Abstract
Objective: To study the clinical features and diagnosis of bursal‐side partial‐thickness rotator cuff tears.
Methods: From August 1999 to June 2006, 38 patients with bursal‐side partial‐thickness rotator cuff tear were evaluated. Twenty‐eight men and ten women of average age 45.7 years (range, 18–69 years) with 11 left and 27 right shoulders were studied. According to the Ellman classification, 6 cases were classified as grade I, 7 as II and 25 as III. Physical and X‐ray examination, including anteroposterior and supraspinatus outlet views, were performed on both shoulders of all patients. Ultrasonography and MR examination were performed in 27 and 35 patients, respectively. Thirteen patients underwent arthroscopic subacromial decompression and debridement of the rotator cuff. Twenty five patients underwent arthroscopic or mini‐open subacromial decompression and rotator cuff repair.
Results: All patients had shoulder pain, with 18 cases of night pain. No statistical difference in the incidence of night pain was found between the three groups. Strength of forward flexion and abduction of the affected shoulder was decreased in 25 patients. The Neer impingement sign was found in 35 cases (92.1%), Hawkins impingement sign in 27 (71.1%), tenderness of the greater tuberosity in 34 (89.5%), painful arc in 26 (68.4%), and traction test in 26 (68.4%). The positive rates for ultrasonography and MR were 48.1% and 74.3%, respectively.
Conclusions: Long‐standing motion pain, impingement sign, painful arc, lock and crepitus in the subacromial space are suggestive of bursal‐side tears. MRI is much more accurate than ultrasonography. Fat‐suppressed T2‐weighted images must be included. Arthroscopy is still the gold standard for making the diagnosis.
Keywords: Lacerations, Magnetic resonance imaging, Rotator cuff, Shoulder joint, Ultrasonography
Introduction
Rotator cuff tear is the main reason for pain and dysfunction of the shoulder joint. The estimated prevalence of partial‐thickness rotator cuff tears is significant, and can be expected to increase in light of our aging population and the association between increasing age and rotator cuff pathology. Unfortunately, compared with full‐thickness tears, there is little concern about partial‐thickness tears because of the difficulty in making this diagnosis. The accuracy of ultrasonography and MR for diagnosing partial‐thickness tears is less than that for full‐thickness tears. There is no consensus on a single algorithmic treatment approach for patients with symptomatic, partial‐thickness rotator cuff tear. With development of MRI and arthroscopic technology, partial‐thickness tears of the rotator cuff have received more attention, including many descriptive reports 1 , 2 , 3 , 4 , 5 , 6 . In this study, data from 38 patients with bursal‐side partial‐thickness rotator cuff tear has been analyzed to summarize its clinical features and diagnosis.
Materials and methods
Patient data
From August 1999 to June 2006, 38 patients with bursal‐side partial‐thickness rotator cuff tear were evaluated. The diagnosis was confirmed by arthroscopy in all patients. There were 28 men and 10 women, with an average age of 45.7 years (range, 18–69 years). Eleven left and 27 right shoulders were involved. The duration of shoulder pain ranged from 10 days to 20 years with an average of 24 months. Twenty‐ three patients had a history of acute trauma to the shoulder.
Clinical evaluation
Before surgery, all patients were evaluated by personal interview and physical examination of both shoulders. Physical examination included assessment of active and passive range of motion (ROM), muscle strength, tenderness and some special tests such as the Neer impingement sign 7 , painful arc, and Jobe test.
Imaging evaluation
Plain radiographs
All patients underwent plain radiography, including anteroposterior and supraspinatus outlet views. Acromial morphology was divided into three categories according to the Bigliani classification 8 .
Ultrasonography (US)
Twenty seven patients underwent US of both shoulders, all examinations being performed by the same doctor. Signs considered diagnostic of bursal‐side partial‐thickness tear included a defect on the bursal side of the rotator cuff, distinct hypoechoic or mixed echo on the bursal side of the rotator cuff, or focal thinning of the tendon.
MRI
Thirty five patients underwent MR examination. The diagnosis was made mainly on the basis of oblique coronal fat‐depressed T2 images. Signs considered diagnostic of bursal‐side partial‐thickness rotator cuff tear included a defect on the bursal side of the rotator cuff, and a fluid‐intensity signal within the tendons which are in contact with bursal side of the rotator cuff.
