Abstract
Objective
The purpose of this study was to present the surgical technique and clinical results of percutaneous compression plate (PCCP) for the treatment of femoral neck fractures.
Methods
Between December 2010 and April 2013, 74 consecutive patients with 74 femoral neck fractures were treated by closed reduction and PCCP implants in our university hospital. Their mean age was 51.3 years (range, 15–83 years); 38 (51.4%) were male and 46 (62.2%) of the fractures were on the left. The patients' clinical and radiographic data were analyzed retrospectively.
Results
There were 45 undisplaced (60.8%) and 29 displaced fractures (39.2%). Eight patients (10.8%) were lost to follow‐up. The mean duration of follow‐up was 18.8 months for the remaining 66 patients. At the last follow‐up, mean Harris hip score was 92.9 (range, 75–100), and 65 patients (98.5%) had excellent and good outcomes. Sixty‐five patients (98.5%) were able to walk independently and one (1.5%) with walking‐sticks. The mean time to clinical fracture healing was 3.9 months. There were no cases of nonunion. Two patients (3.0%) had delayed union and two (3.0%) developed avascular necrosis, one of 29 (3.7%) with a displaced fracture and one of 45 (2.6%) with an undisplaced fracture. There were no other complications or prosthetic replacement.
Conclusions
PCCP is a stable internal fixation device that resists axial and rotational stresses. Our PCCP procedure has a low incidence of nonunion and avascular necrosis.
Keywords: Femoral neck fracture, Internal fixation, Percutaneous compression plate
Introduction
Hip fractures are associated with a 30% mortality rate at one year and result in profound temporary, and sometimes permanent, impairment of independence and quality of life1. Approximately 50% of all hip fractures are femoral neck fractures. In young and active patients, the goal of treatment is to preserve the femoral head, achieve union, and avoid avascular necrosis (AVN) by anatomic reduction and stable fixation of the femoral neck2, 3. In older patients, the fracture pattern alone determines the treatment of undisplaced fractures, which are also managed with internal fixation3, 4.
Currently, the preferred means of fixation are multiple cannulated screws (MCS) and sliding hip screws (SHS)5, 6. Regardless of the means of fixation, femoral neck fractures are associated with a high incidence of serious complications; namely, nonunion and AVN which are reported to occur in 33% and 16% of displaced fractures and 6% and 4% of undisplaced fractures7, 8. Accordingly, the rate of revision surgery is as high as 48%9.
The percutaneous compression plate (PCCP), a minimally invasive, double axis implant that provides rotational stability, prevents fracture dislocation and allows immediate full weight‐bearing, was originally developed for the treatment of pertrochanteric hip fractures by Gotfried10. A recent study has confirmed that PCCPs provide better biomechanical stability than standard SHS in patients with femoral neck fractures11. However, there few clinical reports of the outcomes of this approach in a series of patients with femoral neck fractures. Described here are the results for the first 74 patients treated at one center with PCCP.
Materials and Methods
Patients
Between December 2010 and April 2013, 74 consecutive patients with 74 femoral neck fractures were treated by closed reduction and internal fixation with PCCPs in the Orthopedic Department of our hospital. Details of the treatment and follow‐up of the patients were prospectively recorded and retrospectively analyzed.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (i) age 65 years or less with a displaced or undisplaced fracture or older than 65 years with an undisplaced femoral neck fracture; (ii) surgery performed within two weeks of fracture; (iii) underwent closed reduction and percutaneous fixation with a PCCP; and (iv) more than 6 months of follow‐up.
Patients with pre‐existing symptomatic osteoarthritis of the hip, rheumatoid arthritis, open, previous or pathologic fractures and malignant disease were excluded.
Principles of Treatment
On admission to hospital, tibial tubercle traction was implemented in patients with displaced fractures. T‐sharps were used in those with undisplaced fractures. Routine investigations included complete blood cell count, urine and stool monitoring, biochemical monitoring, electrocardiography and chest radiography. A first‐generation cephalosporin (2.0 gqd, i.v.) was administered intra‐operatively and for 48 h postoperatively. Drainage tubes were not employed in any patient.
