Abstract
Objective
Distal radius fractures are among the most common fractures encountered in clinical practice. Although multiple epidemiological studies have been done in Western populations, there is a lack of data within Asia. Our study aims to fill this knowledge gap.
Methods
This study included all patients aged 16 years and above with distal radius fractures seen between November 2008 and May 2009 by the Department of Hand and Reconstructive Microsurgery at the Singapore National University Hospital. A retrospective analysis was done. Information captured included clinical data, hand dominance, AO classification of fractures, mechanism of injury, associated injuries as well as treatment modalities.
Results
Of the 431 fractures, 238 were males, 181 were females. These fractures occur at all ages, peaking at the 50 to 60 years age group. The peak incidence of distal radius fractures in females occurred in the perimenopausal age group, whereas the incidence for males peaked between age of 30 to 50. By AO classification, 53% were type A; 13% were type B and 32% were type C. A fall on the outstretched hand from a standing position is the most common mechanism of injury. As the intensity of the injury mechanism increased, the percentage of type C fractures increased correspondingly. Older patients were more likely to be treated conservatively compared to younger patients. AO severity classification correlated well with the clinician's decision to surgically fix the fracture. No correlation between hand dominancy and fracture site found was found.
Conclusion
We compared our data with that of previous similar studies, and found similarities as well as differences in results. Nevertheless, the epidemiogical data gathered in this study has added to our knowledge of distal radius fractures in an Asian population.
Keywords: Epidemiology, Radius fracture, Review
Introduction
Distal radius fractures are among the most common fractures encountered in clinical practice, with increasing incidence in many parts of the world including the United States1 and Scandinavia2. As a result, this fracture presents a substantial cost to a country's healthcare sector3. Although multiple epidemiological studies have been done in Western populations, there is a lack of data within Asia. Fracture patterns and demographics may vary between different populations.
Our study aims to fill this knowledge gap. The epidemiological data obtained from a predominantly Asian population can help to guide treatment and prevention of these fractures.
Materials and Methods
This study included all patients aged 16 and above with distal radius fractures (i.e. involving the distal 3 cm of the radius including open fractures, bilateral fractures and in association with other injuries) seen between November 2008 and May 2009 by a single centre in Singapore. Patient case records (electronic and hard copies) were reviewed retrospectively to ensure they met the above criteria. Patients who did not meet these criteria were excluded from the study. Information captured included patient clinical data, hand dominance, Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification of fractures, mechanism of injury, associated injuries as well as treatment modalities. Statistical analysis was done using Chi‐square test, with significance level set at P < 0.05.
Results
Clinical Data
The number of patients who fitted the inclusion criteria was 419, of which 12 had bilateral fractures, bringing the total number of fractures to 431. Males outnumbered females, 238 to 181. These fractures occurred at all ages in our study population, peaking at the 50 to 60 years age group.
Figure 1 shows a breakdown of the age histogram by sex. The peak incidence of distal radius fractures in females occurred in the perimenopausal period (50–60 years) age group, whereas the incidence for males peaked between the age of 40 to 50 years.
Figure 1.
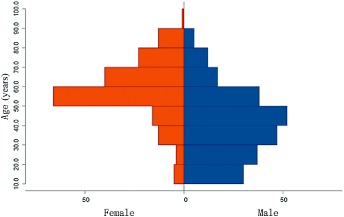
Age histogram by sex.
A breakdown of our study population by race showed Chinese forming the majority (69.2%), followed by Malays (13.1%), Indians (8.6%) and other races (9.1%). This was similar to the makeup of the local population, of which 76.8% were Chinese, 13.9 % were Malays, 7.9% were Indians and 1.4% other races.
AO Classification
Our study used the classification by AO group, which classifies the fractures into type A (extra‐articular), type B (partial articular), and type C (complete articular)4. Our study found 231 or 54% of fractures falling into the extra‐articular type A group, 60 or 14% falling into the partial articular type B group and 140 or 32% falling into the complete articular type C category.