Operative methods
All patients underwent arthroscopic inspection of the shoulder joint and subacromial space. Six cases were classified as grade I, 7 as II and 25 as III according to the Ellman classification 4 . Thirteen patients underwent arthroscopic subacromial decompression and debridement of the rotator cuff. Twenty‐five patients underwent arthroscopic or mini‐open subacromial decompression and rotator cuff repair.
Statistical analysis
Fisher's exact test was used to compare the incidence of night pain between grade I, grade II and grade III groups by using SPSS 11.5 software. P < 0.05 was considered to be statistically significant.
Results
All patients had shoulder pain. Eighteen patients experienced consistent pain including night pain (Table 1). Sixteen patients complained of pain after light activities. Three patients felt pain after sport and one during sports training. Nine patients experienced muscle weakness. Although the incidence of night pain was greater in the grade III group, no statistical difference was found between grade I, grade II and grade III groups (P= 0.095).
Table 1.
Relationship between night pain and tear
| Tear degree | Number | Night pain | No night pain |
|---|---|---|---|
| Grade I, II | 13 | 4 | 9 |
| Grade III | 25 | 14 | 11 |
The active ROM of the shoulder joint in flexion and abduction are shown in Table 2. Muscle strength in flexion and abduction was grade 5 in 13 patients and grade 4 in 25. The Neer impingement sign was found in 35 cases (35/38, 92.1%), Hawkins impingement sign in 27 (27/38, 71.1%), tenderness of the greater tuberosity in 34 (34/38, 89.5%), painful arc in 26 (26/38, 68.4%), traction test in 26 (26/38, 68.4%), supraspinatus test in 22 (22/38, 57.9%), and four patients had crepitus in the subacromial space.
Table 2.
Number of patients with varying angles of active flexion and abduction
| Items | >150° | 121°–150° | 91°–120° | 46°–90° | 30°–45° |
|---|---|---|---|---|---|
| Active flexion | 24 | 4 | 1 | 7 | 2 |
| Active abduction | 26 | 3 | 1 | 6 | 2 |
Results of X‐ray examination
According to the Bigliani classification 8 , 2 patients had a flat, 26 a curved and 10 a hooked acromion. Sclerotic change on the undersurface of the acromion and greater tubercle was seen in 36 patients. Cortical cystic changes in the greater tubercle were seen in 32 patients.
Results of US
Results of US are shown in Table 3. The features of the thirteen correctly diagnosed cases included defects on the bursal side of the cuff in four patients, distinct hypoechoic or mixed echoes on the bursal side of the cuff in six and thinning of the tendon in three.
Table 3.
Diagnostic value of US and MR
| Items | Bursal‐side tear | Full‐thickness tear | No tear | Articular‐side tear | Interstitial tear | Positive rate (%) |
|---|---|---|---|---|---|---|
| US (n= 27) | 13 | 4 | 8 | 1 | 1 | 48.1 (13/27) |
| MR (n= 35) | 26 | 1 | 7 | 1 | — | 74.3 (26/35) |
Results of MR examination
Results of MR are shown in Table 3. The images of the 26 correctly diagnosed cases included defects on the bursal side of the cuff in 4 patients and fluid‐intensity signal within the tendons extending to the bursal surface of the cuff in 17.
Concomitant injuries
Concomitant injuries included articular‐side tear of the rotator cuff in 2 cases, partial tear of the subscapular tendon in 3, inflammation of the long head of the biceps tendon (LHBT) in 22, partial tear of the LHBT in 1, superior labrum anterior and posterior (SLAP) I injury in 15, SLAP II injury in 2, and posterior‐superior labrum injury in 1.
Discussion
Partial‐thickness tears of the rotator cuff are not rare. Cadaver study has consistently shown that partial‐thickness tears are more common than full‐thickness ones 9 . Ellman divided partial‐thickness tears of the rotator cuff into three types according to the site of the tear: bursal side tear, articular side tear and interstitial tear (1, 2, 3) 4 . Each type is divided into three grades according to tear depth, that is, grade I: tears less than 3 mm; grade II: tears of 3 to 6 mm; and grade III: tears more than half the thickness of the tendon (4, 5, 6). Many studies have shown that articular side tear occurs more frequently than bursal side tear. Partial tears are found almost exclusively in the supraspinatus tendon 1 , 2 , 3 , 4 , 5 , 6 .
Figure 1.