Postoperatively, patients were instructed to ambulate with walking‐sticks or a walker within 3 days of surgery, followed by a gradual increase to full weight bearing by 2–3 months. After discharge, patients were followed up monthly until six months from injury, then every three months.
Data of Eligible Patients
Age at the time of surgery, sex, affected side, mechanism of injury, previous history, concurrent injury, Garden's classification12, Pauwel's classification13 and bone quality assessed according to the Singh index14 were recorded preoperatively for all eligible patients.
Duration from injury to operation, operation time, intraoperative blood loss, perioperative transfusions, quality of reduction, preoperative, postoperative and total hospital stay, postoperative complications, fracture consolidation, pre‐injury activity, Harris hip score and activity at the last follow‐up were recorded postoperatively. The quality of reduction was assessed on the first postoperative radiographs according to the Garden alignment index15, 16.
Surgical Technique for PCCP
After induction of general anesthesia, the patient was positioned supine on the traction table with the contralateral limb flexed and abducted to allow positioning of the image intensifier. For displaced fractures, the fracture was first reduced by gentle longitudinal traction to restore the limb length and then further reduced by internal rotation, after which the reduction was checked on anterior‐posterior (AP) and lateral views. After connecting to the introducer, an approximately 2 cm incision was made opposite the proximal border of the lesser trochanter and a PCCP plate introduced using a chisel end as a periostotome elevator. The height was checked via a template with the scope and the plate fixed by a register pin to allow confirmation of the position of the distal neck screw on AP and lateral radiographs. An inferior incision of approximately 3 cm was then made, the plate applied to the femoral shaft by means of a bone hook and the height checked, after which the screws were placed in the following order: distal neck screw, proximal, middle and distal shaft screws, proximal neck screw and all checked by radiographically (Fig. 1).
Figure 1.
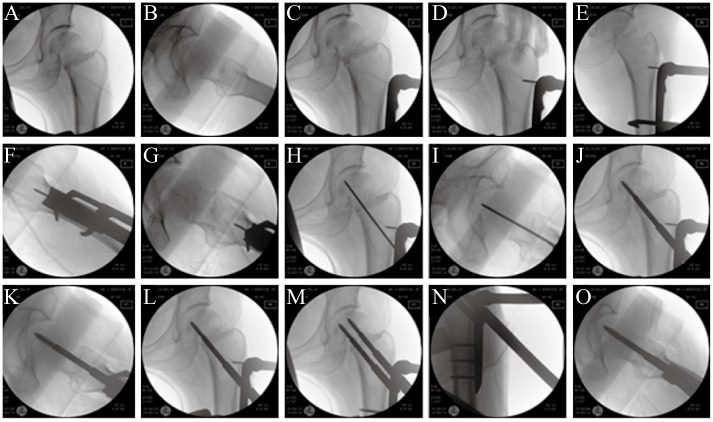
Intraoperative radiographs of internal fixation procedure. (A, B) After reduction had been achieved, the fracture is checked on AP and lateral views. (C) After it has been introduced, the height of the plate is checked on the AP view. (D) The plate is fixed with a register pin. (E, F) A bone hook is used to fix the plate temporarily and the position of the plate is checked on AP and lateral views. (G) The register pin is used to confirm the direction of the distal neck screw on the lateral view. (H, I): The guide wire is advanced into the femoral neck and its position confirmed on AP and lateral views. (J, K) The distal neck screw is screwed up to the subchondral bone and checked on AP and lateral views. (L) The fracture is compressed. (M) After the other screws have been fixed, the neck screws are checked on the AP view. (N) The three shaft screws are checked on the AP view. (O) The two neck screws are checked on the lateral view.