Mechanism of Injury
Our study also classified the mechanism of injury. Type 1 injuries are those resulting from a low velocity fall on the outstretched hand (FOOSH), such as from a standing position (i.e. at ground level). Type 2 are FOOSH injuries of intermediate velocity, such as from a low height (<2 m), bicycle and other sporting activities. Type 3 are FOOSH of a high velocity, such as from a significant height of >2 m, or flung in a motor vehicle accident. Type 4 are crush injuries. Based on our records, Type 1 injuries are the most common (211, 49%), followed by Type 2 injuries (102, 23%), Type 3 (28, 6%) and Type 4 crush injuries (10, 2%). Eighty (20%) of the injuries were not clearly assignable to a fall into any of the above categories.
Distribution of Fracture Type by Mechanism of Injury
Using this classification of mechanism of injury as described above, we compared the first three injury mechanisms, which were all FOOSH injuries but with increasing intensity, against the AO classification (Fig. 2), and we found that as the intensity of the mechanism increased, the percentage of type C fractures increased correspondingly, at the expense of the type A fractures. The percentage of type B fractures remained relatively constant. Thus in a fall injury, the force of a fall corresponds well with classification of distal radius fractures by AO.
Figure 2.
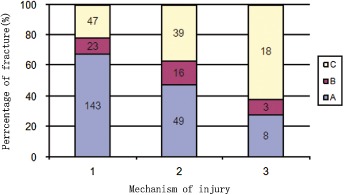
Relationship between mechanism of injury and AO classification. Type A, extra‐articular fracture; type B, partial articular fracture; type C, complete articular fracture. Type 1 injuries are those resulting from a low velocity fall on the outstretched hand (FOOSH); type 2 are FOOSH injuries of intermediate velocity; type 3 are FOOSH of a high velocity.
Age and AO Classification
Seventy‐eight (65.6%) of patients above 60 years of age sustained AO Type A fractures. Thirteen (10.9%) of them sustained Type B fractures while 28 (23.5%) sustained Type C injuries. Of the patients aged 60 or less, 153 (49.0%) sustained Type A fractures, 47 (15.1%) sustained Type B while 112 (35.9%) sustained Type C fractures. This is summarized in Table 1. Thus based on our observations, patients above 60 years of age are more likely to sustain extra‐articular Type A injuries while patients aged 60 or less tend to sustain partial or complete articular injuries.
Table 1.
Relationship between age and AO classification [cases (%)]
| Type | Age (years) | |
|---|---|---|
| >60 | ≤60 | |
| A (231 cases) | 78 (65.6) | 153 (49.0) |
| B (60 cases) | 13 (10.9) | 47 (15.1) |
| C (140 cases) | 28 (23.5) | 112 (35.9) |
| Total (431 cases) | 119 | 312 |
Age and Mode of Treatment
A total of 61.5% of our patients underwent surgery. On reviewing the relationship between age of the patient and mode of treatment, we found that older patients (i.e. more than 60 years of age) were more likely to be treated conservatively, without surgery, as compared to younger patients (i.e. 60 years or less). Table 2 shows this correlation: 94 out of 111 (84.7%) patients aged above 60 with fractures of the distal radius were treated conservatively, compared to 164 out of 308 (53.2%) patients aged 60 or below (P < 0.05). This relation holds true even when we analysed the individual fracture pattern by AO classification. For each fracture type, patients aged 60 years or less were more likely to get surgical treatment as compared to those aged above 60 years (Table 3).
Table 2.
Relationships between age and mode of treatment (cases)
| Age (years) | Cases | Surgery | |
|---|---|---|---|
| No | Yes | ||
| >60 | 111 | 94 | 17 |
| ≤60 | 308 | 164 | 144 |
| Total | 419 | 258 | 161 |
Table 3.
