported in 2 cases (Figure); in one of these cases, the patient remained asymptomatic, while in the other, a transient scotoma was seen that lasted a few weeks and corresponded to the area of subretinal hemorrhage with nearby retinal whitening. An increased number of symptomatic floaters were reported in 1 patient following laser vitreolysis. In 14 patients, a single complication was reported, whereas in 1 patient, both glaucoma and a retinal tear were reported.
Figure. Transient Hemorrhage and Scotoma Following Laser Vitreolysis.
A, Fundus photograph of a patient 3 days after laser vitreolysis. B, Enlargement of the boxed area in part A demonstrating retinal whitening with associated retinal hemorrhage and possible microhole (white arrowhead) and another area of subretinal hemorrhage (black arrowhead). This patient had a superotemporal scotoma corresponding to the location of this pathologic finding. C, One month later, these findings and scotoma have nearly resolved spontaneously.
Discussion
On behalf of the ASRS ReST Committee, we present a spectrum of complications in 15 patients following laser vitreolysis. This analysis was based on voluntary reports submitted during a 6-month periond to the ASRS ReST Committee. These 15 cases represent, to our knowledge, the largest collection of complications reported to date and include complications of elevated intraocular pressure leading to glaucoma; cataracts, including posterior capsule defects requiring cataract surgery; retinal tear; retinal detachment; retinal hemorrhages; scotomas; and an increased number of floaters.
Peer-reviewed reports regarding laser vitreolysis are limited. A few small case series and individual case reports have described complications, including transient elevation of intraocular pressure,6 refractory glaucoma requiring surgery,7 and acute cataract formation or posterior lens capsule injury8,9,10 requiring surgery, with implantation of an intraocular lens into the sulcus.11,12 Cases of retinal detachment,8,9 uveitis,6 retinal hemorrhage,8,10 and an absolute scotoma hypothesized to be secondary to a detached fragment of neurosensory retina13 have also been described. In the largest peer-reviewed study to date, a retrospective review of 39 eyes treated with laser vitreolysis did not report any postoperative complications, but 7.7% of treated eyes experienced worsening symptoms.14 The spectrum of complications submitted to the ASRS ReST Committee is consistent with these previous reports and indicates that these complications remain relevant to laser vitreolysis as currently performed.
Limitations
There are inherent limitations to this retrospective analysis of voluntarily submitted reports. This collection of reported complications, although robust, is likely underreported and not comprehensive, and there is no way to currently evaluate the number of laser vitreolysis procedures performed. This type of analysis cannot estimate complication rates or their relative frequencies, which would be best determined in prospective, controlled studies. Nearly all reported complications were submitted by physicians other than the treating clinician, suggesting underreporting due to reluctance to report complications in one’s own patients. Alternatively, laser vitreolysis may be performed most commonly by general ophthalmologists, while reporting to ASRS is most commonly done by retina specialists.
Furthermore, the submitted reports were based on the reporting physician’s assessment without additional validation. This analysis cannot definitively identify a causal association between laser vitreolysis and these complications. In addition, these reports did not include details about techniques, equipment, or experience level of the treating clinicians, which is particularly important for procedures for which formal training is not common. However, the geographic distribution of the 15 submitted cases broadly across the United States suggests that these complications are not attributable to a single clinician, device, experience level, or technique.
Because of the sensitive nature of procedural complications, particularly those generally not performed by the reporting retina specialist and compounded by the “off-label” nature of this procedure, the ASRS ReST Committee chose not to solicit further information from reporting clinicians at the time of this pilot assessment. Visual acuity changes, management details, outcomes including floater dissolution and patient satisfaction, and other clinical details are important but not well captured from analysis of voluntary reports. The goals of this pilot assessment were to gauge the spectrum of complications in order to promptly communicate these findings to the ophthalmology community.