Results
Relevant preoperative data on the 74 patients with femoral neck fractures are listed in Table 1. Their mean age was 51.3 years (range, 15–83 years); 38 (51.4%) were male and 46 (62.2%) of the fractures were on the left. Forty‐three patients (58.1%) had fallen from standing and the other 31 (41.9%) had been injured in traffic accidents or other high energy trauma; among the latter were 13 (17.6%) patients with polytrauma. According to the Garden classification, there were 45 (60.8%) non‐displaced and 29 (39.2%) displaced fractures. The Singh index gradings14 were as follows: 47 (63.5%) grade 6, 20 (27.0%) grade 5 and 7 (9.5%) grade 4. The duration from injury to operation was 5.7 days (range, 2–13 days). The operative time was 73.4 min (range, 35–210 min). The intraoperative blood loss was 116.4 mL (range, 10–500 mL). Seventy patients (94.6%) did not need perioperative blood transfusion. The preoperative hospital stay was 4.9 days (range, 2–9 days), the postoperative hospital stay 8.0 days (range, 2–15 days) and the total hospital stay 12.9 days (range, 7–19 days). The surgeons' learning curve was such that the average operation time was within 45 minutes. According to the Garden alignment index, anatomic reduction was achieved in 24/29 (82.8%) displaced fractures and acceptable reduction in 5/29 (17.2%) fractures. There were no general or local intraoperative complications. There were no postoperative superficial infections, pulmonary embolism, deep vein thrombosis or decubitus ulcers.
Table 1.
Preoperative data on the 74 patients with femoral neck fractures
| Characteristic | No. of patients | Percent (%) |
|---|---|---|
| Side of fracture | ||
| Left | 46 | 62.2 |
| Right | 28 | 37.8 |
| Mechanism | ||
| Fall from standing | 43 | 58.1 |
| Traffic accident or other high energy trauma | 31 | 41.9 |
| Comorbidities | ||
| Hypertension | 23 | 31.1 |
| Diabetes mellitus | 9 | 12.2 |
| Heart condition | 2 | 2.7 |
| Stroke | 2 | 2.7 |
| Polytrauma | 13 | 17.6 |
| Fracture classification | ||
| Non‐displaced fracture (Garden I and II) | 45 | 60.8 |
| Displaced fracture (Garden III and IV) | 29 | 39.2 |
| Pauwels I | 1 | 1.4 |
| Pauwels II | 44 | 59.5 |
| Pauwels III | 29 | 39.2 |
| Bone quality (Singh index) | ||
| Grade 6 | 47 | 63.5 |
| Grade 5 | 20 | 27.0 |
| Grade 4 | 7 | 9.5 |
Eight of 74 patients (10.8%) were to lost follow‐up, leaving 66 patients for analysis, including 27 displaced and 39 undisplaced fractures. The mean duration of follow‐up was 18.9 months (range, 6–34 months). The mean time to clinical fracture healing was 3.9 months (range, 1.5–10 months). Functionally, prior to fracture, all patients were independent walkers. At the last follow‐up, the mean Harris hip score was 92.9 (75–100). The scores of 52 patients (78.8%) were excellent; 13 (19.7%) good and one (19.7%) moderate. Sixty‐five patients (98.5%) were walking independently and one (1.5%) with walking‐sticks. There were no instances of material failure, re‐displacement, nonunion, death or prosthetic replacement. Two patients (3.0%) with displaced fractures had delayed union. One of these, a 61‐year‐old man with a Garden III femoral neck fracture, achieved acceptable reduction with internal fixation. His time to clinical fracture healing was 10 months without any intervention and his Harris hip score was 95 with independent walking at the last follow‐up (19 months postoperatively). The other patient with delayed union, a 38‐year‐old man, had a Garden III femoral neck fracture. His time to clinical fracture healing was about 7.5 months, acceptable reduction being achieved without any intervention. However, he gradually developed AVN and collapse of the femoral head (Fig. 2). His Harris hip score was 90 with independent walking at the last follow‐up (28 months postoperatively). In addition, another patient, a 66‐year‐old man with a Garden II femoral neck fracture, developed cystic changes in the femoral head. His time to clinical fracture healing was about 4 months and his Harris hip score 96 with independent walking at the last follow‐up (31 months postoperatively). Two patients (3.0%) developed AVN, one of 29 (3.7%) with a displaced fracture and one of 45 (2.6%) with an undisplaced fracture; they were treated conservatively and required no medications.