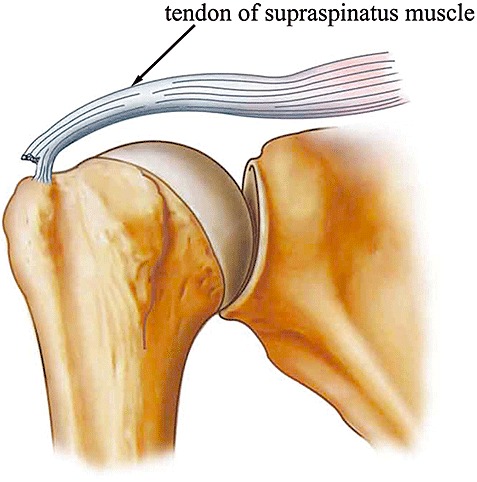
Diagrammatic representation of a bursal side tear.
Figure 2.
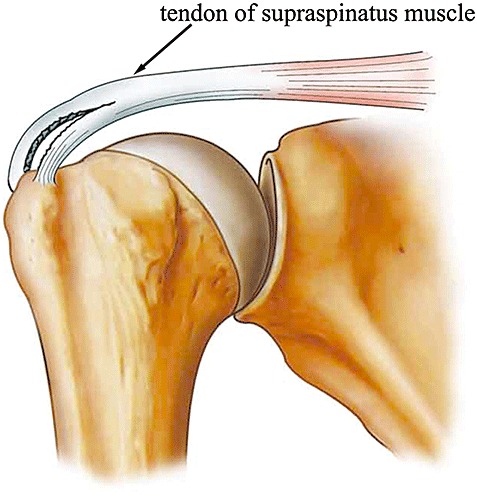
Diagrammatic representation of an articular side tear.
Figure 3.
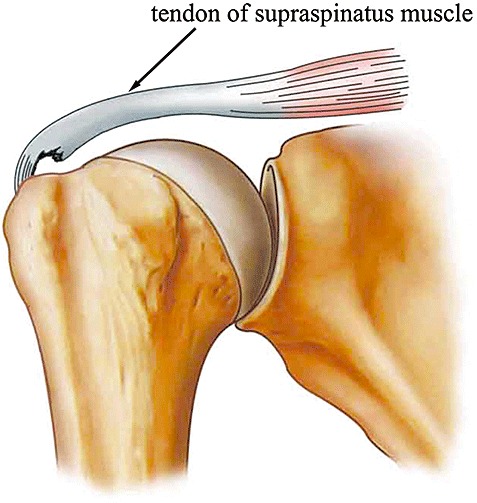
Diagrammatic representation of an interstitial tear.
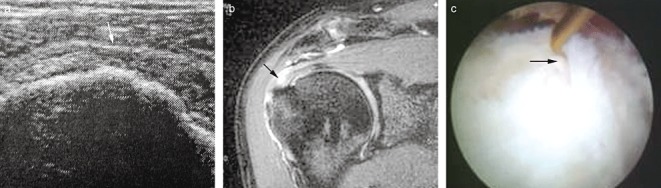
Figure 4.

Grade I tear (a) US showing high intensity signal on the bursal side of the supraspinatus tendon (black arrow); (b) MRI showing high intensity signal on the bursal side of the supraspinatus tendon (black arrow); (c) Arthroscopic view, showing irregularity and wear on the bursal side of the supraspinatus tendon (black arrow).
Figure 5.
Grade II tear (a) US showing a partial defect on the bursal side of the supraspinatus tendon (white arrow); (b) MRI showing high intensity signal involving less than half of the tendon thickness (black arrow); (c) Arthroscopic view, showing tear involving less than half of the tendon thickness (black arrow).
Figure 6.

Grade III tear (a) US showing that the supraspinatus tendon has become thinner (white arrow); (b) MRI showing an extensive tear on the bursal side of the supraspinatus tendon (white arrow); (c) Arthroscopic view, showing an extensive tear on the bursal side of the supraspinatus tendon with retraction of the stump (black arrows), and some residual tendon on the articular side (white arrow).
Factors related to the development of partial‐thickness tears are classified as intrinsic, and extrinsic or traumatic. Fukuda has hassuggested that subacromial impingement is the main reason for bursal side tears 9 . Ellman has suggested that type II and III acromial tears tend to cause subacromial impingement 4 . In the present study, 36 patients had type II or III acromions, which indicates that subacromial impingement is an important reason for bursal side tears.