Conclusions
Because laser vitreolysis procedures appear to be increasingly performed, it is important for clinicians to be fully aware of its risk vs benefit profile. Success rates in the peer-reviewed literature have been reported only in small retrospective series ranging from 0% to 100%.15 Rigorous prospective studies will be critical to better understand the efficacy of this procedure and the frequency, prognosis, and mechanism of associated complications. The ASRS ReST Committee will continue to monitor and communicate ongoing reports of all device-related and drug-related adverse events.
References
- 1.Peyman GA. Contact lenses for Nd:YAG application in the vitreous. Retina. 1984;4(2):129-131. [PubMed] [Google Scholar]
- 2.Tsai WF, Chen YC, Su CY. Treatment of vitreous floaters with neodymium YAG laser. Br J Ophthalmol. 1993;77(8):485-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toczołowski J, Katski W. Use of Nd:YAG laser in treatment of vitreous floaters [in Polish]. Klin Oczna. 1998;100(3):155-157. [PubMed] [Google Scholar]
- 4.Vandorselaer T, Van De Velde F, Tassignon MJ. Eligibility criteria for Nd-YAG laser treatment of highly symptomatic vitreous floaters. Bull Soc Belge Ophtalmol. 2001;(280):15-19. [PubMed] [Google Scholar]
- 5.Karickhoff JR. Laser Treatment of Eye Floaters. Falls Church, VA: Washington Medical Publishing LLC; 2005. [Google Scholar]
- 6.Aron-Rosa D, Greenspan DA. Neodymium:YAG laser vitreolysis. Int Ophthalmol Clin. 1985;25(3):125-134. [DOI] [PubMed] [Google Scholar]
- 7.Cowan LA, Khine KT, Chopra V, Fazio DT, Francis BA. Refractory open-angle glaucoma after neodymium-yttrium-aluminum-garnet laser lysis of vitreous floaters. Am J Ophthalmol. 2015;159(1):138-143. [DOI] [PubMed] [Google Scholar]
- 8.Little HL, Jack RL. Q-switched neodymium: YAG laser surgery of the vitreous. Graefes Arch Clin Exp Ophthalmol. 1986;224(3):240-246. [DOI] [PubMed] [Google Scholar]
- 9.Tassignon MJ, Kreissig I, Stempels N, Brihaye M. Indications for Q-switched and mode-locked Nd:YAG lasers in vitreoretinal pathology. Eur J Ophthalmol. 1991;1(3):123-130. [DOI] [PubMed] [Google Scholar]
- 10.Fankhauser F, Kwasniewska S, van der Zypen E. Vitreolysis with the Q-switched laser. Arch Ophthalmol. 1985;103(8):1166-1171. [DOI] [PubMed] [Google Scholar]
- 11.Koo EH, Haddock LJ, Bhardwaj N, Fortun JA. Cataracts induced by neodymium-yttrium-aluminium-garnet laser lysis of vitreous floaters. Br J Ophthalmol. 2017;101(6):709-711. [DOI] [PubMed] [Google Scholar]
- 12.Noristani R, Schultz T, Dick HB. Cataract formation after YAG laser vitreolysis: importance of femtosecond laser anterior capsulotomies in perforated posterior capsules. Eur J Ophthalmol. 2016;26(6):e149-e151. doi: 10.5301/ejo.5000854 [DOI] [PubMed] [Google Scholar]
- 13.Van der Veken A, Van de velde F, Smeets B, Tassignon MJ. Nd:YAG laser posterior hyaloidotomy for the treatment of a premacular vitreous floater. Bull Soc Belge Ophtalmol. 1997;265:39-43. [PubMed] [Google Scholar]
- 14.Delaney YM, Oyinloye A, Benjamin L. Nd:YAG vitreolysis and pars plana vitrectomy: surgical treatment for vitreous floaters. Eye (Lond). 2002;16(1):21-26. [DOI] [PubMed] [Google Scholar]
- 15.Milston R, Madigan MC, Sebag J. Vitreous floaters: etiology, diagnostics, and management. Surv Ophthalmol. 2016;61(2):211-227. [DOI] [PubMed] [Google Scholar]