Figure 2.

A Garden III and Pauwels II femoral neck fracture in a 38‐year‐old man treated by closed reduction and fixation with a percutaneous compression plate (PCCP). (A) Preoperative radiograph; (B) Radiograph after fixation with PCCP; (C) Radiograph 28 months after operation showing avascular necrosis and collapse of the femoral head.
Discussion
Osteosynthesis for femoral neck fractures has been studied extensively. The two most commonly used types of implant for these fractures are MCS and SHS. Screw and side‐plate constructs seem to perform better than MCS9, 17. The disadvantages of MCS are the poor hold of the fracture laterally5. The SHS provides poorer rotational stability than three cannulated screws18. The addition of a de‐rotation screw to SHS can offset this disadvantage; however, this device still lacks a stable‐angle configuration and offers no advantages with regard to fracture union19.
The chisel end of the plate and modular design of the neck screw allows PCCPs to be introduced through a small incision. The 135° angled plate and double‐axis neck screw configuration maintain the neck shaft angle and resist vertical shearing, varus and rotational stress. Fracture compression is performed by the surgeon. Additionally, controlled fracture impaction is achieved passively by the patient during subsequent postoperative ambulation, facilitating fracture healing20. PCCPs have been demonstrated to provide better biomechanical stability in femoral neck fractures than standard SHS in vitro 11. Several authors have reported excellent results for treatment of femoral neck fracture with PCCPs. In 2007, Brandt was the first to report a patient with a femoral neck fracture treated with PCCP who was mobilized with full weight‐bearing from the first postoperative day without any limitations. The blood loss was minimal and the wounds (two small incisions of 2 cm each) healed without complications21. Mukherjee and Ashworth were the first to report using a PCCPs to treat an intracapsular neck of femur fracture with nonunion. Postoperatively, the patient was fullly weight‐bearing and completely pain‐free with bony union at 6 months22.
In the present series, nonunion did not occur in any patient. In comparison, several published series of other implants have reported a rate of nonunion of 6% for undisplaced and 33% for displaced fractures7, 8. The outcome of treatment of femoral neck fractures with Targon femoral neck hip screws is satisfactory; however, the reported rate of nonunion is 2.7% for undisplaced and 15.4% for displaced fractures23. Poor reduction and fracture displacement after fixation of femoral neck fractures have been consistently found to be predictive of nonunion2. In our series, two patients (3.0%) with displaced fractures and acceptable reduction had delayed union. The delayed union may have been associated with the level of reduction and fracture displacement.
Regarding AVN, the overall rate in this series was 2.6% for undisplaced and 3.7% for displaced fractures, which is lower than the reported 4% for undisplaced and 16% for displaced fractures7, 8. Our rate is also lower than the 4.5% for undisplaced and 11.1% for displaced fractures reported by Parker et al.23. The primary source of the blood supply to the femoral head is the deep branch of the medial femoral circumflex artery. Impaired blood supply to the femoral head increases the risk of AVN. Previous studies have suggested that displaced fractures are more frequently associated with AVN than undisplaced fractures. Subcapital fractures are particularly prone to the development of AVN because the terminal branches of medial femoral circumflex artery enter the head in this region24.
The role of capsulotomy or aspiration in the treatment of femoral neck fractures remains controversial. Previous studies have suggested that increased intracapsular pressure is a major factor in the development of AVN in undisplaced fractures25. However, studies on displaced fractures do not support the theory that AVN is a consequence of hip joint tamponade26. In our study, we did not perform capsulotomy or aspiration; thus, increased intracapsular pressure may have contributed to development of AVN in the one patient with an undisplaced fracture in whom this complication occurred.