Relationship between AO classification and treatment modality, comparing older and younger patients [cases (%)]
| Type | Treatment modality | Age (years) | P‐value | |
|---|---|---|---|---|
| >60 | ≤60 | |||
| A | Surgery | 6 (7.7) | 47 (30.7) | <0.05 |
| Conservation | 72 (92.3) | 106 (69.3) | ||
| B | Surgery | — | 19 (40.4) | <0.05 |
| Conservation | 13 (100) | 28 (59.6) | ||
| C | Surgery | 11 (39.3) | 83 (74.1) | <0.05 |
| Conservation | 17 (60.7) | 29 (25.9) | ||
AO Classification and Mode of Treatment
Figure 3 shows the rate of fracture fixation in the various AO groups. It shows that Type C fractures were more likely to receive surgical fixation compared to A and B type fractures.
Figure 3.
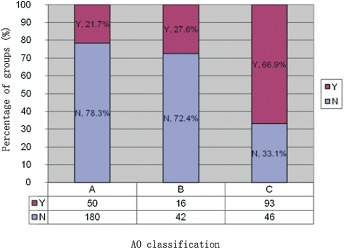
Relationship between AO fracture classification and mode of treatment. Y = Surgery; N = No surgery.
Associated Bony Injuries of the Ipsilateral Arm
Based on our study, there is a high incidence (155 cases, 36%) of associated ulnar styloid fractures. These injuries have treatment implications because of risk of associated triangular fibrocartilage complex (TFCC) injuries and distal radio‐ulnar joint (DRUJ) instability.
Other associated non‐ulnar styloid bony injuries include fractures of the scaphoid (10, 2.3%), metacarpal (5, 1.2%), phalangeal fractures/dislocation (2, 0.5%), radiocarpal dislocation (2, 0.5%), and proximal injuries (5, 1.2%).
Effect of Hand Dominance
Our study found no correlation between hand dominancy and fracture site. 195 patients fell on their dominant hand while 224 fell on their non‐dominant hand. This was not statistically significant.
Discussion
Distal radius fractures are one of the most common extremity fractures encountered. The vast majority of epidemiological studies of this injury are performed in the West. However, we noticed that our patient profile differed from those published, prompting this study. The results show that our pattern of injury differs from many countries, with a larger proportion of males and younger people with this injury. This reflects the kind of activities in our population, e.g. manual work with risks of falls and motorcycle accidents.
In our study, the proportion of males was quite close to that of females. The ratio of male to females was 1.3:1. This is in direct contrast to previous studies5, 6, 7, 8, 9, 10, 11, 12, 13 which show a predominantly female patient profile. The reason for this is that we see males who get injured as a result of industrial work injuries and motor vehicle accidents, especially involving motorcycles which are very common in Singapore.
The age distribution of our study population peaking at the 50 to 60 years age group, is in contrast with the bimodal distribution of these fractures previously reported6. The data from Cuenca et al. was more similar, although their incidence peaked at age of 60 to 69 years14.
The age distribution by sex is similar to previously reported data for females6, 15, steadily increasing until the perimenopausal age group, supporting our opinion that post‐menopausal osteoporosis is a risk factor for distal radius fractures. However, after this peak the incidence of distal radius fractures in our study decreases, unlike in other study populations5, 8, 16, 17 where the incidence continues to increase with age. We postulate that this difference could be due to the fact that the elderly females in our population tend to be less physically active with age compared to their Western counterparts. It can also be due to the fact that Singapore is a tropical country that is warm all year round, thus the risk of slipping on icy streets is negligible compared to countries with more seasonal weather.
In our male population, the peak incidence occurs in persons who were injured at work and in motor vehicle accidents. The incidence decreases with age once past this peak, which differs from previous studies5, 8, but similar to the study by the Royal Infirmary Hospital, Edinburgh18.
We reviewed the age distribution of our local population via the latest population census to check if the age distribution of our study group was merely a reflection of the local age distribution, and found that the peak age group in Singapore is the 30 to 39 years age group, which differs from our study population. Thus, our study age distribution probably provides an actual reflection of the fracture distribution across the different age groups. We do note that the population census in the year 2000 was at least 8 years preceding the study. However these were the latest figures from the national registry at the time the study was performed.
Only two other studies looked at fracture classification according to the AO system5, 19. Our findings are similar to theirs, with type A being the most common and type B the least. Low‐moderate trauma, typically a fall on the outstretched hand from a standing position is the most common mechanism of injury4, 6.