Diagnosis of bursal side partial‐thickness tear remains difficult 1 , 5 . Compared with cuff inflammation and full thickness tears, its clinical features are nonspecific. Patients often report pain and stiffness of the affected shoulder. Nocturnal pain and pain exacerbated by overhead activity are common. Fukuda has stressed that partial tears can be more painful than full‐thickness tears 9 . As to the incidence of night pain, Guo‐qing Cui reported that no statistically significant difference was found between a partial‐thickness tear group and a no tear group, and therefore concluded that night pain is not helpful in predicting the existence of tears 10 .In the present study, the incidence of night pain was higher in the grade III group, but no statistical difference was found compared with the grade I and II groups, suggesting that night pain has no definite value in judging the degree of tears. Some bursal‐side tears can lead to lock and crepitus in the subacromial space, which can be helpful in making the diagnosis. In the present study, all patients had shoulder pain, with 18 cases of night pain. As for physical examination, some authors have reported that impingement signs, painful arc 2 , 10 , crepitus and tenderness of the greater tuberosity 8 , 10 have a high positive rate. Usually, muscle weakness is not evident because of the remaining tendon fibers. In this study, signs which were often positive included the Neer impingement sign, tenderness of the greater tuberosity, and painful arc.
In the past, bursography has been used to demonstrate bursal‐side tears but its accuracy is not high 9 . Fukuda has suggested that subacromial inflammation and adhesions probably limit its accuracy 9 . In recent years, with the development of US and MR, both methods have become routine for the diagnosis of rotator cuff tears. Several authors have found that both methods are highly accurate for diagnosing full‐thickness tears, but that their accuracy in diagnosing partial tears is not high. Teefey et al. have reported that the accuracy of US and MRI for diagnosing full‐thickness tears is 98% and 100%, respectively, but the accuracy is only 68% and 63% for partial tears 11 .
US is a dynamic examination that can provide bilateral information. It is well tolerated and less expensive and time‐consuming than MRI 12 . However, it is more dependent on the skill and experience of the operator in both performance and interpretation. The diagnostic signs of bursal‐side partial‐thickness tear include: (i) a defect on the bursal side of the cuff due to the tendon having retracted from the bone, producing a “bare area”; (ii) distinct hypoechoic or mixed echo on the bursal side of the cuff, the abnormal echo probably representing a new acoustic interface produced by a tear within the tendon; and (iii) the tendon has become thinner 11 , 12 , 13 . However, it is difficult to distinguish partial‐thickness tears from scarring within the tendon or small full‐thickness lesions. Because of tendon retraction, extensive partial tears often demonstrate a focal defect simulating a full‐thickness tear. In addition, if the ROM is limited during examination, especially in extension and rotation, some small tears can be missed. Of the patients reported here, US correctly identified 13 cases whose images corresponded to one of these three signs. A full‐thickness tear rather than a partial tear was incorrectly identified in four cases whose tears were extensive grade III tears. Eight false‐negatives occurred, among which were two grade I tears, two grade II tears, and four grade III tears, of which two were longitudinal tears.
MR is less operator‐dependent, provides images that are inherently easier for orthopaedic surgeons to review, and is better for the evaluation of other structures, such as the labrum, articular cartilage and surrounding muscles and bone, for morphologic changes that may contribute to the patient's symptoms 14 . However, it is more expensive. The diagnostic signs of bursal‐side partial‐thickness tear include: (i) a defect on the bursal side of the cuff, and (ii) fluid‐intensity signal within the tendons extending to the bursal surface 11 . A grade III bursal‐side tear appears as a focal defect, which simulates a full‐thickness tear on MR 11 . As for grade I and II tears, MR usually shows a fluid‐intensity signal within the tendons that cannot be distinguished from degeneration and inflammation. A full‐thickness, rather than a partial, tear was incorrectly identified in one case whose tear was an extensive grade III one. There were seven false‐negatives, among which were three grade 1 tears, one grade II tear, and three grade III tears, among which two were longitudinal tears. Because MR arthrography (MRA) does not contribute to the diagnosis, routine MR is adequate. Compared with T1‐weighted images, fat‐suppressed T2‐weighted images can show fluid‐intensity signal within the tendons more clearly (Fig. 7). Of the seven false‐negatives, three cases did not have fat‐suppressed T2‐weighted images when their shoulders were subject to MRA.
Figure 7.