Whether duration from injury to surgery can lead to AVN in patients with femoral neck fractures is controversial. Razik et al. have demonstrated that the method of internal fixation is a stronger predictor of AVN of the femoral head than delay in internal fixation. They found no support for the current belief that early surgical fixation of femoral neck fractures reduces the risk of AVN27. Wongwai et al. have reported a low rate of AVN in young patients in whom reduction and screw fixation of displaced femoral neck fractures was delayed for up to 30 days28. In our study, all patients underwent delayed surgery and there was a low rate of AVN. However, with displaced fractures, employment of tibial tubercle traction assists in reduction of the fracture and unkinking of vessels, thus improving blood flow to the femoral head and minimizing the risk of AVN4. With undisplaced fractures, use of T‐sharps may prevent subsequent displacement and vascular damage.
The current study had some limitations; namely, the relatively small number of cases and short follow‐up limits the conclusions. It was also a single‐center study and there was no comparison group of patients or randomization to a group treated with a conventional fixation method such as SHS or MCS.
In summary, the PCCP is a stable internal fixation device that resists axial and rotational stresses. When used to treat femoral neck fractures, it achieves good functional reduction and has a low risk of nonunion and AVN.
Disclosure: This work was supported by the Jiangsu Province Key Medical Center, Jiangsu Provincial Special Program of Medical Science (BL2012004), the National Nature Science Foundation of China (Grant nos. 81472077, 81372018, 81101399), and the Project of Jiangsu College Graduate Research and Innovation Program (CXZZ13_0835).
References
- 1. Zielinski SM, Meeuwis MA, Heetveld MJ, et al Adherence to a femoral neck fracture treatment guideline. Int Orthop, 2013, 37: 1327–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yang JJ, Lin LC, Chao KH, et al Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am, 2013, 95: 61–69. [DOI] [PubMed] [Google Scholar]
- 3. Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type‐3 vertical femoral neck fractures. J Bone Joint Surg Am, 2008, 90: 1654–1659. [DOI] [PubMed] [Google Scholar]
- 4. Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. J Bone Joint Surg Am, 2008, 90: 2254–2266. [PubMed] [Google Scholar]
- 5. Parker MJ, Stedtfeld HW. Internal fixation of intracapsular hip fractures with a dynamic locking plate: initial experience and results for 83 patients treated with a new implant. Injury, 2010, 41: 348–351. [DOI] [PubMed] [Google Scholar]
- 6. Rupprecht M, Grossterlinden L, Ruecker AH, et al A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma, 2011, 71: 625–634. [DOI] [PubMed] [Google Scholar]
- 7. Conn KS, Parker MJ. Undisplaced intracapsular hip fracture: results of internal fixation in 375 patients. Clin Orthop Relat Res, 2004, 421: 249–254. [PubMed] [Google Scholar]
- 8. Lu‐Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck: a meta‐analysis of one hundred and six published reports. J Bone Joint Surg Am, 1994, 76: 15–25. [DOI] [PubMed] [Google Scholar]
- 9. Eberle S, Wutte C, Bauer C, von Oldenburg G, Panzer S, Augat P. Evaluation of risk for secondary fracture after removal of a new femoral neck plate for intracapsular hip fractures. J Orthop Trauma, 2011, 25: 721–725. [DOI] [PubMed] [Google Scholar]
- 10. Gotfried Y. Percutaneous compression plating of intertrochanteric hip fractures. J Orthop Trauma, 2000, 14: 490–495. [DOI] [PubMed] [Google Scholar]