We postulate that the reason why type B fractures are seen least frequently is because to cause a partial articular fracture like a sagittal split (i.e. type B1), a specific force such as a direct impact onto the radius is needed, and this occurs less commonly than a fall on an outstretched hand (Fig. 3).
To our knowledge, ours is the only study comparing fracture pattern with the mechanism of injury. Our findings suggest that in a fall, the greater the force of fall, the more likely the development of complete intra‐articular C‐type fractures.
The percentage of patients who were treated surgically is relatively high compared to the study done by Fanuele et al. across the US9. This is due to our relatively younger patient profile having more severe injuries and C‐type fractures. From our study, patients aged above 60 were more likely to receive conservative treatment probably due to a variety of reasons. It could be that their injuries tend to be less severe (by AO classification) which we showed in our study, or it could also be due to other factors like personal reluctance to undergo surgery or the presence of comorbidities which increases surgical risk, as our subgroup analysis for each fracture type showed a predisposition towards conservative treatment in patients aged above 60 years. Future epidemiological studies can look into these other possible factors. The current recommendation by the American Academy of Orthopaedic Surgeons (AAOS)20 for surgical fixation includes radial shortening >3 mm, dorsal tilt >10 degrees and intra‐articular step of >2 mm. Perhaps future studies can correlate these recommendations to clinical outcomes in a predominantly Asian population to see to what extent these recommendations benefit Asian patients.
The relatively high incidence of associated injuries of the ipsilateral arm suggest that they should be actively sought in a case of distal radius fracture. Our data differed slightly from that from Edinburgh (Broadbent et al.19), who found that distal radius fractures were most commonly associated with fractures of the proximal humerus, followed by fractures of the radial head and olecranon. However, fractures of the hand were excluded from their study. Because the superficial part of the TFCC is attached to the ulnar styloid, fractures of the distal radius with associated fractures of the ulna styloid can cause injury to the TFCC and lead to DRUJ instability. This can lead to ulna‐sided wrist pain as well as decrease in forearm rotation21.
Pesola et al.22 suggests a lateralizing predisposition for left distal radius fractures in older compared with younger individuals who are right hand handed. Our study found no such correlation.
To our knowledge, our study is the only comprehensive epidemiological review in a predominantly Asian population. Entry criteria were clearly defined (i.e. distal 3 cm of the radius). Other studies had more ambiguous entry criteria. Mechanism of injury was also clearly defined in our study7. This was less well defined in previous studies5, 23.
Our study does not allow us to calculate the incidence rate of distal radius fractures among our local population, unlike previous studies5, 6, 23. Although our centre is based in the Western part of the country, patients can choose where they seek medical treatment, so not all residents in that region are seen at our centre.
Our results fill a knowledge gap in epidemiology of a very common fracture. Distal radius fractures occur in all age groups, peaking at uniquely different ages in males and females. Type A fractures are the most common, while type B are the least common. The mechanism of injury correlates well with the AO classification. The AO classification, in turn, correlates well with percentage of fractures fixed surgically. These fractures are more likely to be treated conservatively in older (>60 years) patients. Associated injuries (ulnar styloid, scaphoid, metacarpal etc.) are common and should be actively looked for. Our study found no correlation between hand dominance and fracture site.
The distal radius fracture patterns seen in our hospital differs from that in many reports. A larger proportion of males and younger people with this injury, reflects the kind of activities in our population, e.g. manual work with risks of falls and motorcycle accidents. This has implications on efforts on injury prevention, treatment and outcomes assessment.
Disclosure: The authors state that they have no actual or potential conflict of interest.