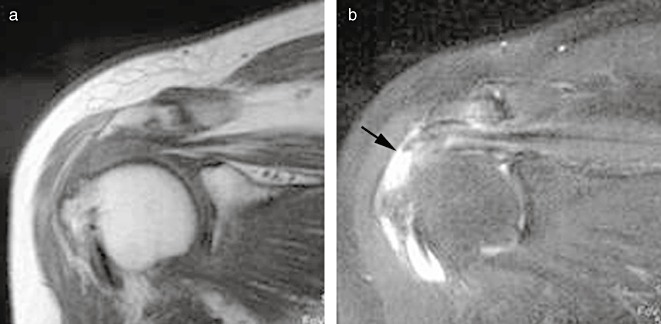
Compared with (a) T1‐weighted images, (b) fat‐suppressed T2‐weighted images can show fluid‐intensity signal (black arrow) within the tendons more clearly.
Arthroscopy is still the gold standard for diagnosing partial tears 1 . Bursal‐side tears usually lie in the anterior part of the supraspinatus tendon, and the supraspinatus tendon adjacent to the biceps tendon must be inspected. Once the tears have been found, degenerative and scar tissue should be thoroughly resected in order to confirm their size and depth.
Conclusion
Bursal‐side partial‐thickness rotator cuff tears are not rare. Long‐standing motion pain, impingement signs, painful arc, lock and crepitus in the subacromial space are suggestive of bursal‐side tears. Compared with that of US, the accuracy of MR is much higher. Fat‐suppressed T2‐weighted images must be performed. Arthroscopy is still the gold standard for making this diagnosis.
Disclosure
Neither authors nor a member of their immediate families received funding, grants, payments, or other benefits from any commercial entity.
References
- 1. Weber SC. Arthroscopic debridement and acromioplasty versus mini‐open repair in the treatment of significant partial‐thickness rotator cuff tears. Arthroscopy, 1999, 15: 126–131. [DOI] [PubMed] [Google Scholar]
- 2. Lyons TR, Savoie FH 3rd, Field LD. Arthroscopic repair of partial‐thickness tears of the rotator cuff. Arthroscopy, 2001, 17: 219–223. [DOI] [PubMed] [Google Scholar]
- 3. Cordasco FA, Backer M, Craig EV, et al The partial‐thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med, 2002, 30: 257–260. [DOI] [PubMed] [Google Scholar]
- 4. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res, 1990, 254: 64–74. [PubMed] [Google Scholar]
- 5. Itoi E, Tabata S. Incomplete rotator cuff tears. Results of operative treatment. Clin Orthop Relat Res, 1992, 284: 128–135. [PubMed] [Google Scholar]
- 6. Park JY, Chung KT, Yoo MJ. A serial comparison of arthroscopic repairs for partial‐ and full‐thickness rotator cuff tears. Arthroscopy, 2004, 20: 705–711. [DOI] [PubMed] [Google Scholar]
- 7. Neer CS 2nd. Impingement lesions. Clin Orthop Relat Res, 1983, 173: 70–78. [PubMed] [Google Scholar]
- 8. Millstein ES, Snyder SJ. Arthroscopic evaluation and management of rotator cuff tears. Orthop Clin North Am, 2003, 34: 507–520. [DOI] [PubMed] [Google Scholar]
- 9. Fukuda H. The management of partial‐thickness tears of the rotator cuff. J Bone Joint Surg Br, 2003, 85: 3–11. [DOI] [PubMed] [Google Scholar]
- 10. Cui GQ, Ao YF, Yu CL, et al A clinical analysis of 38 cases of subacromial impingement syndrome (Chin). Zhonghua Gu Ke Za Zhi, 2000, 20: 467–469. [Google Scholar]
- 11. Teefey SA, Rubin DA, Middleton WD, et al Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy‐one consecutive cases. J Bone Joint Surg Am, 2004, 86‐A: 708–716. [PubMed] [Google Scholar]
- 12. Lin FJ, Cui GQ, Zhang W, et al Ultrasonography of rotator cuff tear (Chin). Zhongguo Chao Sheng Yi Xue Za Zhi, 2001, 17: 224–226. [Google Scholar]
- 13. Lü K, Jiang YX. Ultrasonography of normal rotator cuff and rotator cuff tear (Chin). Zhonghua Yi Xue Chao Sheng Za Zhi, 2005, 14: 154–155. [Google Scholar]
- 14. Zheng ZZ, Xie JX, Fan JD, et al Rotator cuff diseases: a comparative study of X‐arthrography, conventional MRI, and MRI arthrography (Chin). Zhonghua Gu Ke Za Zhi, 2001, 21: 412–416. [Google Scholar]