- 11. Brandt E, Verdonschot N, van Vugt A, van Kampen A. Biomechanical analysis of the percutaneous compression plate and sliding hip screw in intracapsular hip fractures: experimental assessment using synthetic and cadaver bones. Injury, 2006, 37: 979–983. [DOI] [PubMed] [Google Scholar]
- 12. Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma, 2015, 29(3): 121–129. [DOI] [PubMed] [Google Scholar]
- 13. Bartonicek J. Pauwels’ classification of femoral neck fractures: correct interpretation of the original. J Orthop Trauma, 2001, 15: 358–360. [DOI] [PubMed] [Google Scholar]
- 14. Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am, 1970, 52: 457–467. [PubMed] [Google Scholar]
- 15. Karanicolas PJ, Bhandari M, Walter SD, et al Interobserver reliability of classification systems to rate the quality of femoral neck fracture reduction. J Orthop Trauma, 2009, 23: 408–412. [DOI] [PubMed] [Google Scholar]
- 16. Seyfettinoğlu F, Ersan O, Kovalak E, Duygun F, Ozsar B, Ateş Y. Fixation of femoral neck fractures with three screws: results and complications. Acta Orthop Traumatol Turc, 2011, 45: 6–13. [DOI] [PubMed] [Google Scholar]
- 17. Nowotarski PJ, Ervin B, Weatherby B, Pettit J, Goulet R, Norris B. Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel's type C femoral neck fractures. Injury, 2012, 43: 802–806. [DOI] [PubMed] [Google Scholar]
- 18. Aminian A, Gao F, Fedoriw WW, Zhang LQ, Kalainov DM, Merk BR. Vertically oriented femoral neck fractures: mechanical analysis of four fixation techniques. J Orthop Trauma, 2007, 21: 544–548. [DOI] [PubMed] [Google Scholar]
- 19. Makki D, Mohamed AM, Gadiyar R, Patterson M. Addition of an anti‐rotation screw to the dynamic hip screw for femoral neck fractures. Orthopedics, 2013, 36: e865–e888. [DOI] [PubMed] [Google Scholar]
- 20. Brighton CT, Fisher JR Jr, Levine SE, et al The biochemical pathway mediating the proliferative response of bone cells to a mechanical stimulus. J Bone Joint Surg Am, 1996, 78: 1337–1347. [DOI] [PubMed] [Google Scholar]
- 21. Brandt SE. A new and stable implant in the treatment of the intracapsular hip fracture: a case report. Injury Extra, 2008, 39: 137–139. [Google Scholar]
- 22. Mukherjee P, Ashworth MJ. A new device to treat intra‐capsular fracture neck of femur non‐union. Strateg Trauma Limb Reconstr, 2010, 5: 159–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Parker M, Cawley S, Palial V. Internal fixation of intracapsular fractures of the hip using a dynamic locking plate: two‐year follow‐up of 320 patients. Bone Joint J, 2013, 95: 1402–1405. [DOI] [PubMed] [Google Scholar]
- 24. Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br, 2000, 82: 679–683. [DOI] [PubMed] [Google Scholar]
- 25. Crawfurd EJ, Emery RJ, Hansell DM, Phelan M, Andrews BG. Capsular distension and intracapsular pressure in subcapital fractures of the femur. J Bone Joint Surg Br, 1988, 70: 195–198. [DOI] [PubMed] [Google Scholar]
- 26. Holmberg S, Dalen N. Intracapsular pressure and caput circulation in nondisplaced femoral neck fractures. Clin Orthop Relat Res, 1987, 219: 124–126. [PubMed] [Google Scholar]
- 27. Razik F, Alexopoulos AS, El‐Osta B, et al Time to internal fixation of femoral neck fractures in patients under sixty years–does this matter in the development of osteonecrosis of femoral head? Int Orthop, 2012, 36: 2127–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wongwai T, Wajanavisit W, Woratanarat P. Non‐union and avascular necrosis of delayed reduction and screw fixation in displaced femoral neck fracture in young adults. J Med Assoc Thai, 2012, 95 (Suppl. 10): S120–S127. [PubMed] [Google Scholar]