References
- 1. Melton LJ 3rd, Amadio PC, Crowson CS, O'Fallon WM. Long‐term trends in the incidence of distal forearm fractures. Osteoporos Int, 1998, 8: 341–348. [DOI] [PubMed] [Google Scholar]
- 2. Bengnér U, Johnell O. Increasing incidence of forearm fractures. A comparison of epidemiologic patterns 25 years apart. Acta Orthop Scand, 1985, 56: 158–160. [DOI] [PubMed] [Google Scholar]
- 3. Kakarlapudi TK, Santini A, Shahane SA, Douglas D. The cost of treatment of distal radial fractures. Injury, 2000, 31: 229–232. [DOI] [PubMed] [Google Scholar]
- 4. Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br, 1996, 78: 726–731. [PubMed] [Google Scholar]
- 5. Brogren E, Petranek M, Atroshi I. Incidence and characteristics of distal radius fractures in a southern Swedish region. BMC Musculoskelet Disord, 2007, 8: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Owen RA, Melton LJ 3rd, Johnson KA, Ilstrup DM, Riggs BL. Incidence of Colles’ fracture in a North American community. Am J Public Health, 1982, 72: 605–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thompson PW, Taylor J, Dawson A. The annual incidence and seasonal variation of fractures of the distal radius in men and women over 25 years in Dorset, UK. Injury, 2004, 35: 462–466. [DOI] [PubMed] [Google Scholar]
- 8. Maravic M, Le Bihan C, Landais P, Fardellone P. Incidence and cost of osteoporotic fractures in France during 2001. A methodological approach by the national hospital database. Osteoporos Int, 2005, 16: 1475–1480. [DOI] [PubMed] [Google Scholar]
- 9. Fanuele J, Koval KJ, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am, 2009, 91: 1313–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hove LM, Fjeldsgaard K, Reitan R, Skjeie R, Sörensen FK. Fractures of the distal radius in a Norwegian city. Scand J Plast Reconstr Surg Hand Surg, 1995, 29: 263–267. [DOI] [PubMed] [Google Scholar]
- 11. Falch JA. Epidemiology of fractures of the distal forearm in Oslo, Norway. Acta Orthop Scand, 1983, 54: 291–295. [DOI] [PubMed] [Google Scholar]
- 12. Solgaard S, Petersen VS. Epidemiology of distal radius fractures. Acta Orthop Scand, 1985, 56: 391–393. [DOI] [PubMed] [Google Scholar]
- 13. Larsen CF, Lauritsen J. Epidemiology of acute wrist trauma. Int J Epidemiol, 1993, 22: 911–916. [DOI] [PubMed] [Google Scholar]
- 14. Cuenca J, Martínez AA, Herrera A, Domingo J. The incidence of distal forearm fractures in Zaragoza (Spain). Chir Main, 2003, 22: 211–215. [DOI] [PubMed] [Google Scholar]
- 15. Kulej M, Dragan S, Krawczyk A, Orzechowski W, Płochowski J. Epidemiology of distal radius fractures in own material–own experience. Ortop Traumatol Rehabil, 2008, 10: 463–477. [PubMed] [Google Scholar]
- 16. Miller SW, Evans JG. Fractures of the distal forearm in Newcastle: an epidemiological survey. Age Ageing, 1985, 14: 155–158. [DOI] [PubMed] [Google Scholar]
- 17. van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone, 2001, 29: 517–522. [DOI] [PubMed] [Google Scholar]
- 18. Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury, 2006, 37: 691–697. [DOI] [PubMed] [Google Scholar]
- 19. Broadbent MR, Quaba O, Hadjucka C, McQueen MM. The epidemiology of multifocal upper limb fractures. Scand J Surg, 2003, 92: 220–223. [DOI] [PubMed] [Google Scholar]
- 20. American Academy of Orthopaedic Surgeons . The treatment of distal radius fractures‐guideline and evidence report. Dec 5 2009.
- 21. Tsai PC, Paksima N. The distal radioulnar joint. Bull NYU Hosp Jt Dis, 2009, 67: 90–96. [PubMed] [Google Scholar]
- 22. Pesola GR, Feinberg GA, Ahsan H. Preferential distal radius fracture in right‐handed individuals presenting to an ED. Am J Emerg Med, 2003, 21: 552–555. [DOI] [PubMed] [Google Scholar]
- 23. Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal radius fractures in older women: a 10‐year follow‐up study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc, 2002, 50: 97–103. [DOI] [PubMed] [Google Scholar]


